Abstract
Selegiline (L-deprenyl) is a selective, irreversible inhibitor of monoamine oxidase B (MAO-B) at the conventional dose (10 mg/day oral) that is used in the treatment of Parkinson’s disease. However, controlled studies have demonstrated antidepressant activity for high doses of oral selegiline and for transdermal selegiline suggesting that when plasma levels of selegiline are elevated, brain MAO-A might also be inhibited. Zydis selegiline (Zelapar) is an orally disintegrating formulation of selegiline, which is absorbed through the buccal mucosa producing higher plasma levels of selegiline and reduced amphetamine metabolites compared with equal doses of conventional selegiline. Although there is indirect evidence that Zydis selegiline at high doses loses its selectivity for MAO-B, there is no direct evidence that it also inhibits brain MAO-A in humans. We measured brain MAO-A in 18 healthy men after a 28-day treatment with Zydis selegiline (2.5, 5.0, or 10 mg/day) and in 3 subjects receiving the selegiline transdermal system (Emsam patch, 6 mg/day) using positron emission tomography and the MAO-A radiotracer [11C]clorgyline. We also measured dopamine transporter (DAT) availability in three subjects from the 10 mg group. The 10 mg Zydis selegiline dose significantly inhibited MAO-A (36.9±19.7%, range 11–70%, p<0.007)) but not DAT; and while Emsam also inhibited MAO-A (33.2±28.9 (range 9–68%) the difference did not reach significance (p=0.10)) presumably because of the small sample size. Our results provide the first direct evidence of brain MAO-A inhibition in humans by formulations of selegiline, which are currently postulated but not verified to target brain MAO-A in addition to MAO-B.
Similar content being viewed by others
INTRODUCTION
Developed in the 1950s, monoamine oxidase (MAO) inhibitors were the first effective medications for the treatment of depression, and probably remain some of the most effective agents today despite the introduction of newer drugs (Shulman et al, 2013). Unfortunately, the early MAO inhibitors were non-selective and irreversibly inhibited both MAO isoforms (MAO-A and MAO-B) in the gut as well as in the brain, causing serious hypertensive reactions following the ingestion of foodstuffs containing tyramine. This is referred to as the ‘cheese effect’ (Finberg and Gillman, 2011). The antidepressant effect of MAO inhibitors is generally attributed to their inhibition of brain MAO-A, which breaks down the neurotransmitters serotonin and norepinephrine, are involved with mood, and are targets for most antidepressants (Lipper et al, 1979; Finberg, 2014, review).
Selegiline (L-deprenyl) is an irreversible inhibitor of MAO-B with selectivity for MAO-B vs MAO-A (Robinson, 1985; Santana et al, 2008). At low doses (10 mg/day, oral), selegiline specifically inhibits brain MAO-B while leaving brain MAO-A substantially intact (Riederer and Youdim, 1986; Fowler et al, 2001), and is used to treat Parkinson’s disease. However, controlled studies have demonstrated antidepressant activity for high doses of oral selegiline, suggesting that when plasma levels of selegiline are elevated, its selectivity for MAO-B is lost resulting in MAO-A inhibition, producing antidepressant activity and requiring the limitation of dietary tyramine (Prasad et al, 1988; Schulz et al, 1989; Sunderland et al, 1985, 1994; Mann et al, 1989).
To reduce the inhibition of gut MAO-A, two different formulations of selegiline have been developed. Selegiline transdermal system (Emsam) enables absorption from the skin directly into the bloodstream. Preclinical measurements in guinea pigs showed preferential inhibition of CNS MAO-A and MAO-B compared with intestinal and hepatic tissues unlike oral administration, which resulted in similar levels of brain and gut MAO-A inhibition (Mawhinney et al, 2003). Pharmacokinetic studies in healthy humans comparing the selegiline transdermal system with oral selegiline capsules showed a significant reduction in both tyramine pressor sensitivity and amphetamine metabolites (Azzaro et al, 2006, 2007). The use of selegiline transdermal system enabled controlled clinical trials to treat depression without dietary restrictions (Bodkin and Amsterdam, 2002; Amsterdam, 2003; Feiger et al, 2006).
Zydis selegiline (Zelapar) is a freeze-dried formulation, which when allowed dissolving on the tongue without swallowing, is absorbed primarily through the buccal mucosa into the bloodstream thereby reducing the opportunity for first pass metabolism and inhibition of gut MAO. Pharmacokinetic studies have shown that Zydis selegiline inhibits MAO-B at one-eighth of the conventional oral dose (10 mg/day) and decreases amphetamine metabolites by 80–90% (Clarke et al, 2003a, 2003b; Löhle and Storch, 2008). In addition, repeated doses of Zydis selegiline 10 mg (but not the 1.25 mg dose) resulted in a significant reduction in the urinary excretion of 5-hydroxy-indoleacetic acid, a peripheral marker for MAO-A activity consistent with inhibition of MAO-A in addition to MAO-B (Clarke et al, 2003a). However, even though the antidepressant activity of high dose and other formulations of selegiline have been attributed to the inhibition of brain MAO-A (Finberg, 2014 for review), this has never been confirmed in humans.
The purpose of this study was to investigate whether formulations of selegiline, which bypass first-pass metabolism, also inhibit brain MAO-A in humans utilizing positron emission tomography (PET) imaging and the MAO-A radiotracer [11C]clorgyline (Fowler et al, 1996). We examined different daily doses of Zydis selegiline (2.5, 5.0, or 10 mg) given for 28 days to 18 healthy human subjects and by the selegiline transdermal system (6 mg/day) in 3 subjects. As dopamine transporter (DAT) inhibition has also been suggested as a possible mechanism for the antidepressant activity of selegiline (Mann et al, 1989), we also measured DAT availability in three subjects receiving the 10 mg dose of Zydis selegiline using the DAT radiotracer, [11C]cocaine (Fowler et al, 1989).
MATERIALS AND METHODS
This study was carried out at Brookhaven National Laboratory and approved by the local Institutional Review Board (Committee on Research Involving Human Subjects, Stony Brook University). All subjects gave their written informed consent.
Subjects and Study Design
Twenty-eight subjects were screened and twenty normal healthy non-smoking males aged 18–38 years were enrolled. Inclusion criteria were: healthy, non-smoking males, body mass index (BMI, kg/m2) ⩾21 and ⩽30, able to understand and give informed consent. Key exclusion criteria included presence of a significant acute or chronic medical disorder that might complicate or interfere with MAO inhibitor therapy, current or past psychiatric or neurological disease, cardiovascular disease, endocrinological disease, history or presence of phenylketonuria, and history of substance abuse, including alcohol or nicotine abuse as defined by DSM-IV criteria, within the past 12 months. All subjects were instructed to abstain from taking prescription or nonprescription drugs within 7 days (2 months for neuroleptics and fluoxetine or any other drug with a prolonged half-life) and to adhere to a low-tyramine diet during the study and 2 weeks following study participation. Subject demographics are summarized in Table 1. All study participants also consented to participate in an imaging genetic study and provided blood sample for MAO-A genotyping as described previously (Sabol et al, 1998).
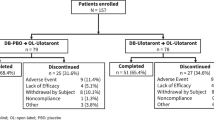
This was an open-label, non-randomized, single-center study designed to evaluate the effects of administration of three different daily doses of Zydis selegiline (2.5, 5.0, or 10.0 mg) on healthy subjects for 28 days on brain MAO-A. Six subjects were assigned to each dose. Three subjects were assigned to the Emsam group (6 mg/24 h). One subject participated in both the Zydis selegiline (2.5 mg) and the Emsam groups. Zelapar Orally Disintegrating Tablets, each containing 1.25 mg of selegiline Zydis formulation, were administered orally by dissolution on the tongue (not swallowed). Instructions for dosing and the first dose of Zydis selegiline was observed by study personnel after the baseline PET scan. Subjects were instructed not to take the last tablets on the day before the second PET scan but to wait as it would be administered 2 h before the last PET scan. Each 6 mg/24 h Emsam patch was supplied as a 20 mg/20 cm2 transdermal system and the first patch was applied following the baseline PET scan. The duration of treatment was 28 days and the last patch was applied 2 h before the second PET scan.
A treatment log was provided to each subject and weekly phone reminders were made to take the medication and to follow dietary restrictions. Missed doses were noted on the dispensing logs. Subjects who missed 20% of the doses were withdrawn from the study. Subjects were instructed to return unused study drugs and empty wrappers, which were inventoried to assess subject compliance throughout the treatment period.
Zydis selegiline tolerability was assessed as oropharyngeal irritation at baseline and day 28. Blood and urine samples for clinical laboratory tests were obtained at screening, day 28 and the post-treatment follow-up visit. Adverse event queries were conducted at each visit and during periodic telephone calls during dosing. Vital signs were measured at screening, baseline, immediately before and after each PET scan, and at the follow-up visit.
[11C]Clorgyline and [11C]Cocaine PET Scans
[11C]Clorgyline synthesis and PET scans were carried out as described previously (MacGregor et al, 1988; Alia-Klein et al, 2008). Each subject had two PET scans with [11C]clorgyline (average 6.6±0.9 mCi/scan; specific activity, 0.9±0.4 mCi/nmol at time of injection), one at baseline and the second at 28 days after dosing. An arterial plasma input function for [11C]clorgyline was measured (Alexoff et al, 1995). Three subjects who received the 10 mg Zydis selegiline dose also had a scan with [11C]cocaine (average 7.2±0.4 mCi/scan; specific activity, 0.95±0.31 mCi/nmol at time of injection) on the same day (2 h apart) using the synthesis and scanning protocol reported previously (Volkow et al, 1997).
Image Analysis
Emission data were attenuation corrected and reconstructed using filtered back projection. Region of interest (ROI) placement for the [11C]clorgyline and the [11C]cocaine scans was made as described previously (Fowler et al, 2010; Volkow et al, 2009). Composite images were created by first normalizing each subject’s scan to a standard template. Images from each of the six MAO-A subjects or three DAT subjects were then averaged at baseline and post dosing with 10 mg of Zydis selegiline.
Data Analysis
For quantification of MAO-A activity, PET time-activity data for [11C]clorgyline from different brain regions and time-activity data in arterial plasma were used to calculate the model terms K1 and λk3 at baseline and after Zydis selegiline and Emsam. The model term K1 is related to blood flow (F) and permeability surface area product (PS) via the K1=F(1-e-(PS/F). The model term λk3 is a function of the concentration of catalytically active MAO-A molecules, where k3 is related to the irreversible binding of [11C]clorgyline by MAO-A, k2 is related to the efflux of radiotracer from brain to blood and λ is defined as K1/k2 and is independent of blood flow (Fowler et al, 1996; Logan et al, 1991). [11C]Clorgyline binding (λk3) in human brain has recently been shown to be proportional to MAO-A protein content (Tong et al, 2013). For the [11C]cocaine scans, PET time-activity curves in the caudate, putamen, and cerebellum and the arterial input function were used to calculate K1 and the non-displaceable binding potential (BPND) as an index of DAT availability using the Logan plot (Logan et al, 1990).
Estimation of the Degree of Inhibition of [11C]Clorgyline Binding to MAO-A by Zydis Selegiline and Emsam
For each subject, a λk3 value for each of the 12 ROIs was determined at baseline and after Zydis selegiline or Emsam administration. A composite global λk3 value for each subject at baseline and after drug was also determined by averaging the regional λk3 values. For each subject, the percent inhibition of MAO-A was determined from the percent change in λk3 relative to baseline for each of the ROIs and these values were averaged to give an average percent change (mean±SD) at each drug dose.
Statistical Analysis of [11C]Clorgyline Data and [11C]Cocaine Data
A one-way ANOVA analysis was used to examine whether there was a significant dose-related change in the % inhibition of [11C]clorgyline binding (λk3) after a 28-day dosing regimen for the 2.5 vs 5.0 vs 10.0 mg Zydis selegiline doses. Pair-wise differences were examined via the Tukey method at the family-wise error rate of 0.05 (one-tailed) with two-tailed test being used to examine differences in K1. Unpaired t-test was used to examine whether there was a statistically significant difference in the percent change in [11C]clorgyline binding for the Zydis selegiline 10-mg group and the Emsam group. For the 10-mg group, we subjected the individual ROI data to a repeated measures ANOVA analysis to determine whether the percent change differed between the ROIs. To assess whether subject characteristics (age and BMI) and weight-adjusted dose influenced the percent change in MAO-A, we performed correlation analysis for each dose group. A comparison of BPND for [11C]cocaine at baseline and after the 10 mg dose of Zydis selegiline was made using a paired t-test, two-tailed. We also performed a correlation analysis between the % change in DAT and the % change in MAO-A for the three subjects in whom both measures were made.
RESULTS
There was no statistical difference in age or BMI for the three dose groups for Zydis selegiline (Table 1). All doses of Zydis selegiline and the Emsam patch were tolerated and there were no adverse events and no changes in vital signs after the 28-day period. Weekly phone call reminders and tablet and patch container inventories indicated compliance with the medication instructions.
Effect of Orally Disintegrating Selegiline (Zydis Selegiline) and Selegline Transdermal System (Emsam) on [11C]Clorgyline Binding in the Brain
There were no significant differences in K1 after either Zydis selegiline or Emsam administration (Table 2). The average values of λk3 for the 2.5, 5.0, and 10 mg doses of Zydis selegiline and Emsam groups are presented in Table 2. There was no difference between the baseline λk3 values for the three groups, or were there differences between the baseline and post treatment values of λk3 for the 2.5 and 5.0 mg groups. However, the 10-mg group showed a significant reduction of λk3, which corresponded to a 36.9±19.7% inhibition of MAO-A, although the percent reduction varied between subjects (range 11–70%). Table 2 also shows an increasing reduction in λk3 from baseline values as a function of Zydis dose, although only the 10-mg dose reaches statistical significance. MAO-A reduction can be seen in the averaged PET images at baseline and after treatment with 10 mg Zydis selegiline (Figure 1, top row). The λk3 reduction with Emsam ranged from 7.5 to 68% with no significant difference between the 10 mg Zydis selegiline and the Emsam group. We also compared percent change in λk3 for the 12 individual ROIs for the 10-mg group and found a significant region effect (repeated ANOVA in 12 ROI, F=1.2, p=0.04) driven by lower inhibition in the cerebellum relative to other regions of interest.
Composite PET images of MAO-A (λk3, top row) and of DAT (BPND, bottom row) at baseline and after 10 mg of Zydis selegiline administration.
Individual values for the composite λk3 values at baseline and after treatment for each of the subjects are shown in Figure 2. There were no significant associations between percent change in λk3 after Zydis selegiline and subject’s age, BMI, genotype or weight-adjusted dose of drug. However, for the 10 mg Zydis selegiline group, there was a significant correlation between baseline λk3 and percent change in λk3 with higher baseline λk3 values showing the largest decreases in MAO-A after drug (R=0.83; p=0.04)
Composite global values of λk3 for each individual subject at baseline and after a 28-day Zydis selegiline treatment for the 2.5 (upper left), 5.0 (upper right), and 10 mg (lower left) groups. Composite global values for the three Emsam-treated subjects are also shown.
Baseline λk3’s differed by 4% for the one subject (#094530) who participated in both the Zydis selegiline group and the Emsam group 14 months apart. Test/retest reproducibility for λk3 was 10.9±5.0% from prior human studies (Fowler et al, 1996). Thus, our results indicate that percent MAO-A inhibition with the 10-mg Zydis selegiline dose is at least threefold higher than the test/retest variability.
[11C]Cocaine Binding in Brain
For three of the subjects in the 10-mg Zydis selegiline group, we measured DAT availability with [11C]cocaine at baseline and after treatment. The average non-displaceable binding potential (BPND) although lower with Zydis selegiline did not differ significantly from the baseline (Figure 1, bottom row; Table 3). There was a significant decrease in the value of K1 after Zydis selegiline in caudate and putamen but the decrease in cerebellum was not significant (Table 3). A correlation analysis between the % change in DAT and the % change in MAO-A for the three subjects in whom both measures were made was not significant though we note that the sample size was small.
DISCUSSION
There is growing evidence that different formulations and different routes of administration of the same drug molecule can have a profound effect on drug bioavailability, pharmacokinetics, and pharmacodynamics (Smith and Uhl, 2009). We report here the first measurements confirming brain MAO-A inhibition in humans receiving formulations of selegiline, which reduce or bypass first-pass metabolism. We found that 10 mg of Zydis selegiline for 28 days loses its selectivity for MAO-B and significantly inhibits brain MAO-A and that the Emsam patch for 28 days showed >30% inhibition of MAO-A in two of the three subjects tested.
Our results confirming inhibition of brain MAO-A with high dose Zydis selegiline and with the Emsam patch provide the first direct evidence in the humans that brain MAO-A inhibition may contribute to its pharmacological and therapeutic profile, particularly for depression. They are consistent with those of Clarke et al who reported that repeated doses of high-dose Zydis selegiline reduces the urinary excretion of 5-hydroxy-indoleacetic acid, a peripheral marker for MAO-A activity (Clarke et al, 2003a, 2003b), and also with preclinical studies with the selegiline transdermal system which showed targeted inhibition of the MAO enzymes in the CNS while limiting MAO-A inhibition in the gut (Mawhinney et al, 2003).
Meyer et al (2006) reported that patients with major depressive disorder have an average 34% elevation of brain MAO-A, which may contribute to the monoamine imbalance in depression. We can speculate that brain MAO-A inhibition by formulations of selegiline, which result in brain MAO-A inhibition, may contribute to a rebalancing of brain monoamines. Interestingly, there is a high comorbidity between smoking and depression (Glassman et al, 1990). Biologically based self-medication hypotheses have been proposed to account for this observation including nicotine-induced release of norepinephrine and dopamine, which are neurotransmitters mediating arousal and stimulation (Lerman et al, 1996; Pomerleau and Pomerleau, 1984). As tobacco smoke inhibits brain MAO-A by ∼30% (Fowler et al, 1996), brain MAO-A inhibition by cigarette smoke may also contribute to a rebalancing of brain monoamines thus alleviating depression symptoms.
Even though the primary pharmacological action of selegiline is MAO-B inhibition, its pharmacology is complex (Finberg, 2014 for review) and other mechanisms including the actions of amphetamine metabolites (Engberg et al, 1991), increased DAT expression (Lamensdorf et al, 1999), and DAT upregulation (Wiener et al, 1989) have also been proposed to account for the antidepressant efficacy of high doses of selegiline (Mann et al, 1989). Significant decreases in amphetamine metabolites with transdermal (Azzaro et al, 2007) and orally disintegrating formulations of selegiline (Clarke et al, 2003a) reduce the likelihood that selegiline metabolites play a role in the pharmacological effects of these formulations. Similar to our prior PET study with conventional selegiline (10 mg/day for 1 week; Fowler et al, 2001), we did not find significant brain DAT inhibition by 10 mg Zydis selegiline. We note that DAT inhibitor drugs like methylphenidate and modafinil at therapeutic doses inhibit >50% of DAT (Volkow et al, 2002; Volkow et al, 2009), whereas the DAT reduction we observed with Zydis selegiline for three subjects was <15%, which is not statistically significant and is unlikely to contribute to the pharmacological profile of this formulation.
There was a large individual variability in the percent change in [11C]clorgyline binding (λk3) within the 10 mg Zydis selegiline and the Emsam groups (Figure 2). We found no significant associations between the percent change in [11C]clorgyline binding and subject demographics or with the weight-adjusted dose of Zydis selegiline. However, there was a significant correlation between baseline λk3 and percent change in λk3 for the 10 mg Zydis selegiline group, with higher baseline λk3 values showing the largest decreases in MAO-A after drug. However, the sample size is small and the mechanism(s) underlying this relationship is unclear.
There is a common polymorphism in the promoter region of the MAOA gene that has two common alleles (4-repeat and 3-repeat) that occur in a 60:40 ratio in male humans, which are commonly referred to as high- and low-MAO-A genotypes as defined by their significantly different transcriptional activities (Sabol et al, 1998). The identification of this polymorphism led to the hypothesis that MAO-A genotype may serve as a marker of MAO-A gene function and to many studies of the association between high- and low-MAOA genotype and vulnerability to environmental stressors in humans (Dorfman et al, 2014). We include MAO-A genotype as one of the variables, which characterize our subjects. In a prior study, we found that high- and low-MAO-A genotype does not correlate with [11C]clorgyline binding in brain in healthy male volunteers (Fowler et al, 2007). In this study, we found no association with the percent change in MAO-A activity with the high-dose Zydis selegiline and Emsam groups and brain MAO-A levels as measured with [11C]clorgyline.
Our study had some limitations that warrant further investigation. This includes the small sample size particularly for the Emsam measures and the DAT measures. In addition, this was an outpatient study. Subjects were contacted weekly to remind them to take the medication as instructed and each subject returned at least 80% of their empty foil wrappers indicating to us that most of the medication was taken. Selegiline plasma measures would have allowed us to assess if plasma levels of selegiline correlated with the level of brain MAO-A blockade and future studies in a larger number of subjects would enable such a correlation to be explored.
In summary, this is the first direct confirmation of brain MAO-A inhibition in humans by high-dose Zydis selegiline and the Emsam selegiline both of which are currently postulated but not verified to inhibit brain MAO-A in addition to MAO-B. This suggests that brain MAO-A inhibition may account for some of the pharmacological and therapeutic effects of high-dose Zydis selegiline and other formulations of selegiline, which avoid first pass metabolism, including reports of antidepressant activity.
FUNDING AND DISCLOSURE
This study was funded by Valeant Pharmaceuticals International. The authors disclose no other conflict of interest that might potentially bias this work.
References
Alexoff DL, Shea C, Fowler JS, King P, Gatley SJ, Schlyer DJ et al (1995). Plasma input function determination for PET using a commercial laboratory robot. Nucl Med Biol 22: 893–904.
Amsterdam JD (2003). A double-blind, placebo-controlled trial of the safety and efficacy of selegiline transdermal system without dietary restrictions in patients with major depressive disorder. J Clin Psychiatry 64: 208–214.
Alia-Klein N, Goldstein RZ, Kriplani A, Logan J, Tomasi D, Williams B et al (2008). Brain monoamine oxidase A activity predicts trait aggression. J Neurosci 28: 5099–5104.
Azzaro AJ, Vandenberg CM, Blob LF, Kemper EM, Sharoky M, Oren DA et al (2006). Tyramine pressor sensitivity during treatment with the selegiline transdermal system 6 mg/24 h in healthy subjects. J Clin Pharmacol 46: 933–944.
Azzaro AJ, Ziemniak J, Kemper E, Campbell BJ, VanDenBerg C (2007). Pharmacokinetics and absolute bioavailability of selegiline following treatment of healthy subjects with the selegiline transdermal system (6 mg/24 h): a comparison with oral selegiline capsules. J Clin Pharmacol 47: 1256–1267.
Bodkin JA, Amsterdam JD (2002). Transdermal selegiline in major depression: a double-blind, placebo-controlled, parallel-group study in outpatients. Am J Psychiatry 159: 1869–1875.
Clarke A, Brewer F, Johnson ES, Mallard N, Hartig F, Taylor S et al (2003a). A new formulation of selegiline: improved bioavailability and selectivity for MAO-B inhibition. J Neural Transm 110: 1241–1255.
Clarke A, Johnson ES, Mallard N, Corn TH, Johnston A, Boyce M et al (2003b). A new low-dose formulation of selegiline: clinical efficacy, patient preference and selectivity for MAO-B inhibition. J Neural Transm 110: 1257–1271.
Dorfman HM, Meyer-Lindenberg A, Buckholtz JW (2014). Neurobiological mechanisms for impulsive-aggression: the role of MAOA. Curr Top Behav Neurosci 17: 297–313.
Engberg G, Elebring T, Nissbrandt H (1991). Deprenyl (selegiline), a selective MAO-B inhibitor with active metabolites; effects on locomotor activity, dopaminergic neurotransmission and firing rate of nigral dopamine neurons. J Pharmacol Exp Ther 259: 841–847.
Feiger AD, Rickels K, Rynn MA, Zimbroff DL, Robinson DS (2006). Selegiline transdermal system for the treatment of major depressive disorder: an 8-week, double-blind, placebo-controlled, flexible-dose titration trial. J Clin Psychiatry 67: 1354–1361.
Finberg JPM (2014). Update on the pharmacology of selective inhibitors of MAO-A and MAO-B: Focus on modulations of CNS monoamine neurotransmitter release. Pharmacol Ther 143: 133–152.
Finberg JP, Gillman K (2011). Selective inhibitors of monoamine oxidase type B and the ‘cheese effect’. Int Rev Neurobiol 100: 169–190.
Fowler JS, Azzaro AJ, Fielding RM, Zhu W, Pohusta AK et al (2010). Reversible inhibitors of monoamine oxidase-A (RIMAs): robust, reversible inhibition of human brain MAO-A by CX157. Neuropsychopharmacology 35: 623–631.
Fowler JS, Volkow ND, Logan J, Franceschi D, Wang GJ, MacGregor R et al (2001). Evidence that L-deprenyl treatment for one week does not inhibit MAO A or the dopamine transporter in the human brain. Life Sci 68: 2759–2768.
Fowler JS, Volkow ND, Wang G-J, Pappas N, Logan J, MacGregor RR et al (1996). Brain monoamine oxidase A inhibition in cigarette smokers. Proc Natl Acad Sci USA 93: 14065–14069.
Fowler JS, Volkow ND, Wolf AP, Dewey SL, Schlyer DJ, Macgregor RR et al (1989). Mapping cocaine binding sites in human and baboon brain in vivo. Synapse 4: 371–377.
Fowler JS, Alia-Klein N, Kriplani A, Logan J, Williams B, Zhu W et al (2007). Evidence that brain MAO A activity does not correspond to MAO A genotype in healthy male subjects. Biol Psychiatry 62: 355–358.
Glassman AH, Helzer JE, Covey LS, Cottler LB, Stetner F, Tipp JE et al (1990). Smoking, smoking cessation, and major depression. JAMA 264: 1546–1549.
Lamensdorf I, Porat S, Simantov R, Finberg JP (1999). Effect of low-dose treatment with selegiline on dopamine transporter (DAT) expression and amphetamine-induced dopamine release in vivo. Br J Pharmacol 126: 997–1002.
Lerman C, Audrain J, Orleans CT, Boyd R, Gold K, Main D et al (1996). Investigation of mechanisms linking depressed mood to nicotine dependence. Addict Behav 21: 9–19.
Lipper S, Murphy DL, Slater S, Buchsbaum MS (1979). Comparative behavioral effects of clorgyline and pargyline in man: a preliminary evaluation. Psychopharmacology (Berl) 62: 123–128.
Logan J, Dewey SL, Wolf AP, Fowler JS, Brodie JD, Angrist B et al (1991). Effects of endogenous dopamine on measures of [18F]N-methylspiroperidol binding in the basal ganglia: comparison of simulations and experimental results from PET studies in baboons. Synapse 9: 195–207.
Logan J, Fowler JS, Volkow ND, Wolf AP, Dewey SL, Schlyer DJ et al (1990). Graphical analysis of reversible radioligand binding from time-activity measurements applied to [N-11C-methyl]-(−)-cocaine PET studies in human subjects. J Cereb Blood Flow Metab 10: 740–747.
Löhle M, Storch A (2008). Orally disintegrating selegiline for the treatment of Parkinson's disease. Expert Opin Pharmacother 9: 2881–2891.
MacGregor RR, Fowler JS, Wolf AP, Halldin C, Langstrom B (1988). Synthesis of suicide inhibitors of monoamine oxidase: carbon-11 labeled clorgyline, L-deprenyl and D-deprenyl. J Labeled Compounds Radiopharm 25: 1–9.
Mann JJ, Aarons SF, Wilner PJ, Keilp JG, Sweeney JA, Pearlstein T et al (1989). A controlled study of the antidepressant efficacy and side effects of (−)-deprenyl. A selective monoamine oxidase inhibitor. Arch Gen Psychiatry 46: 45–50.
Mawhinney M, Cole D, Azzaro AJ (2003). Daily transdermal administration of selegiline to guinea-pigs preferentially inhibits monoamine oxidase activity in brain when compared with intestinal and hepatic tissues. J Pharm Pharmacol 55: 27–34.
Meyer JH, Ginovart N, Boovariwala A, Sagrati S, Hussey D, Garcia A et al (2006). Elevated monoamine oxidase A levels in the brain: an explanation for the monoamine imbalance of major depression. Arch Gen Psychiatry 63: 1209–1216.
Pomerleau OF, Pomerleau CS (1984). Neuroregulators and the reinforcement of smoking: towards a biobehavioral explanation. Neurosci Biobehav Rev 8: 503–513.
Prasad A, Glover V, Goodwin BL, Sandler M, Signy M, Smith SE (1988). Enhanced pressor sensitivity to oral tyramine challenge following high dose selegiline treatment. Psychopharmacology (Berl) 95: 540–543.
Riederer P, Youdim MB (1986). Monoamine oxidase activity and monoamine metabolism in brains of parkinsonian patients treated with l-deprenyl. J Neurochem 46: 1359–1365.
Robinson JB (1985). Stereoselectivity and isoenzyme selectivity of monoamine oxidase inhibitors. Enantiomers of amphetamine, N-methylamphetamine and deprenyl. Biochem Pharmacol 34: 4105–4108.
Sabol SZ, Hu S, Hamer D (1998). A functional polymorphism in the monoamine oxidase A gene promoter. Hum Genetics 103: 273.
Santana L, González-Díaz H, Quezada E, Uriarte E, Yáñez M, Viña D et al (2008). Quantitative structure-activity relationship and complex network approach to monoamine oxidase A and B inhibitors. J Med Chem 51: 6740–6751.
Schulz R, Antonin KH, Hoffmann E, Jedrychowski M, Nilsson E, Schick C et al (1989). Tyramine kinetics and pressor sensitivity during monoamine oxidase inhibition by selegiline. Clin Pharmacol Ther 46: 528–536.
Shulman KI, Herrmann N, Walker SE (2013). Current place of monoamine oxidase inhibitors in the treatment of depression. CNS Drugs 27: 789–797.
Smith B, Uhl K (2009). Drug delivery in the twenty-first century: a new paradigm. Clin Pharmacol Ther 85: 451–455.
Sunderland T, Mueller EA, Cohen RM, Jimerson DC, Pickar D, Murphy DL (1985). Tyramine pressor sensitivity changes during deprenyl treatment. Psychopharmacology (Berl) 86: 432–437.
Sunderland T, Cohen RM, Molchan S, Lawlor BA, Mellow AM, Newhouse PA et al (1994). High-dose selegiline in treatment-resistant older depressive patients. Arch Gen Psychiatry 51: 607–615.
Tong J, Meyer JH, Furukawa Y, Boileau I, Chang LJ, Wilson AA et al (2013). Distribution of monoamine oxidase proteins in human brain: implications for brain imaging studies. J Cereb Blood Flow Metab 33: 863–871.
Volkow ND, Fowler JS, Logan J, Alexoff D, Zhu W, Telang F et al (2009). Effects of modafinil on dopamine and dopamine transporters in the male human brain: clinical implications. JAMA 301: 1148–1154.
Volkow ND, Wang G-J, Fischman MW, Foltin RW, Fowler JS, Abumrad NN et al (1997). Relationship between subjective effects of cocaine and dopamine transporter occupancy. Nature 386: 827–830.
Volkow ND, Wang G-J, Fowler JS, Logan J, Franceschi D, Maynard L et al (2002). Relationship between blockade of dopamine transporters by oral methylphenidate and the increases in extracellular dopamine: therapeutic implications. Synapse 34: 181–187.
Wiener HL, Hashim A, Lajtha A, Sershen H (1989). Chronic L-deprenyl-induced up-regulation of the dopamine uptake carrier. Eur J Pharmacol 163: 191–194.
Acknowledgements
This study was carried out using the infrastructure of Brookhaven National Laboratory under contract DE-AC02-98CH10886 with the U.S. Department of Energy (Office of Biological and Environmental Research) and was funded by Valeant Pharmaceuticals International. We thank Michael Schueller for cyclotron operations and Donald Warner for PET operations. NDV, was supported by the National Institute on Drug Abuse and MJ, GJW, FT and KA-T were supported by the National Institute of Alcohol Abuse and Alcoholism; JSF was supported in part from a K award from NIH (K05DA020001); FM-P and MG were employed by Valeant Pharmaceuticals International at the time of this study and joined Targeted Medical Pharma Inc and Novartis Pharmaceuticals after this study was completed. This work was presented in part at the 63rd Annual Meeting of the American Academy of Neurology, Honolulu Hawaii, 13 April 2011 and the International Congress of Parkinson’s Disease and Movement Disorders meeting in Toronto 8 June 2011.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author Contributions
JSF, SF and NDV wrote the manuscript. JSF, SF, FM-P, G-JW and MG designed the study. FT, JSF, G-JW, MJ, DLA, KA-T, PC, BH, CS, YX, LM, ES performed the work. JL and JSF analyzed the data.
PowerPoint slides
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Fowler, J., Logan, J., Volkow, N. et al. Evidence that Formulations of the Selective MAO-B Inhibitor, Selegiline, which Bypass First-Pass Metabolism, also Inhibit MAO-A in the Human Brain. Neuropsychopharmacol 40, 650–657 (2015). https://doi.org/10.1038/npp.2014.214
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2014.214
This article is cited by
-
Safety comparisons among monoamine oxidase inhibitors against Parkinson’s disease using FDA adverse event reporting system
Scientific Reports (2023)
-
A systematic review of the potential effects of medications and drugs of abuse on dopamine transporter imaging using [123I]I-FP-CIT SPECT in routine practice
European Journal of Nuclear Medicine and Molecular Imaging (2023)
-
From warrior genes to translational solutions: novel insights into monoamine oxidases (MAOs) and aggression
Translational Psychiatry (2021)
-
The catecholaldehyde hypothesis: where MAO fits in
Journal of Neural Transmission (2020)
-
Selegiline: a molecule with innovative potential
Journal of Neural Transmission (2020)