Key Points
-
Patients with heart failure (HF) are characterized by relevant problems during sleep, including short sleep time, low sleep quality, and sleep-disordered breathing
-
Approximately 33% of patients with HF have insomnia, potentially related to HF features, adverse effects of medications, or to conditions that often accompany chronic diseases such as mood disorders and psychological stress
-
ACC/AHA guidelines have identified sleep deprivation and poor sleep quality as barriers to self-care and treatment adherence in patients with HF
-
Sleep-disordered breathing is highly prevalent in patients with HF; both central and obstructive sleep apnoeas are frequently observed in these patients, and were shown to have an important added prognostic value
-
Continuous positive airway pressure has a beneficial effect on left ventricular ejection fraction and is currently the best treatment option for obstructive sleep apnoeas in patients with HF
-
At present, no consensus exists on whether central sleep apnoeas should be treated and what the optimal therapy in HF might be
Abstract
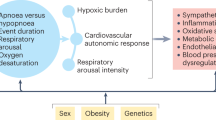
Awareness of the importance of sleep-related disorders in patients with cardiovascular diseases is growing. In particular, sleep-disordered breathing, short sleep time, and low sleep quality are frequently reported by patients with heart failure (HF). Sleep-disordered breathing, which includes obstructive sleep apnoea (OSA) and central sleep apnoea (CSA), is common in patients with HF and has been suggested to increase the morbidity and mortality in these patients. Both OSA and CSA are associated with increased sympathetic activation, vagal withdrawal, altered haemodynamic loading conditions, and hypoxaemia. Moreover, OSA is strongly associated with arterial hypertension, the most common risk factor for cardiac hypertrophy and failure. Intrathoracic pressure changes are also associated with OSA, contributing to haemodynamic alterations and potentially affecting overexpression of genes involved in ventricular remodelling. HF treatment can decrease the severity of both OSA and CSA. Indeed, furosemide and spironolactone administration, exercise training, cardiac resynchronization therapy, and eventually heart transplantation have shown a positive effect on OSA and CSA in patients with HF. At present, whether CSA should be treated and, if so, which is the optimal therapy is still debated. By contrast, more evidence is available on the beneficial effects of OSA treatment in patients with HF.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Desai, A. S. & Stevenson, L. W. Rehospitalization for heart failure: predict or prevent? Circulation 126, 501–506 (2012).
Hayes, D. Jr., Anstead, M. I., Ho, J. & Phillips, B. A. Insomnia and chronic heart failure. Heart Fail. Rev. 14, 171–182 (2009).
Jimenez, J. A., Greenberg, B. H. & Mills, P. J. Effects of heart failure and its pharmacological management on sleep. Drug Discov. Today Dis. Models 8, 161–166 (2011).
Redeker, N. S. et al. Nocturia, sleep and daytime function in stable heart failure. J. Card. Fail. 18, 569–575 (2012).
Luyster, F. S., Buysse, D. J. & Strollo, P. J. Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J. Clin. Sleep Med. 6, 196–204 (2010).
Lesman-Leegte, I. et al. Quality of life and depressive symptoms in the elderly: a comparison between patients with heart failure and age- and gender-matched community controls. J. Card. Fail. 15, 17–23 (2009).
Mills, P. J. et al. Sleep and health-related quality of life in heart failure. Congest. Heart Fail. 15, 228–233 (2009).
Riegel, B. et al. Modifiable factors associated with sleep dysfunction in adults with heart failure. Eur. J. Cardiovasc. Nurs. 11, 402–409 (2012).
Riegel, B. et al. State of the science: promoting self-care in persons with heart failure: a scientific statement from the American Heart Association. Circulation 120, 1141–1163 (2009).
McMurray, J. J. et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 33, 1787–1847 (2012).
Cowie, M. R. et al. Adaptive servo-ventilation for central sleep apnea in systolic heart failure. N. Engl. J. Med. 373, 1095–1105 (2015).
US National Library of Science. ClinicalTrials.gov [online], https://clinicaltrials.gov/ct2/show/NCT01128816 (2015).
US National Library of Science. ClinicalTrials.gov [online], https://clinicaltrials.gov/ct2/show/NCT01953874 (2016).
Redline, S. et al. The scoring of respiratory events in sleep: reliability and validity. J. Clin. Sleep Med. 3, 169–200 (2007).
Tkacova, R., Niroumand, M., Lorenzi-Filho, G. & Bradley, T. D. Overnight shift from obstructive to central apneas in patients with heart failure: role of PCO2 and circulatory delay. Circulation 103, 238–243 (2001).
Alex, C. G., Onal, E. & Lopata, M. Upper airway occlusion during sleep in patients with Cheyne–Stokes respiration. Am. Rev. Respir. Dis. 133, 42–45 (1986).
Shepard, J. W. et al. Effects of changes in central venous pressure on upper airway size in patients with obstructive sleep apnea. Am. J. Respir. Crit. Care Med. 153, 250–254 (1996).
Chiu, K. L. et al. Fluid shift by lower body positive pressure increases pharyngeal resistance in healthy subjects. Am. J. Respir. Crit. Care Med. 174, 1378–1383 (2006).
Yumino, D. & Bradley, T. D. Central sleep apnea and Cheyne–Stokes respiration. Proc. Am. Thorac. Soc. 5, 226–236 (2008).
Lévy, P. et al. Obstructive sleep apnoea syndrome. Nat. Rev. Dis. Primers 1, 15015 (2015).
Peppard, P. E. et al. Increased prevalence of sleep-disordered breathing in adults. Am. J. Epidemiol. 177, 1006–1014 (2013).
Eckert, D. J., Jordan, A. S., Merchia, P. & Malhotra, A. Central sleep apnea: pathophysiology and treatment. Chest 131, 595–607 (2007).
Mason, R. J. et al. Murray and Nadel's Textbook of Respiratory Medicine (Elsevier Saunders, 2010).
Arzt, M. et al. Prevalence and predictors of sleep-disordered breathing in patients with stable chronic heart failure: the SchlaHF Registry. JACC Heart Fail. 4, 116–125 (2016).
Bitter, T. et al. Sleep-disordered breathing in heart failure with normal left ventricular ejection fraction. Eur. J. Heart Fail. 11, 602–608 (2009).
Javaheri, S. et al. Sleep apnea in 81 ambulatory male patients with stable heart failure. Types and their prevalences, consequences, and presentations. Circulation 97, 2154–2159 (1998).
Sin, D. D. et al. Risk factors for central and obstructive sleep apnea in 450 men and women with congestive heart failure. Am. J. Respir. Crit. Care Med. 160, 1101–1106 (1999).
Schulz, R. et al. Sleep apnoea in heart failure. Eur. Respir. J. 29, 1201–1205 (2007).
Shahar, E. et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am. J. Respir. Crit. Care Med. 163, 19–25 (2001).
Tremel, F. et al. High prevalence and persistence of sleep apnoea in patients referred for acute left ventricular failure and medically treated over 2 months. Eur. Heart J. 20, 1201–1209 (1999).
Solin, P. et al. Influence of pulmonary capillary wedge pressure on central apnea in heart failure. Circulation 99, 1574–1579 (1999).
Oldenburg, O. et al. Sleep-disordered breathing in patients with symptomatic heart failure: a contemporary study of prevalence in and characteristics of 700 patients. Eur. J. Heart Fail. 9, 251–257 (2007).
Lofaso, F., Verschueren, P., Rande, J. L., Harf, A. & Goldenberg, F. Prevalence of sleep-disordered breathing in patients on a heart transplant waiting list. Chest 106, 1689–1694 (1994).
Grimm, W. et al. Severe central sleep apnea is associated with atrial fibrillation in patients with left ventricular systolic dysfunction. Pacing Clin. Electrophysiol. 38, 706–712 (2015).
O'Meara, E. et al. Sex differences in clinical characteristics and prognosis in a broad spectrum of patients with heart failure: results of the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity (CHARM) program. Circulation 115, 3111–3120 (2007).
Lombardi, C. et al. High-altitude hypoxia and periodic breathing during sleep: gender-related differences. J. Sleep Res. 22, 322–330 (2013).
Caravita, S. et al. Sex and acetazolamide effects on chemoreflex and periodic breathing during sleep at altitude. Chest 147, 120–131 (2015).
Malhotra, A. & White, D. P. Obstructive sleep apnoea. Lancet 360, 237–245 (2002).
Efken, C., Bitter, T., Prib, N., Horstkotte, D. & Oldenburg, O. Obstructive sleep apnoea: longer respiratory event lengths in patients with heart failure. Eur. Respir. J. 41, 1340–1346 (2013).
Bradley, T. D. & Floras, J. S. Sleep apnea and heart failure: part I: obstructive sleep apnea. Circulation 107, 1671–1678 (2003).
Brinker, J. A. et al. Leftward septal displacement during right ventricular loading in man. Circulation 61, 626–633 (1980).
Mebazaa, A., Gheorghiade, M., Zannad, F. & Parrillo, J. E. Acute Heart Failure (Springer-Verlag, 2008).
Dimsdale, J. E., Coy, T., Ziegler, M. G., Ancoli-Israel, S. & Clausen, J. The effect of sleep apnea on plasma and urinary catecholamines. Sleep 18, 377–381 (1995).
Kato, M. et al. Impairment of endothelium-dependent vasodilation of resistance vessels in patients with obstructive sleep apnea. Circulation 102, 2607–2610 (2000).
Parati, G. et al. Position paper on the management of patients with obstructive sleep apnea and hypertension: joint recommendations by the European Society of Hypertension, by the European Respiratory Society and by the members of European COST (COoperation in Scientific and Technological research) ACTION B26 on obstructive sleep apnea. J. Hypertens. 30, 633–646 (2012).
Yokoe, T. et al. Elevated levels of C-reactive protein and interleukin-6 in patients with obstructive sleep apnea syndrome are decreased by nasal continuous positive airway pressure. Circulation 107, 1129–1134 (2003).
Skatrud, J. B. & Dempsey, J. A. Interaction of sleep state and chemical stimuli in sustaining rhythmic ventilation. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 55, 813–822 (1983).
Zhou, X. S., Shahabuddin, S., Zahn, B. R., Babcock, M. A. & Badr, M. S. Effect of gender on the development of hypocapnic apnea/hypopnea during NREM sleep. J. Appl. Physiol. (1985) 89, 192–199 (2000).
Eckert, D. J., Malhotra, A. & Jordan, A. S. Mechanisms of apnea. Prog. Cardiovasc. Dis. 51, 313–323 (2009).
Khoo, M. C., Gottschalk, A. & Pack, A. I. Sleep-induced periodic breathing and apnea: a theoretical study. J. Appl. Physiol. (1985) 70, 2014–2024 (1991).
Bradley, T. D. & Phillipson, E. A. Central sleep apnea. Clin. Chest Med. 13, 493–505 (1992).
Dempsey, J. A. et al. Role of central/peripheral chemoreceptors and their interdependence in the pathophysiology of sleep apnea. Adv. Exp. Med. Biol. 758, 343–349 (2012).
Lorenzi-Filho, G., Azevedo, E. R., Parker, J. D. & Bradley, T. D. Relationship of carbon dioxide tension in arterial blood to pulmonary wedge pressure in heart failure. Eur. Respir. J. 19, 37–40 (2002).
Kohnlein, T., Welte, T., Tan, L. B. & Elliott, M. W. Central sleep apnoea syndrome in patients with chronic heart disease: a critical review of the current literature. Thorax 57, 547–554 (2002).
Szollosi, I., Roebuck, T., Thompson, B. & Naughton, M. T. Lateral sleeping position reduces severity of central sleep apnea/Cheyne–Stokes respiration. Sleep 29, 1045–1051 (2006).
Arzt, M. et al. Enhanced ventilatory response to exercise in patients with chronic heart failure and central sleep apnea. Circulation 107, 1998–2003 (2003).
Kasai, T., Floras, J. S. & Bradley, T. D. Sleep apnea and cardiovascular disease: a bidirectional relationship. Circulation 126, 1495–1510 (2012).
Naughton, M. T. et al. Effects of nasal CPAP on sympathetic activity in patients with heart failure and central sleep apnea. Am. J. Respir. Crit. Care Med. 152, 473–479 (1995).
Bitter, T. et al. Cheyne–Stokes respiration and obstructive sleep apnoea are independent risk factors for malignant ventricular arrhythmias requiring appropriate cardioverter-defibrillator therapies in patients with congestive heart failure. Eur. Heart J. 32, 61–74 (2011).
Parker, J. D. et al. Acute and chronic effects of airway obstruction on canine left ventricular performance. Am. J. Respir. Crit. Care Med. 160, 1888–1896 (1999).
Morgan, B. J., Denahan, T. & Ebert, T. J. Neurocirculatory consequences of negative intrathoracic pressure versus asphyxia during voluntary apnea. J. Appl. Physiol. (1985) 74, 2969–2975 (1993).
Somers, V. K., Mark, A. L., Zavala, D. C. & Abboud, F. M. Contrasting effects of hypoxia and hypercapnia on ventilation and sympathetic activity in humans. J. Appl. Physiol. (1985) 67, 2101–2106 (1989).
Horner, R. L., Brooks, D., Kozar, L. F., Tse, S. & Phillipson, E. A. Immediate effects of arousal from sleep on cardiac autonomic outflow in the absence of breathing in dogs. J. Appl. Physiol. (1985) 79, 151–162 (1995).
Coccagna, G., Mantovani, M., Brignani, F., Parchi, C. & Lugaresi, E. Continuous recording of the pulmonary and systemic arterial pressure during sleep in syndromes of hypersomnia with periodic breathing. Bull. Physiopathol. Respir. (Nancy) 8, 1159–1172 (1972).
Peppard, P. E., Young, T., Palta, M. & Skatrud, J. Prospective study of the association between sleep-disordered breathing and hypertension. N. Engl. J. Med. 342, 1378–1384 (2000).
Xie, A., Skatrud, J. B., Puleo, D. S. & Morgan, B. J. Exposure to hypoxia produces long-lasting sympathetic activation in humans. J. Appl. Physiol. (1985) 91, 1555–1562 (2001).
Arabi, Y. et al. Daytime blood pressure elevation after nocturnal hypoxia. J. Appl. Physiol. (1985) 87, 689–698 (1999).
Eisenberg, E., Zimlichman, R. & Lavie, P. Plasma norepinephrine levels in patients with sleep apnea syndrome. N. Engl. J. Med. 322, 932–933 (1990).
Thomas, J. A. & Marks, B. H. Plasma norepinephrine in congestive heart failure. Am. J. Cardiol. 41, 233–243 (1978).
Spaak, J. et al. Muscle sympathetic nerve activity during wakefulness in heart failure patients with and without sleep apnea. Hypertension 46, 1327–1332 (2005).
Szollosi, I., Krum, H., Kaye, D. & Naughton, M. T. Sleep apnea in heart failure increases heart rate variability and sympathetic dominance. Sleep 30, 1509–1514 (2007).
Parati, G., Saul, J. P., Di Rienzo, M. & Mancia, G. Spectral analysis of blood pressure and heart rate variability in evaluating cardiovascular regulation. A critical appraisal. Hypertension 25, 1276–1286 (1995).
Noda, A. et al. Continuous positive airway pressure improves daytime baroreflex sensitivity and nitric oxide production in patients with moderate to severe obstructive sleep apnea syndrome. Hypertens. Res. 30, 669–676 (2007).
Parati, G. et al. Autonomic cardiac regulation in obstructive sleep apnea syndrome: evidence from spontaneous baroreflex analysis during sleep. J. Hypertens. 15, 1621–1626 (1997).
Lombardi, C. et al. Daytime sleepiness and neural cardiac modulation in sleep-related breathing disorders. J. Sleep Res. 17, 263–270 (2008).
Parati, G., Di Rienzo, M. & Mancia, G. How to measure baroreflex sensitivity: from the cardiovascular laboratory to daily life. J. Hypertens. 18, 7–19 (2000).
Fletcher, E. C. et al. Pulmonary edema develops after recurrent obstructive apneas. Am. J. Respir. Crit. Care Med. 160, 1688–1696 (1999).
Sin, D. D. et al. Relationship of systolic BP to obstructive sleep apnea in patients with heart failure. Chest 123, 1536–1543 (2003).
Carlson, J. T., Rangemark, C. & Hedner, J. A. Attenuated endothelium-dependent vascular relaxation in patients with sleep apnoea. J. Hypertens. 14, 577–584 (1996).
Dyugovskaya, L., Lavie, P. & Lavie, L. Increased adhesion molecules expression and production of reactive oxygen species in leukocytes of sleep apnea patients. Am. J. Respir. Crit. Care Med. 165, 934–939 (2002).
Schulz, R. et al. Enhanced release of superoxide from polymorphonuclear neutrophils in obstructive sleep apnea. Impact of continuous positive airway pressure therapy. Am. J. Respir. Crit. Care Med. 162, 566–570 (2000).
Shamsuzzaman, A. S. et al. Elevated C-reactive protein in patients with obstructive sleep apnea. Circulation 105, 2462–2464 (2002).
Rifai, N. & Ridker, P. M. Inflammatory markers and coronary heart disease. Curr. Opin. Lipidol. 13, 383–389 (2002).
Godoy, J., Mellado, P., Tapia, J. & Santin, J. Obstructive sleep apnea as an independent stroke risk factor: possible mechanisms. Curr. Mol. Med. 9, 203–209 (2009).
Bradley, T. D. & Floras, J. S. Obstructive sleep apnoea and its cardiovascular consequences. Lancet 373, 82–93 (2009).
Tkacova, R., Rankin, F., Fitzgerald, F. S., Floras, J. S. & Bradley, T. D. Effects of continuous positive airway pressure on obstructive sleep apnea and left ventricular afterload in patients with heart failure. Circulation 98, 2269–2275 (1998).
Floras, J. S. Clinical aspects of sympathetic activation and parasympathetic withdrawal in heart failure. J. Am. Coll. Cardiol. 22, 72a–84a (1993).
La Rovere, M. T. et al. Baroreflex sensitivity and heart rate variability in the identification of patients at risk for life-threatening arrhythmias: implications for clinical trials. Circulation 103, 2072–2077 (2001).
Parati, G., Lombardi, C. & Narkiewicz, K. Sleep apnea: epidemiology, pathophysiology, and relation to cardiovascular risk. Am. J. Physiol. Regul. Integr. Comp. Physiol. 293, R1671–R1683 (2007).
Franklin, K. A., Nilsson, J. B., Sahlin, C. & Naslund, U. Sleep apnoea and nocturnal angina. Lancet 345, 1085–1087 (1995).
Hla, K. M. et al. Coronary heart disease incidence in sleep disordered breathing: the Wisconsin Sleep Cohort Study. Sleep 38, 677–684 (2015).
Nadeem, R. et al. Serum inflammatory markers in obstructive sleep apnea: a meta-analysis. J. Clin. Sleep Med. 9, 1003–1012 (2013).
El-Solh, A. A. et al. Adhesion molecules in patients with coronary artery disease and moderate-to-severe obstructive sleep apnea. Chest 121, 1541–1547 (2002).
Ip, M. S. et al. Circulating nitric oxide is suppressed in obstructive sleep apnea and is reversed by nasal continuous positive airway pressure. Am. J. Respir. Crit. Care Med. 162, 2166–2171 (2000).
Hedner, J. A., Wilcox, I., Laks, L., Grunstein, R. R. & Sullivan, C. E. A specific and potent pressor effect of hypoxia in patients with sleep apnea. Am. Rev. Respir. Dis. 146, 1240–1245 (1992).
Jelic, S. et al. Vascular inflammation in obesity and sleep apnea. Circulation 121, 1014–1021 (2010).
Jelic, S. et al. Endothelial repair capacity and apoptosis are inversely related in obstructive sleep apnea. Vasc. Health Risk Manag. 5, 909–920 (2009).
Emin, M. et al. Increased internalization of complement inhibitor CD59 may contribute to endothelial inflammation in obstructive sleep apnea. Sci. Transl. Med. 8, 320ra1 (2016).
Cohn, J. N., Ferrari, R. & Sharpe, N. Cardiac remodeling — concepts and clinical implications: a consensus paper from an international forum on cardiac remodeling. J. Am. Coll. Cardiol. 35, 569–582 (2000).
Bernardi, L. et al. Slow breathing increases arterial baroreflex sensitivity in patients with chronic heart failure. Circulation 105, 143–145 (2002).
Parati, G. et al. Recommendations for the management of patients with obstructive sleep apnoea and hypertension. Eur. Respir. J. 41, 523–538 (2013).
Malone, S. et al. Obstructive sleep apnoea in patients with dilated cardiomyopathy: effects of continuous positive airway pressure. Lancet 338, 1480–1484 (1991).
Bradley, T. D., Hall, M. J., Ando, S. & Floras, J. S. Hemodynamic effects of simulated obstructive apneas in humans with and without heart failure. Chest 119, 1827–1835 (2001).
Javaheri, S., Shukla, R., Zeigler, H. & Wexler, L. Central sleep apnea, right ventricular dysfunction, and low diastolic blood pressure are predictors of mortality in systolic heart failure. J. Am. Coll. Cardiol. 49, 2028–2034 (2007).
Lanfranchi, P. A. et al. Prognostic value of nocturnal Cheyne–Stokes respiration in chronic heart failure. Circulation 99, 1435–1440 (1999).
Sin, D. D., Logan, A. G., Fitzgerald, F. S., Liu, P. P. & Bradley, T. D. Effects of continuous positive airway pressure on cardiovascular outcomes in heart failure patients with and without Cheyne–Stokes respiration. Circulation 102, 61–66 (2000).
Franklin, K. A., Sandstrom, E., Johansson, G. & Balfors, E. M. Hemodynamics, cerebral circulation, and oxygen saturation in Cheyne–Stokes respiration. J. Appl. Physiol. (1985) 83, 1184–1191 (1997).
Trinder, J. et al. Pathophysiological interactions of ventilation, arousals, and blood pressure oscillations during Cheyne–Stokes respiration in patients with heart failure. Am. J. Respir. Crit. Care Med. 162, 808–813 (2000).
Javaheri, S. & Corbett, W. S. Association of low PaCO2 with central sleep apnea and ventricular arrhythmias in ambulatory patients with stable heart failure. Ann. Intern. Med. 128, 204–207 (1998).
Costanzo, M. R. et al. Mechanisms and clinical consequences of untreated central sleep apnea in heart failure. J. Am. Coll. Cardiol. 65, 72–84 (2015).
Pinna, G. D., Maestri, R., Mortara, A. & La Rovere, M. T. Cardiorespiratory interactions during periodic breathing in awake chronic heart failure patients. Am. J. Physiol. Heart Circ. Physiol. 278, H932–H941 (2000).
Leung, R. S. et al. Influence of Cheyne–Stokes respiration on cardiovascular oscillations in heart failure. Am. J. Respir. Crit. Care Med. 167, 1534–1539 (2003).
Brack, T., Jubran, A., Laghi, F. & Tobin, M. J. Fluctuations in end-expiratory lung volume during Cheyne–Stokes respiration. Am. J. Respir. Crit. Care Med. 171, 1408–1413 (2005).
Lorenzi-Filho, G., Dajani, H. R., Leung, R. S., Floras, J. S. & Bradley, T. D. Entrainment of blood pressure and heart rate oscillations by periodic breathing. Am. J. Respir. Crit. Care Med. 159, 1147–1154 (1999).
Ponikowski, P. et al. Detection and significance of a discrete very low frequency rhythm in RR interval variability in chronic congestive heart failure. Am. J. Cardiol. 77, 1320–1326 (1996).
Guyenet, P. G., Koshiya, N., Huangfu, D., Verberne, A. J. & Riley, T. A. Central respiratory control of A5 and A6 pontine noradrenergic neurons. Am. J. Physiol. (1985) 264, R1035–R1044 (1993).
Brack, T. et al. Daytime Cheyne–Stokes respiration in ambulatory patients with severe congestive heart failure is associated with increased mortality. Chest 132, 1463–1471 (2007).
Corra, U. et al. Sleep and exertional periodic breathing in chronic heart failure: prognostic importance and interdependence. Circulation 113, 44–50 (2006).
Meguro, K., Adachi, H., Oshima, S., Taniguchi, K. & Nagai, R. Exercise tolerance, exercise hyperpnea and central chemosensitivity to carbon dioxide in sleep apnea syndrome in heart failure patients. Circ. J. 69, 695–699 (2005).
Ponikowski, P. et al. Chemoreceptor dependence of very low frequency rhythms in advanced chronic heart failure. Am. J. Physiol. 272, H438–H447 (1997).
Hanly, P. J. & Zuberi-Khokhar, N. S. Increased mortality associated with Cheyne–Stokes respiration in patients with congestive heart failure. Am. J. Respir. Crit. Care Med. 153, 272–276 (1996).
Naughton, M. T. Cheyne–Stokes respiration: friend or foe? Thorax 67, 357–360 (2012).
Roebuck, T. et al. Increased long-term mortality in heart failure due to sleep apnoea is not yet proven. Eur. Respir. J. 23, 735–740 (2004).
Mansfield, D. et al. Raised sympathetic nerve activity in heart failure and central sleep apnea is due to heart failure severity. Circulation 107, 1396–1400 (2003).
Yeh, G. Y. et al. Enhancement of sleep stability with Tai Chi exercise in chronic heart failure: preliminary findings using an ECG-based spectrogram method. Sleep Med. 9, 527–536 (2008).
Parthasarathy, S. et al. Persistent insomnia is associated with mortality risk. Am. J. Med. 128, 268–275.e2 (2015).
McEwen, B. S. Sleep deprivation as a neurobiologic and physiologic stressor: allostasis and allostatic load. Metabolism 55, S20–S23 (2006).
Arzt, M. et al. Sleepiness and sleep in patients with both systolic heart failure and obstructive sleep apnea. Arch. Intern. Med. 166, 1716–1722 (2006).
Grimm, W., Hildebrandt, O., Nell, C. & Koehler, U. Excessive daytime sleepiness and central sleep apnea in patients with stable heart failure. Int. J. Cardiol. 176, 1447–1448 (2014).
McKelvie, R. S. et al. The 2011 Canadian Cardiovascular Society heart failure management guidelines update: focus on sleep apnea, renal dysfunction, mechanical circulatory support, and palliative care. Can. J. Cardiol. 27, 319–338 (2011).
Mehra, R. & Redline, S. Arrhythmia risk associated with sleep disordered breathing in chronic heart failure. Curr. Heart Fail. Rep. 11, 88–97 (2014).
[No authors listed.] Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep 22, 667–689 (1999).
American Academy of Sleep Medicine. International Classification of Sleep Disorders (American Academy of Sleep Medicine, 2014).
Farre, R., Montserrat, J. M. & Navajas, D. Noninvasive monitoring of respiratory mechanics during sleep. Eur. Respir. J. 24, 1052–1060 (2004).
Janssens, J. P., Borel, J. C. & Pepin, J. L. Nocturnal monitoring of home non-invasive ventilation: contribution of simple tools such as pulse-oximetry, capnography, built-in ventilator software and autonomic markers of sleep fragmentation. Rev. Mal. Respir. 31, 107–118 (in French) (2014).
Pinna, G. D. et al. Can cardiorespiratory polygraphy replace portable polysomnography in the assessment of sleep-disordered breathing in heart failure patients? Sleep Breath. 18, 475–482 (2014).
Ward, N. R. et al. Utility of overnight pulse oximetry and heart rate variability analysis to screen for sleep-disordered breathing in chronic heart failure. Thorax 67, 1000–1005 (2012).
Defaye, P. et al. A pacemaker transthoracic impedance sensor with an advanced algorithm to identify severe sleep apnea: the DREAM European study. Heart Rhythm 11, 842–848 (2014).
Oldenburg, O. et al. Nocturnal hypoxaemia is associated with increased mortality in stable heart failure patients. Eur. Heart J. http://dx.doi.org/10.1093/eurheartj/ehv624 (2015).
Bucca, C. B. et al. Diuretics in obstructive sleep apnea with diastolic heart failure. Chest 132, 440–446 (2007).
Tkacova, R. et al. Continuous positive airway pressure improves nocturnal baroreflex sensitivity of patients with heart failure and obstructive sleep apnea. J. Hypertens. 18, 1257–1262 (2000).
Kauta, S. R., Keenan, B. T., Goldberg, L. & Schwab, R. J. Diagnosis and treatment of sleep disordered breathing in hospitalized cardiac patients: a reduction in 30-day hospital readmission rates. J. Clin. Sleep Med. 10, 1051–1059 (2014).
Kaneko, Y. et al. Cardiovascular effects of continuous positive airway pressure in patients with heart failure and obstructive sleep apnea. N. Engl. J. Med. 348, 1233–1241 (2003).
Mansfield, D. R. et al. Controlled trial of continuous positive airway pressure in obstructive sleep apnea and heart failure. Am. J. Respir. Crit. Care Med. 169, 361–366 (2004).
Sun, H., Shi, J., Li, M. & Chen, X. Impact of continuous positive airway pressure treatment on left ventricular ejection fraction in patients with obstructive sleep apnea: a meta-analysis of randomized controlled trials. PLoS ONE 8, e62298 (2013).
Wang, H. et al. Influence of obstructive sleep apnea on mortality in patients with heart failure. J. Am. Coll. Cardiol. 49, 1625–1631 (2007).
Kasai, T. et al. Prognosis of patients with heart failure and obstructive sleep apnea treated with continuous positive airway pressure. Chest 133, 690–696 (2008).
Somers, V. K. et al. Sleep apnea and cardiovascular disease: an American Heart Association/american College Of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council On Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation 118, 1080–1111 (2008).
Khayat, R. N. et al. Cardiac effects of continuous and bilevel positive airway pressure for patients with heart failure and obstructive sleep apnea: a pilot study. Chest 134, 1162–1168 (2008).
Sharples, L. et al. Clinical effectiveness and cost-effectiveness results from the randomised controlled Trial of Oral Mandibular Advancement Devices for Obstructive sleep apnoea-hypopnoea (TOMADO) and long-term economic analysis of oral devices and continuous positive airway pressure. Health Technol. Assess. 18, 1–296 (2014).
McDaid, C. et al. Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea-hypopnoea syndrome: a systematic review and economic analysis. Health Technol. Assess. 13, 4 (2009).
Schwartz, A. R. Hypoglossal nerve stimulation — optimizing its therapeutic potential in obstructive sleep apnea. J. Neurol. Sci. 346, 1–3 (2014).
Lin, H. C., Friedman, M., Chang, H. W. & Gurpinar, B. The efficacy of multilevel surgery of the upper airway in adults with obstructive sleep apnea/hypopnea syndrome. Laryngoscope 118, 902–908 (2008).
Hudgel, D. W. & Thanakitcharu, S. Pharmacologic treatment of sleep-disordered breathing. Am. J. Respir. Crit. Care Med. 158, 691–699 (1998).
De Backer, W. A. Central sleep apnoea, pathogenesis and treatment: an overview and perspective. Eur. Respir. J. 8, 1372–1383 (1995).
Javaheri, S. et al. Effect of theophylline on sleep-disordered breathing in heart failure. N. Engl. J. Med. 335, 562–567 (1996).
Bradley, T. D. & Floras, J. S. Sleep apnea and heart failure: part II: central sleep apnea. Circulation 107, 1822–1826 (2003).
Walsh, J. T. et al. Effects of captopril and oxygen on sleep apnoea in patients with mild to moderate congestive cardiac failure. Br. Heart J. 73, 237–241 (1995).
Baylor, P., Tayloe, D., Owen, D. & Sanders, C. Cardiac failure presenting as sleep apnea: elimination of apnea following medical management of cardiac failure. Chest 94, 1298–1300 (1988).
Dark, D. S. et al. Breathing pattern abnormalities and arterial oxygen desaturation during sleep in the congestive heart failure syndrome: improvement following medical therapy. Chest 91, 833–836 (1987).
Giannoni, A. et al. Combined increased chemosensitivity to hypoxia and hypercapnia as a prognosticator in heart failure. J. Am. Coll. Cardiol. 53, 1975–1980 (2009).
Hermand, E., Lhuissier, F. J., Larribaut, J., Pichon, A. & Richalet, J. P. Ventilatory oscillations at exercise: effects of hyperoxia, hypercapnia, and acetazolamide. Physiol. Rep. 3, e12446 (2015).
Hanly, P. J. et al. The effect of oxygen on respiration and sleep in patients with congestive heart failure. Ann. Intern. Med. 111, 777–782 (1989).
Staniforth, A. D., Kinnear, W. J., Starling, R., Hetmanski, D. J. & Cowley, A. J. Effect of oxygen on sleep quality, cognitive function and sympathetic activity in patients with chronic heart failure and Cheyne–Stokes respiration. Eur. Heart J. 19, 922–928 (1998).
Teschler, H., Dohring, J., Wang, Y. M. & Berthon-Jones, M. Adaptive pressure support servo-ventilation: a novel treatment for Cheyne–Stokes respiration in heart failure. Am. J. Respir. Crit. Care Med. 164, 614–619 (2001).
Stub, D. et al. Air versus oxygen in ST-segment-elevation myocardial infarction. Circulation 131, 2143–2150 (2015).
Chua, T. P. et al. Clinical characteristics of chronic heart failure patients with an augmented peripheral chemoreflex. Eur. Heart J. 18, 480–486 (1997).
Yamada, K. et al. Role of central sympathoexcitation in enhanced hypercapnic chemosensitivity in patients with heart failure. Am. Heart J. 148, 964–970 (2004).
Tomita, T. et al. Attenuation of hypercapnic carbon dioxide chemosensitivity after postinfarction exercise training: possible contribution to the improvement in exercise hyperventilation. Heart 89, 404–410 (2003).
Naughton, M. T., Liu, P. P., Bernard, D. C., Goldstein, R. S. & Bradley, T. D. Treatment of congestive heart failure and Cheyne–Stokes respiration during sleep by continuous positive airway pressure. Am. J. Respir. Crit. Care Med. 151, 92–97 (1995).
Naughton, M. T., Benard, D. C., Rutherford, R. & Bradley, T. D. Effect of continuous positive airway pressure on central sleep apnea and nocturnal PCO2 in heart failure. Am. J. Respir. Crit. Care Med. 150, 1598–1604 (1994).
Badr, S. Central sleep apnea in patients with congestive heart failure. Heart Fail. Rev. 14, 135–141 (2009).
Javaheri, S. Effects of continuous positive airway pressure on sleep apnea and ventricular irritability in patients with heart failure. Circulation 101, 392–397 (2000).
Tkacova, R., Liu, P. P., Naughton, M. T. & Bradley, T. D. Effect of continuous positive airway pressure on mitral regurgitant fraction and atrial natriuretic peptide in patients with heart failure. J. Am. Coll. Cardiol. 30, 739–745 (1997).
Bradley, T. D. et al. Continuous positive airway pressure for central sleep apnea and heart failure. N. Engl. J. Med. 353, 2025–2033 (2005).
Arzt, M. et al. Suppression of central sleep apnea by continuous positive airway pressure and transplant-free survival in heart failure: a post hoc analysis of the Canadian Continuous Positive Airway Pressure for Patients with Central Sleep Apnea and Heart Failure Trial (CANPAP). Circulation 115, 3173–3180 (2007).
Meza, S., Mendez, M., Ostrowski, M. & Younes, M. Susceptibility to periodic breathing with assisted ventilation during sleep in normal subjects. J. Appl. Physiol. (1985) 85, 1929–1940 (1998).
Arzt, M. et al. Effects of dynamic bilevel positive airway pressure support on central sleep apnea in men with heart failure. Chest 134, 61–66 (2008).
Fietze, I. et al. Bi-level positive pressure ventilation and adaptive servo ventilation in patients with heart failure and Cheyne–Stokes respiration. Sleep Med. 9, 652–659 (2008).
Brown, L. K. & Javaheri, S. Adaptive servo-ventilation for the treatment of central sleep apnea in congestive heart failure: what have we learned? Curr. Opin. Pulm. Med. 20, 550–557 (2014).
Oldenburg, O., Spiesshofer, J., Fox, H., Prib, N. & Horstkotte, D. Performance of conventional and enhanced adaptive servoventilation (ASV) in heart failure patients with central sleep apnea who have adapted to conventional ASV. Sleep Breath. 19, 795–800 (2015).
Aurora, R. N. et al. The treatment of central sleep apnea syndromes in adults: practice parameters with an evidence-based literature review and meta-analyses. Sleep 35, 17–40 (2012).
Ohmura, T. et al. Impact of predischarge nocturnal pulse oximetry (sleep-disordered breathing) on postdischarge clinical outcomes in hospitalized patients with left ventricular systolic dysfunction after acute decompensated heart failure. Am. J. Cardiol. 113, 697–700 (2014).
Padeletti, M., Green, P., Mooney, A. M., Basner, R. C. & Mancini, D. M. Sleep disordered breathing in patients with acutely decompensated heart failure. Sleep Med. 10, 353–360 (2009).
Garrigue, S., Bordier, P., Barold, S. S. & Clementy, J. Sleep apnea: a new indication for cardiac pacing? Pacing Clin. Electrophysiol. 27, 204–211 (2004).
Garrigue, S. et al. Benefit of atrial pacing in sleep apnea syndrome. N. Engl. J. Med. 346, 404–412 (2002).
Ueno, L. M. et al. Effects of exercise training in patients with chronic heart failure and sleep apnea. Sleep 32, 637–647 (2009).
Yamamoto, U. et al. Six-month aerobic exercise training ameliorates central sleep apnea in patients with chronic heart failure. J. Card. Fail. 13, 825–829 (2007).
Lamba, J. et al. Cardiac resynchronization therapy for the treatment of sleep apnoea: a meta-analysis. Europace 13, 1174–1179 (2011).
US National Library of Science. ClinicalTrials.gov [online], https://clinicaltrials.gov/ct2/show/NCT02577445 (2015).
Abraham, W. T. et al. Phrenic nerve stimulation for the treatment of central sleep apnea. JACC Heart Fail. 3, 360–369 (2015).
Hetzenecker, A. et al. Adaptive servo-ventilation therapy of central sleep apnoea and its effect on sleep quality. Clin. Res. Cardiol. 105, 189–195 (2016).
Javaheri, S. Sleep dysfunction in heart failure. Curr. Treat. Options Neurol. 10, 323–335 (2008).
Botelho, R. V., Bittencourt, L. R., Rotta, J. M. & Tufik, S. A prospective controlled study of sleep respiratory events in patients with craniovertebral junction malformation. J. Neurosurg. 99, 1004–1009 (2003).
Chervin, R. D. Sleepiness, fatigue, tiredness, and lack of energy in obstructive sleep apnea. Chest 118, 372–379 (2000).
Myers, K. A., Mrkobrada, M. & Simel, D. L. Does this patient have obstructive sleep apnea?: The Rational Clinical Examination systematic review. JAMA 310, 731–741 (2013).
Bitter, T., Fox, H., Gaddam, S., Horstkotte, D. & Oldenburg, O. Sleep-disordered breathing and cardiac arrhythmias. Can. J. Cardiol. 31, 928–934 (2015).
Young, T. et al. The occurrence of sleep-disordered breathing among middle-aged adults. N. Engl. J. Med. 328, 1230–1235 (1993).
Epstein, L. J. et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J. Clin. Sleep Med. 5, 263–276 (2009).
White, L. H. & Bradley, T. D. Role of nocturnal rostral fluid shift in the pathogenesis of obstructive and central sleep apnoea. J. Physiol. 591, 1179–1193 (2013).
Nelson, K. A. & Trupp, R. J. Sleep and heart failure. Crit. Care Nurs. Clin. North Am. 27, 511–522 (2015).
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed equally to researching data, discussions of content, writing the article, and to reviewing and editing the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Parati, G., Lombardi, C., Castagna, F. et al. Heart failure and sleep disorders. Nat Rev Cardiol 13, 389–403 (2016). https://doi.org/10.1038/nrcardio.2016.71
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2016.71
This article is cited by
-
The effect of using a sports application on the quality of sleep in patients with heart failure: a randomized clinical trial study
BMC Sports Science, Medicine and Rehabilitation (2024)
-
Interaction effects between sleep disorders and depression on heart failure
BMC Cardiovascular Disorders (2023)
-
Eating habit of adding salt to foods and incident sleep apnea: a prospective cohort study
Respiratory Research (2023)
-
Effects of continuous positive airway pressure therapy on left ventricular performance in patients with severe obstructive sleep apnea
Scientific Reports (2023)
-
Screening obstructive sleep apnea patients via deep learning of knowledge distillation in the lateral cephalogram
Scientific Reports (2023)