Key Points
-
Cervical cancer is potentially a completely preventable disease
-
The licensed vaccines are safe and highly effective against the most common human papillomavirus (HPV) types found in cervical and other anogenital cancers and are likely to prevent HPV+ oropharyngeal cancers
-
Implementation of HPV vaccination is lagging where it is most needed: in the poorest and most at-risk communities that lack screening programmes and have the highest rates of HIV
-
Local production of biosimilar HPV vaccines is progressing, especially in China, but acceptance of virological end points and/or immunological non-inferiority by regulators could speed access
-
The current HPV vaccines do not cover all oncogenic types, and efforts are underway to increase the breadth of protection, including targeting of L2
-
HPV vaccination affects the cost and benefits of screening by reducing the prevalence of high-grade intraepithelial neoplasia associated with vaccine-targeted types
-
Effective communication to policymakers, physicians, patients and their families of the safety and benefits of HPV vaccination is critical to promote global implementation and fully realize the potential for prevention of cervical and other HPV-related cancers
-
In current populations with a high prevalence of HPV, the application of mathematical modelling is critical to optimize cervical cancer prevention and to balance the use of limited public resources for both HPV vaccination and screening programmes
Abstract
The discovery of genotype 16 as the prototype oncogenic human papillomavirus (HPV) initiated a quarter century of laboratory and epidemiological studies that demonstrated their necessary, but not sufficient, aetiological role in cervical and several other anogenital and oropharyngeal cancers. Early virus-induced immune deviation can lead to persistent subclinical infection that brings the risk of progression to cancer. Effective secondary prevention of cervical cancer through cytological and/or HPV screening depends on regular and widespread use in the general population, but coverage is inadequate in low-resource settings. The discovery that the major capsid antigen L1 could self-assemble into empty virus-like particles (VLPs) that are both highly immunogenic and protective led to the licensure of several prophylactic VLP-based HPV vaccines for the prevention of cervical cancer. The implementation of vaccination programmes in adolescent females is underway in many countries, but their impact critically depends on the population coverage and is improved by herd immunity. This Review considers how our expanding knowledge of the virology and immunology of HPV infection can be exploited to improve vaccine technologies and delivery of such preventive strategies to maximize reductions in HPV-associated disease, including incorporation of an HPV vaccine covering oncogenic types within a standard multitarget paediatric vaccine.
Similar content being viewed by others
Introduction
High-risk human papillomavirus (hrHPV) is an established carcinogen in the cervix, penis, vulva, vagina, anus and oropharynx1. Approximately 5% of all cancers can be attributed to HPV, but the fraction linked to HPV varies markedly by geographical region and level of economic development. Worldwide, almost all 530,000 cases per annum of cervical cancer are HPV-driven. HPV-associated cancer of five other sites accounts for a further 113,400 cases2,3. Persistence of hrHPV infection is the main factor driving dysplasia and increased risk of cancer development4. In the absence of intervention, the risk of cervical cancer rises with increasing dysplasia to around 50% in women with high-grade cervical intraepithelial neoplasia (CIN3)5. The worldwide prevalence of HPV infection in women without cervical lesions is 11.7%, with higher rates in Latin America, Eastern Europe and sub-Saharan Africa2. Successful prophylactic vaccination against hrHPV types can prevent dysplasia and thus cervical cancer4. Prevention of hrHPV infection is also important for men as it also causes anogenital and oropharyngeal cancer in both sexes, as well as penile cancer6,7. Immunosuppressed individuals are also at higher risk of HPV-associated cancers8,9.
Extensive virological and epidemiological studies provide an understanding of the natural history of HPV and carcinogenesis and reveal opportunities to harness the host immune response to prevent and/or treat HPV disease. This Review focuses on the development and impact of current HPV prophylactic vaccines and the prospects for continued improvements for maximal cancer control, although recent clinical data provide early signs that therapeutic approaches can increase clearance rates of existing infection and disease, suggesting additional opportunities to more quickly reduce HPV-associated cancer rates10,11.
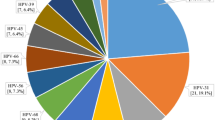
Oncogenic HPV genotypes
Papilloma viruses have an ∼8 kb, histone-bound, double-stranded DNA genome encoding six early genes (E1, E2, E4, E5, E6 and E7) and two late genes (L1 and L2) that produce its non-enveloped T = 7d capsid12. HPVs are characterized by genotype, defined as >10% L1 DNA sequence divergence from other known genotypes (generally termed 'types'), and numbered in order of discovery13. More than 200 HPV types have been identified thus far14. The HPV types within the β-species and γ-species are typically benign and infect skin15,16. Infection may be clinically unapparent or produce cutaneous warts that generally resolve within a year but can be recalcitrant, especially in immunosuppressed patients9. The α-species includes ∼40 HPV types that are trophic for genital mucosa and spread by sexual intercourse. Many αHPV types produce benign disease, for example, genital warts caused by HPV-6 and HPV-11. However, there are 13 hrHPV types, HPV-16, HPV-18, HPV-31, HPV-33, HPV-35, HPV-39, HPV-45, HPV-51, HPV-52, HPV-56, HPV-58, HPV-59 and HPV-68, defined as carcinogenic or probably carcinogenic, plus a group of possibly carcinogenic types (HPV-26, HPV-30, HPV-34, HPV-53, HPV-66, HPV-67, HPV-69, HPV-70, HPV-73, HPV-82 and HPV-85)1,17. Ninety-nine per cent of cervical cancers contain HPV18, with HPV-16 accounting for 50–60% and HPV-18 accounting for ∼20%, and the remaining fraction is caused by the other oncogenic types in the α7, α9 and, to a lesser extent, the α5, α6 and α11 species17. Therefore, all licensed HPV vaccines directly target HPV-16 and HPV-18, but the most recently approved vaccine also targets the next five most common types in cervical cancer (HPV-31, HPV-33, HPV-45, HPV-52 and HPV-58) and the two low-risk types most prevalent in genital warts (HPV-6 and HPV-11).
HPV infection in the cervix
HPV infection typically occurs at a site of epithelial abrasion, and the squamocolumnar junction of the cervix is particularly susceptible to transformation by hrHPV19. Infection is localized to a few cells surrounding the wound and is not lytic. Rather, infection is stealthy and durable. The life cycle of the virus is completely dependent on the differentiation of the epithelium and does not cause cell death, and there is no systemic viraemia20 (Fig. 1).
Abrasion, which leads to denudation of the basement membrane (BM) from epithelial cells, provides access to the basal keratinocytes. During the course of human papillomavirus (HPV) infection, the virus binds to heparin sulfate proteoglycans (HSPGs) and/or laminin 5 on the BM through the major capsid protein L1 (Refs 95,149,150,151). This triggers conformational changes in the capsid that further expose the minor capsid protein L2, including a conserved site on the L2 amino terminus that is susceptible to cleavage by extracellular furin152,153. Furin cleavage of L2 reveals several conserved protective epitopes of L2, including residues 17–36, on the capsid surface154 and is critical to infection. This is followed by virus uptake into the target basal keratinocyte155. Several uptake pathways have been implicated, none of which are necessarily mutually exclusive156. In the infected basal cells (which might include stem cells), the viral genome replicates and establishes ∼50 HPV episome copies, which then segregate between the daughter progeny as the cells undergo cell division. The early viral proteins E6 and E7 are key to stimulating the continued proliferation and milieu for E1 and E2-driven vegetative viral genome replication to a very high copy number. Terminal differentiation of infected cells in the upper epithelial layers activates the expression of E4 and then L1 and L2 to package the very high copy numbers of the viral genome. The virions are released as E4 disintegrates the cytokeratin filaments, and the keratinocyte remnants are sloughed off the epithelial surface. Thus, the viral life cycle is completed without directly causing cell death and without systemic viraemia or apparent inflammation to avoid alerting the local immune responses20. APC, antigen-presenting cell.
Early extracellular events. HPV infects the epithelium (Fig. 1, magnified area) by binding of L1 to heparan sulfate proteoglycans (HPSGs) on the basement membrane that are exposed by an abrasion. Binding induces a conformational change in the capsid, revealing the amino terminus of L2, which is then available for cleavage by extracellular furin. L2 cleavage by furin is a prerequisite to virus uptake and internalization over several hours by the target cell21.
Virus uptake and delivery of its genome to the nucleus. Uptake of the bound virus occurs via endosomal vesicles and is L1-mediated. Once the virus has entered the cell, L2 is essential for infection as the endosomal virus engages the retromer and travels towards the nucleus. While L1 is being degraded, L2 mediates its escape in complex with the viral genome from the endosome into the trans-Golgi network22,23. The entry of the L2-genome complex into the nucleus is dependent on cell cycle progression and occurs upon transient nuclear membrane breakdown during mitosis24. Once inside the nucleus, the L2–genome complex associates with promyelocytic leukaemia nuclear bodies (termed ND-10), and early viral transcription is initiated25,26.
Viral transcription programmes and completing the viral life cycle. Early viral proteins E1 and E2 co-opt the host DNA replication machinery to establish 50–100 episomal copies per cell25. Use of the host replication machinery ensures a low error rate and thus the rate of viral evolution is very slow, meaning that immune escape through mutation is not an important issue for HPV vaccination because variants are of the same serotype27. The productive phase of the unique life cycle of HPV exhibits exquisite spatial and temporal regulation following keratinocyte differentiation in the squamous epithelium (Fig. 1). Triggered by epithelial differentiation of daughter basal cells leaving the basement membrane, the switch to high copy number (>103 per cell) HPV genome replication and the expression of the late viral (capsid) genes for virion assembly occur only in the upper, terminally differentiated layers of the epithelium, and virus-laden squames are shed. Although vaccination with the capsid antigens can trigger cellular immune responses, they are not therapeutic because the basal epithelial cells harbouring HPV express only the early genes10,11. Consequently, most therapeutic vaccines target E6 and/or E7, as the other early viral proteins are not typically expressed in cancer or not obligatory for tumour cell viability10,11.
To access host replication factors, the virus drives the host keratinocyte into S phase12. This occurs through expression of the three viral oncoproteins E5, E6 and E7. E5 increases growth factor signalling, in particular epidermal growth factor receptor (EGFR), to promote exit from G0–G1. E6 binds and triggers proteasomal degradation of p53 and other pro-apoptotic factors to promote cell survival and PDZ proteins to promote de-differentiation of cells. E6 also activates MYC expression and telomerase to promote cell survival. E7 binds to multiple targets, notably RB, to overcome the restriction point (Fig. 2). The viral oncoproteins encoded by βHPV types share some targets but act somewhat differently16.
While high-risk human papillomavirus (hrHPV) infection alone is not sufficient to cause cancer, it regulates pathways that promote the hallmarks of cancer157, via E6, E7 and E5 (Ref. 12). This includes sustaining proliferative signalling via E7 and E5; enabling replicative immortality via E6; activating invasion and metastasis (that is, subverting keratinocyte differentiation via E6); deregulating cellular energetics via E6; and inducing local angiogenesis via E6 and E7, through the dysregulation of pathways as indicated in the figure. While this dysregulation triggers growth suppressors that promote cell death, they are restrained by E6 (via degradation of p53 and BCL-2 homologous antagonist/killer (BAK) and upregulation of BCL-2). The derailing of cell cycle control results in double-stranded (ds)DNA breaks, genomic instability and mutations that can lead to additional 'hits' that drive towards lethal cancer12. Numerous mechanisms to avoid destruction by promoting immune deviation have been evolved by hrHPV, as reviewed in Refs 158,159. E6 and/or E7 expression interferes with several aspects of innate immune activation, including detection of viral DNA by cyclic GMP–AMP synthase–stimulator of interferon genes protein (cGAS–STING) and Toll-like receptor 9 (TLR9); production of interferon-κ (IFN-κ) and CXC-chemokine ligand 14 (CXCL14), which are important for Langerhans cell chemotaxis; suppression of pro-inflammatory responses — including through type 1 interferon signalling (interferon regulatory factor 1 (IRF1)) — and production of CC-chemokine ligand 20 (CCL20), to prevent the recruitment of antigen-presenting cells (APCs) to the site of infection. E5 interferes with T cell recognition through disruption of antigen presentation via modulation of major histocompatibility complex (MHC) I and MHC II cell surface expression and downregulation of transporter associated with antigen processing (TAP), while neutralizing antibody (nAb) production is hampered by release of virions outside the body rather than into systemic circulation. Furthermore, E6 and E7 expression induces production of interleukin-6 (IL-6), which recruits monocytes that generate tumour-promoting inflammation via local expression of CCL2 and matrix metalloproteinase 9 (MMP9). Such virus-mediated immune interference combines to promote the persistence of the infection and thereby promote the risk of cancer. EGFR, epidermal growth factor receptor; HDAC, histone deacetylase; HIF1α, hypoxia-inducible factor 1α; KDM6A, lysine-specific demethylase 6A; VEGF, vascular endothelial growth factor. Figure adapted with permission from Ref. 157, Elsevier.
Ectopic expression of E6 and E7 of hrHPV, but not low-risk HPV (lrHPV), is sufficient to immortalize primary keratinocytes and induce genomic instability12. Carcinogenesis is not beneficial to the virus but is an unfortunate consequence of viral oncogene expression and the resultant genomic instability and dysregulated proliferation12 (Fig. 2). Oncogenicity varies among hrHPV, but HPV-16 and HPV-18 are associated with the most rapid carcinogenic progression4. Additional genetic hits are necessary for carcinogenesis; smoking, oral contraceptives and multiparity are cofactors for cervical cancer28 and ultraviolet light is a cofactor for non-melanoma skin cancers16.
Self-limited versus persistent infection
Fortunately, the majority of hrHPV infections do not progress to cancer but instead resolve spontaneously. Thus, the tension between persistence and clearance is central to the carcinogenic potential of hrHPVs. It remains controversial whether clearance is control to below the level of detection or complete elimination of the virus29,30,31,32. There has been much interest in whether this dichotomy reflects infection of a stem cell (which would remain in the basal layer, producing HPV+ daughter cells) or infection of a more differentiated keratinocyte (for example, an HPV+ transit-amplifying cell, which rises through the epithelium and is lost). Likewise, the site of infection may also be important, with recent evidence suggesting that the CK7+ and p63− cells of the squamocolumnar junction are residual embryonic cells that provide a niche for cervical carcinogenesis33.
There is an increased burden of HPV-associated cancers in patients with a compromised immune system, whether iatrogenically in organ transplant recipients9, via co-infection with HIV8 or via certain genetic syndromes (for example, epidermodysplasia verruciformis or warts, hypogammaglobulinaemia, immunodeficiency and myelokathexis (WHIM) syndrome)34. These observations, as well as studies in animal models12, support a central role for cellular immunity in the natural control of HPV infection.
Neutralizing antibodies (nAbs) can be protective, but these are triggered only after infection and cannot eliminate virus-infected cells. However, the relevance of capsid-binding antibodies is indicated because numerous genotypes exist with great variation in the immunodominant L1 surface loops that form neutralizing epitopes that are type-restricted35. However, the roles of macrophages and natural killer (NK) cells in the control of infection, as well as defence mechanisms within the infected keratinocyte, are less well understood. Langerhans cells are the primary antigen-presenting cell (APC) in the epithelium and are likely critical to the recognition of infection and the induction of HPV-specific cellular immunity36.
Most times, a combination of innate and adaptive immunity eliminates infection36 (Fig. 3). Effector T cells targeting early viral proteins (notably E2, E6 and E7) can attack the virus-infected cells. Helper T cells that recognize L1 facilitate the induction of nAbs that can prevent virus transmission and reinfection of the host37. However, with HPV persistence, lesion progression can be driven by de-repressed expression of E6 and E7, which can result from methylation of the E2 promoter but is most commonly attributed to viral integration12. This leads to immune deviation by compromising the innate immune system via a series of interacting and self-reinforcing events mediated through modulation of different immune activation pathways. For example, E6 and/or E7 interfere with recognition by intrinsic immune receptors cyclic GMP–AMP synthase–stimulator of interferon genes protein (cGAS–STING) and Toll-like receptor 9 (TLR9), including through interferon regulatory factor 1 (IRF1) or IRF3 inhibition, and thereby block innate signalling of the viral genome presence while suppression of interferon-κ (IFNκ), CXC-chemokine ligand 14 (CXCL14) and CC-chemokine ligand 20 (CCL20) production prevents the recruitment of APCs to the site of infection. Such events compromise and/or delay the induction of an adaptive immune response (Fig. 2), facilitating viral persistence and increased risk of cancer. E6 and E7 overexpression also compromises cellular DNA repair and induces extra centrosomes (leading to genomic instability38,39,40), and it can further increase immune escape41,42,43,44. This and additional cofactors provide genetic changes driving malignant transformation over 1–2 decades after initial HPV infection12.
The immune system controls most human papillomavirus (HPV) infections before cancer can develop. The process of virus uptake into epithelial cells occurs over several hours and thus offers a time window for the action of vaccine or naturally induced neutralizing antibodies (nAbs). The first step is the detection of damage by the innate immune response arm via local antigen-presenting cells (APCs) and their activation (step 1). The secretion of pro-inflammatory cytokines and chemokines supports the viral antigen processing and migration to loco-regional lymph nodes (LNs) (step 2). Here, activated APCs stimulate various viral-antigen-specific CD4+ T cells that can either help activation of CD8+ T cells (for example, in targeting early viral antigens) or help B cells to produce nAbs that are, for example, directed against capsid proteins (step 3). The local activation of the innate immune response results in the attraction of nonspecific effectors (such as natural killer (NK) cells), the secretion of interferons (which can directly affect the HPV infection) and the attraction of more APCs to further drive activation of adaptive immunity (step 4). This inflammatory state provides the signals to attract the effector CD8+ T cells, which can target the virus-infected cells in the basal layers of the epithelium and are critical to clearance of the virus infection (step 5). Long-lived plasma cells secrete nAbs that can access the infection site either by transudation from the blood to the mucosal secretions or by serous exudation. Only the viral particles, and not the HPV-infected cells, can be targeted by nAbs, which are thus unable to cure infection but can stop further infections (step 6). Such antibody responses in women occur many months after HPV infection, and the levels detected are not necessarily sufficient to prevent a subsequent infection by the same virus type. It is likely that long-term natural protection against a specific HPV-type infection is the result of cell-mediated immunity, with nAbs contributing to a much lesser extent. BM, basement membrane; MHC, major histocompatibility complex; TCR, T cell receptor.
Vaccine requirements
Induction of nAbs is the major basis of vaccine-induced protection but requires immunization with the killed or attenuated natural pathogen or a subunit vaccine. An ideal vaccine should provide protection against all hrHPV types, and also the possibly carcinogenic types, to eliminate the need for cervical screening17. Sterilizing immunity may be required, as the cervical location of infection lacks secondary lymphoid tissue wherein substantial numbers of memory B cells could reside, ready to produce antibody at sufficient levels and, in time, to neutralize the virus before uptake45. Unfortunately, the levels of type-specific antibody produced in natural infection are often insufficient to protect against subsequent reinfection. Therefore, a vaccine should deliver an improved response compared with natural serological responses.
To ensure protective immune responses throughout sexually active life, high and sustained levels of serum antibody are desired following HPV vaccination. The ability of natural HPV exposure to improve B cell memory is not known. Therefore, maximal longevity of antibody levels directly induced by vaccination is needed. The current model suggests that plasma cells are imprinted with a predetermined lifespan. This model is based on the magnitude of B cell signalling that occurs during induction of an antigen-specific humoral immune response46. Importantly, the magnitude and longevity of antibody responses are increased by adjuvants, for example, alum and MF59, which, among other effects, promote slow-release antigen depots to prolong antigen exposure, and danger signals such as monophosphoryl lipid A, which promote B cell activation via TLRs47,48.
The ultimate goal is the best use of resources to have the maximum impact in preventing HPV-associated cancer. The key elements of a suitable vaccination programme will ideally be the selection of an optimal immunization age (and possible catch-up cohorts), the decision on sex-independent vaccination or whether female-only vaccination provides sufficient vaccination coverage, and how to integrate vaccination with programmes for surveillance and treatment of HPV disease. Currently, the main problem is the lack of access to HPV vaccination in low-income and middle-income countries (LMICs), where cervical screening is inadequate if at all present and wherein >86% of cervical cancer cases and 88% of related deaths occur2,3. With a predominance of sexual transmission, the coverage requirements for HPV vaccination will likely be <95% because of herd immunity49.
Virus-like particle vaccines
In the early 1990s, it was discovered that recombinant expression of L1 in a range of systems yielded virus-like particles (VLPs)that were devoid of the oncogenic viral genome and immunologically similar to native virions — a eureka moment for vaccine development50. Studies in diverse animal models have consistently shown that vaccination with L1 VLP, even without adjuvant, elicited high and durable titres of nAbs that protected against experimental viral challenge, as demonstrated by passive-transfer studies51,52. However, it was also shown that the protection elicited by L1 VLP was type-restricted, indicating that to achieve broad protection, an HPV vaccine would likely need to contain L1 VLP of several key types. As 70–80% of cervical cancer is caused by HPV-16 and HPV-1812, these two types were the focus of the first vaccines, with the intent of achieving broader protection through cross reactivity or expansion of the range of VLP types.
Assessing vaccine immunogenicity and efficacy. Vaccine development starts with the task of assessing safety and immunogenicity. The serological assays used to assess immunogenicity are outlined in Box 1. These approaches differ considerably in the spectrum and potential relevance of the detected antibodies (Box 1; Fig. 4). Efficacy depends on the integrated effects of antibody specificity, avidity and local in vivo concentration and potentially effector cells, such as phagocytes or local memory B cells. These qualities will also influence the potential for cross-protection and longevity.
Vaccination with human papillomavirus (HPV) capsid antigens can induce different types of type-specific antibodies, most of which can bind to the native virion, but not all will necessarily neutralize the virus by preventing uptake by the target cell. Antibodies depicted in black represent non-neutralizing antibodies (non-nAbs), which are not able to directly influence the infectivity of the virus. The available data suggest that an initial step that can be blocked by some L1- virus-like-particle (VLP)-induced nAbs is the binding to heparin sulfate proteoglycans (HSPGs) on the basement membrane (BM) (indicated by red cross)160,161. Orange nAbs represent those that can potentially influence infectivity after HSPG-binding events that occur before and after changes to L2 (indicated by orange cross). These antibodies are detected with different assay types (Box 1). Immunization with L1 VLPs cannot reflect all the potential structures through which antibodies may be able to block the infection process (Fig. 1), most notably L2, which is poorly immunogenic in natural infection. Nevertheless, L2 is a potentially effective target for prophylaxis. L2 vaccination induces nAbs (depicted in green) that neutralize the virion after binding and only after a conformational change in the capsid and cleavage of L2 by extracellular furin to render L2 protective epitopes, such as residues 17–36, accessible to antibody binding (indicated by green cross)146. L2-specific antibodies have a much lower titre and avidity than L1 VLP-specific antibodies. The L2 epitope spacing will probably not allow bivalent binding of this antibody. The different types of antibodies may include recognition of different epitopes of L1 or L2 molecules. Late events associated with virus uptake and processing by the cell may also be interfered with by nAbs. There are clearly still gaps in our knowledge of the infection process and the nature of antibodies that can influence the process, including the contribution of phagocytes that recognize the crystallizable fragment (Fc) of capsid-reactive antibodies.
The two pioneering vaccines (Table 1) — a bivalent (2vHPV) vaccine (L1 VLPs of HPV-16 and HPV-18 with AS04, an adjuvant comprising aluminium hydroxide and monophosphoryl lipid A) marketed as Cervarix and a quadrivalent (4vHPV) vaccine (L1 VLPs of HPV-6, HPV-11, HPV-16 and HPV-18 with an aluminium hydroxyphosphate sulfate (AHSS) adjuvant) marketed as Gardasil — were shown to induce antibody titres 2–3 orders of magnitude higher than those seen in natural infection, as assessed by various different serological assays53. As it takes 1–2 decades from hrHPV infection to the development of cervical cancer and because the ablation of CIN2/3 precursor lesions protects against cervical cancer, the presence of such precursor lesions is used as the efficacy end point of clinical trials. In registration trials and subsequent population surveys, vaccines based on L1 VLP proved remarkably safe as well as effective for protection against new infections and disease associated with the types targeted by each vaccine. Thus, they were approved for protection against anogenital infection and disease associated with the types used to make the VLP54,55,56,57. Of note, there is no approval of these vaccines yet for the prevention of HPV-associated oropharyngeal squamous cell carcinoma (OPSCC), and this reflects the lack of a validated precursor lesion in the oral cavity for use as a disease end point in efficacy trials58. HPV tests for cervical cancer screening have been licensed in some countries. Therefore, the option of using persistent HPV infection over 6 or 12 months as an end point for the approval of vaccines, especially of next-generation vaccines and of vaccines for the prevention of HPV-associated OPSCC, is being considered59,60.
Cross-protection, dosing schedules and longevity. Vaccine-mediated, type-specific protection has been shown to be durable for at least a decade. Importantly, this protection was not absolutely type-specific because significant cross-protection (particularly by vaccination with the 2vHPV vaccine) was observed against very closely related types from within the same species, for example, HPV-16 with HPV-31 and HPV-33, or HPV-18 with HPV-45. Indeed, while only 52% of CIN3 is associated with HPV-16 and HPV-18, vaccination with the 2vHPV vaccine showed an efficacy of 93% in protecting against CIN3, irrespective of the HPV type55,57. Although the substantially lower titres of cross-neutralizing antibody compared with those of type-specific antibodies raised concern about the durability of cross-protection61, there has been little evidence of the waning of cross-protection in patients who have been vaccinated three times as per recommendation62. Indeed, recent data from Scotland confirm cross-protection through a decrease in the prevalence of HPV-31, HPV-33 and HPV-45 during the 5-year follow-up after vaccination with the 2vHPV vaccine63,64.
Both the 4vHPV vaccine and the 2vHPV vaccine induce sustained levels of antibodies against HPV-16 and HPV-18, but the responses are not identical. Five years after vaccination, females aged 18–45 years who received the 2vHPV vaccine showed higher serum nAb responses than those given the 4vHPV vaccine, where seropositivity rates against HPV-18 decreased across all age groups53. In addition, vaccination with the 2vHPV vaccine produces a T helper 1 (TH1) cell-biased response that favours immunoglobulin G1 (IgG1) and IgG3 serum responses65,66, while vaccination with the 4vHPV vaccine produces a TH2-biased response that favours IgG1, IgG4 and IgA serum responses67. These vaccines use different adjuvants and L1 expression systems to generate VLP — differences that potentially affect relative immunogenicity (titre), longevity and breadth of immunity.
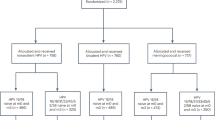
An important factor in vaccine immunogenicity is also the age of the recipients. For example, in females aged 10–17 years who received the 2vHPV vaccine, the geometric mean titres (GMTs) of IgG are at least twice as high as those of females aged 18–25 years68. Subsequent immune-bridging studies demonstrated that 9–14-year-old females who received two doses of the 2vHPV vaccine with an interval of 0 and 6 months showed non-inferior immune responses compared with those who received three doses of the 4vHPV vaccine on a schedule of 0, 2 and 6 months, and the efficacy against disease was established in these groups69. On the basis of such studies, the World Health Organization (WHO) has now recommended two doses of the 4vHPV vaccine or the 2vHPV vaccine for 9–15-year-old females. Remarkably, recent evidence suggests that durable type-specific immunity can be achieved with a single dose of either the 2vHPV vaccine70 or the 4vHPV vaccine71. Analysis of the impact of bivalent HPV vaccination in a population of 14–18-year-old females in the UK also shows evidence of type-specific protection but not cross-protection following a single dose of vaccine72. At this point, both the 2vHPV vaccine-vaccinated and the 4vHPV vaccine-vaccinated populations appear to be potently and durably protected against the HPV types they were designed to prevent. A major randomized trial (ESCUDDO) to test the efficacy of single-dose vaccination is underway, and it will also provide some independent comparisons between HPV vaccines73.
A 9-valent (9vHPV) vaccine, Gardasil 9, that contains VLPs from HPV-6, HPV-11, HPV-16, HPV-18, HPV-31, HPV-33, HPV-45, HPV-52 and HPV-58 has now been tested in comparison with the 4vHPV vaccine from the same manufacturer. The 9vHPV vaccine prevented infection and disease related to HPV-31, HPV-33, HPV-45, HPV-52 and HPV-58 in a susceptible population of 16–26-year-old females and generated an antibody response to HPV-6, HPV-11, HPV-16 and HPV-18 that was non-inferior to that generated by the 4vHPV vaccine. The 9vHPV vaccine did not demonstrably prevent infection and disease related to HPV types beyond the nine types covered by the vaccine, although the study was not powered to do so74.
Effectors of protection
An understanding of the mechanism of protection is important to identify the relevant immune correlates of protection and thus facilitate the development of biosimilar and second-generation prophylactic vaccines (Fig. 5a). Passive transfer into naive animals of L1 VLP-specific immune serum, IgG or purified monoclonal antibodies that show in vitro neutralizing activity protects against experimental animal papillomavirus or HPV pseudovirion (PsV) challenge51,52,75,76 (Box 1). Although L1 VLP vaccines induce very high titres of serum neutralizing IgG, protection can be achieved with much lower titres77, as seen with cross-protection and, as discussed below, with L2-based vaccines21,78. Figure 4 summarizes the different phases of early infection and potential specificities of antibodies that may be relevant to neutralization.
a | The challenges and possible solutions to bringing a novel preventive human papillomavirus (HPV) vaccine from its initial invention through licensure. b | Challenges and possible solutions to achieving global use of licensed HPV vaccines and herd immunity and thus recognizing the full potential of cancer prevention. FDA, US Food and Drug Administration; Gavi, Global Alliance for Vaccines and Immunization; IP, intellectual property; WHO, World Health Organization.
The role of nAbs as the primary effector of protection is widely accepted; however, this concept does not consider the contribution of cellular immunity and a potential therapeutic benefit. Vaccination with L1 VLP does not confer a therapeutic benefit in most disease models or clinical studies79, although there have been hints of activity80. L1 VLP immunization does induce a robust L1-specific CD8+ T cell response, but basal keratinocytes harbouring HPV do not detectably express L1 and thus presumably escape this response. The activity of T helper cells is important to achieve a robust response. L1 VLP challenge studies demonstrate the induction of a rapid anamnestic response81,82, which has been suggested to prolong protection if titres decline.
Immunogenicity of capsid proteins
The data emerging from the UK showing that HPV-16 and HPV-18 L1 VLP immunization reduces the occurrence of HPV-6-associated and HPV-11-associated genital warts83, as well as the reports of the high efficacy of single-dose L1 VLP immunization on HPV prevalence and disease70,71,72, merit further discussion. One possibility to explain the unexpected cross-protection is that the adjuvant AS04 in the bivalent vaccine induces a particularly effective T cell response against L1, which will cross-react to HPV-6 and HPV-11 L1 proteins and act either directly, by enhancing local innate control, or by providing help for subsequent specific, therapeutic adaptive immunity against other viral targets. AS04 contains the TLR4 agonist monophosphoryl lipid A and aluminium salts and is particularly effective in activating APCs, inducing cytokines that enhance the adaptive immune response and inducing a TH1-type response, thereby enhancing humoral and cellular responses48. TH1 immune cell-derived IFNγ induces anti-viral protein effector functions, leading to inhibition of viral transcription or translation and infection84. Such events are likely to contribute to local control of HPV infections.
A key feature of L1 VLPs is their high immunogenicity, which is present even without adjuvant and also in immunocompromised patients with HIV85,86. As mentioned before, even a single dose of the 2vHPV or 4vHPV vaccines is sufficient to induce a robust, durable IgG response indicative of antibody class switching, somatic hypermutation, affinity maturation and memory B cell development that does not require subsequent re-exposure or boosting70,71. This immunogenicity likely reflects the highly ordered and closely packed 3D structure of L1 VLP87. By comparison, denatured L1 protein is not an effective immunogen88, while capsomers, comprising L1 pentamers, are strongly immunogenic but do not achieve the titres of L1 VLP (which are formed from 72 capsomers) without the use of adjuvants89,90. The close spacing of the epitopes is also important, likely reflecting their ability to perform bivalent immunoglobulin binding and crosslinking of B cell receptors87. The remarkable immunogenicity of L1 VLPs may also derive from a direct activation of immature dendritic cells and induction of key chemokines, cytokines and co-stimulatory molecules central to effective antigen presentation91,92.
By contrast, the L2 protein does not form VLP on its own and is weakly immunogenic when given without an adjuvant93. There are only 12–72 copies of L2 per virion compared with 360 L1 in the capsid, and thus L2 is spaced further apart94,95, which potentially contributes to the poor immunogenicity of L2 in the context of the capsid compared with that of the immunodominant L1 (Ref. 93). Nevertheless, vaccination with L2 is protective, although the antibody response elicited by L2 is characterized by a lower titre and avidity than that elicited by L1 VLP96. We speculate that these differences may reflect, in part, the inability of antibodies directed against L2 to bind bivalently to the capsid because of the greater separation of L2 epitopes compared with L1 epitopes87,97. Despite these differences, vaccination with L2 using an adjuvant such as alum provides durable immunity in animal models, and passive-transfer studies show that low titres of nAbs with moderate avidity suffice for protection76,97,98. Interestingly, the subdominant protective epitopes of L2 are well conserved between types and broadly cross-protective in animal models97,98,99.
Antibody-mediated protection
Vaginal fluids of vaccinated patients contain neutralizing IgG at levels consistent across the menstrual cycle but much lower than the levels in serum45. Notably, studies in animals show that protection also occurs at extragenital sites, and passive intraperitoneal transfer of nAbs even just before experimental HPV challenge provides robust protection. This suggests that abrasion of the epithelium at the site of infection is sufficient to support exudation of serum IgG and neutralize the inoculum75. It is unclear whether the viral inoculum can reactivate putative local memory B cells to produce sufficient neutralizing IgG locally in time to prevent infection, although such an anamnestic response might be important if antibody titres have declined substantially many years after vaccination81,100,101.
An important question is which serum level of antibody is correlated with immunity. To date, there has not been enough breakthrough infection for type-specific immunity in vaccinated patients to determine the minimum titre required for protection. However, it may be possible to approach this question by analysing the level of cross-protection that is often insufficient in patients and associated with much lower titres of cross-neutralizing antibodies102. International serologic units have been established for HPV-16 and HPV-18, and ongoing efforts to further this standardization are critical103. Immune-bridging studies have been used to obtain licensure for vaccination in female and male adolescents and young adult females104 for a two-dose vaccination schedule105 and for using the 9vHPV vaccine for vaccination against HPV-16 and HPV-1874. These efforts underline the growing importance of serological standardization and the need to define a minimum titre that correlates with protection, especially for the development of low-cost biosimilar and L2 vaccines60.
Application of preventive HPV vaccines
The primary factor limiting the impact of vaccination is inadequate population coverage106 (Fig. 5b). In a few developed countries and some LMICs using school-based vaccination programmes, high and sustained levels of vaccination coverage (70–90%) have been achieved when targeting adolescent females64,107,108,109. This level of vaccination coverage is sufficient to achieve a significant reduction in hrHPV prevalence and associated cervical lesion rates, as well as herd immunity in males within the general population110. Unfortunately, even in most highly developed countries, such a level of vaccination coverage has not been consistently achieved. Critically, global estimates of HPV vaccination delivery by region and income level show virtually no significant delivery to many poorer populations of women worldwide107. The relatively high cost of the current vaccines is one contributing factor. Although efforts such as the Gavi Vaccine Alliance (see related links) have reduced the price of the current vaccines for developing countries with the greatest burden of cervical cancer, the commitment of national governments to support the logistics for establishing and sustaining efficient vaccination programmes is central to any long-term success111. Unfortunately, vaccination programmes compete with screening-based approaches for funding, and vaccination has little or no benefit for those already infected with HPV79. The HPV-FASTER protocol, which includes extending routine vaccination programmes to females up to 30 years of age in conjunction with at least one HPV screening test for females at 30 years of age or older may, based on modelling studies, accelerate the reduction in cervical cancer incidence. Indeed, modelling suggests that temporary introduction of catch-up vaccination for older females, although less effective, would advance the date to achieve cervical cancer reduction by several years. Refining this protocol for a particular population will require further investigation, including cost-effectiveness modelling to determine the age ranges for HPV vaccination and screening intervals in public health programmes, and to estimate possible impact based on the resources available112.
Targeting adolescent females before sexual debut was considered the best strategy to deliver cervical cancer protection and has shown remarkable success64. However, given the durable responses to HPV vaccination seen thus far, it is likely feasible to implement a childhood regimen and even to piggyback HPV vaccines in the same vial with other childhood vaccines administered within existing regimens to reduce infrastructure demands. This would need to be phased in to replace the current vaccination schedule for adolescents so that no child reaches sexual debut without HPV vaccination.
The need for refrigeration of the vaccine is another hurdle in underdeveloped nations. This may be addressed with lyophilized formulations or with heat-stable capsomer preparations113,114. Thus, a combination of technical improvements, additional low-cost producers and the continued commitment of public health professionals to demonstrate the safety and benefits of HPV vaccination is critical for global implementation (Fig. 5b).
In areas of limited resources, there has been debate about whether to prioritize vaccination of adolescent females or to promote sex-independent vaccination. It is clear that females suffer the greatest burden of cancer caused by HPV, but to achieve herd immunity most effectively115, to address other HPV-related cancer types and to reach men who have sex with men, it is recommended to vaccinate adolescent males as well. Indeed, immunization of adolescent males also improves the resilience of programmes, accelerates the reduction in HPV prevalence116, increases cross-protection and provides a health benefit to unvaccinated females115. Co-infection with HIV is associated with increased risk of HPV-associated cancers. Patients with HIV respond to HPV vaccination with titres suggestive of protection, although this remains unproven86,117,118.
Promising avenues for HPV vaccination
Table 1 summarizes HPV vaccines either licensed or in clinical development. Emergence of local biosimilar vaccine production is likely to advance sustainable implementation of HPV vaccination worldwide by reducing costs and promoting access. Indeed, a major effort is underway to develop two additional bivalent HPV vaccines using L1 VLP purified from Escherichia coli. These vaccines are Cecolin, which targets HPV-16 and HPV-18 and is in a phase III clinical trial119, and Gecolin, which targets HPV-6 and HPV-11 (Ref. 120). Likewise, local production of the currently licensed vaccines could reduce pricing substantially111.
There remains considerable interest in developing preventive HPV vaccines with broader coverage of HPV types. Currently, cervical screening, which is of considerable cost, is continued even in vaccinated patients because of the potential for disease caused by hrHPVs other than those targeted by the licensed vaccines. Notably, the predictive value, benefit:risk ratio and cost-effectiveness of cytologic screening are remarkably reduced in vaccinated women because of the dramatic reduction in the prevalence of CIN2/3 (Refs 110,121,122). The lower incidence of disease in vaccinated women alters the key performance indicators of cervical cytology, colposcopy referral criteria, colposcopy practice and histology reporting123. This impact might be mitigated to some degree by increasing intervals between screening and/or switching to HPV testing (which could include self-testing) as the primary screening modality124. Although a dual approach of screening and vaccination is being promoted112, the logistics and price of this approach will still be very challenging in many developing countries. However, childhood vaccination in this context has proved feasible for many pathogens106, and future developments in HPV vaccination that piggyback other paediatric immunization regimens are a good option for improving vaccination coverage and delivering substantial population protection with limited resources.
The cutaneous βHPV and γHPV species also have significant clinical impact15,125. Prevention of common foot and hand warts associated with γHPV types would reduce health-care costs125. In addition, βHPV types are associated with non-melanoma skin cancer in patients with immunity compromised through treatment (for example, organ transplant recipients), HIV co-infection or hereditary disease (epidermodysplasia verruciformis or WHIM syndrome)15,16. While vaccination would likely need to start in childhood126, a recent animal study has suggested that VLP vaccination prevents the development of non-melanoma skin cancer in infected immunocompromised hosts126,127.
A major challenge for the L1 VLP technology is the complexity of manufacturing a sufficiently multivalent formulation to comprehensively target the plethora of HPV types associated with disease. The 9vHPV vaccine targets the seven most common types detected in cervical cancer (Table 1), but including more L1 VLPs to cover the remaining high-risk types (each causing a very small fraction of cancers) is likely to make the vaccine prohibitively costly. The alternative approach is to find a single broadly protective antigen. The amino terminus of L2 harbours several well-conserved protective epitopes93, such as residues 17–36, recognized by monoclonal antibody RG175,128.
Neutralizing epitopes of L1 VLP are conformational, but they are linear for L2 and thus can be readily linked to further broaden immunity and fused with an adjuvant, for example, a TLR agonist76,129, to boost immunogenicity and extend protection. The immunogenicity of L2 protective epitopes can potentially be improved by displaying these epitopes on the immunodominant surface loops of L1 VLP130; the VLP of other viruses (such as adeno-associated virus (AAV))131 or bacteriophages132,133; or on a thioredoxin scaffold134 (Table 1). Several of these products are being prepared for early phase trials. The success of the L1 VLP vaccines demonstrates the potential of this approach but also represents a commercial hurdle unless L2 vaccines can also be useful in other indications (Fig. 5a).
There is still a massive global burden of HPV disease, and, unfortunately, vaccination with capsid antigens alone is not therapeutic for pre-existing infection. In an effort to combine both prophylaxis and therapeutic activity, early viral antigens E7 and/or E6 have been incorporated into L1 VLP or fused with L2 (Refs 135,136) (Table 1). Both approaches have been explored in early phase therapeutic studies and found to be both immunogenic and well tolerated. In these small trials, there was limited evidence of therapeutic activity, and prophylactic efficacy was not examined135,137. Given the delayed and uneven implementation of prophylactic HPV vaccination programmes, there remains a need to screen for and treat HPV-associated cervical disease. Figure 5 summarizes the challenges and some potential solutions for delivering substantial improvement in effective prophylactic HPV vaccination worldwide.
Conclusions
As the aetiology of hrHPV in anogenital and oropharyngeal cancers is well established, there are continuous efforts to fully implement vaccination programmes globally and to broaden coverage to all medically significant genotypes. In parallel, population-based HPV testing and/or cytological screening programmes can identify females for ablative therapy to prevent cervical cancer. The burden of HPV-related cancer falls primarily on the disadvantaged and medically underserved populations of the world, and, therefore, a focus on addressing issues constraining the delivery of these remarkably effective and safe interventions (as well as standard-of-care surgery and chemoradiation for patients with cancer) remains paramount. The prevention of HPV-related head and neck cancers would be a very beneficial, although unproven, outcome of vaccination. Preventive HPV vaccines to target a broader range of HPV types are being developed. While some may even protect against cutaneous warts and non-melanoma skin cancer associated with βHPV, the primary aim would be to reduce and eventually eliminate the need for continued cervical cancer screening. Indeed, there are important questions of how appropriate are current cervical cancer screening paradigms in properly vaccinated females, given their reduced predictive value and increased cost:benefit ratio, and what alternative screening technologies (for example, self-testing and point-of-care testing) or screening and vaccination combinations (for example, HPV-FASTER) might be substituted. In the long term, and provided there is sustained immunity, incorporating an HPV vaccine against oncogenic types within a multitarget paediatric vaccine regimen offers a viable strategy to improve vaccination coverage without added visits and ensures that everyone receives vaccination before sexual debut; however, this approach would need to be phased in. For current generations exposed to a high prevalence of HPV infection, the use of scarce resources for vaccination and screening must be carefully optimized through mathematical modelling to maximize benefits, as exemplified by HPV-FASTER112. Finally, the success of HPV vaccines in preventing cancer ultimately revolves around the effective communication of their safety and benefits to policymakers, physicians, patients and their families.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Volume 90. Human Papillomaviruses (IARC, 2007).
Forman, D. et al. Global burden of human papillomavirus and related diseases. Vaccine 30 (Suppl. 5), F12–F23 (2012). This study provides a recent summary of the global impact of HPV on cancer.
Plummer, M. et al. Global burden of cancers attributable to infections in 2012: a synthetic analysis. Lancet Glob. Health 4, e609–e616 (2016).
Kjaer, S. K., Frederiksen, K., Munk, C. & Iftner, T. Long-term absolute risk of cervical intraepithelial neoplasia grade 3 or worse following human papillomavirus infection: role of persistence. J. Natl Cancer Inst. 102, 1478–1488 (2010).
McCredie, M. R. et al. Natural history of cervical neoplasia and risk of invasive cancer in women with cervical intraepithelial neoplasia 3: a retrospective cohort study. Lancet Oncol. 9, 425–434 (2008).
Gillison, M. L. et al. Human papillomavirus and diseases of the upper airway: head and neck cancer and respiratory papillomatosis. Vaccine 30 (Suppl. 5), F34–F54 (2012).
Moscicki, A. B. et al. Updating the natural history of human papillomavirus and anogenital cancers. Vaccine 30 (Suppl. 5), F24–F33 (2012).
Denny, L. A. et al. Human papillomavirus, human immunodeficiency virus and immunosuppression. Vaccine 30 (Suppl. 5), F168–F174 (2012).
Wieland, U., Kreuter, A. & Pfister, H. Human papillomavirus and immunosuppression. Curr. Probl. Dermatol. 45, 154–165 (2014).
Stern, P. L. et al. Therapy of human papillomavirus-related disease. Vaccine 30 (Suppl. 5), F71–F82 (2012).
van der Burg, S. H., Arens, R., Ossendorp, F., van Hall, T. & Melief, C. J. Vaccines for established cancer: overcoming the challenges posed by immune evasion. Nat. Rev. Cancer 16, 219–233 (2016).
zur Hausen, H. Papillomaviruses and cancer: from basic studies to clinical application. Nat. Rev. Cancer 2, 342–350 (2002).
de Villiers, E. M., Fauquet, C., Broker, T. R., Bernard, H. U. & zur Hausen, H. Classification of papillomaviruses. Virology 324, 17–27 (2004). This study presents the phylogeny of the papillomaviruses.
Bernard, H. U. et al. Classification of papillomaviruses (PVs) based on 189 PV types and proposal of taxonomic amendments. Virology 401, 70–79 (2010).
McLaughlin-Drubin, M. E. Human papillomaviruses and non-melanoma skin cancer. Semin. Oncol. 42, 284–290 (2015).
Tommasino, M. The biology of beta human papillomaviruses. Virus Res. 231, 128–138 (2017).
Geraets, D. et al. Detection of rare and possibly carcinogenic human papillomavirus genotypes as single infections in invasive cervical cancer. J. Pathol. 228, 534–543 (2012).
Walboomers, J. M. et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J. Pathol. 189, 12–19 (1999). This study demonstrates that hrHPV is a necessary cause of cervical cancer.
Mirkovic, J. et al. Carcinogenic HPV infection in the cervical squamo-columnar junction. J. Pathol. 236, 265–271 (2015).
Doorbar, J. et al. The biology and life-cycle of human papillomaviruses. Vaccine 30 (Suppl. 5), F55–F70 (2012).
Day, P. M. et al. In vivo mechanisms of vaccine-induced protection against HPV infection. Cell Host Microbe 8, 260–270 (2010). This study demonstrates the power of the mouse vaginal challenge model using HPV pseudovirion and reveals important mechanistic aspects of infection of the genital tract.
Day, P. M., Thompson, C. D., Schowalter, R. M., Lowy, D. R. & Schiller, J. T. Identification of a role for the trans-Golgi network in human papillomavirus 16 pseudovirus infection. J. Virol. 87, 3862–3870 (2013).
Lipovsky, A. et al. Genome-wide siRNA screen identifies the retromer as a cellular entry factor for human papillomavirus. Proc. Natl Acad. Sci. USA 110, 7452–7457 (2013).
Pyeon, D., Pearce, S. M., Lank, S. M., Ahlquist, P. & Lambert, P. F. Establishment of human papillomavirus infection requires cell cycle progression. PLOS Pathog. 5, e1000318 (2009).
Day, P. M., Baker, C. C., Lowy, D. R. & Schiller, J. T. Establishment of papillomavirus infection is enhanced by promyelocytic leukemia protein (PML) expression. Proc. Natl Acad. Sci. USA 101, 14252–14257 (2004).
Bienkowska-Haba, M. et al. Incoming human papillomavirus 16 genome is lost in PML protein-deficient HaCaT keratinocytes. Cell. Microbiol. 19, e12708 (2017).
Pastrana, D. V., Vass, W. C., Lowy, D. R. & Schiller, J. T. NHPV16 VLP vaccine induces human antibodies that neutralize divergent variants of HPV16. Virology 279, 361–369 (2001).
Castellsague, X. & Munoz, N. Chapter 3: Cofactors in human papillomavirus carcinogenesis — role of parity, oral contraceptives, and tobacco smoking. J. Natl Cancer Inst. Monogr. 31, 20–28 (2003).
Hinten, F. et al. Reactivation of latent HPV infections after renal transplantation. Am. J. Transplant. 17, 1563–1573 (2017).
Gravitt, P. E. Evidence and impact of human papillomavirus latency. Open Virol. J. 6, 198–203 (2012).
Maglennon, G. A., McIntosh, P. B. & Doorbar, J. Immunosuppression facilitates the reactivation of latent papillomavirus infections. J. Virol. 88, 710–716 (2014).
Wang, J. W. et al. Immunologic control of Mus musculus papillomavirus type 1. PLOS Pathog. 11, e1005243 (2015).
Yang, E. J. et al. Microanatomy of the cervical and anorectal squamocolumnar junctions: a proposed model for anatomical differences in HPV-related cancer risk. Mod. Pathol. 28, 994–1000 (2015).
Dotta, L., Tassone, L. & Badolato, R. Clinical and genetic features of Warts, Hypogammaglobulinemia, Infections and Myelokathexis (WHIM) syndrome. Curr. Mol. Med. 11, 317–325 (2011).
Roden, R. B. et al. In vitro generation and type-specific neutralization of a human papillomavirus type 16 virion pseudotype. J. Virol. 70, 5875–5883 (1996).
Trimble, C. L. et al. Human papillomavirus 16-associated cervical intraepithelial neoplasia in humans excludes CD8 T cells from dysplastic epithelium. J. Immunol. 185, 7107–7114 (2010).
de Jong, A. et al. Human papillomavirus type 16-positive cervical cancer is associated with impaired CD4+ T-cell immunity against early antigens E2 and E6. Cancer Res. 64, 5449–5455 (2004).
Jeon, S., Allen-Hoffmann, B. L. & Lambert, P. F. Integration of human papillomavirus type 16 into the human genome correlates with a selective growth advantage of cells. J. Virol. 69, 2989–2997 (1995).
Jeon, S. & Lambert, P. F. Integration of human papillomavirus type 16 DNA into the human genome leads to increased stability of E6 and E7 mRNAs: implications for cervical carcinogenesis. Proc. Natl Acad. Sci. USA 92, 1654–1658 (1995).
The Cancer Genome Atlas Research Network et al. Integrated genomic and molecular characterization of cervical cancer. Nature 543, 378–384 (2017).
van Esch, E. M. et al. Intraepithelial macrophage infiltration is related to a high number of regulatory T cells and promotes a progressive course of HPV-induced vulvar neoplasia. Int. J. Cancer 136, E85–E94 (2015).
van Esch, E. M. et al. Expression of coinhibitory receptors on T cells in the microenvironment of usual vulvar intraepithelial neoplasia is related to proinflammatory effector T cells and an increased recurrence-free survival. Int. J. Cancer 136, E95–E106 (2015).
Heeren, A. M., Kenter, G. G., Jordanova, E. S. & de Gruijl, T. D. CD14+ macrophage-like cells as the linchpin of cervical cancer perpetrated immune suppression and early metastatic spread: A new therapeutic lead? Oncoimmunology 4, e1009296 (2015).
Heeren, A. M. et al. Prognostic effect of different PD-L1 expression patterns in squamous cell carcinoma and adenocarcinoma of the cervix. Mod. Pathol. 29, 753–763 (2016).
Schwarz, T. F. et al. Correlation between levels of human papillomavirus (HPV)-16 and 18 antibodies in serum and cervicovaginal secretions in girls and women vaccinated with the HPV-16/18 AS04-adjuvanted vaccine. Hum. Vaccin 6, 1054–1061 (2010).
Amanna, I. J. & Slifka, M. K. Mechanisms that determine plasma cell lifespan and the duration of humoral immunity. Immunol. Rev. 236, 125–138 (2010).
Giannini, S. L. et al. Enhanced humoral and memory B cellular immunity using HPV16/18 L1 VLP vaccine formulated with the MPL/aluminium salt combination (AS04) compared to aluminium salt only. Vaccine 24, 5937–5949 (2006).
Di Pasquale, A., Preiss, S., Tavares Da Silva, F. & Garcon, N. Vaccine adjuvants: from 1920 to 2015 and beyond. Vaccines 3, 320–343 (2015).
Baussano, I., Lazzarato, F., Brisson, M. & Franceschi, S. Human papillomavirus vaccination at a time of changing sexual behavior. Emerg. Infect. Dis. 22, 18–23 (2016).
Deschuyteneer, M. et al. Molecular and structural characterization of the L1 virus-like particles that are used as vaccine antigens in Cervarix, the AS04-adjuvanted HPV-16 and -18 cervical cancer vaccine. Hum. Vaccin 6, 407–419 (2010).
Suzich, J. A. et al. Systemic immunization with papillomavirus L1 protein completely prevents the development of viral mucosal papillomas. Proc. Natl Acad. Sci. USA 92, 11553–11557 (1995). This study demonstrates that passive transfer of VLP-immune sera protects naive animals from experimental viral challenge.
Breitburd, F. et al. Immunization with viruslike particles from cottontail rabbit papillomavirus (CRPV) can protect against experimental CRPV infection. J. Virol. 69, 3959–3963 (1995).
Einstein, M. H. et al. Comparison of long-term immunogenicity and safety of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine and HPV-6/11/16/18 vaccine in healthy women aged 18–45 years: end-of-study analysis of a Phase III randomized trial. Hum. Vaccin Immunother. 10, 3435–3445 (2014). This study provides a head-to-head comparison of the immunogenicity of the first two licensed HPV vaccines.
Schiller, J. T., Castellsague, X. & Garland, S. M. A review of clinical trials of human papillomavirus prophylactic vaccines. Vaccine 30 (Suppl. 5), F123–F138 (2012).
Lehtinen, M. et al. Overall efficacy of HPV-16/18 AS04-adjuvanted vaccine against grade 3 or greater cervical intraepithelial neoplasia: 4-year end-of-study analysis of the randomised, double-blind PATRICIA trial. Lancet Oncol. 13, 89–99 (2012). This study presents a demonstration of the 2vHPV vaccine efficacy.
Munoz, N. et al. Impact of human papillomavirus (HPV)-6/11/16/18 vaccine on all HPV-associated genital diseases in young women. J. Natl Cancer Inst. 102, 325–339 (2010). This is an important 4vHPV vaccine efficacy study.
Lang Kuhs, K. A. et al. Effect of different human papillomavirus serological and DNA criteria on vaccine efficacy estimates. Am. J. Epidemiol. 180, 599–607 (2014).
Chung, C. H., Bagheri, A. & D'Souza, G. Epidemiology of oral human papillomavirus infection. Oral Oncol. 50, 364–369 (2014).
Gillison, M. L., Chaturvedi, A. K. & Lowy, D. R. HPV prophylactic vaccines and the potential prevention of noncervical cancers in both men and women. Cancer 113, 3036–3046 (2008).
Lowy, D. R., Herrero, R. & Hildesheim, A. Primary endpoints for future prophylactic human papillomavirus vaccine trials: towards infection and immunobridging. Lancet Oncol. 16, e226–e233 (2015).
Bissett, S. L., Draper, E., Myers, R. E., Godi, A. & Beddows, S. Cross-neutralizing antibodies elicited by the Cervarix(R) human papillomavirus vaccine display a range of Alpha-9 inter-type specificities. Vaccine 32, 1139–1146 (2014).
Wheeler, C. M. et al. Efficacy, safety, and immunogenicity of the human papillomavirus 16/18 AS04-adjuvanted vaccine in women older than 25 years: 7-year follow-up of the phase 3, double-blind, randomised controlled VIVIANE study. Lancet Infect. Dis. 16, 1154–1168 (2016).
Cameron, R. L. et al. Human papillomavirus prevalence and herd immunity after introduction of vaccination program, Scotland, 2009–2013. Emerg. Infect. Dis. 22, 56–64 (2016).
Kavanagh, K. et al. Changes in the prevalence of human papillomavirus following a national bivalent human papillomavirus vaccination programme in Scotland: a 7-year cross-sectional study. Lancet Infect. Dis. 17, 1293–1302 (2017).
Scherpenisse, M. et al. Characteristics of HPV-specific antibody responses induced by infection and vaccination: cross-reactivity, neutralizing activity, avidity and IgG subclasses. PLOS ONE 8, e74797 (2013).
Herrin, D. M. et al. Comparison of adaptive and innate immune responses induced by licensed vaccines for Human Papillomavirus. Hum. Vaccin. Immunother. 10, 3446–3454 (2014).
Ruiz, W., McClements, W. L., Jansen, K. U. & Esser, M. T. Kinetics and isotype profile of antibody responses in rhesus macaques induced following vaccination with HPV 6, 11, 16 and 18 L1-virus-like particles formulated with or without Merck aluminum adjuvant. J. Immune Based Ther. Vaccines 3, 2 (2005).
Schwarz, T. F. & Leo, O. Immune response to human papillomavirus after prophylactic vaccination with AS04-adjuvanted HPV-16/18 vaccine: improving upon nature. Gynecol. Oncol. 110, S1–10 (2008).
Leung, T. F. et al. Comparative immunogenicity and safety of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine and HPV-6/11/16/18 vaccine administered according to 2- and 3-dose schedules in girls aged 9–14 years: Results to month 12 from a randomized trial. Hum. Vaccin Immunother. 11, 1689–1702 (2015).
Kreimer, A. R. et al. Efficacy of fewer than three doses of an HPV-16/18 AS04-adjuvanted vaccine: combined analysis of data from the Costa Rica Vaccine and PATRICIA Trials. Lancet Oncol. 16, 775–786 (2015). This is a landmark study showing the potential for vaccine type-specific protective efficacy with even a single dose of the 2vHPV vaccine.
Sankaranarayanan, R. et al. Immunogenicity and HPV infection after one, two, and three doses of quadrivalent HPV vaccine in girls in India: a multicentre prospective cohort study. Lancet Oncol. 17, 67–77 (2016). This study provides evidence for a remarkable protective efficacy of even a single dose of the 4vHPV vaccine.
Cuschieri, K. et al. Impact of partial bivalent HPV vaccination on vaccine-type infection: a population-based analysis. Br. J. Cancer 114, 1261–1264 (2016). This study describes the population-based impact of a national HPV vaccination programme.
Kreimer, A. R., Sherman, M. E., Sahasrabuddhe, V. V. & Safaeian, M. The case for conducting a randomized clinical trial to assess the efficacy of a single dose of prophylactic HPV vaccines among adolescents. J. Natl Cancer Inst. 107, dju436 (2015).
Joura, E. A. et al. A 9-valent HPV vaccine against infection and intraepithelial neoplasia in women. N. Engl. J. Med. 372, 711–723 (2015). This study provides a demonstration of the efficacy of the 9vHPV vaccine and the use of immuno-bridging.
Gambhira, R. et al. A protective and broadly cross-neutralizing epitope of human papillomavirus L2. J. Virol. 81, 13927–13931 (2007). This study presents the identification of a key cross-neutralizing L2 epitope with a monoclonal antibody and its ability to mediate protection.
Kalnin, K. et al. Incorporation of RG1 epitope concatemers into a self-adjuvanting Flagellin-L2 vaccine broaden durable protection against cutaneous challenge with diverse human papillomavirus genotypes. Vaccine 35, 4942–4951 (2017).
Longet, S., Schiller, J. T., Bobst, M., Jichlinski, P. & Nardelli-Haefliger, D. A murine genital-challenge model is a sensitive measure of protective antibodies against human papillomavirus infection. J. Virol. 85, 13253–13259 (2011).
Day, P. M. et al. A human papillomavirus (HPV) in vitro neutralization assay that recapitulates the in vitro process of infection provides a sensitive measure of HPV L2 infection-inhibiting antibodies. Clin. Vaccine Immunol. 19, 1075–1082 (2012).
Hildesheim, A. et al. Impact of human papillomavirus (HPV) 16 and 18 vaccination on prevalent infections and rates of cervical lesions after excisional treatment. Am. J. Obstet. Gynecol. 215, 212.e1–212.e15 (2016).
Jardine, D. et al. A randomized trial of immunotherapy for persistent genital warts. Hum. Vaccin. Immunother. 8, 623–629 (2012).
Olsson, S. E. et al. Induction of immune memory following administration of a prophylactic quadrivalent human papillomavirus (HPV) types 6/11/16/18 L1 virus-like particle (VLP) vaccine. Vaccine 25, 4931–4939 (2007).
Olsson, S. E. et al. Evaluation of quadrivalent HPV 6/11/16/18 vaccine efficacy against cervical and anogenital disease in subjects with serological evidence of prior vaccine type HPV infection. Hum. Vaccin 5, 696–704 (2009).
Canvin, M., Sinka, K., Hughes, G. & Mesher, D. Decline in genital warts diagnoses among young women and young men since the introduction of the bivalent HPV (16/18) vaccination programme in England: an ecological analysis. Sex. Transm. Infect. 93, 125–128 (2017).
Day, P. M., Thompson, C. D., Lowy, D. R. & Schiller, J. T. Interferon gamma prevents infectious entry of human papillomavirus 16 via an L2-dependent mechanism. J. Virol. 91, e00168-17 (2017).
Harro, C. D. et al. Safety and immunogenicity trial in adult volunteers of a human papillomavirus 16 L1 virus-like particle vaccine. J. Natl Cancer Inst. 93, 284–292 (2001).
Faust, H. et al. Human Papillomavirus neutralizing and cross-reactive antibodies induced in HIV-positive subjects after vaccination with quadrivalent and bivalent HPV vaccines. Vaccine 34, 1559–1565 (2016). This study demonstrates the immunogenicity of HPV vaccines in patients with HIV.
Chackerian, B., Lenz, P., Lowy, D. R. & Schiller, J. T. Determinants of autoantibody induction by conjugated papillomavirus virus-like particles. J. Immunol. 169, 6120–6126 (2002).
Kirnbauer, R., Booy, F., Cheng, N., Lowy, D. R. & Schiller, J. T. Papillomavirus L1 major capsid protein self-assembles into virus-like particles that are highly immunogenic. Proc. Natl Acad. Sci. USA 89, 12180–12184 (1992). This study demonstrates the importance of VLP structure in the induction of nAbs.
Thones, N., Herreiner, A., Schadlich, L., Piuko, K. & Muller, M. A direct comparison of human papillomavirus type 16 L1 particles reveals a lower immunogenicity of capsomeres than viruslike particles with respect to the induced antibody response. J. Virol. 82, 5472–5485 (2008).
Senger, T. et al. Virus-like particles and capsomeres are potent vaccines against cutaneous alpha HPVs. Vaccine 28, 1583–1593 (2010).
Lenz, P. et al. Papillomavirus-like particles induce acute activation of dendritic cells. J. Immunol. 166, 5346–5355 (2001).
Fausch, S. C., Da Silva, D. M. & Kast, W. M. Differential uptake and cross-presentation of human papillomavirus virus-like particles by dendritic cells and Langerhans cells. Cancer Res. 63, 3478–3482 (2003).
Roden, R. B. et al. Minor capsid protein of human genital papillomaviruses contains subdominant, cross-neutralizing epitopes. Virology 270, 254–257 (2000).
Buck, C. B. et al. Arrangement of L2 within the papillomavirus capsid. J. Virol. 82, 5190–5197 (2008).
Guan, J. et al. Cryoelectron microscopy maps of human papillomavirus 16 reveal L2 densities and heparin binding site. Structure 25, 253–263 (2017).
Chandrachud, L. M. et al. Vaccination of cattle with the N-terminus of L2 is necessary and sufficient for preventing infection by bovine papillomavirus-4. Virology 211, 204–208 (1995). This study demonstrates the potential of the amino terminus of L2 as a prophylactic vaccine antigen.
Tumban, E., Peabody, J., Peabody, D. S. & Chackerian, B. A universal virus-like particle-based vaccine for human papillomavirus: longevity of protection and role of endogenous and exogenous adjuvants. Vaccine 31, 4647–4654 (2013).
Gambhira, R. et al. Protection of rabbits against challenge with rabbit papillomaviruses by immunization with the N terminus of human papillomavirus type 16 minor capsid antigen L2. J. Virol. 81, 11585–11592 (2007).
Jagu, S. et al. Phylogenetic considerations in designing a broadly protective multimeric L2 vaccine. J. Virol. 87, 6127–6136 (2013).
Scherer, E. M. et al. Characteristics of memory B cells elicited by a highly efficacious HPV vaccine in subjects with no pre-existing immunity. PLOS Pathog. 10, e1004461 (2014).
Matsui, K. et al. Circulating CXCR5(+)CD4(+) T follicular-like helper cell and memory B cell responses to human papillomavirus vaccines. PLOS ONE 10, e0137195 (2015).
Kemp, T. J. et al. Kinetic and HPV infection effects on cross-type neutralizing antibody and avidity responses induced by Cervarix((R)). Vaccine 31, 165–170 (2012).
Eklund, C., Unger, E. R., Nardelli-Haefliger, D., Zhou, T. & Dillner, J. International collaborative proficiency study of Human Papillomavirus type 16 serology. Vaccine 30, 294–299 (2012).
Block, S. L. et al. Comparison of the immunogenicity and reactogenicity of a prophylactic quadrivalent human papillomavirus (types 6, 11, 16, and 18) L1 virus-like particle vaccine in male and female adolescents and young adult women. Pediatrics 118, 2135–2145 (2006).
Huang, L. M. et al. Sustained immunogenicity of 2-dose human papillomavirus 16/18 AS04-adjuvanted vaccine schedules in girls aged 9–14 years: a randomized trial. J. Infect. Dis. 215, 1711–1719 (2017).
Doherty, M., Buchy, P., Standaert, B., Giaquinto, C. & Prado-Cohrs, D. Vaccine impact: Benefits for human health. Vaccine 34, 6707–6714 (2016).
Bruni, L. et al. Global estimates of human papillomavirus vaccination coverage by region and income level: a pooled analysis. Lancet Glob. Health 4, e453–e463 (2016).
Binagwaho, A. et al. Integration of comprehensive women's health programmes into health systems: cervical cancer prevention, care and control in Rwanda. Bull. World Health Organ. 91, 697–703 (2013).
Dorji, T. et al. Introduction of a National HPV vaccination program into Bhutan. Vaccine 33, 3726–3730 (2015).
Drolet, M. et al. Population-level impact and herd effects following human papillomavirus vaccination programmes: a systematic review and meta-analysis. Lancet Infect. Dis. 15, 565–580 (2015). This study documents the herd immunity effects in adolescent males after high uptake of HPV vaccination in female adolescents.
Clendinen, C., Zhang, Y., Warburton, R. N. & Light, D. W. Manufacturing costs of HPV vaccines for developing countries. Vaccine 34, 5984–5989 (2016).
Bosch, F. X. et al. HPV-FASTER: broadening the scope for prevention of HPV-related cancer. Nat. Rev. Clin. Oncol. 13, 119–132 (2016).
Rose, R. C. et al. Human papillomavirus type 11 recombinant L1 capsomeres induce virus-neutralizing antibodies. J. Virol. 72, 6151–6154 (1998).
Hassett, K. J. et al. Development of a highly thermostable, adjuvanted human papillomavirus vaccine. Eur. J. Pharm. Biopharm. 94, 220–228 (2015).
Lehtinen, M. et al. Impact of gender-neutral or girls-only vaccination against human papillomavirus — results of a community-randomized clinical trial (I). Int. J. Cancer 142, 949–958 (2018). This study presents a comparison of the impact of sex-independent or female-only HPV vaccination in adolescents.
Elfstrom, K. M., Lazzarato, F., Franceschi, S., Dillner, J. & Baussano, I. Human papillomavirus vaccination of boys and extended catch-up vaccination: effects on the resilience of programs. J. Infect. Dis. 213, 199–205 (2016).
Toft, L. et al. Comparison of the immunogenicity and reactogenicity of Cervarix and Gardasil human papillomavirus vaccines in HIV-infected adults: a randomized, double-blind clinical trial. J. Infect. Dis. 209, 1165–1173 (2014).
Giacomet, V. et al. Safety and immunogenicity of a quadrivalent human papillomavirus vaccine in HIV-infected and HIV-negative adolescents and young adults. Vaccine 32, 5657–5661 (2014).
US National Library of Medicine. ClinicalTrials.gov https://www.clinicaltrials.gov/ct2/show/NCT01735006?term=NCT01735006&rank=1 (2017).
US National Library of Medicine. ClinicalTrials.gov https://www.clinicaltrials.gov/ct2/show/NCT02710851?term=NCT02710851&rank=1 (2016).
Kitchener, H. et al. The clinical effectiveness and cost-effectiveness of primary human papillomavirus cervical screening in England: extended follow-up of the ARTISTIC randomised trial cohort through three screening rounds. Health Technol. Assess. 18, 1–196 (2014).
Rodriguez, A. C. et al. Impact of human papillomavirus vaccination on cervical cytology screening, colposcopy, and treatment. Am. J. Epidemiol. 178, 752–760 (2013).
Palmer, T. J. et al. HPV immunisation and cervical screening—confirmation of changed performance of cytology as a screening test in immunised women: a retrospective population-based cohort study. Br. J. Cancer 114, 582–589 (2016). This study illustrates the impact of HPV vaccination on the performance of cytological screening.
Barroeta, J. E., Adhikari-Guragain, D. & Grotkowski, C. E. Cervical cancer screening in the era of HPV vaccination: a review of shifting paradigms in cytopathology. Diagn. Cytopathol. 45, 903–914 (2017).
Kwok, C. S., Gibbs, S., Bennett, C., Holland, R. & Abbott, R. Topical treatments for cutaneous warts. Cochrane Database Syst. Rev. 9, CD001781 (2012).
Vinzon, S. E. & Rosl, F. HPV vaccination for prevention of skin cancer. Hum. Vaccin. Immunother. 11, 353–357 (2015).
Vinzon, S. E. et al. Protective vaccination against papillomavirus-induced skin tumors under immunocompetent and immunosuppressive conditions: a preclinical study using a natural outbred animal model. PLOS Pathog. 10, e1003924 (2014). This study demonstrates that VLP vaccination of infected animals can prevent skin tumours in the Mastomys natalensis papillomavirus (MnPV) model.
Rubio, I. et al. The N-terminal region of the human papillomavirus L2 protein contains overlapping binding sites for neutralizing, cross-neutralizing and non-neutralizing antibodies. Virology 409, 348–359 (2011).
Alphs, H. H. et al. Protection against heterologous human papillomavirus challenge by a synthetic lipopeptide vaccine containing a broadly cross-neutralizing epitope of L2. Proc. Natl Acad. Sci. USA 105, 5850–5855 (2008).
Schellenbacher, C. et al. Efficacy of RG1-VLP vaccination against infections with genital and cutaneous human papillomaviruses. J. Invest. Dermatol. 133, 2706–2713 (2013).
Nieto, K. et al. Development of AAVLP(HPV16/31L2) particles as broadly protective HPV vaccine candidate. PLOS ONE 7, e39741 (2012).
Palmer, K. E. et al. Protection of rabbits against cutaneous papillomavirus infection using recombinant tobacco mosaic virus containing L2 capsid epitopes. Vaccine 24, 5516–5525 (2006).
Tumban, E. et al. Preclinical refinements of a broadly protective VLP-based HPV vaccine targeting the minor capsid protein, L2. Vaccine 33, 3346–3353 (2015).
Rubio, I. et al. Potent anti-HPV immune responses induced by tandem repeats of the HPV16 L2 (20 – 38) peptide displayed on bacterial thioredoxin. Vaccine 27, 1949–1956 (2009).
Kaufmann, A. M. et al. Vaccination trial with HPV16 L1E7 chimeric virus-like particles in women suffering from high grade cervical intraepithelial neoplasia (CIN 2/3). Int. J. Cancer 121, 2794–2800 (2007).
de Jong, A. et al. Enhancement of human papillomavirus (HPV) type 16 E6 and E7-specific T-cell immunity in healthy volunteers through vaccination with TA-CIN, an HPV16 L2E7E6 fusion protein vaccine. Vaccine 20, 3456–3464 (2002).
Daayana, S. et al. Phase II trial of imiquimod and HPV therapeutic vaccination in patients with vulval intraepithelial neoplasia. Br. J. Cancer 102, 1129–1136 (2010).
Opalka, D. et al. Simultaneous quantitation of antibodies to neutralizing epitopes on virus-like particles for human papillomavirus types 6, 11, 16, and 18 by a multiplexed luminex assay. Clin. Diagn. Lab Immunol. 10, 108–115 (2003).
Kirnbauer, R. et al. A virus-like particle enzyme-linked immunosorbent assay detects serum antibodies in a majority of women infected with human papillomavirus type 16. J. Natl Cancer Inst. 86, 494–499 (1994). This study presents the application of L1 VLP enzyme-linked immunosorbent assay (ELISA) for HPV serology.
Pastrana, D. V. et al. Reactivity of human sera in a sensitive, high-throughput pseudovirus-based papillomavirus neutralization assay for HPV16 and HPV18. Virology 321, 205–216 (2004). This study describes a high-throughput, PsV-based neutralization assay.
Kwak, K. et al. Impact of inhibitors and L2 antibodies upon the infectivity of diverse alpha and beta human papillomavirus types. PLOS ONE 9, e97232 (2014).
Conway, M. J., Cruz, L., Alam, S., Christensen, N. D. & Meyers, C. Differentiation-dependent interpentameric disulfide bond stabilizes native human papillomavirus type 16. PLOS ONE 6, e22427 (2011).
Cruz, L., Biryukov, J., Conway, M. J. & Meyers, C. Cleavage of the HPV16 minor capsid protein L2 during virion morphogenesis ablates the requirement for cellular furin during de novo infection. Viruses 7, 5813–5830 (2015).
Conway, M. J., Cruz, L., Alam, S., Christensen, N. D. & Meyers, C. Cross-neutralization potential of native human papillomavirus N-terminal L2 epitopes. PLOS ONE 6, e16405 (2011).
Wang, J. W. et al. Preparation and properties of a papillomavirus infectious intermediate and its utility for neutralization studies. Virology 449, 304–316 (2014).
Wang, J. W. et al. Seroepidemiology of human papillomavirus 16 (HPV16) L2 and generation of L2-specific human chimeric monoclonal antibodies. Clin. Vaccine Immunol. 22, 806–816 (2015).
Roberts, J. N. et al. Genital transmission of HPV in a mouse model is potentiated by nonoxynol-9 and inhibited by carrageenan. Nat. Med. 13, 857–861 (2007).
Mejia, A. F. et al. Preclinical model to test human papillomavirus virus (HPV) capsid vaccines in vivo using infectious HPV/cottontail rabbit papillomavirus chimeric papillomavirus particles. J. Virol. 80, 12393–12397 (2006).
Richards, K. F., Bienkowska-Haba, M., Dasgupta, J., Chen, X. S. & Sapp, M. Multiple heparan sulfate binding site engagements are required for the infectious entry of human papillomavirus type 16. J. Virol. 87, 11426–11437 (2013).
Cruz, L. & Meyers, C. Differential dependence on host cell glycosaminoglycans for infection of epithelial cells by high-risk HPV types. PLOS ONE 8, e68379 (2013).
Culp, T. D., Budgeon, L. R., Marinkovich, M. P., Meneguzzi, G. & Christensen, N. D. Keratinocyte-secreted laminin 5 can function as a transient receptor for human papillomaviruses by binding virions and transferring them to adjacent cells. J. Virol. 80, 8940–8950 (2006).
Richards, R. M., Lowy, D. R., Schiller, J. T. & Day, P. M. Cleavage of the papillomavirus minor capsid protein, L2, at a furin consensus site is necessary for infection. Proc. Natl Acad. Sci. USA 103, 1522–1527 (2006).
Kines, R. C., Thompson, C. D., Lowy, D. R., Schiller, J. T. & Day, P. M. The initial steps leading to papillomavirus infection occur on the basement membrane prior to cell surface binding. Proc. Natl Acad. Sci. USA 106, 20458–20463 (2009).
Day, P. M., Gambhira, R., Roden, R. B., Lowy, D. R. & Schiller, J. T. Mechanisms of human papillomavirus type 16 neutralization by l2 cross-neutralizing and l1 type-specific antibodies. J. Virol. 82, 4638–4646 (2008).
Day, P. M., Lowy, D. R. & Schiller, J. T. Heparan sulfate-independent cell binding and infection with furin-precleaved papillomavirus capsids. J. Virol. 82, 12565–12568 (2008).
DiGiuseppe, S., Bienkowska-Haba, M., Guion, L. G. & Sapp, M. Cruising the cellular highways: How human papillomavirus travels from the surface to the nucleus. Virus Res. 231, 1–9 (2017).
Hanahan, D. & Weinberg, R. A. Hallmarks of cancer: the next generation. Cell 144, 646–674 (2011).
Westrich, J. A., Warren, C. J. & Pyeon, D. Evasion of host immune defenses by human papillomavirus. Virus Res. 231, 21–33 (2017).
Smola, S., Trimble, C. & Stern, P. L. Human papillomavirus-driven immune deviation: challenge and novel opportunity for immunotherapy. Ther. Adv. Vaccines 5, 69–82 (2017).
Roden, R. B. et al. Neutralization of bovine papillomavirus by antibodies to L1 and L2 capsid proteins. J. Virol. 68, 7570–7574 (1994).
Day, P. M. et al. Neutralization of human papillomavirus with monoclonal antibodies reveals different mechanisms of inhibition. J. Virol. 81, 8784–8792 (2007).
Vandepapeliere, P. et al. Randomized controlled trial of an adjuvanted human papillomavirus (HPV) type 6 L2E7 vaccine: infection of external anogenital warts with multiple HPV types and failure of therapeutic vaccination. J. Infect. Dis. 192, 2099–2107 (2005).
Acknowledgements
R.B.S.R. was supported by US Public Health Service grants (grants.nih.gov) from the National Cancer Institute of the National Institutes of Health under awards numbered R01CA118790 and P50CA098252. P.L.S. thanks the University of Manchester and Cancer Research UK for support. The content of this Review is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders had no role in the research performed for this Review, the decision to publish or the preparation of the manuscript. The authors thank M. Stoler for helpful discussions. The authors apologize to the many people whose work they could not cite, or cite indirectly, because of space limitations.
Author information
Authors and Affiliations
Contributions
R.B.S.R. and P.L.S. researched data for the article, made substantial contributions to discussions of the content, wrote the article and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
R.B.S.R. is a member of Papivax, LLC, has Papivax Biotech Inc. stock options and is a member of Papivax Biotech Inc.'s scientific advisory board. Under a licence agreement between PathoVax LLC and Johns Hopkins University, R.B.S.R. is entitled to distributions of payments associated with an invention described in this Review. R.B.S.R. also owns equity in PathoVax LLC and is a member of its scientific advisory board. Under a license agreement between BravoVax and Johns Hopkins University, R.B.S.R. is entitled to distributions of payments associated with an an L2 multimer invention described in this Review. These arrangements have been reviewed and approved by Johns Hopkins University in accordance with its conflict of interest policies. P.L.S. has no competing interests.
Related links
RELATED LINKS
Glossary
- Retromer
-
A complex of proteins that is important for recycling of transmembrane receptors from endosomes to the trans-Golgi network.
- Type-restricted
-
Reactive with the same (homologous) type but not most other types, although weakly cross-reactive with some very closely related types. This contrasts with 'type-specific', which denotes reactivity only to the homologous type.
- Immune deviation
-
Mechanisms that subvert the development of an effective anti-viral immune response, thereby facilitating the establishment of a persistent infection.
- Sterilizing immunity
-
A humoral response that completely neutralizes the viral inoculum such that no infection occurs upon natural exposure.
- Vaccination coverage
-
The per cent of vaccinated individuals in a predefined susceptible population.
- Raft-derived viruses
-
The complete papillomavirus life cycle can be accomplished in vitro using organotypic raft culture, including the production of native virions.
- Opsonization
-
A process, such as antibody binding, by which a pathogen is marked for ingestion and eliminated by phagocytes.
- Quasivirion
-
An infectious virion comprising the papillomavirus capsid that has packaged a heterologous papillomavirus genome, typically produced in 293T cells expressing a human papillomavirus (HPV) capsid delivering a cottontail rabbit papillomavirus genome.
- Herd immunity
-
The indirect protection for individuals who are not immunized that occurs when a large percentage of their surrounding population has become immune through vaccination such that the likelihood of exposure of a vaccine-naive member of the general population to the infectious disease is substantially reduced.
- CIN2/3
-
Moderate and/or high-grade cervical intraepithelial neoplasia, the precursor lesion of cervical cancer and the disease detected by cervical screening with Papanicolaou smear and conformational biopsy.
- Geometric mean titres
-
(GMTs). The simple arithmetic mean of the logarithms of the last positive dilution of each serum that binds to and neutralizes a fixed viral inoculum.
- Biosimilar
-
A type of biological product that is licensed (approved) because it is highly similar to an already approved biological product, known as the biological reference product, and has been shown to have no clinically meaningful differences from the reference product.
- Pseudovirion
-
(PsV). A single round infectious virion comprising the papillomavirus capsid that has packaged a reporter plasmid, typically produced in 293TT cells, and delivering either luciferase or green fluorescent protein (GFP).
- Anamnestic response
-
A more rapid and profound immune response upon re-exposure to an antigen that occurs after initial exposure or vaccination and is driven by immunological memory.
- Breakthrough infection
-
An infection that occurs despite prior vaccination.
Rights and permissions
About this article
Cite this article
Roden, R., Stern, P. Opportunities and challenges for human papillomavirus vaccination in cancer. Nat Rev Cancer 18, 240–254 (2018). https://doi.org/10.1038/nrc.2018.13
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrc.2018.13
This article is cited by
-
Unraveling Emerging Anal Cancer Clinical Biomarkers from Current Immuno-Oncogenomics Advances
Molecular Diagnosis & Therapy (2024)
-
Comprehensive Analysis of the SUMO-related Signature: Implication for Diagnosis, Prognosis, and Immune Therapeutic Approaches in Cervical Cancer
Biochemical Genetics (2024)
-
Exploring the link between viruses and cancer in companion animals: a comprehensive and comparative analysis
Infectious Agents and Cancer (2023)
-
Bioinformatics analysis of immune characteristics in tumors with alternative carcinogenesis pathways induced by human papillomaviruses
Virology Journal (2023)
-
Can prophylactic HPV vaccination reduce the recurrence of cervical lesions after surgery? Review and prospect
Infectious Agents and Cancer (2023)