Abstract
This protocol describes targetable reactive electrophiles and oxidants (T-REX)—a live-cell-based tool designed to (i) interrogate the consequences of specific and time-resolved redox events, and (ii) screen for bona fide redox-sensor targets. A small-molecule toolset comprising photocaged precursors to specific reactive redox signals is constructed such that these inert precursors specifically and irreversibly tag any HaloTag-fused protein of interest (POI) in mammalian and Escherichia coli cells. Syntheses of the alkyne-functionalized endogenous reactive signal 4-hydroxynonenal (HNE(alkyne)) and the HaloTag-targetable photocaged precursor to HNE(alkyne) (also known as Ht-PreHNE or HtPHA) are described. Low-energy light prompts photo-uncaging (t1/2 <1–2 min) and target-specific modification. The targeted modification of the POI enables precisely timed and spatially controlled redox events with no off-target modification. Two independent pathways are described, along with a simple setup to functionally validate known targets or discover novel sensors. T-REX sidesteps mixed responses caused by uncontrolled whole-cell swamping with reactive signals. Modification and downstream response can be analyzed by in-gel fluorescence, proteomics, qRT-PCR, immunofluorescence, fluorescence resonance energy transfer (FRET)-based and dual-luciferase reporters, or flow cytometry assays. T-REX targeting takes 4 h from initial probe treatment. Analysis of targeted redox responses takes an additional 4–24 h, depending on the nature of the pathway and the type of readouts used.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout










Similar content being viewed by others
Change history
10 November 2016
In the version of this article initially published online, there were three errors. (1) In the Reagent Setup, the instructions for preparing LB-ampicillin-chloramphenicol medium gave an incorrect concentration for ampicillin; it should read "100 μg/ml ampicillin." (2) The text for Step 11B(vi) incorrectly described the bromination procedure; it should read: "Brominate 0.35 g of the resulting alcohol 6 (1.4 mmol) in 20 ml of distilled DCM at 4 °C by adding 0.5 g of CBr4 (1.54 mmol) and 0.44 g of PPh3 (1.68 mmol). Stir the mixture for 15 min" (instead of "...by adding 0.5 g of CBr4 (1.54 mmol) and 0.44 g of PPh3 (1.68 mmol) to 20 ml of distilled DCM at 0 °C"). (3) In Figure 10, under the arrow between compounds 12 and 13, the label "(ii) Me2S" should be omitted. These errors have been corrected for all versions of the article.
References
Jacob, C. & Winyard\, P.G. Redox Signaling and Regulation in Biology and Medicine (Wiley-VCH, 2009).
Stadtman, E.R. Protein oxidation and aging. Science 257, 1220–1224 (1992).
Schopfer, F.J., Cipollina, C. & Freeman, B.A. Formation and signaling actions of electrophilic lipids. Chem. Rev. 111, 5997–6021 (2011).
Winterbourn, C.C. Reconciling the chemistry and biology of reactive oxygen species. Nat. Chem. Biol. 4, 278–286 (2008).
Murphy, M.P. et al. Unraveling the biological roles of reactive oxygen species. Cell Metab. 13, 361–366 (2011).
Holmstrom, K.M. & Finkel, T. Cellular mechanisms and physiological consequences of redox-dependent signalling. Nat. Rev. Mol. Cell Biol. 15, 411–421 (2014).
Jacobs, A.T. & Marnett, L.J. Systems analysis of protein modification and cellular responses induced by electrophile stress. Acc. Chem. Res. 43, 673–683 (2010).
Delmastro-Greenwood, M., Freeman, B.A. & Wendell, S.G. Redox-dependent anti-inflammatory signaling actions of unsaturated fatty acids. Annu. Rev. Physiol. 76, 79–105 (2014).
Crunkhorn, S. Deal watch: Abbott boosts investment in NRF2 activators for reducing oxidative stress. Nat. Rev. Drug Discov. 11, 96 (2012).
Dinkova-Kostova, A.T. & Kostov, R.V. Glucosinolates and isothiocyanates in health and disease. Trends Mol. Med. 18, 337–347 (2012).
Gupta, S.C., Patchva, S. & Aggarwal, B.B. Therapeutic roles of curcumin: lessons learned from clinical trials. AAPS J. 15, 195–218 (2013).
Fernandez-Fernandez, B., Ortiz, A., Gomez-Guerrero, C. & Egido, J. Therapeutic approaches to diabetic nephropathy--beyond the RAS. Nat. Rev. Nephrol. 10, 325–346 (2014).
Bomprezzi, R. Dimethyl fumarate in the treatment of relapsing–remitting multiple sclerosis: an overview. Ther. Adv. Neurol. Disord. 8, 20–30 (2015).
Hermann, C., Zeiher, A.M. & Dimmeler, S. Shear stress inhibits H2O2-induced apoptosis of human endothelial cells by modulation of the glutathione redox cycle and nitric oxide synthase. Arterioscler Thromb. Vasc. Biol. 17, 3588–3592 (1997).
De Keulenaer, G.W. et al. Oscillatory and steady laminar shear stress differentially affect human endothelial redox state: role of a superoxide-producing NADH oxidase. Circ. Res. 82, 1094–1101 (1998).
Cunningham, K.S. & Gotlieb, A.I. The role of shear stress in the pathogenesis of atherosclerosis. Lab. Invest. 85, 9–23 (2005).
Kim, S.K., Woodcroft, K.J., Oh, S.J., Abdelmegeed, M.A. & Novak, R.F. Role of mechanical and redox stress in activation of mitogen-activated protein kinases in primary cultured rat hepatocytes. Biochem. Pharmacol. 70, 1785–1795 (2005).
Lehoux, S. Redox signalling in vascular responses to shear and stretch. Cardiovasc Res. 71, 269–279 (2006).
Sundaresan, M., Yu, Z.X., Ferrans, V.J., Irani, K. & Finkel, T. Requirement for generation of H2O2 for platelet-derived growth factor signal transduction. Science 270, 296–299 (1995).
Bae, Y.S., Oh, H., Rhee, S.G. & Yoo, Y.D. Regulation of reactive oxygen species generation in cell signaling. Mol. Cells 32, 491–509 (2011).
Schieber, M. & Chandel, N.S. ROS function in redox signaling and oxidative stress. Curr. Biol. 24, R453–462 (2014).
Brewer, T.F., Garcia, F.J., Onak, C.S., Carroll, K.S. & Chang, C.J. Chemical approaches to discovery and study of sources and targets of hydrogen peroxide redox signaling through NADPH oxidase proteins. Annu. Rev. Biochem. 84, 765–790 (2015).
Brownlee, M. Biochemistry and molecular cell biology of diabetic complications. Nature 414, 813–820 (2001).
Green, K., Brand, M.D. & Murphy, M.P. Prevention of mitochondrial oxidative damage as a therapeutic strategy in diabetes. Diabetes 53 (Suppl. 1), S110–S118 (2004).
Nishikawa, T. & Araki, E. Impact of mitochondrial ROS production in the pathogenesis of diabetes mellitus and its complications. Antioxid. Redox Signal. 9, 343–353 (2007).
Weerapana, E. et al. Quantitative reactivity profiling predicts functional cysteines in proteomes. Nature 468, 790–795 (2010).
Codreanu, S.G. et al. Alkylation damage by lipid electrophiles targets functional protein systems. Mol. Cell. Proteomics 13, 849–859 (2014).
Wang, C., Weerapana, E., Blewett, M.M. & Cravatt, B.F. A chemoproteomic platform to quantitatively map targets of lipid-derived electrophiles. Nat. Methods 11, 79–85 (2014).
Niphakis, M.J. et al. A global map of lipid-binding proteins and their ligandability in cells. Cell 161, 1668–1680 (2015).
Yang, J., Tallman, K.A., Porter, N.A. & Liebler, D.C. Quantitative chemoproteomics for site-specific analysis of protein alkylation by 4-hydroxy-2-nonenal in cells. Anal. Chem. 87, 2535–2541 (2015).
Kim, H.Y., Tallman, K.A., Liebler, D.C. & Porter, N.A. An azido-biotin reagent for use in the isolation of protein adducts of lipid-derived electrophiles by streptavidin catch and photorelease. Mol. Cell Proteomics 8, 2080–2089 (2009).
Furdui, C.M. & Poole, L.B. Chemical approaches to detect and analyze protein sulfenic acids. Mass Spectrom. Rev. 33, 126–146 (2014).
Yang, J., Carroll, K.S. & Liebler, D.C. The expanding landscape of the thiol redox proteome. Mol. Cell Proteomics 15, 1–11 (2016).
Codreanu, S.G., Zhang, B., Sobecki, S.M., Billheimer, D.D. & Liebler, D.C. Global analysis of protein damage by the lipid electrophile 4-hydroxy-2-nonenal. Mol. Cell Proteomics 8, 670–680 (2009).
Rossi, A. et al. Anti-inflammatory cyclopentenone prostaglandins are direct inhibitors of IkappaB kinase. Nature 403, 103–108 (2000).
Straus, D.S. et al. 15-deoxy-delta 12,14-prostaglandin J2 inhibits multiple steps in the NF-kappa B signaling pathway. Proc. Natl. Acad. Sci. USA 97, 4844–4849 (2000).
Ji, C., Kozak, K.R. & Marnett, L.J. IkappaB kinase, a molecular target for inhibition by 4-hydroxy-2-nonenal. J. Biol. Chem. 276, 18223–18228 (2001).
Rudolph, T.K. & Freeman, B.A. Transduction of redox signaling by electrophile-protein reactions. Sci. Signal. 2, re7 (2009).
Diab, A. et al. Peroxisome proliferator-activated receptor-gamma agonist 15-deoxy-Delta(12,14)-prostaglandin J(2) ameliorates experimental autoimmune encephalomyelitis. J. Immunol. 168, 2508–2515 (2002).
Uchida, K. Redox-derived damage-associated molecular patterns: ligand function of lipid peroxidation adducts. Redox Biol. 1, 94–96 (2013).
Cubillos-Ruiz, J.R. et al. ER stress sensor XBP1 controls anti-tumor immunity by disrupting dendritic cell homeostasis. Cell 161, 1527–1538 (2015).
Doyle, K. & Fitzpatrick, F.A. Redox signaling, alkylation (carbonylation) of conserved cysteines inactivates class I histone deacetylases 1, 2, and 3 and antagonizes their transcriptional repressor function. J. Biol. Chem. 285, 17417–17424 (2010).
Fritz, K.S. et al. 4-Hydroxynonenal inhibits SIRT3 via thiol-specific modification. Chem. Res. Toxicol. 24, 651–662 (2011).
Galligan, J.J. et al. Stable histone adduction by 4-oxo-2-nonenal: a potential link between oxidative stress and epigenetics. J. Am. Chem. Soc. 136, 11864–11866 (2014).
Kondo, M. et al. 15-Deoxy-Delta(12,14)-prostaglandin J(2): the endogenous electrophile that induces neuronal apoptosis. Proc. Natl. Acad. Sci. USA 99, 7367–7372 (2002).
Jacobs, A.T. & Marnett, L.J. HSF1-mediated BAG3 expression attenuates apoptosis in 4-hydroxynonenal-treated colon cancer cells via stabilization of anti-apoptotic Bcl-2 proteins. J. Biol. Chem. 284, 9176–9183 (2009).
Chipuk, J.E. et al. Sphingolipid metabolism cooperates with BAK and BAX to promote the mitochondrial pathway of apoptosis. Cell 148, 988–1000 (2012).
Droge, W. Free radicals in the physiological control of cell function. Physiol. Rev. 82, 47–95 (2002).
Foyer, C., Faragher, R. & Thornalley, P. (eds.) Redox Metabolism and Longevity Relationships in Animals and Plants. (Taylor & Francis, 2009).
Stadtman, E.R. & Berlett, B.S. Reactive oxygen-mediated protein oxidation in aging and disease. Chem. Res. Toxicol. 10, 485–494 (1997).
Dalleau, S., Baradat, M., Gueraud, F. & Huc, L. Cell death and diseases related to oxidative stress: 4-hydroxynonenal (HNE) in the balance. Cell Death Differ. 20, 1615–1630 (2013).
Levine, R.L. Carbonyl modified proteins in cellular regulation, aging, and disease. Free Radic. Biol. Med. 32, 790–796 (2002).
Dalle-Donne, I., Rossi, R., Colombo, R., Giustarini, D. & Milzani, A. Biomarkers of oxidative damage in human disease. Clin. Chem. 52, 601–623 (2006).
Paulsen, C.E. & Carroll, K.S. Cysteine-mediated redox signaling: chemistry, biology, and tools for discovery. Chem. Rev. 113, 4633–4679 (2013).
Fang, X. et al. Temporally controlled targeting of 4-hydroxynonenal to specific proteins in living cells. J. Am. Chem. Soc. 135, 14496–14499 (2013).
Lin, H.Y., Haegele, J.A., Disare, M.T., Lin, Q. & Aye, Y. A generalizable platform for interrogating target- and signal-specific consequences of electrophilic modifications in redox-dependent cell signaling. J. Am. Chem. Soc. 137, 6232–6244 (2015).
Parvez, S. et al. Substoichiometric hydroxynonenylation of a single protein recapitulates whole-cell-stimulated antioxidant response. J. Am. Chem. Soc. 137, 10–13 (2015).
Janssen, D.B. Evolving haloalkane dehalogenases. Curr. Opin. Chem. Biol. 8, 150–159 (2004).
Los, G.V. & Wood, K. A novel technology for cell imaging and protein analysis. Methods Mol. Biol. 356, 195–208 (2007).
Los, G.V. et al. HaloTag: a novel protein labeling technology for cell imaging and protein analysis. ACS Chem. Biol. 3, 373–382 (2008).
Ohana, R.F. et al. HaloTag7: a genetically engineered tag that enhances bacterial expression of soluble proteins and improves protein purification. Protein Expr. Purif. 68, 110–120 (2009).
Long, M.J.C., Poganik, J.R. & Aye, Y. On-demand targeting: investigating biology with proximity-directed chemistry. J. Am. Chem. Soc. 138, 3610–3622 (2016).
Rogakou, E.P., Pilch, D.R., Orr, A.H., Ivanova, V.S. & Bonner, W.M. DNA double-stranded breaks induce histone H2AX phosphorylation on serine 139. J. Biol. Chem. 273, 5858–5868 (1998).
Morgan, M.J. & Liu, Z.G. Crosstalk of reactive oxygen species and NF-kappaB signaling. Cell Res. 21, 103–115 (2011).
Tjalkens, R.B., Cook, L.W. & Petersen, D.R. Formation and export of the glutathione conjugate of 4-hydroxy-2, 3-E-nonenal (4-HNE) in hepatoma cells. Arch. Biochem. Biophys. 361, 113–119 (1999).
Volkel, W. et al. Glutathione conjugates of 4-hydroxy-2(E)-nonenal as biomarkers of hepatic oxidative stress-induced lipid peroxidation in rats. Free Radic. Biol. Med. 38, 1526–1536 (2005).
Banerjee, R. Redox Biochemistry (Wiley, 2007).
Cao, Z., Hardej, D., Trombetta, L.D. & Li, Y. The role of chemically induced glutathione and glutathione S-transferase in protecting against 4-hydroxy-2-nonenal-mediated cytotoxicity in vascular smooth muscle cells. Cardiovasc. Toxicol. 3, 165–177 (2003).
Kolb, H.C., Finn, M.G. & Sharpless, K.B. Click chemistry: diverse chemical function from a few good reactions. Angew. Chem. Int. Ed. Engl. 40, 2004–2021 (2001).
Aye, Y., Li, M., Long, M.J.C. & Weiss, R.S. Ribonucleotide reductase and cancer: biological mechanisms and targeted therapies. Oncogene 34, 2011–2021 (2015).
Hayes, J.D. & Dinkova-Kostova, A.T. The Nrf2 regulatory network provides an interface between redox and intermediary metabolism. Trends Biochem. Sci. 39, 199–218 (2014).
Kobayashi, A. et al. Oxidative stress sensor Keap1 functions as an adaptor for Cul3-based E3 ligase to regulate proteasomal degradation of Nrf2. Mol. Cell Biol. 24, 7130–7139 (2004).
Krief, S. et al. Identification and characterization of cvHsp: a novel human small stress protein selectively expressed in cardiovascular and insulin-sensitive tissues. J. Biol. Chem. 274, 36592–36600 (1999).
Rosenfeld, G.E., Mercer, E.J., Mason, C.E. & Evans, T. Small heat shock proteins Hspb7 and Hspb12 regulate early steps of cardiac morphogenesis. Dev. Biol. 381, 389–400 (2013).
Marvin, M. et al. Developmental expression patterns of the zebrafish small heat shock proteins. Dev. Dyn. 237, 454–463 (2008).
Ma, Q. Role of nrf2 in oxidative stress and toxicity. Annu. Rev. Pharmacol. Toxicol. 53, 401–426 (2013).
Sporn, M.B. & Liby, K.T. NRF2 and cancer: the good, the bad and the importance of context. Nat. Rev. Cancer 12, 564–571 (2012).
Garber, K. Biochemistry: a radical treatment. Nature 489, S4–S6 (2012).
Uchida, K. & Stadtman, E.R. Modification of histidine residues in proteins by reaction with 4-hydroxynonenal. Proc. Natl. Acad. Sci. USA 89, 4544–4548 (1992).
Uchida, K. & Stadtman, E.R. Covalent attachment of 4-hydroxynonenal to glyceraldehyde-3-phosphate dehydrogenase. A possible involvement of intra- and intermolecular cross-linking reaction. J. Biol. Chem. 268, 6388–6393 (1993).
Nadkarni, D.V. & Sayre, L.M. Structural definition of early lysine and histidine adduction chemistry of 4-hydroxynonenal. Chem. Res. Toxicol. 8, 284–291 (1995).
Papa, A. et al. Cancer-associated PTEN mutants act in a dominant-negative manner to suppress PTEN protein function. Cell 157, 595–610 (2014).
Covey, T.M., Edes, K., Coombs, G.S., Virshup, D.M. & Fitzpatrick, F.A. Alkylation of the tumor suppressor PTEN activates Akt and β-catenin signaling: a mechanism linking inflammation and oxidative stress with cancer. PLoS One 5, e13545 (2010).
Shearn, C.T. et al. Increased carbonylation of the lipid phosphatase PTEN contributes to Akt2 activation in a murine model of early alcohol-induced steatosis. Free Radic. Biol. Med. 65, 680–692 (2013).
Shearn, C.T. et al. Phosphatase and tensin homolog deleted on chromosome 10 (PTEN) inhibition by 4-hydroxynonenal leads to increased Akt activation in hepatocytes. Mol. Pharmacol. 79, 941–952 (2011).
Leslie, N.R. & Foti, M. Non-genomic loss of PTEN function in cancer: not in my genes. Trends Pharmacol. Sci. 32, 131–140 (2011).
Trotman, L.C. et al. Pten dose dictates cancer progression in the prostate. PLoS Biol. 1, E59 (2003).
Covey, T.M., Edes, K. & Fitzpatrick, F.A. Akt activation by arachidonic acid metabolism occurs via oxidation and inactivation of PTEN tumor suppressor. Oncogene 26, 5784–5792 (2007).
Ananthanarayanan, B., Ni, Q. & Zhang, J. Signal propagation from membrane messengers to nuclear effectors revealed by reporters of phosphoinositide dynamics and Akt activity. Proc. Natl. Acad. Sci. USA 102, 15081–15086 (2005).
Antal, C.E. & Newton, A.C. Spatiotemporal dynamics of phosphorylation in lipid second messenger signaling. Mol. Cell Proteomics 12, 3498–3508 (2013).
Doudna, J.A. & Charpentier, E. Genome editing. The new frontier of genome engineering with CRISPR-Cas9. Science 346, 1258096 (2014).
Fellmann, C.L. & Scott, W. Stable RNA interference rules for silencing. Nat. Cell Biol. 16, 10–18 (2014).
Assou, S. et al. Dynamic changes in gene expression during human early embryo development: from fundamental aspects to clinical applications. Hum. Reprod. Update 17, 272–290 (2011).
García-Santamarina, S. et al. Monitoring in vivo reversible cysteine oxidation in proteins using ICAT and mass spectrometry. Nat. Protoc. 9, 1131–1145 (2014).
Lo Conte, M., Lin, J., Wilson, M.A. & Carroll, K.S. A chemical approach for the detection of protein sulfinylation. ACS Chem. Biol. 10, 1825–1830 (2015).
Yang, J. et al. Global, in situ, site-specific analysis of protein S-sulfenylation. Nat. Protoc. 10, 1022–1037 (2015).
Gautier, A. et al. An engineered protein tag for multiprotein labeling in living cells. Chem. Biol. 15, 128–136 (2008).
Grune, T., Siems, W.G., Zollner, H. & Esterbauer, H. Metabolism of 4-hydroxynonenal, a cytotoxic lipid peroxidation product, in Ehrlich mouse ascites cells at different proliferation stages. Cancer Res. 54, 5231–5235 (1994).
Srivastava, S. et al. Metabolism of the lipid peroxidation product, 4-hydroxy-trans-2-nonenal, in isolated perfused rat heart. J. Biol. Chem. 273, 10893–10900 (1998).
Blankespoor, R.L. et al. Photochemistry of 1-alkoxy- and 1-(benzyloxy)-9,10-anthraquinones in methanol: a facile process for the preparation of aldehydes and ketones. J. Org. Chem. 60, 6852–6859 (1995).
Wood, K.V. Luciferase Assay Method. US patent 5,283,179 (1994).
Sherf, B.A., Wood, K.V. & Schenborn, E.T. Quenching Reagents and Assays for Enzyme-mediated Luminescence. US patent 5,744,320 (1998).
Grune, T. & Davies, K.J.A. The proteasomal system and HNE-modified proteins. Mol. Aspects Med. 24, 195–204 (2003).
Acknowledgements
We thank the laboratories of T. Evans (Weill Cornell Medicine, New York) and J. Zhang (University of California, San Diego) for plasmids encoding zebrafish hspb7 and the lnPAkt (PIP3-reporter) construct, respectively. We acknowledge all of the Aye Laboratory members who have contributed to T-REX redox targeting protocols, particularly J. Li, X. Fang and Y. Fu, as well as Q. Lin of the State University of New York at Albany for assistance with the LC–MS/MS analysis of modifications on the protein pulled down from cells. Funding was provided by the NIH Director's New Innovator award (1DP2GM114850), the National Science Foundation (NSF) CAREER award (CHE-1351400), the Beckman Young Investigator award and the Sloan Research Fellowship (to Y.A.) and the Burroughs Wellcome Funds CTRG (to principal investigator (PI) Y.A. and host T. Evans). S.P. is a Howard Hughes Medical Institute international predoctoral fellow (59108350). J.A.H. acknowledges the CBI training grant (T32GM008500, PI – H. Lin). V.N.P. thanks the Douglas family for an undergraduate research fellowship. D.K.L. thanks the Cornell University P3 scholars program. Imaging and flow cytometry data were acquired at the Cornell University Biotechnology Resource Center (NIH 1S10RR025502) and the Cornell University cytometry core (supported in part by the Empire State Stem Cell Fund), respectively. We acknowledge the NSF (NSF MRI: CHE-1531632 to Y.A. (PI)) for NMR instrumentation support at Cornell University.
Author information
Authors and Affiliations
Contributions
H.-Y.L. and Y.Z. were joint second authors of this work. S.P., M.J.C.L., H.-Y.L., Y.Z., J.A.H., V.N.P., D.K.L. and Y.A. developed protocols. S.P. and V.N.P. contributed to the data associated with T-REX in E. coli cells. M.J.C.L., Y.Z., J.A.H. and D.K.L. obtained the data associated with T-REX in cultured human cells. H.-Y.L. collected LC-MS/MS data. H.-Y.L. and Y.Z. contributed to chemical synthesis. S.P., M.J.C.L. and H.-Y.L. wrote the protocols. Y.A. wrote the manuscript with proofreading/editing contributions from S.P., M.J.C.L., Y.Z. and J.A.H.
Corresponding author
Ethics declarations
Competing interests
Licensing application on this work is being pursued.
Integrated supplementary information
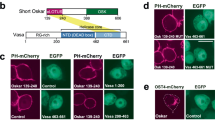
Supplementary Figure 1 Executing T-REX in mammalian cells
HEK-293 cells cultured (a) in 2x 55 cm2 adherent cell culture plates, and (b and c) in a 48-well multi-well adherent cell culture plate. No cover was placed on the plates during photo-uncaging. See Main Text for detailed experimental conditions and equipment specifications. Also see Supplementary Videos 1, 2
Supplementary Figure 2 Evaluation of time-dependent redox signal release in cells in T-REX method and validation that HaloTag does not react with HNE.
(a) Measurements of HNE release efficiency in cells. HEK293T cells expressing HaloTag alone treated under standard T-REX conditions with Ht-PreHNE were exposed to UV light (0.3 mW/cm2, 365 nm) for the indicated time periods at which point the cells were harvested, lysed, and subjected to Click coupling and in-gel fluorescence analysis followed by western blot. Error bars designate SD (N=3). (b) Controls to show that HaloTag does not react with HNE. Purified recombinant HaloTag was treated with either the photocaged precursor Ht-PreHNE (Figure 2, inset, and Figure 10) (2 equiv., lane a, positive control), or directly with reactive electrophile HNE (Figure 10) (0, 2, 4, 8, 16 equiv., lane b, c, d, e, f, respectively). After 20-min incubation, the samples were analyzed by in-gel fluorescence. M, molecular weight ladder.
Supplementary Figure 3 UV light exposure employed in T-REX is non-invasive: representative data for γ-H2AX1 and NF-κB2, markers for DNA damage and inflammatory signaling, respectively.
(a) HEK293T cells were exposed to UV light (0.3 mW/cm2, 340 nm) for the indicated time periods. Mitomycin C (10 μg/ml for 24 h)3 and aphidicolin (10 μg/ml for 36 h)4 serve as positive controls. After 12 hours post the end of UV illumination, cells were fixed and analyzed by standard immunofluorescence imaging method using γ-H2AX antibody (Millipore 05-636 at 1:1000 dilution). Data show mean +/- S.D. N > 50 cells. (b) HEK293T cells stably expressing NRE-inducible firefly luciferase5 were transfected with the respective plasmids encoding indicated transgene (empty vector, HaloTag alone, or Halo-Keap1 and Renilla luciferase) under constitutive CMV promoters. 24 hours post transfection, half of the plates were exposed to UV light (0.3 mW/cm2, 365 nm) over 20 min. Phorbol 12-myristate 13-acetate (PMA) (10 ng/mL, 18 h) was used as a positive control for NRE activation5. NRE activation was measured after 18 hrs. Error bars designate S.D. (N = 8 biological replicates).
Supplementary Figure 4 T-REX screen of Halo ORF clones for the discovery of novel electrophile-sensitive targets and pulldown validation of expressed proteins exemplified by zebrafish HSPB7.
(a) T-REX-enabled gel-based screen for bona fide HNE-sensitive targets using Halo-ORFeome library (Promega). Individual wells in a 48-well plate contained live HEK-293 cells ectopically expressing a unique HaloTagged gene of interest. The cells were subjected to T-REX-HNE(alkyne) targeting on demand. Post cell lysis, all samples were treated with TEV protease and subsequently subjected to Click coupling reaction with Cy5 azide. Probing with Halo antibody allowed evaluation of expression level (and/or solubility under the lysis conditions used). The “hit” bands on Cy5-fluorescent gel were judged against Halo protein level revealed by western blot. For example, RRM1, PRKCD, p53R2, and Keap1 (positive control) had roughly similar expression levels. Only RRM1 and Keap1 were HNE-sensitive although all four targets have been previously identified to be potentially redox/HNE-sensitive6–10. See Main Text for discussion. ⌘, a non-specific band. Also see Figure 4 and procedural details in Main Text. (b) Zebrafish HSPB7 expression and protein ID of the band shown in Figure 4a was validated by enrichment from HEK-293 cells ectopically expressing Halo-HSPB7 with the use of HaloTag PEG-Biotin ligand (Promega G8592) and streptavidin sepharose beads (GE Healthcare, cat. no. 17-5113-01), and subsequent on-bead TEV-protease cleavage followed by gel electrophoresis analysis. Theoretical MW of HSPB7 ~ 18 kDa. L, MW ladder.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–4 and Supplementary Tables 1 and 2 (PDF 2343 kb)
Setting up T-REX in cultured mammalian cells:
Caption text: video shows a proper setup for the light illumination of cultured mammalian cells in a 48-well plate. (MP4 35071 kb)
Setting up T-REX in E. coli
Caption text: video shows a proper setup for the light illumination step. (MP4 3685 kb)
Rights and permissions
About this article
Cite this article
Parvez, S., Long, M., Lin, HY. et al. T-REX on-demand redox targeting in live cells. Nat Protoc 11, 2328–2356 (2016). https://doi.org/10.1038/nprot.2016.114
Published:
Issue Date:
DOI: https://doi.org/10.1038/nprot.2016.114
This article is cited by
-
Z-REX: shepherding reactive electrophiles to specific proteins expressed tissue specifically or ubiquitously, and recording the resultant functional electrophile-induced redox responses in larval fish
Nature Protocols (2023)
-
Wdr1 and cofilin are necessary mediators of immune-cell-specific apoptosis triggered by Tecfidera
Nature Communications (2021)
-
Akt3 is a privileged first responder in isozyme-specific electrophile response
Nature Chemical Biology (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.