Key Points
-
A large volume of epidemiological evidence points to an association between body mass index (BMI) and increased risk of several cancer types. Proposed mechanisms for the adiposity–cancer link need to account for the observed specificities of associations by gender, site, histological subtype and molecular phenotype.
-
Underlying the above associations, three mainly 'hormonal' mechanisms have been proposed: altered sex hormone metabolism; increased insulin levels and bioavailability of insulin-like growth factor I (IGF1); and adipokine pathophysiology. Additionally, newer hypotheses have been suggested, including as systemic inflammation and microbiome effects. These hypotheses generally fail to capture the specificity of associations.
-
Intentional weight loss might lead to changes of obesity-associated intermediary biomarkers, which in turn might indicate causal pathways to the development of obesity-associated cancer. However, there are many inconsistencies, particularly for changes in inflammatory markers and circulating IGF measurements.
-
Ectopic fat deposition is of two main types: systemic (such as visceral adipose tissue) and local (such as breast fat and hepatic steatosis). The concept of local ectopic fat is relatively new in the field of cancer, but it has been implicated in the development of cardiovascular disease. This concept confers specificity of association for cancer risk and could pave the way to more-targeted preventive interventions in the future.
Abstract
Excess body adiposity, commonly expressed as body mass index (BMI), is a risk factor for many common adult cancers. Over the past decade, epidemiological data have shown that adiposity–cancer risk associations are specific for gender, site, geographical population, histological subtype and molecular phenotype. The biological mechanisms underpinning these associations are incompletely understood but need to take account of the specificities observed in epidemiology to better inform future prevention strategies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
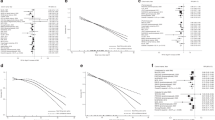
Renehan, A., Tyson, M., Egger, M., Heller, R. F. & Zwahlen, M. Body mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 371, 569–578 (2008). A dose–response meta-analysis standardized across 20 cancer types, demonstrating sex- and site-specific associations between BMI and cancer risk.
World Cancer Research Fund and American Institute for Cancer Research. Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective (AICR, 2007). A series of systematic reviews establishing that body fatness is a risk factor for incidence of several cancer types.
Renehan, A. G. Bariatric surgery, weight reduction and cancer prevention. Lancet Oncol. 10, 640–641 (2009).
Arnold, M. et al. Global burden of cancer attributable to high body-mass index in 2012: a population-based study. Lancet Oncol. 16, 36–46 (2014). An analysis of the global burden of cancer attributable to high BMI. Reports that 3.6% of all new cancers in adults are attributable to high BMI.
Calle, E. E. & Kaaks, R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat. Rev. Cancer 4, 579–591 (2004). A seminal review on obesity and cancer risk, setting down the main biological hypotheses underpinning the link.
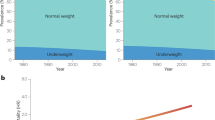
Sperrin, M., Marshall, A. D., Higgins, V., Buchan, I. E. & Renehan, A. G. Slowing down of adult body mass index trend increases in England: a latent class analysis of cross-sectional surveys (1992–2010). Int. J. Obes. 38, 818–824 (2014).
Aune, D. et al. Body mass index, abdominal fatness and pancreatic cancer risk: a systematic review and non-linear dose–response meta-analysis of prospective studies. Ann. Oncol. 23, 843–852 (2012).
Collaborative Group on Epidemiological Studies of Ovarian Cancer. Ovarian cancer and body size: individual participant meta-analysis including 25,157 women with ovarian cancer from 47 epidemiological studies. PLoS Med. 9, e1001200 (2012).
World Cancer Research Fund and American Institute for Cancer Research. Continuous Update Project Report. Food, Nutrition, Physical Activity, and the Prevention of Ovarian Cancer (AICR, 2014).
Larsson, S. C. & Wolk, A. Body mass index and risk of non-Hodgkin's and Hodgkin's lymphoma: a meta-analysis of prospective studies. Eur. J. Cancer 47, 2422–2430 (2011).
Koebnick, C. et al. Body mass index, physical activity, and bladder cancer in a large prospective study. Cancer Epidemiol. Biomarkers Prev. 17, 1214–1221 (2008).
Moore, S. C. et al. Height, body mass index, and physical activity in relation to glioma risk. Cancer Res. 69, 8349–8355 (2009).
Lerro, C. C., McGlynn, K. A. & Cook, M. B. A systematic review and meta-analysis of the relationship between body size and testicular cancer. Br. J. Cancer 103, 1467–1474 (2010).
Bhaskaran, K. et al. Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5.24 million UK adults. Lancet 384, 755–765 (2014).
Freedland, S. J., Giovannucci, E. & Platz, E. A. Are findings from studies of obesity and prostate cancer really in conflict? Cancer Causes Control 17, 5–9 (2006).
Discacciati, A., Orsini, N. & Wolk, A. Body mass index and incidence of localized and advanced prostate cancer — a dose–response meta-analysis of prospective studies. Ann. Oncol. 23, 1665–1671 (2012).
World Cancer Research Fund and American Institute for Cancer Research. Continuous Update Project Report: Diet, Nutrition, Physical Activity, and Prostate Cancer (AICR, 2014).
Coe, P. O., O'Reilly, D. A. & Renehan, A. G. Excess adiposity and gastrointestinal cancer. Br. J. Surg. 101, 1518–1531 (2014).
Keum, N. et al. Adult weight gain and adiposity-related cancers: a dose-response meta-analysis of prospective observational studies. J. Natl Cancer Inst. 107, dju428 (2015).
Smith, L. et al. Body mass index and risk of lung cancer among never, former, and current smokers. J. Natl Cancer Inst. 104, 778–789 (2012).
Steffen, A. et al. Anthropometry and esophageal cancer risk in the European prospective investigation into cancer and nutrition. Cancer Epidemiol. Biomarkers Prev. 18, 2079–2089 (2009).
Gaudet, M. M. et al. Prospective studies of body mass index with head and neck cancer incidence and mortality. Cancer Epidemiol. Biomarkers Prev. 21, 497–503 (2012).
Etemadi, A. et al. A prospective cohort study of body size and risk of head and neck cancers in the NIH-AARP diet and health study. Cancer Epidemiol. Biomarkers Prev. 23, 2422–2429 (2014).
Akbartabartoori, M., Lean, M. E. & Hankey, C. R. Relationships between cigarette smoking, body size and body shape. Int. J. Obes. 29, 236–243 (2005).
Renehan, A. G., Leitzmann, M. F. & Zwahlen, M. Re: body mass index and risk of lung cancer among never, former, and current smokers. J. Natl Cancer Inst. 104, 1680–1681 (2012).
Renehan, A. G. in Handbook of Obesity (eds Bray, G. & Bouchard, C.) 561–572 (Informa Healthcare, 2014).
Crosbie, E. J., Zwahlen, M., Kitchener, H. C., Egger, M. & Renehan, A. G. Body mass index, hormone replacement therapy, and endometrial cancer risk: a meta-analysis. Cancer Epidemiol. Biomarkers Prev. 19, 3119–3130 (2010).
World Cancer Research Fund and American Institute for Cancer Research. Continuous Update Project Report. Food, Nutrition, Physical Activity, and the Prevention of Breast Cancer (AICR, 2010).
Eliassen, A. H. et al. Endogenous steroid hormone concentrations and risk of breast cancer among premenopausal women. J. Natl Cancer Inst. 98, 1406–1415 (2006).
Kaaks, R. et al. Serum sex steroids in premenopausal women and breast cancer risk within the European Prospective Investigation into Cancer and Nutrition (EPIC). J. Natl Cancer Inst. 97, 755–765 (2005).
Renehan, A. G. Obesity and cancer in Asia-Pacific populations. Lancet Oncol. 11, 704–705 (2010).
Huang, Z. et al. Dual effects of weight and weight gain on breast cancer risk. J. Am. Med. Associ. 278, 1407–1411 (1997).
Kaaks, R. et al. Breast-cancer incidence in relation to height, weight and body-fat distribution in the Dutch 'DOM' cohort. Int. J. Cancer 76, 647–651 (1998).
Lahmann, P. H. et al. Body size and breast cancer risk: findings from the European Prospective Investigation into Cancer and Nutrition (EPIC). Int. J. Cancer 111, 762–771 (2004).
Sperrin, M., Marshall, A. D., Higgins, V., Renehan, A. G. & Buchan, I. E. Body mass index relates weight to height differently in women and older adults: serial cross-sectional surveys in England (1992–2011). J. Public Health (Oxf.) fdv067 (2015).
Green, J. et al. Height and cancer incidence in the Million Women Study: prospective cohort, and meta-analysis of prospective studies of height and total cancer risk. Lancet Oncol. 12, 785–794 (2011).
Renehan, A. G. Height and cancer: consistent links, but mechanisms unclear. Lancet Oncol. 12, 716–717 (2011).
Suzuki, R., Orsini, N., Saji, S., Key, T. J. & Wolk, A. Body weight and incidence of breast cancer defined by estrogen and progesterone receptor status — a meta-analysis. Int. J. Cancer 124, 698–712 (2009).
Ahn, J. et al. Adiposity, adult weight change, and postmenopausal breast cancer risk. Arch. Intern. Med. 167, 2091–2102 (2007).
Canchola, A. J. et al. Body size and the risk of postmenopausal breast cancer subtypes in the California Teachers Study cohort. Cancer Causes Control 23, 473–485 (2012).
Harris, H. R., Willett, W. C., Terry, K. L. & Michels, K. B. Body fat distribution and risk of premenopausal breast cancer in the Nurses' Health Study II. J. Natl Cancer Inst. 103, 273–278 (2011).
Ritte, R. et al. Adiposity, hormone replacement therapy use and breast cancer risk by age and hormone receptor status: a large prospective cohort study. Breast Cancer Res. 14, R76 (2012).
Setiawan, V. W. et al. Breast cancer risk factors defined by estrogen and progesterone receptor status: the multiethnic cohort study. Am. J. Epidemiol. 169, 1251–1259 (2009).
Phipps, A. I. et al. Body size, physical activity, and risk of triple-negative and estrogen receptor-positive breast cancer. Cancer Epidemiol. Biomarkers Prev. 20, 454–463 (2011).
Yang, X. R. et al. Associations of breast cancer risk factors with tumor subtypes: a pooled analysis from the Breast Cancer Association Consortium studies. J. Natl Cancer Inst. 103, 250–263 (2011).
Feigelson, H. S. et al. Adult weight gain and histopathologic characteristics of breast cancer among postmenopausal women. Cancer 107, 12–21 (2006).
Palmer, J. R., Adams-Campbell, L. L., Boggs, D. A., Wise, L. A. & Rosenberg, L. A prospective study of body size and breast cancer in black women. Cancer Epidemiol. Biomarkers Prev. 16, 1795–1802 (2007).
Potter, J. D. et al. Progesterone and estrogen receptors and mammary neoplasia in the Iowa Women's Health Study: how many kinds of breast cancer are there? Cancer Epidemiol. Biomarkers Prev. 4, 319–326 (1995).
Suzuki, R., Rylander-Rudqvist, T., Ye, W., Saji, S. & Wolk, A. Body weight and postmenopausal breast cancer risk defined by estrogen and progesterone receptor status among Swedish women: a prospective cohort study. Int. J. Cancer 119, 1683–1689 (2006).
Allred, D. C., Brown, P. & Medina, D. The origins of estrogen receptor α-positive and estrogen receptor α-negative human breast cancer. Breast Cancer Res. 6, 240–245 (2004).
Asselin-Labat, M. L. et al. Control of mammary stem cell function by steroid hormone signalling. Nature 465, 798–802 (2010).
Bokhman, J. V. Two pathogenetic types of endometrial carcinoma. Gynecol. Oncol. 15, 10–17 (1983).
Setiawan, V. W. et al. Type I and II endometrial cancers: have they different risk factors? J. Clin. Oncol. 31, 2607–2618 (2013).
Olsen, C. M. et al. Obesity and risk of ovarian cancer subtypes: evidence from the Ovarian Cancer Association Consortium. Endocr. Relat. Cancer 20, 251–262 (2013).
Campbell, P. T. et al. Case-control study of overweight, obesity, and colorectal cancer risk, overall and by tumor microsatellite instability status. J. Natl Cancer Inst. 102, 391–400 (2010).
Satia, J. A. et al. Diet, lifestyle, and genomic instability in the North Carolina Colon Cancer Study. Cancer Epidemiol. Biomarkers Prev. 14, 429–436 (2005).
Slattery, M. L. et al. Associations between cigarette smoking, lifestyle factors, and microsatellite instability in colon tumors. J. Natl Cancer Inst. 92, 1831–1836 (2000).
Hughes, L. A. et al. Body size and risk for colorectal cancers showing BRAF mutations or microsatellite instability: a pooled analysis. Int. J. Epidemiol. 41, 1060–1072 (2012).
Kuchiba, A. et al. Body mass index and risk of colorectal cancer according to fatty acid synthase expression in the nurses' health study. J. Natl Cancer Inst. 104, 415–420 (2012).
Morikawa, T. et al. Prospective analysis of body mass index, physical activity, and colorectal cancer risk associated with β-catenin (CTNNB1) status. Cancer Res. 73, 1600–1610 (2013).
Khandekar, M. J., Cohen, P. & Spiegelman, B. M. Molecular mechanisms of cancer development in obesity. Nat. Rev. Cancer 11, 886–895 (2011).
Roberts, D. L., Dive, C. & Renehan, A. G. Biological mechanisms linking obesity and cancer risk: new perspectives. Annu. Rev. Med. 61, 301–316 (2010).
van Kruijsdijk, R. C., van der Wall, E. & Visseren, F. L. Obesity and cancer: the role of dysfunctional adipose tissue. Cancer Epidemiol. Biomarkers Prev. 18, 2569–2578 (2009).
Renehan, A. G. in Clinical Endocrine Oncology (eds Hay, I. D. & Wass, J. A. H.) 32–40 (Oxford Univ. Press, 2008).
Travis, R. C. & Key, T. J. Oestrogen exposure and breast cancer risk. Breast Cancer Res. 5, 239–247 (2003).
Key, T. J. et al. Body mass index, serum sex hormones, and breast cancer risk in postmenopausal women. J. Natl Cancer Inst. 95, 1218–1226 (2003). A large pooled analysis that indicates that the association between elevated BMI and postmenopausal breast cancer is, in part, mediated through circulating sex hormones.
Kaaks, R. et al. Postmenopausal serum androgens, oestrogens and breast cancer risk: the European prospective investigation into cancer and nutrition. Endocr. Relat. Cancer. 12, 1071–1082 (2005). A large-scale European study confirming that the association between elevated BMI and postmenopausal breast cancer is, in part, mediated through circulating sex hormones.
Derby, C. A., Zilber, S., Brambilla, D., Morales, K. H. & McKinlay, J. B. Body mass index, waist circumference and waist to hip ratio and change in sex steroid hormones: the Massachusetts Male Ageing Study. Clin. Endocrinol. 65, 125–131 (2006).
Kaaks, R., Lukanova, A. & Kurzer, M. S. Obesity, endogenous hormones, and endometrial cancer risk: a synthetic review. Cancer Epidemiol. Biomarkers Prev. 11, 1531–1543 (2002).
Giovannucci, E. & Michaud, D. The role of obesity and related metabolic disturbances in cancers of the colon, prostate, and pancreas. Gastroenterology 132, 2208–2225 (2007).
Thompson, I. M. et al. The influence of finasteride on the development of prostate cancer. N. Engl. J. Med. 349, 215–224 (2003).
Platz, E. A. et al. Sex steroid hormones and the androgen receptor gene CAG repeat and subsequent risk of prostate cancer in the prostate-specific antigen era. Cancer Epidemiol. Biomarkers Prev. 14, 1262–1269 (2005).
Severi, G. et al. Circulating steroid hormones and the risk of prostate cancer. Cancer Epidemiol. Biomarkers Prev. 15, 86–91 (2006).
Vona-Davis, L. & Rose, D. P. Adipokines as endocrine, paracrine, and autocrine factors in breast cancer risk and progression. Endocr. Relat. Cancer 14, 189–206 (2007).
Dirat, B., Bochet, L., Escourrou, G., Valet, P. & Muller, C. Unraveling the obesity and breast cancer links: a role for cancer-associated adipocytes? Endocr. Dev. 19, 45–52 (2010).
Muller, C. Tumour-surrounding adipocytes are active players in breast cancer progression. Ann. Endocrinol. 74, 108–110 (2013).
Chlebowski, R. T. et al. Estrogen plus progestin and colorectal cancer in postmenopausal women. N. Engl. J. Med. 350, 991–1004 (2004).
McKeown-Eyssen, G. Epidemiology of colorectal cancer revisited: are serum triglycerides and/or plasma glucose associated with risk? Cancer Epidemiol. Biomarkers Prev. 3, 687–695 (1994).
Giovannucci, E. Insulin and colon cancer. Cancer Causes Control 6, 164–179 (1995).
Pollak, M. The insulin and insulin-like growth factor receptor family in neoplasia: an update. Nat. Rev. Cancer 12, 159–169 (2012). An updated review detailing the complexities of the IGF system and its potential links with cancer development and cancer treatment.
Renehan, A. G. et al. Insulin-like growth factor (IGF)-I, IGF binding protein-3, and cancer risk: systematic review and meta-regression analysis. Lancet 363, 1346–1353 (2004). First overview dose–response meta-analysis evaluating the relationships between circulating IGFs and cancer risk.
Clayton, P. E., Banerjee, I., Murray, P. G. & Renehan, A. G. Growth hormone, the insulin-like growth factor axis, insulin and cancer risk. Nat. Rev. Endocrinol. 7, 11–24 (2011).
Xiang, A. H., Watanabe, R. M. & Buchanan, T. A. HOMA and Matsuda indices of insulin sensitivity: poor correlation with minimal model-based estimates of insulin sensitivity in longitudinal settings. Diabetologia 57, 334–338 (2014).
Zhou, X. H. et al. Diabetes, prediabetes and cancer mortality. Diabetologia 53, 1867–1876 (2010).
LeRoith, D. Can endogenous hyperinsulinaemia explain the increased risk of cancer development and mortality in type 2 diabetes: evidence from mouse models. Diabetes Metab. Res. Rev. 26, 599–601 (2010).
Badrick, E. & Renehan, A. G. Diabetes and cancer: 5 years into the recent controversy. Eur. J. Cancer 50, 2119–2125 (2014).
Bordeleau, L. et al. The association of basal insulin glargine and/or n-3 fatty acids with incident cancers in patients with dysglycemia. Diabetes Care 37, 1360–1366 (2014).
Renehan, A. G., Frystyk, J. & Flyvbjerg, A. Obesity and cancer risk: the role of the insulin-IGF axis. Trends Endocrinol. Metab. 17, 328–336 (2006).
Tsilidis, K. K., Papatheodorou, S. I., Evangelou, E. & Ioannidis, J. P. Evaluation of excess statistical significance in meta-analyses of 98 biomarker associations with cancer risk. J. Natl Cancer Inst. 104, 1867–1878 (2012).
Harvie, M. et al. Increase in serum total IGF-I and maintenance of free IGF-I levels following intentional weight loss in pre-menopausal women at increased risk of breast cancer. Open Obes. J. [online] (2010).
Fischer-Posovszky, P., Wabitsch, M. & Hochberg, Z. Endocrinology of adipose tissue — an update. Horm. Metab. Res. 39, 314–321 (2007).
Schaffler, A., Scholmerich, J. & Buechler, C. Mechanisms of disease: adipokines and breast cancer — endocrine and paracrine mechanisms that connect adiposity and breast cancer. Nat. Clin. Pract. Endocrinol. Metab. 3, 345–354 (2007).
Bray, G. A. The underlying basis for obesity: relationship to cancer. J. Nutr. 132, 3451S–3455S (2002).
Rose, D. P., Komninou, D. & Stephenson, G. D. Obesity, adipocytokines, and insulin resistance in breast cancer. Obes Rev. 5, 153–165 (2004).
Vansaun, M. N. Molecular pathways: adiponectin and leptin signaling in cancer. Clin. Cancer Res. 19, 1926–1932 (2013).
Renehan, A. G., Roberts, D. L. & Dive, C. Obesity and cancer: pathophysiological and biological mechanisms. Arch. Physiol. Biochem. 114, 71–83 (2008).
Gialamas, S. P. et al. Circulating leptin levels and risk of colorectal cancer and adenoma: a case-control study and meta-analysis. Cancer Causes Control 24, 2129–2141 (2013).
Fasshauer, M., Klein, J., Neumann, S., Eszlinger, M. & Paschke, R. Hormonal regulation of adiponectin gene expression in 3T3-L1 adipocytes. Biochem. Biophys. Res. Commun. 290, 1084–1089 (2002).
Cnop, M. et al. Relationship of adiponectin to body fat distribution, insulin sensitivity and plasma lipoproteins: evidence for independent roles of age and sex. Diabetologia 46, 459–469 (2003).
Dalamaga, M., Diakopoulos, K. N. & Mantzoros, C. S. The role of adiponectin in cancer: a review of current evidence. Endocr. Rev. 33, 547–594 (2012).
Hotamisligil, G. S. & Erbay, E. Nutrient sensing and inflammation in metabolic diseases. Nat. Rev. Immunol. 8, 923–934 (2008).
Osborn, O. & Olefsky, J. M. The cellular and signaling networks linking the immune system and metabolism in disease. Nat. Med. 18, 363–374 (2012).
Weisberg, S. P. et al. Obesity is associated with macrophage accumulation in adipose tissue. J. Clin. Invest. 112, 1796–1808 (2003).
Erlinger, T. P., Platz, E. A., Rifai, N. & Helzlsouer, K. J. C-reactive protein and the risk of incident colorectal cancer. JAMA 291, 585–590 (2004).
Tsilidis, K. K. et al. C-reactive protein and colorectal cancer risk: a systematic review of prospective studies. Int. J. Cancer 123, 1133–1140 (2008).
Chan, A. T., Ogino, S., Giovannucci, E. L. & Fuchs, C. S. Inflammatory markers are associated with risk of colorectal cancer and chemopreventive response to anti-inflammatory drugs. Gastroenterology 140, 799–808 (2011).
Aleksandrova, K. et al. Circulating C-reactive protein concentrations and risks of colon and rectal cancer: a nested case-control study within the European Prospective Investigation into Cancer and Nutrition. Am. J. Epidemiol. 172, 407–418 (2010).
Song, M. et al. A prospective study of plasma inflammatory markers and risk of colorectal cancer in men. Br. J. Cancer 108, 1891–1898 (2013).
Dieudonne, M. N. et al. Adiponectin mediates antiproliferative and apoptotic responses in human MCF7 breast cancer cells. Biochem. Biophys. Res. Commun. 345, 271–279 (2006).
Hursting, S. D., Nunez, N. P., Varticovski, L. & Vinson, C. The obesity–cancer link: lessons learned from a fatless mouse. Cancer Res. 67, 2391–2393 (2007).
Brenner, D. R. et al. A review of the application of inflammatory biomarkers in epidemiologic cancer research. Cancer Epidemiol. Biomarkers Prev. 23, 1729–1751 (2014).
Byers, T. & Sedjo, R. L. Does intentional weight loss reduce cancer risk? Diabetes Obes. Metab. 13, 1063–1072 (2011). A comprehensive review of the effects of weight-losing interventions on cancer-related intermediary biomarkers. Importantly, the review ranks the relative biomarker changes per 10% weight reduction.
Mason, C. et al. Effects of dietary weight loss and exercise on insulin-like growth factor-I and insulin-like growth factor-binding protein-3 in postmenopausal women: a randomized controlled trial. Cancer Epidemiol. Biomarkers Prev. 22, 1457–1463 (2013).
Balagopal, P. B. et al. Nontraditional risk factors and biomarkers for cardiovascular disease: mechanistic, research, and clinical considerations for youth: a scientific statement from the American Heart Association. Circulation 123, 2749–2769 (2011).
Canoy, D. et al. Body fat distribution and risk of coronary heart disease in men and women in the European Prospective Investigation Into Cancer and Nutrition in Norfolk cohort: a population-based prospective study. Circulation 116, 2933–2943 (2007). One of only a few large-scale studies to evaluate the associations between hip and gluteal fat distribution and risk of a common metabolic disease, coronary heart disease.
Stefan, N., Haring, H. U., Hu, F. B. & Schulze, M. B. Metabolically healthy obesity: epidemiology, mechanisms, and clinical implications. Lancet Diabetes Endocrinol. 1, 152–162 (2013).
Moore, L. L., Chadid, S., Singer, M. R., Kreger, B. E. & Denis, G. V. Metabolic health reduces risk of obesity-related cancer in framingham study adults. Cancer Epidemiol. Biomarkers Prev. 23, 2057–2065 (2014).
Britton, K. A. & Fox, C. S. Ectopic fat depots and cardiovascular disease. Circulation 124, e837–841 (2011). A seminal overview introducing the concepts of ectopic fat and metabolic disease predisposition.
Cornier, M. A. et al. Assessing adiposity: a scientific statement from the American Heart Association. Circulation 124, 1996–2019 (2011).
Ouchi, N., Parker, J. L., Lugus, J. J. & Walsh, K. Adipokines in inflammation and metabolic disease. Nat. Rev. Immunol. 11, 85–97 (2011).
Fabbrini, E. et al. Intrahepatic fat, not visceral fat, is linked with metabolic complications of obesity. Proc. Natl Acad. Sci. USA 106, 15430–15435 (2009).
Kahn, B. B. & Flier, J. S. Obesity and insulin resistance. J. Clin. Invest. 106, 473–481 (2000).
Aleksandrova, K., Nimptsch, K. & Pischon, T. Obesity and colorectal cancer. Front. Biosci. (Elite Ed.) 5, 61–77 (2013).
Moore, L. L. et al. BMI and waist circumference as predictors of lifetime colon cancer risk in Framingham Study adults. Int. J. Obes. Relat. Metab. Disord. 28, 559–567 (2004).
Pischon, T. et al. Body size and risk of colon and rectal cancer in the European Prospective Investigation Into Cancer and Nutrition (EPIC). J. Natl Cancer Inst. 98, 920–931 (2006). One of the first large-scale studies to suggest that indices of central adiposity, such as waist circumference, may be more informative than BMI in the prediction of cancer risk.
Folsom, A. R. et al. Associations of general and abdominal obesity with multiple health outcomes in older women: the Iowa Women's Health Study. Arch. Intern. Med. 160, 2117–2128 (2000).
Keimling, M. et al. Comparison of associations of body mass index, abdominal adiposity, and risk of colorectal cancer in a large prospective cohort study. Cancer Epidemiol. Biomarkers Prev. 22, 1383–1394 (2013). A large study directly comparing the associations of waist circumference versus BMI and colorectal cancer risk, and challenging the notion that there are differences in the strengths of these different associations.
Oxentenko, A. S. et al. Body size and incident colorectal cancer: a prospective study of older women. Cancer Prev. Res. 3, 1608–1620 (2010).
Gaudet, M. M. et al. Waist circumference, body mass index, and postmenopausal breast cancer incidence in the Cancer Prevention Study-II Nutrition Cohort. Cancer Causes Control 25, 737–745 (2014).
Huang, Z. et al. Waist circumference, waist:hip ratio, and risk of breast cancer in the Nurses' Health Study. Am. J. Epidemiol. 150, 1316–1324 (1999).
World Cancer Research Fund and American Institute for Cancer Research. Continuous Update Project Report. Food, Nutrition, Physical Activity, and the Prevention of Pancreatic Cancer. (AICR, 2012).
World Cancer Research Fund and American Institute for Cancer Research. Continuous Update Project Report. Food, Nutrition, Physical Activity, and the Prevention of Endometrial Cancer. (AICR, 2013).
Greenstein, A. S. et al. Local inflammation and hypoxia abolish the protective anticontractile properties of perivascular fat in obese patients. Circulation 119, 1661–1670 (2009).
Fox, C. S. et al. Periaortic fat deposition is associated with peripheral arterial disease: the Framingham heart study. Circ. Cardiovasc. Imag. 3, 515–519 (2010).
Schautz, B., Later, W., Heller, M., Muller, M. J. & Bosy-Westphal, A. Associations between breast adipose tissue, body fat distribution and cardiometabolic risk in women: cross-sectional data and weight-loss intervention. Eur. J. Clin. Nutr. 65, 784–790 (2011).
Martinez-Outschoorn, U. E., Sotgia, F. & Lisanti, M. P. Caveolae and signalling in cancer. Nat. Rev. Cancer 15, 225–237 (2015).
Park, J., Morley, T. S., Kim, M., Clegg, D. J. & Scherer, P. E. Obesity and cancer — mechanisms underlying tumour progression and recurrence. Nat. Rev. Endocrinol. 10, 455–465 (2014).
Stienstra, R. et al. Inflammasome is a central player in the induction of obesity and insulin resistance. Proc. Natl Acad. Sci. USA 108, 15324–15329 (2011).
Stefan, N., Kantartzis, K. & Haring, H. U. Causes and metabolic consequences of fatty liver. Endocr. Rev. 29, 939–960 (2008). A comprehensive review detailing the importance of fat deposition in the liver as a determinant of insulin resistance.
Tacke, F., Luedde, T. & Trautwein, C. Inflammatory pathways in liver homeostasis and liver injury. Clin. Rev. Allergy Immunol. 36, 4–12 (2009).
Park, E. J. et al. Dietary and genetic obesity promote liver inflammation and tumorigenesis by enhancing IL-6 and TNF expression. Cell 140, 197–208 (2010). A seminal biological paper of a diet-induced hepatocellular carcinoma model in mice, identifying the key role of inflammatory mediators.
Wang, Y., Ausman, L. M., Greenberg, A. S., Russell, R. M. & Wang, X. D. Nonalcoholic steatohepatitis induced by a high-fat diet promotes diethylnitrosamine-initiated early hepatocarcinogenesis in rats. Int. J. Cancer 124, 540–546 (2009).
Michelotti, G. A., Machado, M. V. & Diehl, A. M. NAFLD, NASH and liver cancer. Nat. Rev. Gastroenterol. Hepatol. 10, 656–665 (2013).
Hart, C. L., Morrison, D. S., Batty, G. D., Mitchell, R. J. & Davey Smith, G. Effect of body mass index and alcohol consumption on liver disease: analysis of data from two prospective cohort studies. BMJ 340, c1240 (2010). A key paper demonstrating the complex interactions between risk factors for liver disease and mortality, including cancer-related mortality.
Sijens, P. E., Edens, M. A., Bakker, S. J. & Stolk, R. P. MRI-determined fat content of human liver, pancreas and kidney. World J. Gastroenterol. 16, 1993–1998 (2010).
Lashinger, L. M. et al. Genetic reduction of insulin-like growth factor-1 mimics the anticancer effects of calorie restriction on cyclooxygenase-2-driven pancreatic neoplasia. Cancer Prev. Res. 4, 1030–1040 (2011).
Hori, M. et al. Association of pancreatic Fatty infiltration with pancreatic ductal adenocarcinoma. Clin. Transl. Gastroenterol. 5, e53 (2014).
Bertolini, F., Petit, J. Y. & Kolonin, M. G. Stem cells from adipose tissue and breast cancer: hype, risks and hope. Br. J. Cancer 112, 419–423 (2015). A review of innovative thinking on the interplay between stem cells, adipose tissue and cancer development.
Tremaroli, V. & Backhed, F. Functional interactions between the gut microbiota and host metabolism. Nature 489, 242–249 (2012).
Schulz, M. D. et al. High-fat-diet-mediated dysbiosis promotes intestinal carcinogenesis independently of obesity. Nature 514, 508–512 (2014).
Ohtani, N. Microbiome and cancer. Semin. Immunopathol. 37, 65–72 (2015).
Thanassoulis, G. et al. Prevalence, distribution, and risk factor correlates of high pericardial and intrathoracic fat depots in the Framingham heart study. Circ. Cardiovasc. Imag. 3, 559–566 (2010).
Hernan, M. A., Hernandez-Diaz, S. & Robins, J. M. A structural approach to selection bias. Epidemiology 15, 615–625 (2004). A key paper detailing the ways in which epidemiological studies can infer causality.
Hernan, M. A. & Robins, J. M. Instruments for causal inference: an epidemiologist's dream? Epidemiology 17, 360–372 (2006).
Smith, G. D. & Ebrahim, S. Mendelian randomization: prospects, potentials, and limitations. Int. J. Epidemiol. 33, 30–42 (2004).
Smith, G. D., Timpson, N. & Ebrahim, S. Strengthening causal inference in cardiovascular epidemiology through Mendelian randomization. Ann. Med. 40, 524–541 (2008).
Kilpelainen, T. O. et al. Genetic variation near IRS1 associates with reduced adiposity and an impaired metabolic profile. Nat. Genet. 43, 753–760 (2011).
Speliotes, E. K. et al. Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat. Genet. 42, 937–948 (2010).
Tao, M. H. et al. Polymorphisms in the CYP19A1 (aromatase) gene and endometrial cancer risk in Chinese women. Cancer Epidemiol. Biomarkers Prev. 16, 943–949 (2007).
Wen, W. et al. The modifying effect of C-reactive protein gene polymorphisms on the association between central obesity and endometrial cancer risk. Cancer 112, 2409–2416 (2008).
Lurie, G. et al. The obesity-associated polymorphisms FTO rs9939609 and MC4R rs17782313 and endometrial cancer risk in non-Hispanic white women. PLoS ONE 6, e16756 (2011).
Lewis, S. J. et al. Associations between an obesity related genetic variant (FTO rs9939609) and prostate cancer risk. PLoS ONE 5, e13485 (2010).
Tenesa, A. et al. Common genetic variants at the MC4R locus are associated with obesity, but not with dietary energy intake or colorectal cancer in the Scottish population. Int. J. Obes. 33, 284–288 (2009).
Sainz, J. et al. GWAS-identified common variants for obesity are not associated with the risk of developing colorectal cancer. Cancer Epidemiol. Biomarkers Prev. 23, 1125–1128 (2014).
Bellamy, S. L., Lin, J. Y. & Ten Have, T. R. An introduction to causal modeling in clinical trials. Clin. Trials 4, 58–73 (2007).
Dossus, L. et al. Hormonal, metabolic, and inflammatory profiles and endometrial cancer risk within the EPIC Cohort — a factor analysis. Am. J. Epidemiol. 177, 787–799 (2013). A multi-compartment analysis exploring new aetiological pathways linking adiposity and cancer risk. Notably, the study ranks the relative importance of the tested pathways.
Nead, K. T. et al. Evidence of a causal association between insulinemia and endometrial cancer: a Mendelian randomization analysis. J. Natl Cancer Inst. 107, djv178 (2015).
Acknowledgements
The authors acknowledge the many colleagues and other researchers around the world who have shared with them, over many years, their thoughts, experiences and methodological insights into the details and concepts described in this Review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Related links
FURTHER INFORMATION
Supplementary information
41568_2015_BFnrc3967_MOESM207_ESM.pdf
Supplementary information S1 (table) | Summary of findings from epidemiological studies (2006 to 2012) that report associations between serum adiponectin levels and risk of different types of cancer, condensed from Dalamaga et al. review.1 (PDF 74 kb)
Glossary
- Body mass index
-
(BMI). An anthropometric measure of body adiposity defined as the body mass (in kilograms) divided by the square of the body height (in metres).
- Intermediary biomarkers
-
Biomarkers that predict the development of a disease and thought to be on the causal pathway to the development of that disease.
- Sex hormone
-
A family of hormones that share a basic chemical (steroidal) structure. These hormones include androgens, oestrogens and progesterone, and they have important effects on sexual development and reproductive functions.
- Bioavailability
-
The proportion of a substance that can be used physiologically by target tissues.
- Cohort studies
-
Studies in which a group of individuals is investigated prospectively over time. This is the preferred epidemiological study method for evaluating anthropometric measures and cancer risk.
- Relative risk
-
The risk of cancer (or other disease) in a group of exposed persons divided by the risk in a group of unexposed persons. Relative risk is a commonly used measure of association in epidemiological studies.
- Effect modification
-
Also known as effect interaction. When the association of an exposure with the risk of disease differs in the presence of another exposure.
- Anthropometric measures
-
Measurements of the size or proportions of the human body: for example, weight, height and waist circumference.
- Summary risk estimates
-
The weighted summations of collections of study-level risks derived from meta-analyses of studies. These estimates are typically reported as risk or point estimates with 95% confidence intervals.
- Confounding
-
The association or lack of association with an exposure that is actually due to another factor that determines the occurrence of a disease but that is also associated with the exposure.
- Anovulation
-
A menstrual cycle that is not accompanied by the discharge of an egg from the ovary.
- Attributable risk
-
In epidemiology, this is the difference in the rate of a condition between an exposed population and an unexposed population.
- Peripheral adipose tissue
-
Fat stores other than intra-abdominal fat (mainly subcutaneous fat).
- Hyperinsulinaemia
-
A pathophysiological state characterized by elevated levels of insulin in the circulation.
- Reporting bias
-
A scenario in which investigators fail to report outcomes in studies, often because these associations are not significant.
- Visceral adipose tissue
-
(VAT). Adipose tissue arising in the abdominal cavity — namely, the omentum, mesenteric and retro-peritoneal fat stores — but excluding within-viscera fat, such as intrahepatic and intrapancreatic fat.
- Biomarkers
-
Characteristics that are objectively measured and evaluated as indicators of normal biological processes, pathogenic processes or pharmacological responses to a therapeutic intervention.
- Central adiposity
-
The storage of adipose tissue preferentially in adipocytes within the trunk rather than the extremities.
- Steatosis
-
The accumulation of intracellular fats, mainly triglycerides. Used typically to describe fat deposition within the liver (hepatic steatosis) but may equally apply to fat accumulation in other organs.
- White adipose tissue
-
(WAT). A type of body fat. Mammals have three types of body fat: white, brown and beige. The main function of WAT is metabolism.
- Bias
-
A systematic deviation of a result from a true value.
- Structural equation modelling
-
A family of statistical modelling techniques that combine latent variables through regression equations.
Rights and permissions
About this article
Cite this article
Renehan, A., Zwahlen, M. & Egger, M. Adiposity and cancer risk: new mechanistic insights from epidemiology. Nat Rev Cancer 15, 484–498 (2015). https://doi.org/10.1038/nrc3967
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrc3967
This article is cited by
-
Systemic inflammation and insulin resistance-related indicator predicts poor outcome in patients with cancer cachexia
Cancer & Metabolism (2024)
-
Adipo-oncology: adipocyte-derived factors govern engraftment, survival, and progression of metastatic cancers
Cell Communication and Signaling (2024)
-
Body composition and cancer survival: a narrative review
British Journal of Cancer (2024)
-
Body mass index, triglyceride-glucose index, and prostate cancer death: a mediation analysis in eight European cohorts
British Journal of Cancer (2024)
-
Trajectories of body mass index in adulthood and risk of subtypes of postmenopausal breast cancer
Breast Cancer Research (2023)