Abstract
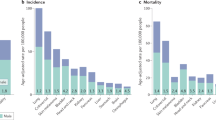
The incidence of many types of cancer arising in organs with non-reproductive functions is significantly higher in male populations than in female populations, with associated differences in survival. Occupational and/or behavioural factors are well-known underlying determinants. However, cellular and molecular differences between the two sexes are also likely to be important. In this Opinion article, we focus on the complex interplay that sex hormones and sex chromosomes can have in intrinsic control of cancer-initiating cell populations, the tumour microenvironment and systemic determinants of cancer development, such as the immune system and metabolism. A better appreciation of these differences between the two sexes could be of substantial value for cancer prevention as well as treatment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2015. CA Cancer J. Clin. 65, 5–29 (2015).
Torre, L. A. et al. Global cancer statistics, 2012. CA Cancer J. Clin. 65, 87–108 (2015).
Rahbari, R., Zhang, L. & Kebebew, E. Thyroid cancer gender disparity. Future Oncol. 6, 1771–1779 (2010).
Ferlay, J. et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 136, E359–E386 (2015).
OuYang, P. Y. et al. The significant survival advantage of female sex in nasopharyngeal carcinoma: a propensity-matched analysis. Br. J. Cancer 112, 1554–1561 (2015).
Wisnivesky, J. P. & Halm, E. A. Sex differences in lung cancer survival: do tumors behave differently in elderly women? J. Clin. Oncol. 25, 1705–1712 (2007).
Dorak, M. T. & Karpuzoglu, E. Gender differences in cancer susceptibility: an inadequately addressed issue. Front. Genet. 3, 268 (2012).
Wang, Y. et al. Effect of luteinizing hormone-induced prohibitin and matrix metalloproteinases on ovarian epithelial tumor cell proliferation. Am. J. Cancer Res. 5, 114–124 (2015).
Mertens-Walker, I., Baxter, R. C. & Marsh, D. J. Gonadotropin signalling in epithelial ovarian cancer. Cancer Lett. 324, 152–159 (2012).
Jacobson, E. M., Hugo, E. R., Borcherding, D. C. & Ben-Jonathan, N. Prolactin in breast and prostate cancer: molecular and genetic perspectives. Discov. Med. 11, 315–324 (2011).
Hartwell, H. J., Petrosky, K. Y., Fox, J. G., Horseman, N. D. & Rogers, A. B. Prolactin prevents hepatocellular carcinoma by restricting innate immune activation of c-Myc in mice. Proc. Natl Acad. Sci. USA 111, 11455–11460 (2014).
Yamamoto, R. et al. Correlation between serum prolactin levels and hepatocellular tumorigenesis induced by 3′-methyl-4-dimethylaminoazobenzene in mice. Br. J. Cancer 72, 17–21 (1995).
Mueller, K. M. et al. Impairment of hepatic growth hormone and glucocorticoid receptor signaling causes steatosis and hepatocellular carcinoma in mice. Hepatology 54, 1398–1409 (2011).
Gabory, A., Attig, L. & Junien, C. Sexual dimorphism in environmental epigenetic programming. Mol. Cell Endocrinol. 304, 8–18 (2009).
Lea, R. W., Dawson, T., Martinez-Moreno, C. G., El-Abry, N. & Harvey, S. Growth hormone and cancer: GH production and action in glioma? Gen. Comp. Endocrinol. 220, 119–123 (2015).
Matsumoto, T. et al. The androgen receptor in health and disease. Annu. Rev. Physiol. 75, 201–224 (2013).
Nugent, B. M. et al. Brain feminization requires active repression of masculinization via DNA methylation. Nat. Neurosci. 18, 690–697 (2015).
Fullwood, M. J. et al. An oestrogen-receptor-α-bound human chromatin interactome. Nature 462, 58–64 (2009).
Melé, M. et al. Human genomics. The human transcriptome across tissues and individuals. Science 348, 660–665 (2015).
Brooks, Y. S. et al. Multifactorial ERβ and NOTCH1 control of squamous differentiation and cancer. J. Clin. Invest. 124, 2260–2276 (2014).
Sugathan, A. & Waxman, D. J. Genome-wide analysis of chromatin states reveals distinct mechanisms of sex-dependent gene regulation in male and female mouse liver. Mol. Cell. Biol. 33, 3594–3610 (2013).
Brisken, C. Progesterone signalling in breast cancer: a neglected hormone coming into the limelight. Nat. Rev. Cancer 13, 385–396 (2013).
Skjefstad, K. et al. The prognostic role of progesterone receptor expression in non-small cell lung cancer patients: gender-related impacts and correlation with disease-specific survival. Steroids 98, 29–36 (2015).
Simon, M. S. et al. Estrogen plus progestin and colorectal cancer incidence and mortality. J. Clin. Oncol. 30, 3983–3990 (2012).
Patrone, C. et al. Regulation of postnatal lung development and homeostasis by estrogen receptor β. Mol. Cell. Biol. 23, 8542–8552 (2003).
Wada-Hiraike, O. et al. Role of estrogen receptor β in colonic epithelium. Proc. Natl Acad. Sci. USA 103, 2959–2964 (2006).
Campbell, L. et al. Estrogen promotes cutaneous wound healing via estrogen receptor β independent of its antiinflammatory activities. J. Exp. Med. 207, 1825–1833 (2010).
Ashcroft, G. S. & Mills, S. J. Androgen receptor-mediated inhibition of cutaneous wound healing. J. Clin. Invest. 110, 615–624 (2002).
Lai, J. J. et al. Monocyte/macrophage androgen receptor suppresses cutaneous wound healing in mice by enhancing local TNF-α expression. J. Clin. Invest. 119, 3739–3751 (2009).
Han, H. J., Heo, J. S. & Lee, Y. J. Estradiol-17β stimulates proliferation of mouse embryonic stem cells: involvement of MAPKs and CDKs as well as protooncogenes. Am. J. Physiol. Cell Physiol. 290, C1067–C1075 (2006).
Strehlow, K. et al. Estrogen increases bone marrow-derived endothelial progenitor cell production and diminishes neointima formation. Circulation 107, 3059–3065 (2003).
Masuda, H. et al. Estrogen-mediated endothelial progenitor cell biology and kinetics for physiological postnatal vasculogenesis. Circ. Res. 101, 598–606 (2007).
Nakada, D. et al. Oestrogen increases haematopoietic stem-cell self-renewal in females and during pregnancy. Nature 505, 555–558 (2014).
Pawluski, J. L., Brummelte, S., Barha, C. K., Crozier, T. M. & Galea, L. A. Effects of steroid hormones on neurogenesis in the hippocampus of the adult female rodent during the estrous cycle, pregnancy, lactation and aging. Front. Neuroendocrinol. 30, 343–357 (2009).
Bayne, S. et al. Estrogen deficiency leads to telomerase inhibition, telomere shortening and reduced cell proliferation in the adrenal gland of mice. Cell Res. 18, 1141–1150 (2008).
Kato, K. et al. Contribution of estrogen receptor α to oncogenic K-Ras-mediated NIH3T3 cell transformation and its implication for escape from senescence by modulating the p53 pathway. J. Biol. Chem. 277, 11217–11224 (2002).
Bain, J. Andropause. Testosterone replacement therapy for aging men. Can. Fam. Physician 47, 91–97 (2001).
Dokal, I. & Vulliamy, T. Dyskeratosis congenita: its link to telomerase and aplastic anaemia. Blood Rev. 17, 217–225 (2003).
Calado, R. T. & Young, N. S. Telomere maintenance and human bone marrow failure. Blood 111, 4446–4455 (2008).
Calado, R. T. et al. Sex hormones, acting on the TERT gene, increase telomerase activity in human primary hematopoietic cells. Blood 114, 2236–2243 (2009).
Fillmore, C. M. et al. Estrogen expands breast cancer stem-like cells through paracrine FGF/Tbx3 signaling. Proc. Natl Acad. Sci. USA 107, 21737–21742 (2010).
Zhang, Y., Eades, G., Yao, Y., Li, Q. & Zhou, Q. Estrogen receptor α signaling regulates breast tumor-initiating cells by down-regulating miR-140 which targets the transcription factor SOX2. J. Biol. Chem. 287, 41514–41522 (2012).
Schroeder, A. et al. Loss of androgen receptor expression promotes a stem-like cell phenotype in prostate cancer through STAT3 signaling. Cancer Res. 74, 1227–1237 (2014).
Huang, C. K., Luo, J., Lee, S. O. & Chang, C. Concise review: androgen receptor differential roles in stem/progenitor cells including prostate, embryonic, stromal, and hematopoietic lineages. Stem Cells 32, 2299–2308 (2014).
Shim, G. J. et al. Disruption of the estrogen receptor β gene in mice causes myeloproliferative disease resembling chronic myeloid leukemia with lymphoid blast crisis. Proc. Natl Acad. Sci. USA 100, 6694–6699 (2003).
Jorgensen, H. G. & Holyoake, T. L. A comparison of normal and leukemic stem cell biology in chronic myeloid leukemia. Hematol. Oncol. 19, 89–106 (2001).
Berger, U. et al. Gender aspects in chronic myeloid leukemia: long-term results from randomized studies. Leukemia 19, 984–989 (2005).
Ohlund, D., Elyada, E. & Tuveson, D. Fibroblast heterogeneity in the cancer wound. J. Exp. Med. 211, 1503–1523 (2014).
Slavin, S. et al. Estrogen receptor α in cancer-associated fibroblasts suppresses prostate cancer invasion via modulation of thrombospondin 2 and matrix metalloproteinase 3. Carcinogenesis 35, 1301–1309 (2014).
Lai, K. P., Yamashita, S., Huang, C. K., Yeh, S. & Chang, C. Loss of stromal androgen receptor leads to suppressed prostate tumourigenesis via modulation of pro-inflammatory cytokines/chemokines. EMBO Mol. Med. 4, 791–807 (2012).
Leach, D. A. et al. Stromal androgen receptor regulates the composition of the microenvironment to influence prostate cancer outcome. Oncotarget 6, 16135–16150 (2015).
Gupta, P. B. et al. Systemic stromal effects of estrogen promote the growth of estrogen receptor-negative cancers. Cancer Res. 67, 2062–2071 (2007).
Pequeux, C. et al. Stromal estrogen receptor-α promotes tumor growth by normalizing an increased angiogenesis. Cancer Res. 72, 3010–3019 (2012).
den Boon, J. A. et al. Molecular transitions from papillomavirus infection to cervical precancer and cancer: role of stromal estrogen receptor signaling. Proc. Natl Acad. Sci. USA 112, E3255–E3264 (2015).
Ellem, S. J. & Risbridger, G. P. Treating prostate cancer: a rationale for targeting local oestrogens. Nat. Rev. Cancer 7, 621–627 (2007).
McPherson, S. J. et al. Estrogen receptor-β activated apoptosis in benign hyperplasia and cancer of the prostate is androgen independent and TNFα mediated. Proc. Natl Acad. Sci. USA 107, 3123–3128 (2010).
Hamada, H. et al. Estrogen receptors α and β mediate contribution of bone marrow-derived endothelial progenitor cells to functional recovery after myocardial infarction. Circulation 114, 2261–2270 (2006).
Seo, K. H. et al. Estrogen enhances angiogenesis through a pathway involving platelet-activating factor-mediated nuclear factor-κB activation. Cancer Res. 64, 6482–6488 (2004).
Stoner, M. et al. Estrogen regulation of vascular endothelial growth factor gene expression in ZR-75 breast cancer cells through interaction of estrogen receptor α and SP proteins. Oncogene 23, 1052–1063 (2004).
Hartman, J. et al. Estrogen receptor β inhibits angiogenesis and growth of T47D breast cancer xenografts. Cancer Res. 66, 11207–11213 (2006).
Sieveking, D. P. et al. A sex-specific role for androgens in angiogenesis. J. Exp. Med. 207, 345–352 (2010).
Yoshida, S. et al. Androgen receptor promotes sex-independent angiogenesis in response to ischemia and is required for activation of vascular endothelial growth factor receptor signaling. Circulation 128, 60–71 (2013).
Cai, J. et al. Androgen stimulates endothelial cell proliferation via an androgen receptor/VEGF/cyclin A-mediated mechanism. Am. J. Physiol. Heart Circ. Physiol. 300, H1210–H1221 (2011).
Dotto, G. P. Multifocal epithelial tumors and field cancerization: stroma as a primary determinant. J. Clin. Invest. 124, 1446–1453 (2014).
Campbell, L. et al. Estrogen receptor-alpha promotes alternative macrophage activation during cutaneous repair. J. Invest. Dermatol. 134, 2447–2457 (2014).
Yang, W. et al. Estrogen represses hepatocellular carcinoma (HCC) growth via inhibiting alternative activation of tumor-associated macrophages (TAMs). J. Biol. Chem. 287, 40140–40149 (2012).
Fang, L. Y. et al. Infiltrating macrophages promote prostate tumorigenesis via modulating androgen receptor-mediated CCL4–STAT3 signaling. Cancer Res. 73, 5633–5646 (2013).
Fish, E. N. The X-files in immunity: sex-based differences predispose immune responses. Nat. Rev. Immunol. 8, 737–744 (2008).
Lai, J. J. et al. Androgen receptor influences on body defense system via modulation of innate and adaptive immune systems: lessons from conditional AR knockout mice. Am. J. Pathol. 181, 1504–1512 (2012).
Templeton, A. J. et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J. Natl Cancer Inst. 106, dju124 (2014).
Whitacre, C. C. Sex differences in autoimmune disease. Nat. Immunol. 2, 777–780 (2001).
von Boehmer, H. & Daniel, C. Therapeutic opportunities for manipulating TReg cells in autoimmunity and cancer. Nat. Rev. Drug Discov. 12, 51–63 (2013).
Nie, J., Li, Y. Y., Zheng, S. G., Tsun, A. & Li, B. FOXP3+ Treg cells and gender bias in autoimmune diseases. Front. Immunol. 6, 493 (2015).
Bacchetta, R. et al. Defective regulatory and effector T cell functions in patients with FOXP3 mutations. J. Clin. Invest. 116, 1713–1722 (2006).
Bennett, C. L. et al. The immune dysregulation, polyendocrinopathy, enteropathy, X-linked syndrome (IPEX) is caused by mutations of FOXP3. Nat. Genet. 27, 20–21 (2001).
Polanczyk, M. J. et al. Cutting edge: estrogen drives expansion of the CD4+CD25+ regulatory T cell compartment. J. Immunol. 173, 2227–2230 (2004).
Walecki, M. et al. Androgen receptor modulates Foxp3 expression in CD4+CD25+Foxp3+ regulatory T-cells. Mol. Biol. Cell 26, 2845–2857 (2015).
Yang, X. O. et al. Molecular antagonism and plasticity of regulatory and inflammatory T cell programs. Immunity 29, 44–56 (2008).
Wen, L. et al. Innate immunity and intestinal microbiota in the development of Type 1 diabetes. Nature 455, 1109–1113 (2008).
Markle, J. G. et al. Sex differences in the gut microbiome drive hormone-dependent regulation of autoimmunity. Science 339, 1084–1088 (2013).
Yurkovetskiy, L. et al. Gender bias in autoimmunity is influenced by microbiota. Immunity 39, 400–412 (2013).
Garrett, W. S. Cancer and the microbiota. Science 348, 80–86 (2015).
Sloan, J. A. et al. Women experience greater toxicity with fluorouracil-based chemotherapy for colorectal cancer. J. Clin. Oncol. 20, 1491–1498 (2002).
Singh, S. et al. Influence of sex on toxicity and treatment outcome in small-cell lung cancer. J. Clin. Oncol. 23, 850–856 (2005).
Bianchi, I., Lleo, A., Gershwin, M. E. & Invernizzi, P. The X chromosome and immune associated genes. J. Autoimmun. 38, J187–J192 (2012).
Dai, R. & Ahmed, S. A. Sexual dimorphism of miRNA expression: a new perspective in understanding the sex bias of autoimmune diseases. Ther. Clin. Risk Manag. 10, 151–163 (2014).
Hewagama, A. et al. Overexpression of X-linked genes in T cells from women with lupus. J. Autoimmun. 41, 60–71 (2013).
Barros, R. P. & Gustafsson, J. A. Estrogen receptors and the metabolic network. Cell Metab. 14, 289–299 (2011).
Mauvais-Jarvis, F. Estrogen and androgen receptors: regulators of fuel homeostasis and emerging targets for diabetes and obesity. Trends Endocrinol. Metab. 22, 24–33 (2011).
Calle, E. E. & Kaaks, R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat. Rev. Cancer 4, 579–591 (2004).
Tisdale, M. J. Cachexia in cancer patients. Nat. Rev. Cancer 2, 862–871 (2002).
Baracos, V. E., Reiman, T., Mourtzakis, M., Gioulbasanis, I. & Antoun, S. Body composition in patients with non-small cell lung cancer: a contemporary view of cancer cachexia with the use of computed tomography image analysis. Am. J. Clin. Nutr. 91, 1133S–1137S (2010).
Cosper, P. F. & Leinwand, L. A. Cancer causes cardiac atrophy and autophagy in a sexually dimorphic manner. Cancer Res. 71, 1710–1720 (2011).
von Haehling, S., Morley, J. E. & Anker, S. D. An overview of sarcopenia: facts and numbers on prevalence and clinical impact. J. Cachexia Sarcopenia Muscle 1, 129–133 (2010).
Vigano, A. et al. Male hypogonadism associated with advanced cancer: a systematic review. Lancet Oncol. 11, 679–684 (2010).
Basaria, S. Male hypogonadism. Lancet 383, 1250–1263 (2014).
Dobs, A. S. et al. Effects of enobosarm on muscle wasting and physical function in patients with cancer: a double-blind, randomised controlled Phase 2 trial. Lancet Oncol. 14, 335–345 (2013).
Li, Z., Tuteja, G., Schug, J. & Kaestner, K. H. Foxa1 and Foxa2 are essential for sexual dimorphism in liver cancer. Cell 148, 72–83 (2012).
Naugler, W. E. et al. Gender disparity in liver cancer due to sex differences in MyD88-dependent IL-6 production. Science 317, 121–124 (2007).
Li, Z. et al. Foxa1 and Foxa2 regulate bile duct development in mice. J. Clin. Invest. 119, 1537–1545 (2009).
Matic, M. et al. Estrogen signalling and the metabolic syndrome: targeting the hepatic estrogen receptor alpha action. PLoS ONE 8, e57458 (2013).
Yamamoto, R., Tatsuta, M. & Terada, N. Suppression by oestrogen of hepatocellular tumourigenesis induced in mice by 3′-methyl-4-dimethylaminoazobenzene. Br. J. Cancer 68, 303–307 (1993).
Porsch Hallstrom, I., Svensson, D. & Blanck, A. Sex-differentiated deoxycholic acid promotion of rat liver carcinogenesis is under pituitary control. Carcinogenesis 12, 2035–2040 (1991).
Kerrigan, J. R. & Rogol, A. D. The impact of gonadal steroid hormone action on growth hormone secretion during childhood and adolescence. Endocr. Rev. 13, 281–298 (1992).
Mode, A. & Gustafsson, J. A. Sex and the liver — a journey through five decades. Drug Metab. Rev. 38, 197–207 (2006).
Herrington, J., Smit, L. S., Schwartz, J. & Carter-Su, C. The role of STAT proteins in growth hormone signaling. Oncogene 19, 2585–2597 (2000).
Di Bisceglie, A. M. Hepatitis B and hepatocellular carcinoma. Hepatology 49, S56–S60 (2009).
Yu, C. P. et al. Estrogen inhibits renal cell carcinoma cell progression through estrogen receptor-beta activation. PLoS ONE 8, e56667 (2013).
Passarelli, M. N. et al. Common single-nucleotide polymorphisms in the estrogen receptor β promoter are associated with colorectal cancer survival in postmenopausal women. Cancer Res. 73, 767–775 (2013).
Press, O. A. et al. Gender-related survival differences associated with EGFR polymorphisms in metastatic colon cancer. Cancer Res. 68, 3037–3042 (2008).
Schmidt, A. N., Nanney, L. B., Boyd, A. S., King, L. E. Jr & Ellis, D. L. Oestrogen receptor-β expression in melanocytic lesions. Exp. Dermatol. 15, 971–980 (2006).
Matsuoka, H. et al. Tamoxifen inhibits tumor cell invasion and metastasis in mouse melanoma through suppression of PKC/MEK/ERK and PKC/PI3K/Akt pathways. Exp. Cell Res. 315, 2022–2032 (2009).
Hartman, J. et al. Tumor repressive functions of estrogen receptor β in SW480 colon cancer cells. Cancer Res. 69, 6100–6106 (2009).
Sareddy, G. R. et al. Therapeutic significance of estrogen receptor β agonists in gliomas. Mol. Cancer Ther. 11, 1174–1182 (2012).
Pinton, G. et al. Estrogen receptor-β affects the prognosis of human malignant mesothelioma. Cancer Res. 69, 4598–4604 (2009).
Yakimchuk, K. et al. Effect of ligand-activated estrogen receptor β on lymphoma growth in vitro and in vivo. Leukemia 25, 1103–1110 (2011).
Stanley, J. A. et al. Androgen receptor expression in human thyroid cancer tissues: a potential mechanism underlying the gender bias in the incidence of thyroid cancers. J. Steroid Biochem. Mol. Biol. 130, 105–124 (2012).
Lee, M. L. et al. Induction of thyroid papillary carcinoma cell proliferation by estrogen is associated with an altered expression of Bcl-xL. Cancer J. 11, 113–121 (2005).
Sarma, K. et al. ATRX directs binding of PRC2 to Xist RNA and Polycomb targets. Cell 159, 869–883 (2014).
Minajigi, A. et al. Chromosomes. A comprehensive Xist interactome reveals cohesin repulsion and an RNA-directed chromosome conformation. Science 349, aab2276 (2015).
Migeon, B. R. The role of X inactivation and cellular mosaicism in women's health and sex-specific diseases. JAMA 295, 1428–1433 (2006).
Kawakami, T. et al. Characterization of loss-of-inactive X in Klinefelter syndrome and female-derived cancer cells. Oncogene 23, 6163–6169 (2004).
Benoit, M. H. et al. Global analysis of chromosome X gene expression in primary cultures of normal ovarian surface epithelial cells and epithelial ovarian cancer cell lines. Int. J. Oncol. 30, 5–17 (2007).
Yildirim, E. et al. Xist RNA is a potent suppressor of hematologic cancer in mice. Cell 152, 727–742 (2013).
Yao, Y. et al. Knockdown of long non-coding RNA XIST exerts tumor-suppressive functions in human glioblastoma stem cells by up-regulating miR-152. Cancer Lett. 359, 75–86 (2015).
Kawakami, T. et al. The roles of supernumerical X chromosomes and XIST expression in testicular germ cell tumors. J. Urol. 169, 1546–1552 (2003).
Bellott, D. W. et al. Mammalian Y chromosomes retain widely expressed dosage-sensitive regulators. Nature 508, 494–499 (2014).
Walport, L. J. et al. Human UTY(KDM6C) is a male-specific N-methyl lysyl demethylase. J. Biol. Chem. 289, 18302–18313 (2014).
Mar, B. G. et al. Sequencing histone-modifying enzymes identifies UTX mutations in acute lymphoblastic leukemia. Leukemia 26, 1881–1883 (2012).
Ntziachristos, P. et al. Contrasting roles of histone 3 lysine 27 demethylases in acute lymphoblastic leukaemia. Nature 514, 513–517 (2014).
Van der Meulen, J. et al. The H3K27me3 demethylase UTX is a gender-specific tumor suppressor in T-cell acute lymphoblastic leukemia. Blood 125, 13–21 (2015).
Van Vlierberghe, P. et al. PHF6 mutations in T-cell acute lymphoblastic leukemia. Nat. Genet. 42, 338–342 (2010).
De Keersmaecker, K. et al. Exome sequencing identifies mutation in CNOT3 and ribosomal genes RPL5 and RPL10 in T-cell acute lymphoblastic leukemia. Nat. Genet. 45, 186–190 (2013).
van Haaften, G. et al. Somatic mutations of the histone H3K27 demethylase gene UTX in human cancer. Nat. Genet. 41, 521–523 (2009).
Dalgliesh, G. L. et al. Systematic sequencing of renal carcinoma reveals inactivation of histone modifying genes. Nature 463, 360–363 (2010).
Northcott, P. A. et al. Medulloblastomics: the end of the beginning. Nat. Rev. Cancer 12, 818–834 (2012).
Robinson, G. et al. Novel mutations target distinct subgroups of medulloblastoma. Nature 488, 43–48 (2012).
Jiang, L. et al. Exome sequencing identifies somatic mutations of DDX3X in natural killer/T-cell lymphoma. Nat. Genet. 47, 1061–1066 (2015).
Wu, D. W. et al. DDX3 loss by p53 inactivation promotes tumor malignancy via the MDM2/Slug/E-cadherin pathway and poor patient outcome in non-small-cell lung cancer. Oncogene 33, 1515–1526 (2014).
Huff, V. Wilms' tumours: about tumour suppressor genes, an oncogene and a chameleon gene. Nat. Rev. Cancer 11, 111–121 (2011).
Rondinelli, B. et al. Histone demethylase JARID1C inactivation triggers genomic instability in sporadic renal cancer. J. Clin. Invest. 125, 4625–4637 (2015).
Karanikas, V. et al. Foxp3 expression in human cancer cells. J. Transl. Med. 6, 19 (2008).
Hinz, S. et al. Foxp3 expression in pancreatic carcinoma cells as a novel mechanism of immune evasion in cancer. Cancer Res. 67, 8344–8350 (2007).
Liu, R. et al. FOXP3 controls an miR-146/NF-κB negative feedback loop that inhibits apoptosis in breast cancer cells. Cancer Res. 75, 1703–1713 (2015).
Liu, R. et al. FOXP3-miR-146-NF-κB axis and therapy for precancerous lesions in prostate. Cancer Res. 75, 1714–1724 (2015).
le Sage, C. et al. Regulation of the p27 (Kip1) tumor suppressor by miR-221 and miR-222 promotes cancer cell proliferation. EMBO J. 26, 3699–3708 (2007).
Li, X. et al. miRNA-223 promotes gastric cancer invasion and metastasis by targeting tumor suppressor EPB41L3. Mol. Cancer Res. 9, 824–833 (2011).
Hui, A. B. et al. Potentially prognostic miRNAs in HPV-associated oropharyngeal carcinoma. Clin. Cancer Res. 19, 2154–2162 (2013).
Singhal, R., Bard, J. E., Nowak, N. J., Buck, M. J. & Kandel, E. S. FOXO1 regulates expression of a microRNA cluster on X chromosome. Aging (Albany NY) 5, 347–356 (2013).
Nadal, M. et al. Aneuploidy of chromosome Y in prostate tumors and seminal vesicles: a possible sign of aging rather than an indicator of carcinogenesis? Mol. Carcinog. 46, 543–552 (2007).
Konig, J. J., Teubel, W., Romijn, J. C., Schroder, F. H. & Hagemeijer, A. Gain and loss of chromosomes 1, 7, 8, 10, 18, and Y in 46 prostate cancers. Hum. Pathol. 27, 720–727 (1996).
Stahl, P. R. et al. Y chromosome losses are exceedingly rare in prostate cancer and unrelated to patient age. Prostate 72, 898–903 (2012).
Kowalski, J. et al. Chromosomal abnormalities of adenocarcinoma of the pancreas: identifying early and late changes. Cancer Genet. Cytogenet. 178, 26–35 (2007).
Bottarelli, L. et al. Sex chromosome alterations associate with tumor progression in sporadic colorectal carcinomas. Clin. Cancer Res. 13, 4365–4370 (2007).
Fadl-Elmula, I. et al. Karyotypic characterization of urinary bladder transitional cell carcinomas. Genes Chromosomes Cancer 29, 256–265 (2000).
Mitelman, F., Johansson, B. & Mertens, F. Mitelman Database of Chromosome Aberrations and Gene Fusions in Cancer. Cancer Gene Anatomy Project (online), (2016).
Forsberg, L. A. et al. Mosaic loss of chromosome Y in peripheral blood is associated with shorter survival and higher risk of cancer. Nat. Genet. 46, 624–628 (2014).
Dumanski, J. P. et al. Mutagenesis. Smoking is associated with mosaic loss of chromosome Y. Science 347, 81–83 (2015).
Bianchi, N. O. Y chromosome structural and functional changes in human malignant diseases. Mutat. Res. 682, 21–27 (2009).
Kido, T. & Lau, Y. F. Roles of the Y chromosome genes in human cancers. Asian J. Androl. 17, 373–380 (2015).
Murakami, S. et al. SRY and OCT4 are required for the acquisition of cancer stem cell-like properties and are potential differentiation therapy targets. Stem Cells 33, 2652–2663 (2015).
Murakami, S. et al. The male-specific factor Sry harbors an oncogenic function. Oncogene 33, 2978–2986 (2014).
Collignon, J. et al. A comparison of the properties of Sox-3 with Sry and two related genes, Sox-1 and Sox-2. Development 122, 509–520 (1996).
Boumahdi, S. et al. SOX2 controls tumour initiation and cancer stem-cell functions in squamous-cell carcinoma. Nature 511, 246–250 (2014).
Yuan, X., Lu, M. L., Li, T. & Balk, S. P. SRY interacts with and negatively regulates androgen receptor transcriptional activity. J. Biol. Chem. 276, 46647–46654 (2001).
Lau, Y. F., Li, Y. & Kido, T. Gonadoblastoma locus and the TSPY gene on the human Y chromosome. Birth Defects Res. C Embryo Today 87, 114–122 (2009).
Kido, T., Hatakeyama, S., Ohyama, C. & Lau, Y. F. Expression of the Y-encoded TSPY is associated with progression of prostate cancer. Genes (Basel) 1, 283–293 (2010).
Kido, T. et al. The potential contributions of a Y-located protooncogene and its X homologue in sexual dimorphisms in hepatocellular carcinoma. Hum. Pathol. 45, 1847–1858 (2014).
Delbridge, M. L. et al. TSPY, the candidate gonadoblastoma gene on the human Y chromosome, has a widely expressed homologue on the X - implications for Y chromosome evolution. Chromosome Res. 12, 345–356 (2004).
Kido, T., Ou, J. H. & Lau, Y. F. The X-linked tumor suppressor TSPX interacts and promotes degradation of the hepatitis B viral protein HBx via the proteasome pathway. PLoS ONE 6, e22979 (2011).
Li, S. et al. Over-expressed testis-specific protein Y-encoded 1 as a novel biomarker for male hepatocellular carcinoma. PLoS ONE 9, e89219 (2014).
Lau, Y. F. & Zhang, J. Expression analysis of thirty one Y chromosome genes in human prostate cancer. Mol. Carcinog. 27, 308–321 (2000).
Tsuei, D. J. et al. RBMY, a male germ cell-specific RNA-binding protein, activated in human liver cancers and transforms rodent fibroblasts. Oncogene 23, 5815–5822 (2004).
Tsuei, D. J. et al. Male germ cell-specific RNA binding protein RBMY: a new oncogene explaining male predominance in liver cancer. PLoS ONE 6, e26948 (2011).
Potter, J. D. Morphogens, morphostats, microarchitecture and malignancy. Nat. Rev. Cancer 7, 464–474 (2007).
Tomasetti, C. & Vogelstein, B. Cancer etiology. Variation in cancer risk among tissues can be explained by the number of stem cell divisions. Science 347, 78–81 (2015).
Sottoriva, A. et al. A Big Bang model of human colorectal tumor growth. Nat. Genet. 47, 209–216 (2015).
Martincorena, I. et al. Tumor evolution. High burden and pervasive positive selection of somatic mutations in normal human skin. Science 348, 880–886 (2015).
Cardiff, R. D. & Borowsky, A. D. Precancer: sequentially acquired or predetermined? Toxicol. Pathol. 38, 171–179 (2010).
Gatenby, R. Perspective: finding cancer's first principles. Nature 491, S55 (2012).
Merlo, L. M., Pepper, J. W., Reid, B. J. & Maley, C. C. Cancer as an evolutionary and ecological process. Nat. Rev. Cancer 6, 924–935 (2006).
Sharma, P. & Allison, J. P. The future of immune checkpoint therapy. Science 348, 56–61 (2015).
Scoggins, C. R. et al. Gender-related differences in outcome for melanoma patients. Ann. Surg. 243, 693–698; discussion 698–700 (2006).
Austad, S. N. Why women live longer than men: sex differences in longevity. Gend. Med. 3, 79–92 (2006).
Thornton, M. J. Estrogens and aging skin. Dermatoendocrinol. 5, 264–270 (2013).
Paterni, I., Granchi, C., Katzenellenbogen, J. A. & Minutolo, F. Estrogen receptors alpha (ERα) and beta (ERβ): subtype-selective ligands and clinical potential. Steroids 90, 13–29 (2014).
Taplin, M. E. Drug insight: role of the androgen receptor in the development and progression of prostate cancer. Nat. Clin. Pract. Oncol. 4, 236–244 (2007).
Ahuja, N., Sharma, A. R. & Baylin, S. B. Epigenetic therapeutics: a new weapon in the war against cancer. Annu. Rev. Med. 67, 73–89 (2016).
Acknowledgements
This work was supported by grants from Swiss National Science Foundation (310030_156191/1), US National Institutes of Health (NIH; R01AR039190; R01AR064786; the content not necessarily representing the official views of NIH), European Research Council (26075083) and OncoSuisse (OCS-2922-02-2012). A.C. is supported by an AIRC-EU FP7 Marie Curie Fellowship granted by the Italian Association for Cancer Research and the European Union FP7 Marie Curie Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Related links
Supplementary information
41568_2016_BFnrc201630_MOESM212_ESM.pdf
Supplementary information S1 (table) | Representative list of X-linked microRNAs and protein coding genes associated with cancer development (PDF 775 kb)
Rights and permissions
About this article
Cite this article
Clocchiatti, A., Cora, E., Zhang, Y. et al. Sexual dimorphism in cancer. Nat Rev Cancer 16, 330–339 (2016). https://doi.org/10.1038/nrc.2016.30
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrc.2016.30
This article is cited by
-
Effect of sex on psychological distress and fatigue over time in a prospective cohort of cancer survivors
Journal of Cancer Survivorship (2024)
-
Is metabolism the magic bullet for targeted cancer therapy?
BMC Cancer (2023)
-
Chronic conditions in women: the development of a National Institutes of health framework
BMC Women's Health (2023)
-
Sex specific regulation of TSPY-Like 2 in the DNA damage response of cancer cells
Cell Death & Disease (2023)
-
Ibrutinib in mantle cell lymphoma: a real-world retrospective multi-center analysis of 77 patients treated in the Czech Republic
Annals of Hematology (2023)