Key Points
-
Quality-of-life (QOL) measurement grew out of work by social scientists and health-services researchers in the 1960s and 1970s to define the value of health-care spending
-
Measuring QOL has some similarity with other forms of clinical testing but, because the objects of measurement are subjective experiences, psychometric tools and theory are used to guide the process
-
The goal of measurement is to use the patterns of responses from patients on QOL scales to marshal evidence that the (unobservable) QOL construct is present at some quantitative level
-
The choice of which instrument to use in a particular area of research or clinical indication is primarily a matter of expert judgment
-
QOL and other patient-reported outcomes are still not measured in most clinical trials of cardiovascular disease
-
A typical approach to QOL measurement is to combine a disease-specific measure that is sensitive to the intervention under study with one or more generic instruments providing normative data
Abstract
The field of quality-of-life (QOL) measurement grew out of attempts in the 1960s and 1970s to connect the ever-increasing levels of public expenditure on technology-based health care for chronic diseases with evidence of the benefits and harms to patients. Most of the concepts, methods, and standards for measuring QOL were derived from psychometrics, but the degree to which current tools adhere to these methods varies greatly. Despite the importance of QOL, patient-reported outcomes are not measured in most cardiovascular clinical trials. Lack of familiarity with QOL measures and their interpretation, and unrealistic expectations about the information these measures can provide, are obstacles to their use. Large clinical trials of revascularization therapy for coronary artery disease and medical treatments for heart failure show small-to-moderate QOL effects, primarily detected with disease-specific instruments. Larger treatment effects, seen in trials of device therapy for heart failure and ablation therapy for atrial fibrillation, have been detected with both generic and disease-specific instruments. A large gap remains between the parameters currently being measured in clinical research and the data needed to incorporate the 'patient's voice' into therapeutic decision-making.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Bakas, T. et al. Systematic review of health-related quality of life models. Health Qual. Life Outcomes 10, 134 (2012).
Bergner, M. Quality of life, health status, and clinical research. Med. Care 27, S148–S156 (1989).
Armstrong, D. & Caldwell, D. Origins of the concept of quality of life in health care: a rhetorical solution to a political problem. Soc. Theory Health 2, 361–371 (2004).
Reiser, S. J. Medicine and the Reign of Technology (Cambridge Univ. Press, 1981).
Gruenberg, E. M. The failures of success. Milbank Mem. Fund. Q. Health Soc. 55, 3–24 (1977).
Cluff, L. E. Chronic disease, function and the quality of care. J. Chron. Dis. 34, 299–304 (1981).
McDermott, W. Absence of indicators of the influence of its physicians on a society's health; impact of physician care on society. Am. J. Med. 70, 833–843 (1981).
Tarlov, A. R. Shattuck lecture — the increasing supply of physicians, the changing structure of the health-services system, and the future practice of medicine. N. Engl. J. Med. 308, 1235–1244 (1983).
Johnson, J. R. & Temple, R. Food and Drug Administration requirements for approval of new anticancer drugs. Cancer Treat. Rep. 69, 1155–1159 (1985).
Croog, S. H. et al. The effects of antihypertensive therapy on the quality of life. N. Engl. J. Med. 314, 1657–1664 (1986).
Bruce, R. A. Evaluation of functional capacity and exercise tolerance of cardiac patients. Mod. Concepts Cardiovasc. Dis. 25, 321–326 (1956).
Geigle, R. & Jones, S. B. Outcomes measurement: a report from the front. Inquiry 27, 7–13 (1990).
Rahimi, K., Malhotra, A., Banning, A. P. & Jenkinson, C. Outcome selection and role of patient reported outcomes in contemporary cardiovascular trials: systematic review. BMJ 341, c5707 (2010).
Goldfarb, M. et al. Outcome reporting in cardiac surgery trials: systematic review and critical appraisal. J. Am. Heart Assoc. 4, e002204 (2015).
McDowell, I. Measuring Health: A Guide to Rating Scales and Questionnaires (Oxford Univ. Press, 2006).
Jones, L. V. & Thissen, D. A. in Handbook of Statistics Vol. 26. (eds Rao, C. R. & Sinharay, S.) 1–27 (Elsevier, 2006).
Spector, P. E. Summated Rating Scales Construction: An Introduction (SAGE Publications, 1992).
DeVellis, R. F. Scale Development: Theory and Applications (Applied Social Research Methods) 3rd edn (SAGE Publications, 2012).
Fayers, P. M. Quality-of-life measurement in clinical trials — the impact of causal variables. J. Biopharm. Stat. 14, 155–176 (2004).
Williams, J. I. & Naylor, C. D. How should health status measures be assessed? Cautionary notes on procrustean frameworks. J. Clin. Epidemiol. 45, 1347–1351 (1992).
Costa, D. S. & King, M. T. Conceptual, classification or causal: models of health status and health-related quality of life. Expert Rev. Pharmacoecon. Outcomes Res. 13, 631–640 (2013).
Wilson, I. B. & Cleary, P. D. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA 273, 59–65 (1995).
Ferrans, C. E., Zerwic, J. J., Wilbur, J. E. & Larson, J. L. Conceptual model of health-related quality of life. J. Nurs. Scholarsh. 37, 336–342 (2005).
Cassel, E. J. The nature of suffering and the goals of medicine. N. Engl. J. Med. 306, 639–645 (1982).
Stewart, A. L. & Ware, J. E. Measuring Functioning and Well-Being: The Medical Outcomes Study Approach (Duke Univ. Press Books, 1992).
Fairclough, D. L. Design and Analysis of Quality of Life Studies in Clinical Trials 2nd edn (Chapman and Hall/CRC, 2010).
Cleary, P. D. in Quality of Life and Pharmacoeconomics in Clinical Trials (ed. Spilker, B.) 73–78 (Lippencott Williams & Wilkins, 1996).
Wiebe, S., Guyatt, G., Weaver, B., Matijevic, S. & Sidwell, C. Comparative responsiveness of generic and specific quality-of-life instruments. J. Clin. Epidemiol. 56, 52–60 (2003).
Scoggins, J. F. & Patrick, D. L. The use of patient-reported outcomes instruments in registered clinical trials: evidence from ClinicalTrials.gov. Contemp. Clin. Trials 30, 289–292 (2009).
Testa, M. A., Anderson, R. B., Nackley, J. F. & Hollenberg, N. K. Quality of life and antihypertensive therapy in men — a comparison of captopril with enalapril. N. Engl. J. Med. 328, 907–913 (1993).
Department of Health & Human Services, U. S. PROMIS®: dynamic tools to measure health outcomes from the patient perspective [online], (2016).
Ara, R. & Wailoo, A. Using health state utility values in models exploring the cost-effectiveness of health technologies. Value Health 15, 971–974 (2012).
Knapp, T. R. The Reliability of Measuring Instruments (Edgeworth Laboratory, 2002).
Furr, R. M. & Bacharach, V. R. Psychometrics: An Introduction (SAGE Publications, 2013).
U.S. Department of Health and Human Services. Patient-reported outcome measures: use in medical product development to support labeling claims. U.S Food and Drug Administration [online], (2009).
Guyatt, G. H., Feeny, D. H. & Patrick, D. L. Measuring health-related quality of life. Ann. Intern. Med. 118, 622–629 (1993).
Revicki, D., Hays, R. D., Cella, D. & Sloan, J. Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J. Clin. Epidemiol. 61, 102–109 (2008).
Liang, M. H. Longitudinal construct validity: establishment of clinical meaning in patient evaluative instruments. Med. Care 38 (9 Suppl.), II84–II90 (2000).
Cook, T. D. & DeMets, D. L. Introduction to Statistical Methods for Clinical Trials (CRC Press, 2008).
Rubin, D. B. Causal inference through potential outcomes and principal stratification: application to studies with 'censoring' due to death. Statist. Sci. 21, 299–309 (2006).
Mark, D. B. et al. Quality-of-life outcomes with coronary artery bypass graft surgery in ischemic left ventricular dysfunction: a randomized trial. Ann. Intern. Med. 161, 392–399 (2014).
Hayden, D., Pauler, D. K. & Schoenfeld, D. An estimator for treatment comparisons among survivors in randomized trials. Biometrics 61, 305–310 (2005).
Ware, J. E. Measuring patients' views: the optimum outcome measure. BMJ 306, 1429–1430 (1993).
McGlothlin, A. E. & Lewis, R. J. Minimal clinically important difference: defining what really matters to patients. JAMA 312, 1342–1343 (2014).
Crosby, R. D., Kolotkin, R. L. & Williams, G. R. Defining clinically meaningful change in health-related quality of life. J. Clin. Epidemiol. 56, 395–407 (2003).
Streiner, D. L. & Norman, G. R. Health Measurement Scales: A Practical Guide To Their Development And Use (Oxford Univ. Press, 2008).
Wright, A., Hannon, J., Hegedus, E. J. & Kavchak, A. E. Clinimetrics corner: a closer look at the minimal clinically important difference (MCID). J. Man. Manip. Ther. 20, 160–166 (2012).
Fayers, P. M. & Manchin, D. Quality of Life: The Assessment, Analysis and Interpretation of Patient-reported Outcomes 2nd edn (Wiley-Blackwell, 2007).
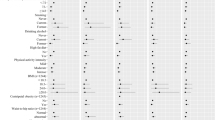
Brettschneider, C. et al. Relative impact of multimorbid chronic conditions on health-related quality of life — results from the MultiCare Cohort Study. PLoS ONE 8, e66742 (2013).
Rapkin, B. D. & Schwartz, C. E. Toward a theoretical model of quality-of-life appraisal: implications of findings from studies of response shift. Health Qual. Life Outcomes 2, 14 (2004).
Ubel, P. A., Peeters, Y. & Smith, D. Abandoning the language of 'response shift': a plea for conceptual clarity in distinguishing scale recalibration from true changes in quality of life. Qual. Life Res. 19, 465–471 (2010).
Sprangers, M. A. & Schwartz, C. E. Do not throw out the baby with the bath water: build on current approaches to realize conceptual clarity. Response to Ubel, Peeters, and Smith. Qual. Life Res. 19, 477–479 (2010).
Feinstein, A. R. Clinimetrics (Yale Univ. Press, 1987).
Fava, G. A. & Belaise, C. A discussion on the role of clinimetrics and the misleading effects of psychometric theory. J. Clin. Epidemiol. 58, 753–756 (2005).
Streiner, D. L. Clinimetrics versus psychometrics: an unnecessary distinction. J. Clin. Epidemiol. 56, 1142–1145 (2003).
Calman, K. C. Quality of life in cancer patients — an hypothesis. J. Med. Ethics 10, 124–127 (1984).
Ruta, D. A., Garratt, A. M., Leng, M., Russell, I. T. & MacDonald, L. M. A new approach to the measurement of quality of life. The Patient-Generated Index. Med. Care 32, 1109–1126 (1994).
Ruta, D. A., Garratt, A. M. & Russell, I. T. Patient centred assessment of quality of life for patients with four common conditions. Qual. Health Care 8, 22–29 (1999).
Joyce, C. R., Hickey, A., McGee, H. M. & O'Boyle, C. A. A theory-based method for the evaluation of individual quality of life: the SEIQoL. Qual. Life Res. 12, 275–280 (2003).
European Medicines Agency Committee for Medicinal Products for Human Use. Reflection paper on the regulatory guidance for the use of health related quality of life (HRQL) measures in the evaluation of medicinal products. International Society for Pharmacoeconomics and Outcomes Research [online], (2005).
Revicki, D. A. FDA draft guidance and health-outcomes research. Lancet 369, 540–542 (2007).
Gnanasakthy, A. et al. A review of patient-reported outcome labels in the United States: 2006 to 2010. Value Health 15, 437–442 (2012).
DeMuro, C. et al. Reasons for rejection of patient-reported outcome label claims: a compilation based on a review of patient-reported outcome use among new molecular entities and biologic license applications, 2006–2010. Value Health 15, 443–448 (2012).
DeMuro, C. et al. Assessment of PRO label claims granted by the FDA as compared to the EMA (2006−2010). 16, 1150–1155 (2013).
Neill, W. A. et al. Cardiac disability. The impact of coronary heart disease on patients' daily activities. Arch. Intern. Med. 145, 1642–1647 (1985).
Skinner, J. S., Albers, C. J., Hall, R. J. & Adams, P. C. Comparison of Nottingham Health Profile (NHP) scores with exercise duration and measures of ischaemia during treadmill exercise testing in patients with coronary artery disease. Eur. Heart J. 16, 1561–1565 (1995).
Ades, P. A. et al. Determinants of disability in older coronary patients. Am. Heart J. 143, 151–156 (2002).
Spertus, J. A., McDonell, M., Woodman, C. L. & Fihn, S. D. Association between depression and worse disease-specific functional status in outpatients with coronary artery disease. Am. Heart J. 140, 105–110 (2000).
Spertus, J. A. et al. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J. Am. Coll. Cardiol. 25, 333–341 (1995).
Chan, P. S., Jones, P. G., Arnold, S. A. & Spertus, J. A. Development and validation of a short version of the Seattle Angina Questionnaire. Circ. Cardiovasc. Qual. Outcomes 7, 640–647 (2014).
Hofer, S., Lim, L., Guyatt, G. & Oldridge, N. The MacNew Heart Disease health-related quality of life instrument: a summary. Health Qual. Life Outcomes 2, 3 (2004).
Hlatky, M. A. et al. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index). Am. J. Cardiol. 64, 651–654 (1989).
Hlatky, M. A. et al. Medical care costs and quality of life after randomization to coronary angioplasty or coronary bypass surgery. N. Engl. J. Med. 336, 92–99 (1997).
Boden, W. E. et al. Optimal medical therapy with or without PCI for stable coronary disease. N. Engl. J. Med. 356, 1503–1516 (2007).
Weintraub, W. S. et al. Effect of PCI on quality of life in patients with stable coronary disease. N. Engl. J. Med. 359, 677–687 (2008).
Serruys, P. W. et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N. Engl. J. Med. 360, 961–972 (2009).
Cohen, D. J. et al. Quality of life after PCI with drug-eluting stents or coronary-artery bypass surgery. N. Engl. J. Med. 364, 1016–1026 (2011).
Farkouh, M. E. et al. Strategies for multivessel revascularization in patients with diabetes. N. Engl. J. Med. 367, 2375–2384 (2012).
Abdallah, M. S. et al. Quality of life after PCI versus CABG among patients with diabetes and multivessel coronary artery disease: a randomized clinical trial. JAMA 310, 1581–1590 (2013).
Nieminen, M. S. et al. Executive summary of the guidelines on the diagnosis and treatment of acute heart failure: the Task Force on Acute Heart Failure of the European Society of Cardiology. Eur. Heart J. 26, 384–416 (2005).
Gheorghiade, M. et al. Acute heart failure syndromes: current state and framework for future research. Circulation 112, 3958–3968 (2005).
West, R. L., Hernandez, A. F., O'Connor, C. M., Starling, R. C. & Califf, R. M. A review of dyspnea in acute heart failure syndromes. Am. Heart J. 160, 209–214 (2010).
Sauser, K., Spertus, J. A., Pierchala, L., Davis, E. & Pang, P. S. Quality of life assessment for acute heart failure patients from emergency department presentation through 30 days after discharge: a pilot study with the Kansas City Cardiomyopathy Questionnaire. J. Card. Fail. 20, 18–22 (2014).
Pang, P. S. et al. A proposal to standardize dyspnoea measurement in clinical trials of acute heart failure syndromes: the need for a uniform approach. Eur. Heart J. 29, 816–824 (2008).
AbouEzzeddine, O. F. et al. Evaluation of a provocative dyspnea severity score. Am. Heart J. 172, 34–41 (2016).
Allen, L. A. et al. Improvements in signs and symptoms during hospitalization for acute heart failure follow different patterns and depend on the measurement scales used: an international, prospective registry to evaluate the evolution of measures of disease severity in acute heart failure (MEASURE-AHF). J. Card. Fail. 14, 777–784 (2008).
Publication Committee for the VMAC Investigators. Intravenous nesiritide versus nitroglycerin for treatment of decompensated congestive heart failure: a randomized controlled trial. JAMA 287, 1531–1540 (2002).
O'Connor, C. M. et al. Effect of nesiritide in patients with acute decompensated heart failure. N. Engl. J. Med. 365, 32–43 (2011).
Wilson, J. R., Rayos, G., Yeoh, T. K., Gothard, P. & Bak, K. Dissociation between exertional symptoms and circulatory function in patients with heart failure. Circulation 92, 47–53 (1995).
Piepoli, M. F. et al. Exercise intolerance in chronic heart failure: mechanisms and therapies. Part I. Eur. J. Cardiovasc. Prev. Rehabil. 17, 637–642 (2010).
Witte, K. K. & Clark, A. L. Why does chronic heart failure cause breathlessness and fatigue? Prog. Cardiovasc. Dis. 49, 366–384 (2007).
Wilson, J. R., Hanamanthu, S., Chomsky, D. B. & Davis, S. F. Relationship between exertional symptoms and functional capacity in patients with heart failure. J. Am. Coll. Cardiol. 33, 1943–1947 (1999).
Russell, S. D., McNeer, F. R. & Higginbotham, M. B. Exertional dyspnea in heart failure: a symptom unrelated to pulmonary function at rest or during exercise. Am. Heart J. 135, 398–405 (1998).
Clark, A. L. Origin of symptoms in chronic heart failure. Heart 92, 12–16 (2006).
Coats, A. J., Clark, A. L., Piepoli, M., Volterrani, M. & Poole-Wilson, P. A. Symptoms and quality of life in heart failure: the muscle hypothesis. Br. Heart J. 72, S36–S39 (1994).
Goldman, L. et al. Pitfalls in the serial assessment of cardiac functional status. How a reduction in 'ordinary' activity may reduce the apparent degree of cardiac compromise and give a misleading impression of improvement. J. Chronic Dis. 35, 763–771 (1982).
Rumsfeld, J. S. et al. Depressive symptoms are the strongest predictors of short-term declines in health status in patients with heart failure. J. Am. Coll. Cardiol. 42, 1811–1187 (2003).
Havranek, E. P., Spertus, J. A., Masoudi, F. A., Jones, P. G. & Rumsfeld, J. S. Predictors of the onset of depressive symptoms in patients with heart failure. J. Am. Coll. Cardiol. 44, 2333–2338 (2004).
Rector, T. S., Francis, G. S. & Cohn, J. N. Patients' self-assessment of their congestive heart failure. Part 1: Patient perceived dysfunction and its poor correlation with maximal exercise tests. Heart Fail. 3, 192–196 (1987).
Rector, T. S., Kubo, S. H. & Cohn, J. N. Patients' self-assessment of their congestive heart failure. Part 2: Content, reliability, and validity of a new measure, the Minnesota Living with Heart Failure questionnaire. Heart Fail. 3, 198–209 (1987).
Rector, T. S. et al. Use of the Living With Heart Failure questionnaire to ascertain patients' perspectives on improvement in quality of life versus risk of drug-induced death. J. Card. Fail. 1, 201–206 (1995).
Green, C. P., Porter, C. B., Bresnahan, D. R. & Spertus, J. A. Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: a new health status measure for heart failure. J. Am. Coll. Cardiol. 35, 1245–1255 (2000).
Spertus, J. et al. Monitoring clinical changes in patients with heart failure: a comparison of methods. Am. Heart J. 150, 707–715 (2005).
Spertus, J. A. & Jones, P. G. Development and validation of a short version of the Kansas City Cardiomyopathy Questionnaire. Circ. Cardiovasc. Qual. Outcomes 8, 469–476 (2015).
Rogers, W. J. et al. Quality of life among 5,025 patients with left ventricular dysfunction randomized between placebo and enalapril: the studies of left ventricular dysfunction. J. Am. Coll. Cardiol. 23, 393–400 (1994).
Rector, T. S., Kubo, S. H. & Cohn, J. N. Validity of the Minnesota Living with Heart Failure questionnaire as a measure of therapeutic response to enalapril or placebo. Am. J. Cardiol. 71, 1106–1107 (1993).
Taylor, A. L. et al. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N. Engl. J. Med. 351, 2049–2057 (2004).
Hjalmarson, A. et al. Effects of controlled-release metoprolol on total mortality, hospitalizations, and well-being in patients with heart failure: the Metoprolol CR/XL Randomized Intervention Trial in congestive heart failure (MERIT-HF). JAMA 283, 1295–1302 (2000).
Tate, C. W. 3rd et al. Quality of life and prognosis in heart failure: results of the Beta-Blocker Evaluation of Survival Trial (BEST). J. Card. Fail. 13, 732–737 (2007).
Gallanagh, S. et al. Evaluation of the functional status questionnaire in heart failure: a sub-study of the second cardiac insufficiency bisoprolol survival study (CIBIS-II). Cardiovasc. Drugs Ther. 25, 77–85 (2011).
Cohn, J. N. et al. Safety and efficacy of carvedilol in severe heart failure. J. Card. Fail. 3, 173–179 (1997).
Cleland, J. G. et al. A comparison of the effects of carvedilol and metoprolol on well-being, morbidity, and mortality (the 'patient journey') in patients with heart failure: a report from the Carvedilol Or Metoprolol European Trial (COMET). J. Am. Coll. Cardiol. 47, 1603–1611 (2006).
Gelber, R. D. & Gelber, S. Quality-of-life assessment in clinical trials. Cancer Treat. Res. 75, 225–246 (1995).
Velazquez, E. J. et al. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N. Engl. J. Med. 364, 1607–1616 (2011).
Abraham, W. T. et al. Cardiac resynchronization in chronic heart failure. N. Engl. J. Med. 346, 1845–1853 (2002).
Cleland, J. G. et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N. Engl. J. Med. 352, 1539–1549 (2005).
Cleland, J. G., Calvert, M. J., Verboven, Y. & Freemantle, N. Effects of cardiac resynchronization therapy on long-term quality of life: an analysis from the CArdiac Resynchronisation-Heart Failure (CARE-HF) study. Am. Heart J. 157, 457–466 (2009).
De Marco, T. et al. Impact of cardiac resynchronization therapy on exercise performance, functional capacity, and quality of life in systolic heart failure with QRS prolongation: COMPANION trial sub-study. J. Card. Fail. 14, 9–18 (2008).
Veazie, P. J. et al. Cardiac resynchronization and quality of life in patients with minimally symptomatic heart failure. J. Am. Coll. Cardiol. 60, 1940–1944 (2012).
Rose, E. A. et al. Long-term use of a left ventricular assist device for end-stage heart failure. N. Engl. J. Med. 345, 1435–1443 (2001).
Slaughter, M. S. et al. Advanced heart failure treated with continuous-flow left ventricular assist device. N. Engl. J. Med. 361, 2241–2251 (2009).
Kim, C. A. et al. Functional status and quality of life after transcatheter aortic valve replacement: a systematic review. Ann. Intern. Med. 160, 243–254 (2014).
Leon, M. B. et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N. Engl. J. Med. 363, 1597–1607 (2010).
Reynolds, M. R. et al. Health-related quality of life after transcatheter aortic valve replacement in inoperable patients with severe aortic stenosis. Circulation 124, 1964–1972 (2011).
Reynolds, M. R. et al. Health-related quality of life after transcatheter or surgical aortic valve replacement in high-risk patients with severe aortic stenosis: results from the PARTNER (Placement of AoRTic TraNscathetER Valve) Trial (Cohort A). J. Am. Coll. Cardiol. 60, 548–558 (2012).
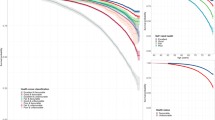
Arnold, S. V. et al. How to define a poor outcome after transcatheter aortic valve replacement: conceptual framework and empirical observations from the placement of aortic transcatheter valve (PARTNER) trial. Circ. Cardiovasc. Qual. Outcomes 6, 591–597 (2013).
Gronefeld, G. C. & Hohnloser, S. H. Quality of life in atrial fibrillation: an increasingly important issue. Eur. Heart J. 5, H25–H33 (2003).
Rienstra, M. et al. Symptoms and functional status of patients with atrial fibrillation: state of the art and future research opportunities. Circulation 125, 2933–2943 (2012).
Savelieva, I., Paquette, M., Dorian, P., Luderitz, B. & Camm, A. J. Quality of life in patients with silent atrial fibrillation. Heart 85, 216–217 (2001).
Aliot, E., Botto, G. L., Crijns, H. J. & Kirchhof, P. Quality of life in patients with atrial fibrillation: how to assess it and how to improve it. Europace 16, 787–796 (2014).
Bubien, R. S., Knotts-Dolson, S. M., Plumb, V. J. & Kay, G. N. Effect of radiofrequency catheter ablation on health-related quality of life and activities of daily living in patients with recurrent arrhythmias. Circulation 94, 1585–1591 (1996).
Reynolds, M. R., Ellis, E. & Zimetbaum, P. Quality of life in atrial fibrillation: measurement tools and impact of interventions. J. Cardiovasc. Electrophysiol. 19, 762–768 (2008).
Wokhlu, A. et al. Long-term quality of life after ablation of atrial fibrillation the impact of recurrence, symptom relief, and placebo effect. J. Am. Coll. Cardiol. 55, 2308–2316 (2010).
US National Library of Science. ClinicalTrials.gov[online], (2015).
Arribas, F. et al. Validation of the AF-QoL, a disease-specific quality of life questionnaire for patients with atrial fibrillation. Europace 12, 364–370 (2010).
Mont, L. et al. Catheter ablation versus antiarrhythmic drug treatment of persistent atrial fibrillation: a multicentre, randomized, controlled trial (SARA study). Eur. Heart J. 35, 501–507 (2014).
Spertus, J. et al. Development and validation of the Atrial Fibrillation Effect on QualiTy-of-Life (AFEQT) Questionnaire in patients with atrial fibrillation. Circ. Arrhythm. Electrophysiol. 4, 15–25 (2011).
Freeman, J. V. et al. Association between atrial fibrillation symptoms, quality of life, and patient outcomes: results from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF). Circ. Cardiovasc. Qual. Outcomes 8, 393–402 (2015).
Jenkins, L. S. et al. Quality of life in atrial fibrillation: the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) study. Am. Heart J. 149, 112–120 (2005).
Hagens, V. E. et al. Effect of rate or rhythm control on quality of life in persistent atrial fibrillation. Results from the Rate Control Versus Electrical Cardioversion (RACE) Study. J. Am. Coll. Cardiol. 43, 241–247 (2004).
Suman-Horduna, I. et al. Quality of life and functional capacity in patients with atrial fibrillation and congestive heart failure. J. Am. Coll. Cardiol. 61, 455–460 (2013).
Wilber, D. J. et al. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA 303, 333–340 (2010).
Reynolds, M. R., Walczak, J., White, S. A., Cohen, D. J. & Wilber, D. J. Improvements in symptoms and quality of life in patients with paroxysmal atrial fibrillation treated with radiofrequency catheter ablation versus antiarrhythmic drugs. Circ. Cardiovasc. Qual. Outcomes 3, 615–623 (2010).
Cosedis Nielsen, J. et al. Radiofrequency ablation as initial therapy in paroxysmal atrial fibrillation. N. Engl. J. Med. 367, 1587–1595 (2012).
Morillo, C. A. et al. Radiofrequency ablation versus antiarrhythmic drugs as first-line treatment of paroxysmal atrial fibrillation (RAAFT-2): a randomized trial. JAMA 311, 692–700 (2014).
Pappone, C. et al. Radiofrequency catheter ablation and antiarrhythmic drug therapy: a prospective, randomized, 4-year follow-up trial: the APAF study. Circ. Arrhythm. Electrophysiol. 4, 808–814 (2011).
Riis, J. et al. Ignorance of hedonic adaptation to hemodialysis: a study using ecological momentary assessment. J. Exp. Psychol. Gen. 134, 3–9 (2005).
World Health Organization. Consitution of the World Health Organization. Am. J. Public Health Nations Health 36, 1315–1323 (1946).
Brook, R. H. et al. Does free care improve adults' health? Results from a randomized controlled trial. N. Engl. J. Med. 309, 1426–1434 (1983).
Bergner, M., Bobbitt, R. A., Carter, W. B. & Gilson, B. S. The Sickness Impact Profile: development and final revision of a health status measure. Med. Care 19, 787–805 (1981).
Bergner, M. et al. The Sickness Impact Profile: conceptual formulation and methodology for the development of a health status measure. Int. J. Health Serv. 6, 393–415 (1976).
Kaplan, R. M., Bush, J. W. & Berry, C. C. Health status: types of validity and the index of well-being. Health Serv. Res. 11, 478–507 (1976).
Torrance, G. W. Toward a utility theory foundation for health status index models. Health Serv. Res. 11, 349–369 (1976).
Patrick, D. L. & Erickson, P. Health Status and Health Policy: Quality of Life in Health Care Evaluation and Resource Allocation (Oxford Univ. Press, 1993).
Califf, R. M., Mark, D. B. & Wagner, G. S. Acute Coronary Care In The Thrombolytic Era 2nd edn (Mosby, 1995).
Douglas, P. S. et al. PROspective Multicenter Imaging Study for Evaluation of chest pain: rationale and design of the PROMISE trial. Am. Heart J. 167, 796–803.e1 (2014).
US National Library of Science. ClinicalTrials.gov[online], (2015).
Califf, R. M. et al. One-year results from the Global Utilization of Streptokinase and TPA for Occluded Coronary Arteries (GUSTO-I) trial. Circulation 94, 1233–1238 (1996).
Mark, D. B. et al. Quality of life after late invasive therapy for occluded arteries. N. Engl. J. Med. 360, 774–783 (2009).
Hlatky, M. A. et al. The effect of obesity on quality of life in patients with diabetes and coronary artery disease. Am. Heart J. 159, 292–300 (2010).
Arnold, S. V. et al. Effects of ranolazine on disease-specific health status and quality of life among patients with acute coronary syndromes: results from the MERLIN-TIMI 36 randomized trial. Circ. Cardiovasc. Qual. Outcomes 1, 107–115 (2008).
Majani, G. et al. Effect of valsartan on quality of life when added to usual therapy for heart failure: results from the Valsartan Heart Failure Trial. J. Card. Fail. 11, 253–259 (2005).
Wong, C. M. et al. Clinical characteristics and outcomes of young and very young adults with heart failure: the CHARM programme (Candesartan in Heart Failure Assessment of Reduction in Mortality and Morbidity). J. Am. Coll. Cardiol. 62, 1845–1854 (2013).
Park, S. J. et al. Left ventricular assist devices as destination therapy: a new look at survival. J. Thorac. Cardiovasc. Surg. 129, 9–17 (2005).
Aranda, J. M. Jr, Conti, J. B., Johnson, J. W., Petersen-Stejskal, S. & Curtis, A. B. Cardiac resynchronization therapy in patients with heart failure and conduction abnormalities other than left bundle-branch block: analysis of the Multicenter InSync Randomized Clinical Evaluation (MIRACLE). Clin. Cardiol. 27, 678–682 (2004).
Flynn, K. E. et al. Effects of exercise training on health status in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA 301, 1451–1459 (2009).
Mark, D. B. et al. Quality of life and economic outcomes with surgical ventricular reconstruction in ischemic heart failure: results from the Surgical Treatment for Ischemic Heart Failure trial. Am. Heart J. 157, 837–844 (2009).
McMurray, J. J. et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N. Engl. J. Med. 371, 993–1004 (2014).
Hamo, C. E. et al. Baseline distribution of participants with depression and impaired quality of life in the Treatment of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist Trial. Circ. Heart Fail. 8, 268–277 (2015).
Xiong, G. L. et al. Health status and depression remission in patients with chronic heart failure: patient-reported outcomes from the SADHART-CHF trial. Circ. Heart Fail. 5, 688–692 (2012).
Califf, R. M. et al. A randomized controlled trial of epoprostenol therapy for severe congestive heart failure: the Flolan International Randomized Survival Trial (FIRST). Am. Heart J. 134, 44–54 (1997).
Dorian, P. et al. The impairment of health-related quality of life in patients with intermittent atrial fibrillation: implications for the assessment of investigational therapy. J. Am. Coll. Cardiol. 36, 1303–1309 (2000).
Singh, S. N. et al. Quality of life and exercise performance in patients in sinus rhythm versus persistent atrial fibrillation: a Veterans Affairs Cooperative Studies Program Substudy. J. Am. Coll. Cardiol. 48, 721–730 (2006).
Kay, G. N. et al. The Ablate and Pace Trial: a prospective study of catheter ablation of the AV conduction system and permanent pacemaker implantation for treatment of atrial fibrillation. APT Investigators. J. Interv. Card. Electrophysiol. 2, 121–135 (1998).
Groenveld, H. F. et al. The effect of rate control on quality of life in patients with permanent atrial fibrillation: data from the RACE II (Rate Control Efficacy in Permanent Atrial Fibrillation II) study. J. Am. Coll. Cardiol. 58, 1795–1803 (2011).
Acknowledgements
The author acknowledges his gratitude to Melanie R. Daniels (Howl, Inc., Durham, North Carolina, USA) for her research and editorial work on this project, and to Dr Kevin Weinfurt (Duke University, Durham, North Carolina, USA) for a critical review of an early version of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares having been a consultant for CardioDx, Gilead, Medtronic, and St. Jude Medical; and receiving research grants from AstraZeneca, Bristol Myers Squibb, Eli Lilly, Gilead, and Medtronic.
Supplementary information
Supplementary information S1 (table)
Clinical trials of revascularization versus medical therapy for CAD (DOCX 34 kb)
Supplementary information S2 (table)
Clinical trials of PCI versus CABG surgery for CAD (DOCX 34 kb)
Supplementary information S3 (table)
Clinical trials of medical therapy for chronic heart failure (DOCX 42 kb)
Supplementary information S4 (table)
Clinical trials of device therapy for chronic heart failure (DOCX 30 kb)
Related links
Rights and permissions
About this article
Cite this article
Mark, D. Assessing quality-of-life outcomes in cardiovascular clinical research. Nat Rev Cardiol 13, 286–308 (2016). https://doi.org/10.1038/nrcardio.2016.10
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2016.10
This article is cited by
-
Patient-centered care in Coronary Heart Disease: what do you want to measure? A systematic review of reviews on patient-reported outcome measures
Quality of Life Research (2023)
-
Evolution of symptoms in patients with stable angina after normal regadenoson myocardial perfusion imaging: The Radionuclide Imaging and Symptomatic Evolution study (RISE)
Journal of Nuclear Cardiology (2022)
-
Atherosclerosis
Nature Reviews Disease Primers (2019)
-
Revascularization in stable coronary disease: evidence and uncertainties
Nature Reviews Cardiology (2018)
-
Lower educational level and unemployment increase the impact of cardiometabolic conditions on the quality of life: results of a population-based study in South Australia
Quality of Life Research (2017)