Abstract
The natural history of ovarian cancer continues to be characterized by late-stage presentation, metastatic bulky disease burden and stagnant mortality statistics, despite prolific drug development. Robust clinical investigation, particularly with modifications to primary treatment surgical goals and adjuvant therapy are increasing median progression-free survival and overall survival, although the cure rates have been affected only modestly. Maintenance therapy holds promise, but studies have yet to identify an agent and/or strategy that can affect survival. Recurrent disease is largely an incurable state; however, current intervention with selected surgery, combination and targeted therapy and investigational protocols are impacting progression-free survival. Ovarian cancer is a diverse and genomically complex disease, which commands global attention. Rational investigation must balance the high rate of discovery with lagging clinical investigation and limited patient resources. Nevertheless, growth in our armamentarium offers unprecedented opportunities for patients suffering with this disease. This Review presents and reviews the contemporary management of the disease spectrum termed epithelial 'ovarian' cancer and describes the direction and early results of clinical investigation.
Key Points
-
Ovarian cancer continues to be characterized by late-stage presentation and bulky intraperitoneal disease burden at presentation
-
Surgery and chemotherapy are the mainstays of primary therapy; 'optimal' surgical cytoreduction is being re-defined as resection of all macroscopic disease
-
Advances in adjuvant chemotherapy have leveraged intraperitoneal administration, dose-dense paclitaxel and the addition of biological agents predominately targeting angiogenesis
-
Maintenance therapy is a promising strategy as a primary or subsequent adjuvant approach, but as yet is not been proven to increase overall survival
-
Recurrence therapy has improved post-progression outcomes, although cures are elusive
-
Closely tied to a wider understanding of the underlying biology of ovarian cancer, drug development is increasingly focused on specific new targets in the hope of optimizing the therapeutic index
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Chen, C. Y. et al. Long-term disease-free survival in three ovarian cancer patients with a single relapse. Eur. J. Gynaecol. Oncol. 33, 321–323 (2012).
Lee, Y. et al. A candidate precursor to serous carcinoma that originates in the distal fallopian tube. J. Pathol. 211, 26–35 (2007).
Singer, G., Shih, I.-M., Truskinovsky, A., Umudum, H. & Kurman, R. J. Mutational analysis of K-ras segregates ovarian serous carcinomas into two types: invasive MPSC (low-grade tumor) and conventional serous carcinoma (high-grade tumor). Int. J. Gynecol. Pathol. 22, 37–41 (2003).
Wu, R., Hu, T. C., Rehemtulla, A., Fearon, E. R. & Cho, K. R. Preclinical testing of PI3K/AKT/mTOR signaling inhibitors in a mouse model of ovarian endometrioid adenocarcinoma. Clin. Cancer Res. 17, 7359–7372 (2011).
Cancer Genome Atlas Research Network. Integrated genomic analyses of ovarian carcinoma. Nature 474, 609–615 (2011).
Berns, E. M. & Bowtell, D. D. The changing view of high-grade serous ovarian cancer. Cancer Res. 72, 2701–2704 (2012).
Bowtell, D. D. The genesis and evolution of high-grade serous ovarian cancer. Nat. Rev. Cancer 10, 803–808 (2010).
Tothill, R. W. et al. Novel molecular subtypes of serous and endometrioid ovarian cancer linked to clinical outcome. Clin. Cancer Res. 14, 5198–5208 (2008).
Wang, Z. C. et al. Profiles of genomic instability in high-grade serous ovarian cancer predict treatment outcome. Clin. Cancer Res. 18, 5806–5815 (2012).
Bottsford-Miller, J. N., Coleman, R. L. & Sood, A. K. Resistance and escape from antiangiogenesis therapy: clinical implications and future strategies. J. Clin. Oncol. 30, 4026–4034 (2012).
Lu, S. & Lu, X. Integrating genome and functional genomics data to reveal perturbed signaling pathways in ovarian cancers. AMIA Summits Transl. Sci. Proc. 2012, 72–78 (2012).
Hoskins, W. J. et al. The effect of diameter of largest residual disease on survival after primary cytoreductive surgery in patients with suboptimal residual epithelial ovarian carcinoma. Am. J. Obstet. Gynecol. 170, 974–979 (1994).
Inciura, A. et al. Comparison of adjuvant and neoadjuvant chemotherapy in the management of advanced ovarian cancer: a retrospective study of 574 patients. BMC Cancer 6, 153 (2006).
Bristow, R. E., Tomacruz, R. S., Armstrong, D. K., Trimble, E. L. & Montz, F. J. Survival effect of maximal cytoreductive surgery for advanced ovarian carcinoma during the platinum era: a meta-analysis. J. Clin. Oncol. 20, 1248–1259 (2002).
Young, R. C. et al. Staging laparotomy in early ovarian cancer. JAMA 250, 3072–3076 (1983).
Le, T., Faught, W., Hopkins, L. & Fung Kee Fung, M. Primary chemotherapy and adjuvant tumor debulking in the management of advanced-stage epithelial ovarian cancer. Int. J. Gynecol. Cancer 15, 770–775 (2005).
Griffiths, C. T. Surgical resection of tumor bulk in the primary treatment of ovarian carcinoma. Natl Cancer Inst. Monogr. 42, 101–104 (1975).
Fader, A. N. & Rose, P. G. Role of surgery in ovarian carcinoma. J. Clin. Oncol. 25, 2873–2883 (2007).
du Bois, A. et al. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: by the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzinom (AGO-OVAR) and the Groupe d'Investigateurs Nationaux Pour les Etudes des Cancers de l'Ovaire (GINECO). Cancer 115, 1234–1244 (2009).
Eisenhauer, E. L. et al. The effect of maximal surgical cytoreduction on sensitivity to platinum-taxane chemotherapy and subsequent survival in patients with advanced ovarian cancer. Gynecol. Oncol. 108, 276–281 (2008).
de Jong, D. et al. Preoperative predictors for residual tumor after surgery in patients with ovarian carcinoma. Oncology 72, 293–301 (2007).
Ivanov, S., Ivanov, S. & Khadzhiolov, N. Prognostic factors and better survival rate after the treatment of advanced ovarian cancer with neoadjuvant chemotherapy [Bulgarian]. Akush. Ginekol. (Sofiia) 43, 17–19 (2004).
Lee, S. J. et al. Preliminary results of neoadjuvant chemotherapy with paclitaxel and cisplatin in patients with advanced epithelial ovarian cancer who are inadequate for optimum primary surgery. J. Obstet. Gynaecol. Res. 32, 99–106 (2006).
Schwartz, P. E. Neoadjuvant chemotherapy for the management of ovarian cancer. Best Pract. Res. Clin. Obstet. Gynaecol. 16, 585–596 (2002).
Vergote, I. B. et al. Neoadjuvant chemotherapy versus primary debulking surgery in advanced ovarian cancer. Semin. Oncol. 27 (3 Suppl. 7), 31–36 (2000).
Vergote, I. et al. Neoadjuvant chemotherapy is the better treatment option in some patients with stage IIIc to IV ovarian cancer. J. Clin. Oncol. 29, 4076–4078 (2011).
Bristow, R. E. & Chi, D. S. Platinum-based neoadjuvant chemotherapy and interval surgical cytoreduction for advanced ovarian cancer: a meta-analysis. Gynecol. Oncol. 103, 1070–1076 (2006).
du Bois, A. et al. Neoadjuvant chemotherapy cannot be regarded as adequate routine therapy strategy of advanced ovarian cancer. Int. J. Gynecol. Cancer 22, 182–185 (2012).
Steed, H. et al. A retrospective analysis of neoadjuvant platinum-based chemotherapy versus up-front surgery in advanced ovarian cancer. Int. J. Gynecol. Cancer 16 (Suppl. 1), 47–53 (2006).
Vergote, I. et al. Neoadjuvant chemotherapy or primary surgery in stage IIIC or IV ovarian cancer. N. Engl. J. Med. 363, 943–953 (2010).
Chi, D. S. et al. An analysis of patients with bulky advanced stage ovarian, tubal, and peritoneal carcinoma treated with primary debulking surgery (PDS) during an identical time period as the randomized EORTC-NCIC trial of PDS vs neoadjuvant chemotherapy (NACT). Gynecol. Oncol. 124, 10–14 (2012).
Morrison, J., Haldar, K., Kehoe, S. & Lawrie, T. A. Chemotherapy versus surgery for initial treatment in advanced ovarian epithelial cancer. Cochrane Database of Systematic Reviews Issue 8. Art. No.: CD005343 http://dx.doi.org/10.1002/14651858.CD005343.pub3.
US National Library of Medicine. ClinicalTrials.gov, [online] (2011).
US National Library of Medicine. ClinicalTrials.gov, [online] (2012).
US National Library of Medicine. ClinicalTrials.gov, [online] (2012).
Greer, B. E. et al. Implications of second-look laparotomy in the context of optimally resected stage III ovarian cancer: a non-randomized comparison using an explanatory analysis: a Gynecologic Oncology Group study. Gynecol. Oncol. 99, 71–79 (2005).
McGuire, W. P. et al. Cyclophosphamide and cisplatin compared with paclitaxel and cisplatin in patients with stage III and stage IV ovarian cancer. N. Engl. J. Med. 334, 1–6 (1996).
Piccart, M. J. et al. Randomized intergroup trial of cisplatin-paclitaxel versus cisplatin-cyclophosphamide in women with advanced epithelial ovarian cancer: three-year results. J. Natl Cancer Inst. 92, 699–708 (2000).
du Bois, A. et al. A randomized clinical trial of cisplatin/paclitaxel versus carboplatin/paclitaxel as first-line treatment of ovarian cancer. J. Natl Cancer Inst. 95, 1320–1329 (2003).
Calvert, A. H. et al. Carboplatin dosage: prospective evaluation of a simple formula based on renal function. J. Clin. Oncol. 7, 1748–1756 (1989).
Jelliffe, R. Estimation of creatinine clearance in patients with unstable renal function, without a urine specimen. Am. J. Nephrol. 22, 320–324 (2002).
Ozols, R. F. et al. Phase III trial of carboplatin and paclitaxel compared with cisplatin and paclitaxel in patients with optimally resected stage III ovarian cancer: a Gynecologic Oncology Group study. J. Clin. Oncol. 21, 3194–3200 (2003).
Katsumata, N. et al. Dose-dense paclitaxel once a week in combination with carboplatin every 3 weeks for advanced ovarian cancer: a phase 3, open-label, randomised controlled trial. Lancet 374, 1331–1338 (2009).
Norton, L. Use of dose-dense chemotherapy in the management of breast cancer. Clin. Adv. Hematol. Oncol. 4, 36–37 (2006).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
Echarri Gonzalez, M. J., Green, R. & Muggia, F. M. Intraperitoneal drug delivery for ovarian cancer: why, how, who, what, and when? Oncology (Williston Park) 25, 156–165, 170 (2011).
Gore, M., du Bois, A. & Vergote, I. Intraperitoneal chemotherapy in ovarian cancer remains experimental. J. Clin. Oncol. 24, 4528–4530 (2006).
Armstrong, D. K. et al. Intraperitoneal cisplatin and paclitaxel in ovarian cancer. N. Engl. J. Med. 354, 34–43 (2006).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
Schmitt, J. & Matei, D. Targeting angiogenesis in ovarian cancer. Cancer Treat. Rev. 38, 272–283 (2012).
Burger, R. A. et al. Incorporation of bevacizumab in the primary treatment of ovarian cancer. N. Engl. J. Med. 365, 2473–2483 (2011).
Perren, T. J. et al. A phase 3 trial of bevacizumab in ovarian cancer. N. Engl. J. Med. 365, 2484–2496 (2011).
Rubin, S. C. et al. Prognostic factors for recurrence following negative second-look laparotomy in ovarian cancer patients treated with platinum-based chemotherapy. Gynecol. Oncol. 42, 137–141 (1991).
Chu, C. S. & Rubin, S. C. Second-look laparotomy for epithelial ovarian cancer: a reappraisal. Curr. Oncol. Rep. 3, 11–18 (2001).
Markman, M. Maintenance chemotherapy: an evolving and increasingly acceptable strategy in cancer management. Curr. Oncol. Rep. 12, 349–351 (2010).
Herzog, T. J., Coleman, R. L., Markman, M., Cella, D. & Thigpen, J. T. The role of maintenance therapy and novel taxanes in ovarian cancer. Gynecol. Oncol. 102, 218–225 (2006).
Mei, L. et al. Maintenance chemotherapy for ovarian cancer. Cochrane Database of Systematic Reviews Issue 9. Art. No.: CD007414 http://dx.doi.org/10.1002/14651858.CD007414.pub2.
Vergote, I. B. et al. Randomized phase III study of erlotinib versus observation in patients with no evidence of disease progression after first-line platin-based chemotherapy for ovarian carcinoma: A GCIG and EORTC-GCG study [abstract]. J. Clin. Oncol. 30 (Suppl.), LBA5000 (2012).
US National Library of Medicine. ClinicalTrials.gov [online], (2011).
Markman, M. et al. Phase III randomized trial of 12 versus 3 months of maintenance paclitaxel in patients with advanced ovarian cancer after complete response to platinum and paclitaxel-based chemotherapy: a Southwest Oncology Group and Gynecologic Oncology Group trial. J. Clin. Oncol. 21, 2460–2465 (2003).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
Herzog, T. J. & Pothuri, B. Ovarian cancer: a focus on management of recurrent disease. Nat. Clin. Pract. Oncol. 3, 604–611 (2006).
Kew, F., Galaal, K., Bryant, A. & Naik, R. Evaluation of follow-up strategies for patients with epithelial ovarian cancer following completion of primary treatment. Cochrane Database of Systematic Reviews Issue 6. Art. No.: CD006119 http://dx.doi.org/10.1002/14651858.CD006119.pub2.
Rustin, G. J. et al. Early versus delayed treatment of relapsed ovarian cancer (MRC OV05/EORTC 55955): a randomised trial. Lancet 376, 1155–1163 (2010).
Fleming, N. D., Cass, I., Walsh, C. S., Karlan, B. Y. & Li, A. J. CA125 surveillance increases optimal resectability at secondary cytoreductive surgery for recurrent epithelial ovarian cancer. Gynecol. Oncol. 121, 249–252 (2011).
Markman, M. et al. Second-line platinum therapy in patients with ovarian cancer previously treated with cisplatin. J. Clin. Oncol. 9, 389–393 (1991).
Naumann, R. W. & Coleman, R. L. Management strategies for recurrent platinum-resistant ovarian cancer. Drugs 71, 1397–1412 (2011).
Rose, P. G. et al. A phase II study of docetaxel in paclitaxel-resistant ovarian and peritoneal carcinoma: a Gynecologic Oncology Group study. Gynecol. Oncol. 88, 130–135 (2003).
Gordon, A. N. et al. Long-term survival advantage for women treated with pegylated liposomal doxorubicin compared with topotecan in a phase 3 randomized study of recurrent and refractory epithelial ovarian cancer. Gynecol. Oncol. 95, 1–8 (2004).
Ferrandina, G. et al. Phase III trial of gemcitabine compared with pegylated liposomal doxorubicin in progressive or recurrent ovarian cancer. J. Clin. Oncol. 26, 890–896 (2008).
ten Bokkel Huinink, W. et al. Topotecan versus paclitaxel for the treatment of recurrent epithelial ovarian cancer. J. Clin. Oncol. 15, 2183–2193 (1997).
Markman, M. et al. Phase II trial of weekly paclitaxel (80 mg/m2) in platinum and paclitaxel-resistant ovarian and primary peritoneal cancers: a Gynecologic Oncology Group study. Gynecol. Oncol. 101, 436–440 (2006).
Rosenberg, P. et al. Randomized trial of single agent paclitaxel given weekly versus every three weeks and with peroral versus intravenous steroid premedication to patients with ovarian cancer previously treated with platinum. Acta Oncol. 41, 418–424 (2002).
Piccart, M. J. et al. Oxaliplatin or paclitaxel in patients with platinum-pretreated advanced ovarian cancer: a randomized phase II study of the European Organization for Research and Treatment of Cancer Gynecology Group. J. Clin. Oncol. 18, 1193–1202 (2000).
Pujade-Lauraine, E. et al. AURELIA: A randomized phase III trial evaluating bevacizumab (BEV) plus chemotherapy (CT) for platinum (PT)-resistant recurrent ovarian cancer (OC) [abstract]. J. Clin. Oncol. 30 (Suppl.), LBA5002 (2012).
Monk, B. J. & Coleman, R. L. Changing the paradigm in the treatment of platinum-sensitive recurrent ovarian cancer: from platinum doublets to nonplatinum doublets and adding antiangiogenesis compounds. Int. J. Gynecol. Cancer 19 (Suppl. 2), S63–S67 (2009).
Monk, B. J., Dalton, H., Benjamin, I. & Tanovic´, A. Trabectedin as a new chemotherapy option in the treatment of relapsed platinum sensitive ovarian cancer. Curr. Pharm. Des. 18, 3754–3769 (2012).
Lorusso, D., Mancini, M., Di Rocco, R., Fontanelli, R. & Raspagliesi, F. The role of secondary surgery in recurrent ovarian cancer. Int. J. Surg. Oncol. 2012, 613980 (2012).
Lee, C. K. et al. Prognostic nomogram to predict progression-free survival in patients with platinum-sensitive recurrent ovarian cancer. Br. J. Cancer 105, 1144–1150 (2011).
Chi, D. S. et al. Guidelines and selection criteria for secondary cytoreductive surgery in patients with recurrent, platinum-sensitive epithelial ovarian carcinoma. Cancer 106, 1933–1939 (2006).
Tian, W. J. et al. A risk model for secondary cytoreductive surgery in recurrent ovarian cancer: an evidence-based proposal for patient selection. Ann. Surg. Oncol. 19, 597–604 (2012).
Tay, E. H., Grant, P. T., Gebski, V. & Hacker, N. F. Secondary cytoreductive surgery for recurrent epithelial ovarian cancer. Obstet. Gynecol. 99, 1008–1013 (2002).
Eisenkop, S. M., Friedman, R. L. & Spirtos, N. M. The role of secondary cytoreductive surgery in the treatment of patients with recurrent epithelial ovarian carcinoma. Cancer 88, 144–153 (2000).
Benedetti Panici, P. et al. Secondary cytoreductive surgery in patients with platinum-sensitive recurrent ovarian cancer. Ann. Surg. Oncol. 14, 1136–1142 (2007).
Harter, P. et al. Surgery in recurrent ovarian cancer: the Arbeitsgemeinschaft Gynaekologische Onkologie (AGO) DESKTOP OVAR trial. Ann. Surg. Oncol. 13, 1702–1710 (2006).
Harter, P. et al. Prospective validation study of a predictive score or operability of recurrent ovarian cancer: the Multicenter Intergroup Study DESKTOP II. A project of the AGO Kommission OVAR, AGO Study Group, NOGGO, AGO-Austria, and MITO. Int. J. Gynecol. Cancer 21, 289–295 (2011).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
US National Library of Medicine. ClinicalTrials.gov [online], (2013).
Zang, R. Y. et al. Predictors of survival in patients with recurrent ovarian cancer undergoing secondary cytoreductive surgery based on the pooled analysis of an international collaborative cohort. Br. J. Cancer 105, 890–896 (2011).
Burger, R. A., Sill, M. W., Monk, B. J., Greer, B. E. & Sorosky, J. I. Phase II trial of bevacizumab in persistent or recurrent epithelial ovarian cancer or primary peritoneal cancer: a Gynecologic Oncology Group Study. J. Clin. Oncol. 25, 5165–5171 (2007).
Hata, K. et al. Expression of the angopoietin-1, angopoietin-2, Tie2, and vascular endothelial growth factor gene in epithelial ovarian cancer. Gynecol. Oncol. 93, 215–222 (2004).
Sallinen, H. et al. Cotargeting of VEGFR-1 and -3 and angiopoietin receptor Tie2 reduces the growth of solid human ovarian cancer in mice. Cancer Gene Ther. 18, 100–109 (2011).
Sood, A. K., Coleman, R. L. & Ellis, L. M. Moving beyond anti-vascular endothelial growth factor therapy in ovarian cancer. J. Clin. Oncol. 30, 345–347 (2012).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
Monk, B. J. et al. Trabectedin plus pegylated liposomal doxorubicin in recurrent ovarian cancer. J. Clin. Oncol. 28, 3107–3114 (2010).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
Vaughan, S. et al. Rethinking ovarian cancer: recommendations for improving outcomes. Nat. Rev. Cancer 11, 719–725 (2011).
Kuo, K. T. et al. Analysis of DNA copy number alterations in ovarian serous tumors identifies new molecular genetic changes in low-grade and high-grade carcinomas. Cancer Res. 69, 4036–4042 (2009).
Kuo, K. T. et al. Frequent activating mutations of PIK3CA in ovarian clear cell carcinoma. Am. J. Pathol. 174, 1597–1601 (2009).
Farley, J. H. et al. A phase II trial of selumetinib in women with recurrent low-grade serous carcinoma of the ovary or peritoneum [abstract]. Cancer Res. 72 (Suppl. 1), CT-05 (2012).
Gershenson, D. M. et al. Recurrent low-grade serous ovarian carcinoma is relatively chemoresistant. Gynecol. Oncol. 114, 48–52 (2009).
Cancer Genome Atlas Network. Comprehensive molecular portraits of human breast tumours. Nature 490, 61–70 (2012).
Yang, D. et al. Association of BRCA1 and BRCA2 mutations with survival, chemotherapy sensitivity, and gene mutator phenotype in patients with ovarian cancer. JAMA 306, 1557–1565 (2011).
Farmer, H. et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature 434, 917–921 (2005).
Fong, P. C. et al. Inhibition of poly(ADP-ribose) polymerase in tumors from BRCA mutation carriers. N. Engl. J. Med. 361, 123–134 (2009).
Kaye, S. B. et al. Phase II, open-label, randomized, multicenter study comparing the efficacy and safety of olaparib, a poly (ADP-ribose) polymerase inhibitor, and pegylated liposomal doxorubicin in patients with BRCA1 or BRCA2 mutations and recurrent ovarian cancer. J. Clin. Oncol. 30, 372–379 (2012).
Ledermann, J. et al. Olaparib maintenance therapy in platinum-sensitive relapsed ovarian cancer. N. Engl. J. Med. 366, 1382–1392 (2012).
Oza, A. M. et al. Olaparib plus paclitaxel and carboplatin (P/C) followed by olaparib maintenance treatment in patients (pts) with platinum-sensitive recurrent serous ovarian cancer (PSR SOC): A randomized, open-label phase II study [abstract]. J. Clin. Oncol. 30 (Suppl.), a5001 (2012).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
Pecot, C. V., Calin, G. A., Coleman, R. L., Lopez-Berestein, G. & Sood, A. K. RNA interference in the clinic: challenges and future directions. Nat. Rev. Cancer 11, 59–67 (2011).
Strait, K. A. et al. Histone deacetylase inhibitors induce G2-checkpoint arrest and apoptosis in cisplatinum-resistant ovarian cancer cells associated with overexpression of the Bcl-2-related protein Bad. Mol. Cancer Ther. 4, 603–611 (2005).
Oda, K. et al. PIK3CA cooperates with other phosphatidylinositol 3′-kinase pathway mutations to effect oncogenic transformation. Cancer Res. 68, 8127–8136 (2008).
Hill, T. P. Phase 0 clinical trials: towards a more complete ethics critique. Ecancermedicalscience 6, 248 (2012).
Kapiriri, L. et al. The case for conducting first-in-human (phase 0 and phase 1) clinical trials in low and middle income countries. BMC Public Health 11, 811 (2011).
Jackson, D. B. & Sood, A. K. Personalized cancer medicine—advances and socio-economic challenges. Nat. Rev. Clin. Oncol. 8, 735–741 (2011).
US National Library of Medicine. ClinicalTrials.gov, [online] (2011).
Mutch, D. G. et al. Randomized phase III trial of gemcitabine compared with pegylated liposomal doxorubicin in patients with platinum-resistant ovarian cancer. J. Clin. Oncol. 25, 2811–2818 (2007).
Brewer, C. A., Blessing, J. A., Nagourney, R. A., Morgan, M. & Hanjani, P. Cisplatin plus gemcitabine in platinum-refractory ovarian or primary peritoneal cancer: a phase II study of the Gynecologic Oncology Group. Gynecol. Oncol. 103, 446–450 (2006).
Miller, D. S. et al. Phase II evaluation of pemetrexed in the treatment of recurrent or persistent platinum-resistant ovarian or primary peritoneal carcinoma: a study of the Gynecologic Oncology Group. J. Clin. Oncol. 27, 2686–2691 (2009).
Rose, P. G., Blessing, J. A., Mayer, A. R. & Homesley, H. D. Prolonged oral etoposide as second-line therapy for platinum-resistant and platinum-sensitive ovarian carcinoma: a Gynecologic Oncology Group study. J. Clin. Oncol. 16, 405–410 (1998).
Markman, M. et al. Phase 2 trial of chronic low-dose oral etoposide as salvage therapy of platinum-refractory ovarian cancer. J. Cancer Res. Clin. Oncol. 119, 55–57 (1992).
Coleman, R. L. et al. A phase II evaluation of nanoparticle, albumin-bound (nab) paclitaxel in the treatment of recurrent or persistent platinum-resistant ovarian, fallopian tube, or primary peritoneal cancer: a Gynecologic Oncology Group study. Gynecol. Oncol. 122, 111–115 (2011).
Parmar, M. K. et al. Paclitaxel plus platinum-based chemotherapy versus conventional platinum-based chemotherapy in women with relapsed ovarian cancer: the ICON4/AGO-OVAR-2.2 trial. Lancet 361, 2099–2106 (2003).
Pfisterer, J. et al. Gemcitabine plus carboplatin compared with carboplatin in patients with platinum-sensitive recurrent ovarian cancer: an intergroup trial of the AGO-OVAR, the NCIC CTG, and the EORTC GCG. J. Clin. Oncol. 24, 4699–4707 (2006).
Pujade-Lauraine, E. et al. Pegylated liposomal doxorubicin and carboplatin compared with paclitaxel and carboplatin for patients with platinum-sensitive ovarian cancer in late relapse. J. Clin. Oncol. 28, 3323–3329 (2010).
Aghajanian, C. et al. OCEANS: a randomized, double-blind, placebo-controlled phase III trial of chemotherapy with or without bevacizumab in patients with platinum-sensitive recurrent epithelial ovarian, primary peritoneal, or fallopian tube cancer. J. Clin. Oncol. 30, 2039–2045 (2012).
Acknowledgements
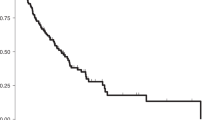
Portions of this work were supported by the Cancer Prevention & Research Institute of Texas (CPRIT,RP120214), NIH (P50 CA083639, P50 CA098258), Ovarian Cancer Research Fund Inc., The Marcus Foundation, and The Ann Rife Cox Chair in Gynecology (R. L. Coleman); NIH (CA109298, P50 CA083639, P50 CA098258, CA128797, RC2GM092599, U54 CA151668), the Ovarian Cancer Research Fund, Inc. (Program Project Development Grant), the DOD (OC073399, W81XWH-10-1-0158, BC085265), the RGK Foundation, the Gilder Foundation, the estate of C. G. Johnson Jr, the Marcus Foundation, the Blanton-Davis Ovarian Cancer Research Program, the Betty Anne Asche Murray Distinguished Professorship (A. K. Sood). The authors thank Robert Bristow for the image used in Figure 1.
Author information
Authors and Affiliations
Contributions
All the authors researched data for the article, made a substantial contribution to discussion of the content, wrote the article and edited it prior to submission.
Corresponding author
Ethics declarations
Competing interests
R. L. Coleman receives research funding from Amgen, AstraZeneca, Esperance Pharmaceuticals, Genentech/Roche, Merck, Millennium and Novartis. He on the Scientific Advisory Board of Abbott, BioMarin Pharmaceutical, Boehringer-Ingelheim, Bristol-Myers Squibb, Clovis Pharmaceuticals, GlaxoSmithKline, Johnson & Johnson, Morphotek/Easai and Nektar. B. J. Monk receives research funding from Novartis, Amgen, Genentech and Lilly; and is on the Speaker's Bureau of Roche/Genentech and Johnson & Johnson. He is also on the Scientific Advisory Board of Astellas, Array, Boehringer-Ingelheim, GlaxoSmithKline, Merck, Qiagen and Roche/Genentech. T. J. Herzog receives research funding from Baye and is on the Scientific Advisory Board of Genentech/Roche, GlaxoSmithKline and Johnson & Johnson. A. K. Sood declares no competing interests.
Rights and permissions
About this article
Cite this article
Coleman, R., Monk, B., Sood, A. et al. Latest research and treatment of advanced-stage epithelial ovarian cancer. Nat Rev Clin Oncol 10, 211–224 (2013). https://doi.org/10.1038/nrclinonc.2013.5
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrclinonc.2013.5
This article is cited by
-
Autophagy modulating therapeutics inhibit ovarian cancer colony generation by polyploid giant cancer cells (PGCCs)
BMC Cancer (2022)
-
The efficacy and safety of angiogenesis inhibitors for recurrent ovarian cancer: a meta‑analysis
Journal of Ovarian Research (2022)
-
Human epidermal growth factor receptor 2 (HER2)-specific chimeric antigen receptor (CAR) for tumor immunotherapy; recent progress
Stem Cell Research & Therapy (2022)
-
Gene polymorphisms of interleukin 10 (− 819 C/T and − 1082 G/A) in women with ovarian cancer
Beni-Suef University Journal of Basic and Applied Sciences (2022)
-
Targeting purine metabolism in ovarian cancer
Journal of Ovarian Research (2022)