Key Points
-
Although few prospective studies of atrial fibrillation (AF) epidemiology in Asian countries have been conducted, AF prevalence is thought to be lower in Asians than in white populations
-
However, Asian individuals seem to be at a higher risk of stroke, and have greater stroke-related morbidity and mortality, than white individuals
-
Asian individuals seem to be at particularly high risk of haemorrhagic stroke and intracranial haemorrhage, which has discouraged the widespread uptake of warfarin in Asian patients with AF
-
Antiplatelet agents have been overused for primary stroke prevention in Asian patients with AF, in whom these drugs are neither safe nor effective
-
Non-vitamin K antagonist anticoagulants are noninferior to warfarin for stroke prevention in AF, and are associated with a reduced incidence of haemorrhagic stroke and intracranial haemorrhage compared with warfarin
-
The efficacy and safety profile of non-vitamin K antagonist anticoagulants in randomized, controlled trials suggest these drugs have great potential as anticoagulants in Asian individuals with AF
Abstract
Anticoagulation is the most-important intervention to prevent stroke in patients with atrial fibrillation (AF). Despite a lower point prevalence of AF in Asian communities and Asian countries than in other populations, individuals of Asian ethnicity are at a disproportionately high risk of stroke and have greater consequent mortality. Warfarin and other vitamin K antagonists are conventionally used for anticoagulation, and demonstrably reduce the risk of stroke and all-cause mortality in patients with AF. The use of warfarin in Asian countries is suboptimal, primarily owing to the universal challenge of achieving controlled anticoagulation with an unpredictable drug as well as concerns about the particularly high-risk of haemorrhage in Asian patients. Instead, antiplatelet therapy has been favoured in Asian communities, this strategy is neither safe nor effective for stroke prevention in these individuals. The non-vitamin K antagonist, oral anticoagulant drugs offer a solution to this challenge. The direct thrombin inhibitor dabigatran, and the direct factor Xa inhibitors apixaban, edoxaban, and rivaroxaban, have demonstrated noninferiority to warfarin in the prevention of stroke and systemic embolism in international, randomized, controlled trials. Importantly, some of these drugs are also associated with a significantly lower incidence of major haemorrhage, and all result in lower rates of intracranial haemorrhage and haemorrhagic stroke than warfarin. In this article, we review the use of the non-vitamin K antagonist anticoagulants in the management of AF in Asian populations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Change history
02 September 2014
In the version of this article initially published online and in print, 'thrombin' was misspelled in Figure 1. The error has been corrected for the HTML and PDF versions of the article.
References
Lip, G. Y., Brechin, C. M. & Lane, D. A. The global burden of atrial fibrillation and stroke: a systematic review of the epidemiology of atrial fibrillation in regions outside North America and Europe. Chest 142, 1489–1498 (2012).
Wolf, P. A., Abbott, R. D. & Kannel, W. B. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 22, 983–988 (1991).
Wang, T. J. et al. Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: the Framingham Heart Study. Circulation 107, 2920–2925 (2003).
Benjamin, E. J. et al. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation 98, 946–952 (1998).
Santangeli, P. et al. Atrial fibrillation and the risk of incident dementia: a meta-analysis. Heart Rhythm 9, 1761–1768 (2012).
Iwasaki, Y. K., Nishida, K., Kato, T. & Nattel, S. Atrial fibrillation pathophysiology: implications for management. Circulation 124, 2264–2274 (2011).
Benjamin, E. J. et al. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA 271, 840–844 (1994).
Krahn, A. D., Manfreda, J., Tate, R. B., Mathewson, F. A. & Cuddy, T. E. The natural history of atrial fibrillation: incidence, risk factors, and prognosis in the Manitoba Follow-Up Study. Am. J. Med. 98, 476–484 (1995).
Gami, A. S. et al. Association of atrial fibrillation and obstructive sleep apnea. Circulation 110, 364–367 (2004).
Watanabe, H. et al. Metabolic syndrome and risk of development of atrial fibrillation: the Niigata preventive medicine study. Circulation 117, 1255–1260 (2008).
Fox, C. S. et al. Parental atrial fibrillation as a risk factor for atrial fibrillation in offspring. JAMA 291, 2851–2855 (2004).
Lubitz, S. A. et al. Genetics of atrial fibrillation: implications for future research directions and personalized medicine. Circ. Arrhythm. Electrophysiol. 3, 291–299 (2010).
Lloyd-Jones, D. et al. Heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation 121, e46–e215 (2010).
Stewart, S., Hart, C. L., Hole, D. J. & McMurray, J. J. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am. J. Med. 113, 359–364 (2002).
Kim, M. H., Johnston, S. S., Chu, B. C., Dalal, M. R. & Schulman, K. L. Estimation of total incremental health care costs in patients with atrial fibrillation in the United States. Circ. Cardiovasc. Qual. Outcomes 4, 313–320 (2011).
Feinberg, W. M., Blackshear, J. L., Laupacis, A., Kronmal, R. & Hart, R. G. Prevalence, age distribution, and gender of patients with atrial fibrillation. Analysis and implications. Arch. Intern. Med. 155, 469–473 (1995).
Heeringa, J. et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur. Heart J. 27, 949–953 (2006).
Go, A. S. et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 285, 2370–2375 (2001).
Chugh, S. S., Blackshear, J. L., Shen, W. K., Hammill, S. C. & Gersh, B. J. Epidemiology and natural history of atrial fibrillation: clinical implications. J. Am. Coll. Cardiol. 37, 371–378 (2001).
Lloyd-Jones, D. M. et al. Lifetime risk for development of atrial fibrillation: the Framingham Heart Study. Circulation 110, 1042–1046 (2004).
Kakkar, A. K. et al. Risk profiles and antithrombotic treatment of patients newly diagnosed with atrial fibrillation at risk of stroke: perspectives from the international, observational, prospective GARFIELD registry. PLoS ONE 8, e63479 (2013).
Mathur, R. et al. Ethnicity and stroke risk in patients with atrial fibrillation. Heart 99, 1087–1092 (2013).
Lip, G. Y. et al. Atrial fibrillation amongst the Indo-Asian general practice population. The West Birmingham Atrial Fibrillation Project. Int. J. Cardiol. 65, 187–192 (1998).
Zhou, Z. & Hu, D. An epidemiological study on the prevalence of atrial fibrillation in the Chinese population of mainland China. J. Epidemiol. 18, 209–216 (2008).
Inoue, H. et al. Prevalence of atrial fibrillation in the general population of Japan: an analysis based on periodic health examination. Int. J. Cardiol. 137, 102–107 (2009).
Lau, C. P. et al. Ethnic differences in atrial fibrillation identified using implanted cardiac devices. J. Cardiovasc. Electrophysiol. 24, 381–387 (2013).
Tsai, C. F., Thomas, B. & Sudlow, C. L. Epidemiology of stroke and its subtypes in Chinese vs white populations: a systematic review. Neurology 81, 264–272 (2013).
Kim, A. S. & Johnston, S. C. Global variation in the relative burden of stroke and ischemic heart disease. Circulation 124, 314–323 (2011).
Gunarathne, A. et al. Ischemic stroke in South Asians: a review of the epidemiology, pathophysiology, and ethnicity-related clinical features. Stroke 40, e415–e423 (2009).
Steg, P. G. et al. One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA 297, 1197–1206 (2007).
Ducrocq, G. et al. Geographic differences in outcomes in outpatients with established atherothrombotic disease: results from the REACH Registry. Eur. J. Prev. Cardiol. http://dx.doi.org/10.1177/2047487313501278.
Khan, N. A. et al. Risk factors, quality of care and prognosis in South Asian, East Asian and White patients with stroke. BMC Neurol. 13, 74 (2013).
Sen, S. et al. Racial-ethnic differences in stroke risk factors and subtypes: results of a prospective hospital-based registry. Int. J. Neurosci. 123, 568–574 (2013).
Goto, S. et al. One-year cardiovascular event rates in Japanese outpatients with myocardial infarction, stroke, and atrial fibrillation. Results from the Japan Thrombosis Registry for Atrial Fibrillation, Coronary, or Cerebrovascular Events (J-TRACE). Circ. J. 75, 2598–2604 (2011).
Li, S. Y. et al. One-year clinical prediction in Chinese ischemic stroke patients using the CHADS2 and CHA2DS2-VASc scores: the China National Stroke Registry. CNS Neurosci. Ther. 18, 988–993 (2012).
Toda, E. et al. Use of the CHADS2 and CHA2DS2-VASC score in Japanese patients with atrial fibrillation, coronary or cerebrovascular events (J-TRACE). J. Am. Coll. Cardiol. 59, E674 (2012).
Yap, K. B., Ng, T. P. & Ong, H. Y. Low prevalence of atrial fibrillation in community-dwelling Chinese aged 55 years or older in Singapore: a population-based study. J. Electrocardiol. 41, 94–98 (2008).
Tanizaki, Y. et al. Incidence and risk factors for subtypes of cerebral infarction in a general population: the Hisayama study. Stroke 31, 2616–2622 (2000).
Chien, K. L. et al. Atrial fibrillation prevalence, incidence and risk of stroke and all-cause death among Chinese. Int. J. Cardiol. 139, 173–180 (2010).
Lip, G. Y., Kamath, S., Jafri, M., Mohammed, A. & Bareford, D. Ethnic differences in patient perceptions of atrial fibrillation and anticoagulation therapy: the West Birmingham Atrial Fibrillation Project. Stroke 33, 238–242 (2002).
Zhao, D. et al. Epidemiological transition of stroke in China: twenty-one-year observational study from the Sino-MONICA-Beijing Project. Stroke 39, 1668–1674 (2008).
Kubo, M. et al. Decreasing incidence of lacunar vs other types of cerebral infarction in a Japanese population. Neurology 66, 1539–1544 (2006).
Greenberg, S. M. et al. Cerebral microbleeds: a guide to detection and interpretation. Lancet Neurol. 8, 165–174 (2009).
Koennecke, H. C. Cerebral microbleeds on MRI: prevalence, associations, and potential clinical implications. Neurology 66, 165–171 (2006).
Bokura, H. et al. Microbleeds are associated with subsequent hemorrhagic and ischemic stroke in healthy elderly individuals. Stroke 42, 1867–1871 (2011).
Lee, S. H., Ryu, W. S. & Roh, J. K. Cerebral microbleeds are a risk factor for warfarin-related intracerebral hemorrhage. Neurology 72, 171–176 (2009).
Suzuki, S. et al. Incidence of major bleeding complication of warfarin therapy in Japanese patients with atrial fibrillation. Circ. J. 71, 761–765 (2007).
Veenstra, D. L. et al. Association of Vitamin K epoxide reductase complex 1 (VKORC1) variants with warfarin dose in a Hong Kong Chinese patient population. Pharmacogenet. Genomics 15, 687–691 (2005).
Hyun, K. K. et al. A comparative analysis of risk factors and stroke risk for Asian and non-Asian men: the Asia Pacific cohort studies collaboration. Int. J. Stroke 8, 606–611 (2013).
Investigators, A. F. Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation. Analysis of pooled data from five randomized controlled trials. Arch. Intern. Med. 154, 1449–1457 (1994).
van Walraven, C. et al. Oral anticoagulants vs aspirin in nonvalvular atrial fibrillation: an individual patient meta-analysis. JAMA 288, 2441–2448 (2002).
Holbrook, A. M. et al. Systematic overview of warfarin and its drug and food interactions. Arch. Intern. Med. 165, 1095–1106 (2005).
Aithal, G. P., Day, C. P., Kesteven, P. J. & Daly, A. K. Association of polymorphisms in the cytochrome P450 CYP2C9 with warfarin dose requirement and risk of bleeding complications. Lancet 353, 717–719 (1999).
D'Andrea, G. et al. A polymorphism in the VKORC1 gene is associated with an interindividual variability in the dose-anticoagulant effect of warfarin. Blood 105, 645–649 (2005).
Kimmel, S. E. et al. A pharmacogenetic versus a clinical algorithm for warfarin dosing. N. Engl. J. Med. 369, 2283–2293 (2013).
Verhoef, T. I. et al. A randomized trial of genotype-guided dosing of acenocoumarol and phenprocoumon. N. Engl. J. Med. 369, 2304–2312 (2013).
Pirmohamed, M. et al. A randomized trial of genotype-guided dosing of warfarin. N. Engl. J. Med. 369, 2294–2303 (2013).
Connolly, S. J. et al. Dabigatran versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 361, 1139–1151 (2009).
Granger, C. B. et al. Apixaban versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 365, 981–992 (2011).
Albertsen, I. E. et al. Risk of stroke or systemic embolism in atrial fibrillation patients treated with warfarin: a systematic review and meta-analysis. Stroke 44, 1329–1336 (2013).
Guo, Y. et al. Stroke risk and suboptimal thromboprophylaxis in Chinese patients with atrial fibrillation: would the novel oral anticoagulants have an impact? Int. J. Cardiol. 168, 515–522 (2012).
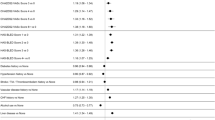
Hori, M. et al. Dabigatran versus warfarin: effects on ischemic and hemorrhagic strokes and bleeding in Asians and non-Asians with atrial fibrillation. Stroke 44, 1891–1896 (2013).
Goto, S. et al. Efficacy and safety of apixaban compared with warfarin for stroke prevention in atrial fibrillation in East Asia. Eur. Heart J. 34, 1039 (2013).
Patel, M. R. et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N. Engl. J. Med. 365, 883–891 (2011).
Goto, S. et al. Regional differences in use of antithrombotic therapy for stroke prevention in atrial fibrillation and associated outcomes: European and Asian insights. Eur. Heart J. 34, 790–791 (2013).
Sato, H. et al. Low-dose aspirin for prevention of stroke in low-risk patients with atrial fibrillation: Japan Atrial Fibrillation Stroke Trial. Stroke 37, 447–451 (2006).
Shinohara, Y. et al. Cilostazol for prevention of secondary stroke (CSPS 2): an aspirin-controlled, double-blind, randomised non-inferiority trial. Lancet Neurol. 9, 959–968 (2010).
Kamal, A. K., Naqvi, I., Husain, M. R. & Khealani, B. A. Cilostazol versus aspirin for secondary prevention of vascular events after stroke of arterial origin. Cochrane Database of Systematic Reviews, Issue 1. Art. No.: CD008076. http://dx.doi.org/10.1002/14651858.CD008076.pub2.
Wan, Y. et al. Anticoagulation control and prediction of adverse events in patients with atrial fibrillation: a systematic review. Circ. Cardiovasc. Qual. Outcomes 1, 84–91 (2008).
Rose, A. J., Ozonoff, A., Grant, R. W., Henault, L. E. & Hylek, E. M. Epidemiology of subtherapeutic anticoagulation in the United States. Circ. Cardiovasc. Qual. Outcomes 2, 591–597 (2009).
Bode, W. et al. The refined 1.9 A crystal structure of human alpha-thrombin: interaction with D-Phe-Pro-Arg chloromethylketone and significance of the Tyr-Pro-Pro-Trp insertion segment. EMBO J. 8, 3467–3475 (1989).
Di Nisio, M., Middeldorp, S. & Buller, H. R. Direct thrombin inhibitors. N. Engl. J. Med. 353, 1028–1040 (2005).
Lee, C. J. & Ansell, J. E. Direct thrombin inhibitors. Br. J. Clin. Pharmacol. 72, 581–592 (2011).
Ho, S. J. & Brighton, T. A. Ximelagatran: direct thrombin inhibitor. Vasc. Health Risk Manag. 2, 49–58 (2006).
Albers, G. W. et al. Ximelagatran vs warfarin for stroke prevention in patients with nonvalvular atrial fibrillation: a randomized trial. JAMA 293, 690–698 (2005).
AstraZeneca. AstraZeneca Decides to Withdraw Exanta™[online], (2006).
Olsson, S. B. Stroke prevention with the oral direct thrombin inhibitor ximelagatran compared with warfarin in patients with non-valvular atrial fibrillation (SPORTIF III): randomised controlled trial. Lancet 362, 1691–1698 (2003).
Deinum, J., Mattsson, C., Inghardt, T. & Elg, M. Biochemical and pharmacological effects of the direct thrombin inhibitor AR-H067637. Thromb. Haemost. 101, 1051–1059 (2009).
Lip, G. Y. et al. Oral direct thrombin inhibitor AZD0837 for the prevention of stroke and systemic embolism in patients with non-valvular atrial fibrillation: a randomized dose-guiding, safety, and tolerability study of four doses of AZD0837 vs. vitamin K antagonists. Eur. Heart J. 30, 2897–2907 (2009).
Olsson, S. B. et al. Safety and tolerability of an immediate-release formulation of theoral direct thrombin inhibitor AZD0837 in the prevention of stroke and systemic embolism in patients with atrial fibrillation. Thromb. Haemost. 103, 604–612 (2010).
Lip, G. Y. et al. Oral direct thrombin inhibitor AZD0837 for the prevention of stroke and systemic embolism in patients with non-valvular atrial fibrillation: a phase II study of AZD0837 in patients who are appropriate for but unable or unwilling to take vitamin K antagonist therapy. Thromb. Res. 127, 91–99 (2011).
Blech, S., Ebner, T., Ludwig-Schwellinger, E., Stangier, J. & Roth, W. The metabolism and disposition of the oral direct thrombin inhibitor, dabigatran, in humans. Drug Metab. Dispos. 36, 386–399 (2008).
Ezekowitz, M. D. et al. Dabigatran with or without concomitant aspirin compared with warfarin alone in patients with nonvalvular atrial fibrillation (PETRO Study). Am. J. Cardiol. 100, 1419–1426 (2007).
Hori, M. et al. Efficacy and safety of dabigatran vs. warfarin in patients with atrial fibrillation-sub-analysis in Japanese population in RE-LY trial. Circ. J. 75, 800–805 (2011).
Hartter, S., Yamamura, N., Stangier, J., Reilly, P. A. & Clemens, A. Pharmacokinetics and pharmacodynamics in Japanese and Caucasian subjects after oral administration of dabigatran etexilate. Thromb. Haemost. 107, 260–269 (2012).
Yeh, C. H., Fredenburgh, J. C. & Weitz, J. I. Oral direct factor Xa inhibitors. Circ. Res. 111, 1069–1078 (2012).
Buller, H. R. et al. Subcutaneous fondaparinux versus intravenous unfractionated heparin in the initial treatment of pulmonary embolism. N. Engl. J. Med. 349, 1695–1702 (2003).
Yusuf, S. et al. Comparison of fondaparinux and enoxaparin in acute coronary syndromes. N. Engl. J. Med. 354, 1464–1476 (2006).
Padmanabhan, K. et al. Structure of human des(1–45) factor Xa at 2.2 A resolution. J. Mol. Biol. 232, 947–966 (1993).
Perzborn, E., Roehrig, S., Straub, A., Kubitza, D. & Misselwitz, F. The discovery and development of rivaroxaban, an oral, direct factor Xa inhibitor. Nat. Rev. Drug Discov. 10, 61–75 (2011).
Perzborn, E. et al. In vitro and in vivo studies of the novel antithrombotic agent BAY 59-7939—an oral, direct factor Xa inhibitor. J. Thromb. Haemost. 3, 514–521 (2005).
Depasse, F. et al. Effect of BAY 59-7939—a novel, oral, direct Factor Xa inhibitor—on clot-bound Factor Xa activity in vitro [abstract]. J. Thromb. Haemost. 3 (Suppl. 1), P1104 (2005).
Kubitza, D., Becka, M., Voith, B., Zuehlsdorf, M. & Wensing, G. Safety, pharmacodynamics, and pharmacokinetics of single doses of BAY 59–7939, an oral, direct factor Xa inhibitor. Clin. Pharmacol. Ther. 78, 412–421 (2005).
Kubitza, D., Becka, M., Wensing, G., Voith, B. & Zuehlsdorf, M. Safety, pharmacodynamics, and pharmacokinetics of BAY 59-7939—an oral, direct factor Xa inhibitor—after multiple dosing in healthy male subjects. Eur. J. Clin. Pharmacol. 61, 873–880 (2005).
Jiang, J. et al. Safety, pharmacokinetics and pharmacodynamics of single doses of rivaroxaban—an oral, direct factor Xa inhibitor—in elderly Chinese subjects. Thromb. Haemost. 103, 234–241 (2010).
Zhao, X. et al. Safety, pharmacokinetics and pharmacodynamics of single/multiple doses of the oral, direct factor Xa inhibitor rivaroxaban in healthy Chinese subjects. Br. J. Clin. Pharmacol. 68, 77–88 (2009).
Stampfuss, J., Kubitza, D., Becka, M. & Mueck, W. The effect of food on the absorption and pharmacokinetics of rivaroxaban. Int. J. Clin. Pharmacol. Ther. 51, 549–561 (2013).
Hori, M. et al. Rivaroxaban vs. warfarin in Japanese patients with atrial fibrillation—the J-ROCKET AF study. Circ. J. 76, 2104–2111 (2012).
Hori, M. et al. Safety and efficacy of adjusted dose of rivaroxaban in Japanese patients with non-valvular atrial fibrillation: subanalysis of J-ROCKET AF for patients with moderate renal impairment. Circ. J. 77, 632–638 (2013).
Lee, M. et al. Low glomerular filtration rate and risk of stroke: meta-analysis. BMJ 341, c4249 (2010).
Alonso, A. et al. Chronic kidney disease is associated with the incidence of atrial fibrillation: the Atherosclerosis Risk in Communities (ARIC) study. Circulation 123, 2946–2953 (2011).
Olesen, J. B. et al. Stroke and bleeding in atrial fibrillation with chronic kidney disease. N. Engl. J. Med. 367, 625–635 (2012).
Lassen, M. R. et al. A phase II randomized, double-blind, five-arm, parallel-group, dose-response study of a new oral directly acting factor Xa inhibitor, razaxaban, for the prevention of deep vein thrombosis in knee replacement surgery (ASH Annual Meeting Abstracts) [abstract 41]. Blood 102, 41 (2003).
Wong, P. C. et al. Razaxaban, a direct factor Xa inhibitor, in combination with aspirin and/or clopidogrel improves low-dose antithrombotic activity without enhancing bleeding liability in rabbits. J. Thromb. Thrombolysis 24, 43–51 (2007).
Wong, P. C. et al. Apixaban, an oral, direct and highly selective factor Xa inhibitor: in vitro, antithrombotic and antihemostatic studies. J. Thromb. Haemost. 6, 820–829 (2008).
Jiang, X., Crain, E. J., Luettgen, J. M., Schumacher, W. A. & Wong, P. C. Apixaban, an oral direct factor Xa inhibitor, inhibits human clot-bound factor Xa activity in vitro. Thromb. Haemost. 101, 780–782 (2009).
Frost, C. et al. Apixaban, a direct factor Xa inhibitor: single-dose pharmacokinetics and pharmacodynamics of an intravenous formulation [abstract 142]. Br. J. Clin. Pharmacol. 48, 1132 (2008).
Frost, C. et al. Apixaban, an oral, direct factor Xa inhibitor: single dose safety, pharmacokinetics, pharmacodynamics and food effect in healthy subjects. Br. J. Clin. Pharmacol. 75, 476–487 (2013).
Vakkalagadda, B. et al. Effect of rifampin on the pharmacokinetics of apixaban, an oral direct inhibitor of factor Xa [abstract 143]. J. Clin. Pharmacol. 49, 1124 (2009).
Easton, J. D. et al. Apixaban compared with warfarin in patients with atrial fibrillation and previous stroke or transient ischaemic attack: a subgroup analysis of the ARISTOTLE trial. Lancet Neurol. 11, 503–511 (2012).
Pisters, R. et al. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest 138, 1093–1100 (2010).
Lopes, R. D. et al. Efficacy and safety of apixaban compared with warfarin according to patient risk of stroke and of bleeding in atrial fibrillation: a secondary analysis of a randomised controlled trial. Lancet 380, 1749–1758 (2012).
Ogawa, S., Shinohara, Y. & Kanmuri, K. Safety and efficacy of the oral direct factor xa inhibitor apixaban in Japanese patients with non-valvular atrial fibrillation. The ARISTOTLE-J study. Circ. J. 75, 1852–1859 (2011).
Connolly, S. J. et al. Apixaban in patients with atrial fibrillation. N. Engl. J. Med. 364, 806–817 (2011).
Hara, T. et al. DX-9065a, a new synthetic, potent anticoagulant and selective inhibitor for factor Xa. Thromb. Haemost. 71, 314–319 (1994).
Fujii, Y. et al. Characteristics of gastrointestinal absorption of DX-9065a, a new synthetic anticoagulant. Drug Metab. Pharmacokinet. 22, 26–32 (2007).
Zafar, M. U. et al. Antithrombotic effects of factor Xa inhibition with DU-176b: phase-I study of an oral, direct factor Xa inhibitor using an ex-vivo flow chamber. Thromb. Haemost. 98, 883–888 (2007).
Furugohri, T. et al. DU-176b, a potent and orally active factor Xa inhibitor: in vitro and in vivo pharmacological profiles. J. Thromb. Haemost. 6, 1542–1549 (2008).
Matsushima, N., Lee, F., Sato, T., Weiss, D. & Mendell, J. Bioavailability and safety of the factor xa inhibitor edoxaban and the effects of quinidine in healthy subjects. Clin. Pharm. Drug Dev. 2, 358 (2013).
Giugliano, R. P. et al. Edoxaban versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 369, 2093–2104 (2013).
Yamashita, T. et al. Randomized, multicenter, warfarin-controlled phase II study of edoxaban in Japanese patients with non-valvular atrial fibrillation. Circ. J. 76, 1840–1847 (2012).
Chung, N. et al. Safety of edoxaban, an oral factor Xa inhibitor, in Asian patients with non-valvular atrial fibrillation. Thromb. Haemost. 105, 535–544 (2011).
Mendell, J., Tachibana, M., Shi, M. & Kunitada, S. Effects of food on the pharmacokinetics of edoxaban, an oral direct factor Xa inhibitor, in healthy volunteers. J. Clin. Pharmacol. 51, 687–694 (2011).
Ahrens, I., Peter, K., Lip, G. Y. & Bode, C. Development and clinical applications of novel oral anticoagulants. Part II. Drugs under clinical investigation. Discov. Med. 13, 445–450 (2012).
Palladino, M., Merli, G. & Thomson, L. Evaluation of the oral direct factor Xa inhibitor—betrixaban. Expert Opin. Investig. Drugs 22, 1465–1472 (2013).
Connolly, S. J. et al. Betrixaban compared with warfarin in patients with atrial fibrillation: results of a phase 2, randomized, dose-ranging study (Explore-Xa). Eur. Heart J. 34, 1498–1505 (2013).
Lu, G. et al. A specific antidote for reversal of anticoagulation by direct and indirect inhibitors of coagulation factor Xa. Nat. Med. 19, 446–451 (2013).
Ansell, J. Blocking bleeding: reversing anticoagulant therapy. Nat. Med. 19, 402–404 (2013).
Dentali, F. et al. Efficacy and safety of the novel oral anticoagulants in atrial fibrillation: a systematic review and meta-analysis of the literature. Circulation 126, 2381–2391 (2011).
Miller, C. S., Grandi, S. M., Shimony, A., Filion, K. B. & Eisenberg, M. J. Meta-analysis of efficacy and safety of new oral anticoagulants (dabigatran, rivaroxaban, apixaban) versus warfarin in patients with atrial fibrillation. Am. J. Cardiol. 110, 453–460 (2012).
Sardar, P. et al. New oral anticoagulants are not superior to warfarin in secondary prevention of stroke or transient ischemic attacks, but lower the risk of intracranial bleeding: insights from a meta-analysis and indirect treatment comparisons. PLoS ONE 8, e77694 (2013).
Capodanno, D., Capranzano, P., Giacchi, G., Calvi, V. & Tamburino, C. Novel oral anticoagulants versus warfarin in non-valvular atrial fibrillation: a meta-analysis of 50,578 patients. Int. J. Cardiol. 167, 1237–1241 (2013).
Bruins Slot, K. M. & Berge, E. Factor Xa inhibitors versus vitamin K antagonists for preventing cerebral or systemic embolism in patients with atrial fibrillation. Cochrane Database of Systematic Reviews 2013, Issue 8. Art. No.: CD008980. http://dx.doi.org/10.1002/14651858.CD008980.pub2.
Rasmussen, L. H., Larsen, T. B., Graungaard, T., Skjoth, F. & Lip, G. Y. Primary and secondary prevention with new oral anticoagulant drugs for stroke prevention in atrial fibrillation: indirect comparison analysis. BMJ 345, e7097 (2012).
Lip, G. Y., Larsen, T. B., Skjoth, F. & Rasmussen, L. H. Indirect comparisons of new oral anticoagulant drugs for efficacy and safety when used for stroke prevention in atrial fibrillation. J. Am. Coll. Cardiol. 60, 738–746 (2012).
Savelieva, I. & Camm, A. J. Practical considerations for using novel oral anticoagulants in patients with atrial fibrillation. Clin. Cardiol. 37, 32–47 (2014).
Wallentin, L. et al. Efficacy and safety of dabigatran compared with warfarin at different levels of international normalised ratio control for stroke prevention in atrial fibrillation: an analysis of the RE-LY trial. Lancet 376, 975–983 (2010).
FDA. FDA Draft Briefing Document for the Cardiovascular and Renal Drugs Advisory Committee (CRDAC) [online], (2011).
Rosendaal, F. R., Cannegieter, S. C., van der Meer, F. J. & Briet, E. A method to determine the optimal intensity of oral anticoagulant therapy. Thromb. Haemost. 69, 236–239 (1993).
You, J. H. Novel oral anticoagulants versus warfarin therapy at various levels of anticoagulation control in atrial fibrillation-a cost-effectiveness analysis. J. Gen. Intern. Med. http://dx.doi.org/10.1007/s11606-013-2639-2.
Ogawa, S. et al. The APHRS's 2013 statement on antithrombotic therapy of patients with nonvalvular atrial fibrillation. J. Arryth. 29, 190–200 (2013).
Group, J. J. Guidelines for pharmacotherapy of atrial fibrillation (JCS2008): digest version. Circ. J. 74, 2479–2500 (2010).
Department of Health, Western Australia. Atrial Fibrillation Working Group. Quick Reference Guide: Atrial Fibrillation Information for the Health Practitioner. Perth: Health Networks Branch [online], (2011).
Author information
Authors and Affiliations
Contributions
I.S., K.K. and J.B. researched data for the article. All authors contributed substantially to the discussion of content. I.S., K.K. and J.B. wrote the manuscript. A.J.C. reviewed/edited the article before submission.
Corresponding author
Ethics declarations
Competing interests
A.J.C has acted as an advisor or consultant for Actelion Pharmaceuticals, ARYx Therapeutics, Bristol-Myers Squibb Company, Cardiome Pharma Corporation, CV Therapeutics, Daiichi Sankyo, Menarini Group, Pfizer, Sanofi, and Xention Limited. He has served as a speaker or a member of the speaker's bureau for Cardiome Pharma Corporation, Daiichi Sankyo, Menarini Group, Pfizer, and Sanofi. He has received grants for clinical research from Bristol-Myers Squibb Company, Daiichi Sankyo, Sanofi, and SERVIER. He has served as a member of the data safety monitoring boards for Bristol-Myers Squibb, Novartis Pharmaceuticals Corporation, SERVIER, and an expert witness for Johnson & Johnson Pharmaceutical Research & Development, Sanofi and SERVIER. The other authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Sabir, I., Khavandi, K., Brownrigg, J. et al. Oral anticoagulants for Asian patients with atrial fibrillation. Nat Rev Cardiol 11, 290–303 (2014). https://doi.org/10.1038/nrcardio.2014.22
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2014.22
This article is cited by
-
Sex-related differences in presentation, treatment, and outcomes of Asian patients with atrial fibrillation: a report from the prospective APHRS-AF Registry
Scientific Reports (2023)
-
Risk of major bleeding and thromboembolism in Asian patients with nonvalvular atrial fibrillation using direct oral anticoagulants versus warfarin
International Journal of Clinical Pharmacy (2022)
-
XaMINA: A Real-World, Prospective, Observational Study of Treatment-Naïve Patients Treated with Rivaroxaban for Stroke Prevention in Atrial Fibrillation in Asia
Advances in Therapy (2022)
-
Changes of antithrombotic prescription in atrial fibrillation patients with acute coronary syndrome or percutaneous coronary intervention and the subsequent impact on long-term outcomes: a longitudinal cohort study
Thrombosis Journal (2021)
-
High incidence of under-treated atrial fibrillation: perspectives from an Asian Stroke Endovascular Thrombectomy Registry
Journal of Thrombosis and Thrombolysis (2020)