Abstract
Frequent binge drinking has been linked to heart disease, high blood pressure, type 2 diabetes, and the development of ethanol dependence. Thus, identifying pharmaceutical targets to treat binge drinking is of paramount importance. Here we employed a mouse model of binge-like ethanol drinking to study the role of neuropeptide Y (NPY). To this end, the present set of studies utilized pharmacological manipulation of NPY signaling, immunoreactivity (IR) mapping of NPY and NPY receptors, and electrophysiological recordings from slice preparations of the amygdala. The results indicated that central infusion of NPY, a NPY Y1 receptor (Y1R) agonist, and a Y2R antagonist significantly blunted binge-like ethanol drinking in C57BL/6J mice (that achieved blood ethanol levels >80 mg/dl in control conditions). Binge-like ethanol drinking reduced NPY and Y1R IR in the central nucleus of the amygdala (CeA), and 24 h of ethanol abstinence after a history of binge-like drinking promoted increases of Y1R and Y2R IR. Electrophysiological recordings of slice preparations from the CeA showed that binge-like ethanol drinking augmented the ability of NPY to inhibit GABAergic transmission. Thus, binge-like ethanol drinking in C57BL/6J mice promoted alterations of NPY signaling in the CeA, and administration of exogenous NPY compounds protected against binge-like drinking. The current data suggest that Y1R agonists and Y2R antagonists may be useful for curbing and/or preventing binge drinking, protecting vulnerable individuals from progressing to the point of ethanol dependence.
Similar content being viewed by others
INTRODUCTION
Alcohol (ethanol) dependence and relapse in abstinent alcoholics are major health problems in the United States, and neurochemical pathways that modulate these disorders are currently under investigation. However, the central mechanisms involved in the regulation of binge alcohol drinking, before the development of dependence, have received far less attention. As with all patterns of alcohol abuse, frequent binge drinking is associated with numerous negative short- and long-term consequences including increased risk of accidental injury (Gmel et al, 2006), increased mood disorders (Okoro et al, 2004), and increased aggressive and violent behavior (Shepherd et al, 2006). Perhaps most alarming is the finding of increased risk for developing alcohol dependence in individuals that binge drink early in life (Hingson et al, 2005, 2006; Miller et al, 2007). Thus, it is of paramount importance to identify neurochemical pathways in the brain that modulate binge drinking as such knowledge will provide insight into novel pharmaceutical treatments that will protect against this dangerous behavior.
The ‘drinking in the dark’ (DID) procedure is a well-established animal model of human binge drinking and has been used to identify neurochemical modulators of binge-like ethanol consumption (Gupta et al, 2008; Hendrickson et al, 2009; Kamdar et al, 2007; Kaur and Ryabinin, 2010; Linsenbardt and Boehm, 2009; Melon and Boehm, 2011; Moore and Boehm, 2009; Sajja and Rahman, 2011). We have recently found that corticotropin-releasing factor (CRF) type-1 receptor (CRF1R) antagonists reduce binge-like ethanol intake in C57BL/6J mice but fail to alter non-binge-like (low level) ethanol intake (Lowery et al, 2010; Sparta et al, 2008). These observations are strikingly similar to evidence showing that CRF1R antagonists protect against excessive dependence-like ethanol drinking in ethanol vapor-exposed rats but fail to alter normal ethanol drinking in nondependent animals (Finn et al, 2007; Funk et al, 2006; Gehlert et al, 2007; Valdez et al, 2002). As with CRF1R antagonists, central administration of neuropeptide Y (NPY) has also been shown to protect against excessive dependence-like ethanol drinking in outbred rats exposed to ethanol vapor without influencing normal ethanol intake in nondependent animals (Gilpin et al, 2008). Furthermore, although the effects of NPY on binge-like ethanol drinking have not been reported, we have previously found that central administration of a range of NPY doses failed to alter low non-binge-like ethanol drinking in C57BL/6J mice (Thiele et al, 2003), analogous to the inability of NPY to blunt low-level ethanol intake in rats not exposed to ethanol vapor. Interestingly, central administration of NPY protected against excessive ethanol drinking in rats selectively bred for high ethanol intake but failed to alter ethanol drinking in rats selected for low ethanol intake (Badia-Elder et al, 2001, 2003), consistent with a selective role for NPY in modulating excessive ethanol consumption. Central NPY acts through three receptor subtypes, namely the Y1 receptor (Y1R), Y2R, and Y5R, all of which couple to G proteins that inhibit production of cyclic AMP (cAMP) (Palmiter et al, 1998). The Y1R is located postsynaptically and NPY signaling via the Y1R protects against ethanol intake (Naveilhan et al, 1998; Thiele et al, 2002). The Y2R is primarily located presynaptically where it acts as an autoreceptor to inhibit release of endogenous NPY and as a heteroreceptor that inhibits the release of glutamate and GABA (King et al, 2000; Qian et al, 1997; Smith-White et al, 2001; Wahlestedt et al, 1986). Consistent with a role as an autoreceptor, a Y2R antagonist was found to reduce ethanol intake, presumably by increasing endogenous NPY signaling (Thorsell et al, 2002).
In light of the parallel observations that NPY and CRF1R antagonist protect against excessive dependence-like ethanol drinking without altering normal ethanol intake in nondependent rodents, and the recent observations that CRF1R antagonists protect against binge-like ethanol drinking (Lowery et al, 2010; Sparta et al, 2008), the main goal of the present set of experiments was to determine if NPY, like CRF1R antagonists, would attenuate binge-like ethanol drinking. Here we show that centrally administered NPY, a Y1R agonist, and a Y2R antagonist protected against binge-like ethanol drinking in C57BL/6J mice. Furthermore, a history of binge-like ethanol drinking was associated with a significant reduction of NPY and Y1R immunoreactivity (IR) in the central nucleus of the amygdala (CeA), whereas 24 h without ethanol access following binge-like ethanol drinking was associated with a significant increase of Y1R and Y2R IR in the CeA. Using whole-cell recordings from tissue slice preparations, we found that NPY-induced inhibition of GABAergic transmission was augmented in the CeA of mice with a history of binge-like drinking. Together, the current findings show that NPY signaling modulates excessive binge-like ethanol intake.
MATERIALS AND METHODS
Animals
Male C57BL/6J mice (Jackson Laboratory, Bar Harbor, ME) were used in all experiments. Mice were ∼8 weeks of age, weighed between 25 and 30 g, and were housed as previously described (Lowery et al, 2010). Experiments were approved by the University of North Carolina Animal Care and Use Committee and complied with the NIH Guide for Care and Use of Laboratory Animals.
DID Procedures
A 4-day DID procedure was used in all experiments (Rhodes et al, 2005). On days 1–3, beginning 2.75 h into the dark cycle, water bottles were removed from all cages. For all experiments involving intracerebroventricular (i.c.v.) administration of compounds, animals were weighed and infused with sterile water or isotonic saline (1 μl) to habituate them to infusion procedures on days 1–3. Beginning 3 h into the dark cycle, bottles containing 20% ethanol (v/v) were weighed and placed on cages for 2 h. The same schedule was followed on day 4 except that i.c.v. infusion of drug was given just before ethanol access (which was extended to 4 h). Immediately after ethanol access, tail blood samples (15 μl) were collected for analysis of blood ethanol concentrations (BECs; Analox Blood Analyzer, Analox Instruments USA, Lunenburg, MA). Two separate studies (NPY and Y1R antagonist infusion studies) used Latin Square designs in which mice experienced each dose of drug in a counterbalanced order (1 DID cycle per dose). The remaining i.c.v. infusion studies used a single-dose exposure design (1 DID cycle per experiment). Additional control studies were performed in which mice were given access to 10% (pharmacology studies) or 3% (immunohistochemistry studies) sucrose (w/v) in the same pattern as 20% ethanol using DID procedures. A lower concentration of sucrose was used in immunohistochemistry studies in an attempt to avoid potential weight gain by mice stemming from 6 weeks of access to sucrose. For the IR study (below), separate groups of mice experienced 1, 3, or 6 four-day DID cycles.
Surgery and Infusion Procedures
Approximately 1 week after arrival, mice underwent surgery to implant cannulae aimed at the lateral ventricle as described previously (Lowery et al, 2010). Mice were allowed to recover ∼1 week before experimental procedures were started. Cannula placement was verified histologically at the end of the experiment.
Drugs
The i.c.v. infusions were given manually in a 1.0 μl volume over a 1-min period with a 1.0 μl Hamilton microsyringe. The following compounds were used: NPY (0, 1, 3, or 10 μg/μl; Phoenix Pharmaceuticals, Burlingame, CA), the selective Y1R agonist [D-His26]-NPY (0, 1, or 3 μg/μl; American Peptide, Sunnyvale, CA), the selective Y1R antagonist BIBP-3226 (0, 0.01, or 0.1 μg/μl; Tocris Bioscience, Ellisville, MO), the selective Y2R agonist NPY13−36 (0, 1, 3, or 10 μg/μl, Phoenix Pharmaceuticals), and the selective Y2R antagonist BIIE-0246 (0, 1, or 3 μg/μl, Tocris Bioscience). The [D-His26]-NPY has been shown to be 90-fold selective for the Y1R vs the Y2R, and 376-fold selective for the Y1R vs the Y5R (Mullins et al, 2001). BIBP-3226 was shown to have almost no affinity at NPY receptors other than the Y1R receptor (Doods et al, 1996). NPY13−36 is 136-fold more selective for the Y2R vs the Y1R, and is 10-fold more selective for the Y2R vs the Y5R (Gerald et al, 1996). BIIE-0246 has almost no affinity for the Y1R and Y5R (Doods et al, 1999). Doses appropriate for i.c.v. administration were based on previous research (Bacchi et al, 2006; Nakhate et al, 2009; Sorensen et al, 2004).
Effects of Binge-Like Ethanol Drinking on NPY, Y1R, and Y2R IR
To control for age between groups that experienced 1–6 cycles of binge-like drinking (described above), the initiation of binge-like drinking was staggered such that all mice experienced their last binge-like drinking cycle at the same age. A control group drank water only throughout the duration of the experiment. Immediately after their last binge-like drinking session, blood samples were collected and mice were anesthetized with a ketamine (117 mg/kg) and xylazine (7.92 mg/kg) cocktail. Within 5 min of anesthesia injection, mice were then transcardially perfused with 0.1 mM of phosphate-buffered saline (PBS, pH 7.4) followed by 4% paraformaldehyde in buffered saline. Brains were collected and postfixed for 48 h in paraformaldehyde at 4 °C and then transferred to PBS until slicing. For comparison with data collected from electrophysiological analyses (see below), an additional set of mice that experienced three binge-like drinking cycles with 20% ethanol were anesthetized and perfused ∼24 h after their last binge-like drinking session (blood samples were collected immediately after the last drinking session). The whole brain was sliced into 40 μm sections using a Leica VT 1000S vibratome (Leica Microsystems, Nussloch, Germany) and stored in a cryopreserve solution until IR analysis. The sections were cut into three sets and processed with antibodies raised against NPY (Phoenix Pharmaceuticals; 1 : 1000; Thiele et al, 2000), Y1R (Antibody 96106 raised against NPY Y1R was provided by CURE/Digestive Disease Research Center, Antibody/RIA Core, NIH grant DK41301 (Los Angeles, CA); 1 : 25 000; Lyons and Thiele, 2010), or Y2R (Neuromics, Edina, MN; 1 : 4000). Tissues from all experimental groups were run through each assay at the same time for each antibody tested. It has previously been shown that the Y1R (Kopp et al, 2002) and Y2R (Brumovsky et al, 2005) antibodies do not react in knockout mice, verifying the selectively of these antibodies. Specificity of the NPY antibody was verified with colocalization of green fluorescent protein (GFP) and NPY (>95%) in NPY-sappphire-GFP transgenic mice (Pinto et al, 2004). NPY and Y1R IR were visualized using standard 3,3′-diamino-benzidine (DAB) procedures that we have described previously (Hayes et al, 2005; Lyons and Thiele, 2010; Navarro et al, 2008). Because Y2R IR is less easily detected, sections for Y2R IR underwent an amplification procedure using a Tyramide Signal Amplification (TSA) detection kit (Jackson Laboratories) to increase signal sensitivity. For the Y2R assay, we used different procedures than used with the NPY and Y1R antibodies, which were based on procedures previously used with the Y2R antibody utilized here (Brumovsky et al, 2005). For NPY and Y1R IR, digital pictures of candidate brain regions were obtained using a Nikon E400 microscope ( × 20 objective) with a Nikon Digital Sight DS-U1 digital camera run with Nikon provided software. For Y2R IR, images of candidate brain regions were obtained using a Leica SP2 upright confocal microscope with 10 × objective and Leica Confocal Software. Anatomical landmarks were carefully noted with the aid of a mouse brain atlas (Franklin and Paxinos, 1997) to ensure the same plane was used throughout the study for each region. Density staining were analyzed by a researcher blind to conditions using Image J Software (Image J, National Institute of Health, Bethesda, MD) by calculating the percentage of the total area studied that showed staining relative to subthreshold background. The size of the area was held constant between animals and groups for each region. The average of the densities for the left and right sides of the brain was calculated for analysis. Counts of NPY cell bodies, in the same area of the CeA used to quantify average densities, were scored by a group-blinded researcher (and average counts from the left and right sides were averaged for analysis).
Effects of Binge-Like Ethanol Drinking on NPY-Induced Inhibition of GABAergic Transmission in the CeA
Male C57BL/6J mice experienced three cycles of binge-like drinking with 20% (v/v) ethanol as described above. A control group of mice had access to only water throughout the experiment. At ∼24 h after the last binge-like drinking session, mice were decapitated and their brains were rapidly removed. Slice preparations of the CeA were carefully prepared and whole-cell recordings were performed as previously described (Kash and Winder, 2006). Briefly, GABAA-IPSCs were pharmacologically isolated by adding 10 μM NBQX. Signals were acquired via a Multiclamp 700B amplifier (Axon Instruments, Sunnyvale, CA), digitized, and analyzed via pClamp 10.2 software (Axon Instruments). Input resistance and series resistance were continuously monitored during experiments. Experiments in which changes in series resistance were >20% were not included in the data analysis. eIPSC experiments were analyzed by measuring the peak amplitude of the synaptic response, which was normalized to the baseline period. Data were analyzed as mean eIPSC peak amplitude over the course of the 20 min of recording and were converted as the proportion of baseline eIPSC and as the mean change of peak amplitude of eIPSC after the application of NPY relative to pre-NPY levels.
Statistical Analyses
For all experiments, differences between groups were analyzed using analysis of variance (ANOVA) or Student's t-tests. When significant differences were found, a post-hoc analysis was performed using Tukey's HSD test. Planned comparisons were performed using Student's t-tests. In all cases, p<0.05 (two tailed) was used to indicate statistical significance. For BEC measures and IR data, in some cases, data were not available for 1 to 2 animals; this accounts for occasional differences in degrees of freedom between similar analyses.
RESULTS
Effects of Centrally Administered NPY Compounds on Binge-Like Ethanol Drinking
Intracerebroventricular administration of NPY
The 3 and 10 μg doses of NPY significantly blunted binge-like ethanol drinking and associated BECs (Figure 1a and b). Two-way (cycles × dose) ANOVAs were used to analyze the Latin Square data. For drinking data, there was a significant main effect of dose (F(3, 127)=3.600; p=0.015), but neither the effect of binge drinking cycle (F(3, 127)=1.082; p=0.359) nor interaction between variables (F(9, 127)=1.234; p=0.280) differed significantly. For BEC data, a two-way ANOVA revealed a significant main effect of dose (F(3, 126)=2.730; p=0.047), but neither the effect of binge drinking cycle (F(3, 126)=1.028; p=0.383) nor the interaction between variables (F(9, 126)=1.216; p=0.291) achieved statistical significance. The post-hoc tests confirmed specific group differences. To determine if the effects of NPY were specific to ethanol intake, a control study was performed in which mice consumed a 10% (w/v) sucrose solution. A group of mice that received a 3 μg dose of NPY (n=20) was compared with vehicle-treated mice (n=19). Relative to the vehicle condition (207.78±15.23 ml/kg), the 3 μg dose of NPY did not significantly alter sucrose intake (182.18±16.79 ml/kg), evidenced by a nonsignificant one-way ANOVA (F(1, 37)=1.267; p=0.268).
NPY significantly blunted binge-like 20% ethanol consumption. (a) Central infusion (i.c.v.) of NPY dose-dependently reduced binge-like ethanol consumption (g/kg per 4 h) and (b) associated BECs (mg/dl; n=32–38 per group). NPY modulates binge-like consumption of 20% ethanol via NPY Y1R activation and Y2R inactivation. (c) The i.c.v. infusion of the Y1R agonist [D-His26]-NPY significantly reduced binge-like ethanol consumption (g/kg per 4 h; n=9 per group). (d) The i.c.v. infusion of the Y1R antagonist BIBP-3226 significantly enhanced binge-like ethanol consumption (n=24–28 per group). (e) The i.c.v. infusion of the Y2R agonist NPY13−36 did not alter binge-like ethanol consumption (n=7–10 per group), (f) but i.c.v. infusion of the Y2R antagonist BIIE-0246 significantly reduced binge-like ethanol consumption (n=8–10 per group). For each compound, i.c.v. infusions were given on day 4 of the 4-day binge-like drinking cycle. The NPY and BIBP-3226 infusion studies involved Latin Square designs in which mice experienced the various doses of compound over multiple binge-like drinking cycles. All data are shown as mean±SEM, and significance was accepted at the p<0.05 level (two tailed). *Significant differences from vehicle.
Intracerebroventricular administration of selective Y1R compounds
Having demonstrated that central NPY can selectively alter binge-like ethanol drinking, we next probed the roles of individual NPY receptors. We found that infusion of both 1 and 3 μg doses of the selective Y1R agonist, [D-His26]-NPY, significantly blunted binge-like ethanol drinking relative to the vehicle condition (Figure 1c; F(2, 24)=3.835; p=0.036). However, relative to the vehicle condition (212.43±13.88 mg/dl), mice treated with the 1 μg (166.20±29.39 mg/dl) and 3 μg (149.80±16.32 mg/dl) doses of [D-His26]-NPY did not show significantly altered BECs (F(2, 24)=2.392; p=0.113). Importantly, relative to the vehicle condition (n=19, intake=147.23±21.31 ml/kg) both a 1 μg (n=10, intake=225.46±12.95 ml/kg) and 3 μg (n=10, intake=241.97±11.40 ml/kg) dose of [D-His26]-NPY increased consumption of a 10% sucrose solution, opposite to effects on binge-like ethanol drinking (F(2, 36)=7.340; p=0.002). It is interesting that NPY (above) did not alter sucrose drinking, yet the selective Y1R agonist significantly increased sucrose drinking. The observation that Y1R and Y2R signaling have opposing effects on caloric intake (Feletou and Levens, 2005) may account for the ability of the selective Y1R agonist to more effectively stimulate sucrose drinking in our paradigm.
In order to determine if endogenous Y1R signaling regulates binge-like ethanol drinking, we next examined the impact of central infusion of the selective Y1R antagonist, BIBP-3226 (Figure 1d). Two-way (cycles × dose) ANOVAs were used to analyze the Latin Square data. For drinking data, there was a significant main effect of dose (F(2, 68)=3.379; p=0.040), but neither the main effect of binge drinking cycle (F(2, 68)=1.066; p=0.350) nor interaction between variables (F(4, 68)=1.027; p=0.780) differed significantly. However, there were no significant differences in BECs between the vehicle group (79.54±14.15 mg/dl) and the groups treated with the 0.01 μg (109.70±15.77 mg/dl) and 0.1 μg (114.01±14.62 mg/dl) doses of the Y1R antagonist. A two-way ANOVA performed on BEC data showed that the main effect of dose (F(2, 63)=1.163; p=0.319), the main effect of binge drinking cycle (F(2, 63)=1.937; p=0.153), and the interaction between variables (F(4, 63)=1.064; p=0.382) all failed to achieve statistical significance. Relative to mice treated with vehicle (n=20, intake=131.63±12.76 ml/kg) mice treated with a 0.01 μg dose of BIBP-3226 (n=20, intake=129.04±16.54 ml/kg) did not show altered consumption of a 10% sucrose solution (F(1, 38)=0.015; p=0.902).
Intracerebroventricular administration of selective Y2R compounds
We next evaluated the role of the Y2R in binge-like ethanol drinking. We found that i.c.v. infusion of a range of concentrations of the selective Y2R agonist NPY13−36 did not significantly alter binge-like ethanol drinking (Figure 1e; F(3, 32)=0.848; p=0.478)) or corresponding BECs (data not shown). Relative to vehicle-treated mice (n=12, intake=212.41±24.58 ml/kg), groups treated with the 3 μg (n=12, intake=141.88±19.43 ml/kg) and 10 μg (n=12, intake=132.04±22.38 ml/kg) doses of NPY13−36 drank significantly less of a 10% sucrose solution (F(2, 33)=3.887; p=0.030), confirming that the doses of the Y2R agonist that we used were in a physiologically relevant range. In contrast, we found that i.c.v. infusion of a 1 μg dose of the selective Y2R antagonist BIIE-0246 significantly blunted binge-like ethanol intake relative to controls (Figure 1f; F(2, 24)=3.766; p=0.039). Furthermore, relative to vehicle treatment (84.57±26.55 mg/dl), the 0.5 μg (36.04±13.75 mg/dl) and 1 μg (21.69±5.82 mg/dl) doses of the Y2R antagonist were associated with significantly reduced BECs (F(2, 24)=3.651; p=0.043). Relative to a vehicle-treated group (n=11, intake=156.10±32.15 ml/kg), a group treated with a 1 μg dose of BIIE-0246 (n=12, intake=156.10±32.15 ml/kg) did not show altered consumption of a 10% sucrose solution (F(1, 21)=0.003; p=0.954). It is interesting to note that the selective Y2R agonist reduced sucrose drinking without influencing ethanol intake, whereas the Y2R antagonist reduced ethanol drinking but did not alter sucrose consumption. It is possible that the Y2R compounds may more efficiently reduce, rather than increase, the high levels of intake characteristic of our drinking procedures. As we would predict that the Y2R agonist would, if anything, increase ethanol drinking, and that the Y2R antagonist would increase sucrose drinking, such effects may have been masked by the high baseline levels of ethanol/sucrose consumption.
A couple of additional observations require consideration. First, it should also be noted that baseline binge-like ethanol drinking (in vehicle-treated groups) varied between studies, but were within a range that we and others have similarly observed using DID procedures (Bulwa et al, 2011; Lowery et al, 2010; Sparta et al, 2008). Importantly, ethanol intake levels within this range were associated with BEC levels that were approximately at or above the BEC level consistent with binge drinking (80 mg/dl). However, given the baseline differences between studies, caution is necessary when making between-study comparisons. Second, in some experiments, compound-induced alterations of ethanol intake were not associated with significant alterations of BECs (although trends were always in the same direction). This may be related to different patterns of ethanol drinking over the 4 h test, perhaps stemming from different durations of pharmacological action between the different compounds in each study. It is also possible the NPY-related compounds are less effective in reducing BEC levels when baseline BECs are excessively high, as was the case with the study that involved the selective Y1R agonist.
Effects of Binge-Like Ethanol Drinking on NPY, Y1R, and Y2R IR
Having demonstrated that NPY, acting via Y1R and Y2R, modulates binge-like ethanol drinking, we next examined the impact of binge-like ethanol drinking on NPY, Y1R, and Y2R IR in the CeA, a region shown to be involved in dependence-like ethanol drinking (Gilpin et al, 2008). On the final binge-like ethanol drinking session, there were no significant differences between groups that experienced 1, 3, or 6 cycles of binge-like drinking (n=10/group) in terms of the amount of ethanol consumed (4.867±0.161, 5.02±0.28, and 5.13±0.274 g/kg, respectively) or BECs (112.94±10.50, 160.54±14.69, and 151.04±19.57 mg/dl, respectively). One-way ANOVAs performed on both data sets failed to achieve statistical significance.
NPY IR
NPY IR following repeated cycles of binge-like drinking of 20% ethanol are presented in Figure 2a, and representative photomicrographs of NPY IR from the CeA of mice that drank water or experienced 1, 3, or 6 cycles of binge-like ethanol drinking are presented in Figure 2b–e, respectively. Relative to water (WAT) drinking control mice, binge-like drinking of the 20% ethanol solution (1, 3, or 6 cycles) was associated with a significant reduction of NPY IR in the CeA, evidenced by a significant one-way ANOVA performed on the data set (F(3, 36)=57.551, p=0.001). However, relative to the WAT group (1.10±0.049% area), a group of mice that experienced 1 cycle of sucrose drinking (0.86±0.046% area) did not show significantly altered NPY IR. An ANOVA performed on NPY-positive cell counts in the CeA (WAT=6.4±0.562 average cells; 1 binge cycle=5.8±0.611 average cells; 3 binge cycles=4.6±0.957 average cells; 6 binge cycles=4.1±0.706 average cells) failed to achieve statistical significance (F(3, 36)=2.135, p=0.113). These latter observations suggest that significant binge-like drinking-induced reduction of NPY IR with densitometry reflects primarily a reduction of NPY in terminal processes.
Binge-like ethanol consumption of 20% ethanol significantly reduced NPY IR in the CeA. NPY IR (% total area) in the CeA after binge-like drinking of ethanol (a), and representative photomicrographs depicting NPY IR in the CeA from mice that drank water (WAT) (b) or that experienced 1 (c), 3 (d), or 6 (e) cycles of binge-like ethanol drinking. There were n=10 mice/group. All data are shown as mean±SEM, and significance was accepted at the p<0.05 level (two tailed). *Significant differences from the WAT group; #Significant differences from the WAT and one binge-like drinking cycle groups. Images were captured at a magnification of × 20, and the scale bar=100 μm.
We also assessed the effects of binge-like ethanol drinking on NPY IR in the BLA (WAT=0.385±0.026% area; 1 binge cycle=0.369±0.035% area; 3 binge cycles=0.396±0.027% area; 6 binge cycles=0.414±0.027% area) and in the medial amygdala (MeA; WAT=0.254±0.048% area; 1 binge cycle=0.257±0.035% area; 3 binge cycles=0.210±0.012% area; 6 binge cycles=0.172±0.012% area) and there were no significant group differences in either region. Representative photomicrographs of NPY IR in the BLA from the WAT group and the group experiencing one cycle of binge-like ethanol drinking are presented in Figure 4a and b, respectively.
Y1R IR
Y1R IR following repeated cycles of binge-like drinking of 20% ethanol is presented in Figure 3a, and representative photomicrographs of Y1R IR from the CeA of mice that experienced one cycle of binge-like ethanol drinking or water control mice are presented in Figure 3b and c, respectively. Binge-like drinking of the 20% ethanol solution was associated with a significant reduction of Y1R IR in the CeA, after 1, 3, or 6 binge-like drinking cycles, when compared with the WAT group (F(3, 34)=30.233, p=0.001). On the other hand, one cycle of binge-like drinking of a 3% sucrose solution (0.11±0.019% area) did not significantly alter Y1R IR in the CeA relative to the WAT group (0.11±0.008% area). We assessed the effects of binge-like ethanol drinking on Y1R IR in the BLA (WAT=0.055±0.007% area; 1 binge cycle=0.052±0.004% area; 3 binge cycles=0.048±0.004% area; 6 binge cycles=0.056±0.007% area) and in the MeA (WAT=0.062±0.005% area; 1 binge cycle=0.058±0.006% area; 3 binge cycles=0.081±0.009% area; 6 binge cycles=0.065±0.008% area), and there were no group differences in either region. Representative photomicrographs of Y1R IR in the BLA from the WAT group and the group experiencing one cycle of binge-like ethanol drinking are presented in Figure 4c and d, respectively.
Binge-like ethanol consumption of 20% ethanol significantly reduced Y1R IR in the CeA. Y1R IR (% total area) in the CeA after binge-like drinking of ethanol (a), and representative photomicrographs depicting Y1R IR in the CeA from mice that experienced one cycle of binge-like ethanol drinking (b) or drank water (WAT) (c). There were n=9–10 mice/group. All data are shown as mean±SEM, and significance was accepted at the p<0.05 level (two tailed). *Significant differences from the WAT group; #Significant differences from the WAT and one binge-like drinking cycle groups. Images were captured at a magnification of × 20 and the scale bar=100 μm.
Representative photomicrographs depicting NPY (a, b) and Y1R (c, d) IR in the BLA. Sections are from the group that drank water (a, c) or the group the experienced one cycle of binge-like ethanol drinking (b, d). Scale bar=100 μm.
Y2R IR
Y2R IR following repeated cycles of binge-like drinking of 20% ethanol is presented in Figure 5a, and representative photomicrographs of Y2R IR from the CeA of mice that experienced one cycle of binge-like ethanol drinking or water control mice are presented in Figure 5b and c, respectively. An ANOVA performed on Y2R IR data was significant (F(2, 25)=4.715, p=0.0119). However, post-hoc tests indicated that although neither binge-like drinking group differed from the water control group, one cycle of binge-like drinking of the 20% ethanol solution was associated with a significant increase of Y2R IR in the CeA when compared with the group that experienced three binge-like drinking cycles. On the other hand, one cycle of binge-like drinking of a 3% sucrose solution (122.74±6.60% area) did not alter Y2R IR in the CeA relative to the WAT group (109.39±2.72% area).
Binge-like ethanol consumption of 20% ethanol did not significantly alter Y2R IR relative to the water (WAT) control group, but Y2R IR was significantly higher in the group that experienced one cycle of binge-like drinking relative to the three cycle binge-like drinking group. Y2R IR (% total area) in the CeA after binge-like drinking of ethanol (a), and representative photomicrographs depicting Y2R IR in the CeA from a mouse that experienced one cycle of binge-like ethanol drinking (b) or drank WAT (c). There were n=7–10 mice/group. All data are shown as mean±SEM, and significance was accepted at the p<0.05 level (two tailed). #Significant differences from the group that experienced three cycles of binge-like ethanol drinking. Images were captured at a magnification of × 10, the area within the white dashed line indicates the region in which Y2R IR was quantified, and the scale bar=200 μm.
Effects of Binge-Like Ethanol Drinking on NPY-Induced Inhibition of GABAergic Transmission in the CeA
We next evaluated the impact of three cycles of binge-like ethanol drinking followed by 24 h without ethanol access or continuous water drinking on NPY modulation of GABAergic function in the CeA (Figure 6). The mice consumed an average of 5.63±0.41, 6.06±0.31, and 5.27±0.34 g/kg of ethanol on the final 4 h test day of each binge-like drinking cycle, and showed average BECs of 131.91±13.37 mg/dl when blood samples were collected immediately after the final binge-like drinking session. Initially, we examined the paired-pulse ratio (PPR) of eIPSCs in CeA neurons. Alterations in this ratio are indicative of alterations in the release of GABA, and previous experiments have demonstrated that in vapor-exposed, dependent-like animals, there is a reduced PPR in the CeA relative to controls (Roberto et al, 2004). We found that there was no difference in the PPR of eIPSCs in the CeA (Figure 6a). Additionally, we measured the frequency (Figure 6b) and the amplitude (Figure 6c) of spontaneous IPSCs, and found no significant differences between the conditions. We next evaluated the ability of 300 nM NPY to modulate GABAergic transmission in the CeA. Representative traces are shown demonstrating the effect of NPY on eIPSCs in the CeA from water-exposed and binge-like ethanol drinking mice (Figure 6d). The normalized average peak amplitude of eIPSC depicted as percentage of baseline from slice preparations from the CeA are presented in Figure 6e. A two-way (2 × 20), ethanol history × min repeated measures ANOVA revealed significant main effects of min (F(19, 228)=4.949, p=0.001), ethanol history (F(1, 12)=4.274, p=0.001), and a significant interaction effect (F(19, 228)=1.72, p=0.034). A t-test performed on eIPSC data represented as percent change relative to baseline was significant (t(12)=2.325, p=0.038; Figure 6f), and indicates that relative to the water drinking control group, a history of binge-like ethanol drinking was associated with a significant increase in NPY-induced inhibition of GABAergic transmission in the CeA.
A history of binge-like ethanol consumption significantly facilitates NPY-induced inhibition of GABAergic transmission in the CeA when assessed ∼24 h after removal of ethanol access in mice that experienced three cycles of binge-like drinking of 20% ethanol. Binge-like ethanol exposure did not alter paired-pulse ratio (a), sIPSC amplitude (b), or sIPSC frequency (c) in the CeA. Representative traces from the water (di) and binge-like ethanol-exposed mice (dii) demonstrate the impact of exogenously applied NPY on eIPSCs. Scale bars represent 100 pA and 20 ms in each panel. Exogenous application of NPY in the CeA significantly reduced eIPSC peak amplitudes (expressed as the mean proportion of baseline) (e) and baseline peak amplitudes (f), an effect that was significantly more robust in animals with a history of binge-like ethanol drinking relative to water drinking animals (n=6–8 per group). Baseline measures were taken during 0–5 min, after which NPY (300 nM) was bath applied for 5–15 min. All data are shown as mean±SEM, and significance was accepted at the p<0.05 level (two tailed). *Significant differences from the water group.
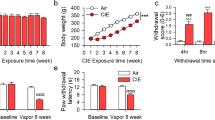
Because IR data described above were from mice that were killed immediately after the final binge-like drinking cycle, we also assessed NPY, Y1R, and Y2R IR in mice that experienced three cycles of binge-like ethanol drinking (or continuous water drinking) and were killed 24 h after the last binge-like drinking session, similar to mice from electrophysiological experiments. The mice consumed an average of 5.37±0.31, 5.38±0.22, and 5.59±0.47 g/kg of ethanol on the final 4 h test day of each binge-like drinking cycle, and showed average BECs of 148.58±37.66 mg/dl when blood samples were collected immediately after the final binge-like drinking session. Relative to water drinking control mice, mice with a history of three binge-like drinking cycles and 24 h without ethanol access showed a significant reduction of NPY IR in the CeA (Figure 7a; t(14)=2.417, p=0.03), but significant increases of Y1R (Figure 7b) and Y2R (Figure 7c) IR, confirmed by significant t-tests (t(15)=2.321, p=0.035 and t(16)=−4.808, p=0.001) for Y1R and Y2R, respectively. An ANOVA performed on NPY-positive cell counts in the CeA (WAT=10.7±0.943 average cells; 3 binge cycles=8.2±0.489 average cells) achieved statistical significance (F(1, 18)=5.531, p=0.030). Thus, blunted binge-like drinking-induced reduction of NPY IR appears to have reflected both a reduction of NPY-positive cell bodies and terminal processes. In Figure 8, representative photomicrographs of the CeA (top row, NPY IR; middle row, Y1R IR, and bottom row, Y2R IR) of mice that experienced three cycles of binge-like ethanol drinking and 24 h without ethanol access (Figure 8a, c, and e) or only drank water (Figure 8b, d, and f) are presented.
NPY IR (a), Y1R IR (b), and Y2R IR (c) (% total area) in mice that experienced three cycles of binge-like drinking of 20% ethanol and then 24 h without ethanol access or drank water (WAT) throughout the study (n=6–10 per group). All data are shown as mean±SEM, and significance was accepted at the p<0.05 level (two tailed). *Significant differences from the WAT group.
Representative photomicrographs depicting IR of NPY (a, b), Y1R (c, d), and Y2R (e, f). The left columns (a, c, and e) are from mice that experienced three cycles of binge-like ethanol drinking of 20% ethanol followed by 24 h without ethanol access, and the right columns (b, d, and f) are from mice that drank water. First scale bar=100 μm and pertains to (a–d), and the second scale bar=200 μm and pertains to (e, f). The area within the white dashed line in (e) indicates the region in which Y2R IR was quantified.
DISCUSSION
This report provides novel evidence that NPY signaling selectively modulates binge-like ethanol drinking in C57BL/6J mice. Briefly, we found that i.c.v. infusion of NPY blunted ethanol drinking associated with DID procedures. In addition, a Y1R agonist and a Y2R antagonist blunted binge-like ethanol drinking, implicating the Y1R and Y2R as key receptors in modulating this behavior. We then examined the influence of a history of binge-like ethanol drinking on NPY signaling in the CeA using immunohistochemistry and electrophysiology approaches. In support of the behavioral findings, we found that binge-like ethanol drinking reduced NPY and Y1R IR in the CeA, and removal of ethanol for 24 h following three cycles of binge-like ethanol drinking promoted increases of Y1R and Y2R IR. Electrophysiological recordings of slice preparations from the CeA showed that binge-like ethanol drinking augmented the ability of NPY to inhibit GABAergic transmission. Taken together, the present observations (and previous data with CRF1R antagonist; Lowery et al, 2010; Sparta et al, 2008) suggest that signaling in critical NPY pathways is weakened (and CRF signaling is enhanced) when sufficient amounts of ethanol have been consumed during a binge-like drinking episode, at which point administration of exogenous NPY is effective in blunting binge-like ethanol intake (either by restoring NPY signaling and/or by countering the effects of CRF). Our previous finding that a range of centrally administered NPY doses did not alter non-binge-like ethanol drinking in C57BL/6J mice (Thiele et al, 2003) suggests that NPY selectively modulates excessive ethanol intake, which is also consistent with previous work on dependence-like ethanol intake (Gilpin et al, 2008). Data from immunohistochemistry and electrophysiology studies point to the CeA as a critical brain region in which NPY modulates binge-like drinking, and future studies that directly manipulate NPY signaling in the CeA will help address this question. Importantly, to the best of our knowledge, these are the first observations of alterations of NPY and NPY receptor signaling in animals voluntarily drinking excessive amounts of ethanol, as previous work has relied on forced ethanol exposure via ethanol vapor (Criado et al, 2011; Ehlers et al, 1998; Gilpin et al, 2011; Slawecki et al, 2005; Walker et al, 2010), ethanol-containing diet (Roy and Pandey, 2002; Zhang et al, 2010), or ethanol injection (Pandey et al, 2008; Sakharkar et al, in press).
The effects of NPY on binge-like ethanol drinking appear to be reciprocally modulated by Y1R and Y2R. Central infusion of a selective Y1R agonist decreased, whereas a selective Y1R antagonist increased, binge-like ethanol intake. In contrast, central infusion of a selective Y2R agonist did not significantly alter binge-like ethanol drinking whereas central infusion of a selective Y2R antagonist significantly decreased binge-like consumption. Importantly, effective doses of selective NPY compounds (and NPY) that altered binge-like ethanol drinking did not influence 10% sucrose consumption in the same direction, suggesting that the effects of these compounds were specific to ethanol intake. Previous work has implicated roles for the Y1R and Y2R in the modulation of ethanol consumption (Thiele et al, 2002, 2004; Thorsell et al, 2002). The ability of the Y1R antagonist to significantly increase binge-like ethanol drinking suggests that Y1R signaling is engaged during binge-like drinking episodes (perhaps early on in the drinking episode); however, Y1R signaling in response to endogenous NPY is not sufficient to protect against binge-like drinking, likely because of blunted NPY signaling that develops over the course of the binge-like drinking episode (see below). The ability of the Y2R antagonist to significantly reduce binge-like ethanol drinking suggests that the Y2R is also engaged during binge-like drinking. The Y2R may be acting as an autoreceptor that reduces NPY release (Chen et al, 1997; King et al, 1999), and thus blocking Y2R would theoretically increase NPY signaling, upregulating the protective effects of NPY.
We found that binge-like ethanol drinking lead to selective alterations to the NPY systems in the CeA, as sucrose drinking did not alter NPY, Y1R, or Y2R IR. A lack of influence of binge-like drinking on NPY or Y1R IR in the BLA and MeA suggests that alterations of IR were specific to the CeA. Although caution is necessary when inferring the direction of changes in signaling based on IR data (Navarro et al, 2008), when viewed together, the pharmacological and IR data strongly suggest that over the course of a binge-like drinking episode, endogenous NPY signaling is blunted, which may motivate continued excessive binge-like drinking. Low endogenous NPY signaling can be overcome by administration of exogenous NPY or a selective Y1R agonist, or a selective Y2R antagonist (which as a presynaptic autoreceptor (Chen et al, 1997; King et al, 1999) may increase endogenous NPY signaling). Interestingly, chronic exposure to ethanol and withdrawal have been reported to cause decreased levels of NPY in the amygdala (Roy and Pandey, 2002; Zhang and Pandey, 2003), revealing similar observations between paradigms promoting binge-like drinking and dependence-like states in rodents.
Because data from the IR studies indicated an important role for the CeA in the modulation of binge-like ethanol drinking, we used in vitro slice electrophysiological procedures to study the effects of binge-like ethanol drinking on basal and NPY-induced alterations of GABAergic transmission. We found no significant differences between binge-like ethanol drinking and water control groups in terms of PPR or spontaneous GABAergic transmission, suggesting that a history of binge-like drinking did not alter basal GABAergic function. This contrasts with previous evidence indicating that baseline GABAergic transmission is upregulated in the CeA of rats previously exposed to ethanol vapor (Roberto et al, 2004), suggesting that on this measure, the effects of a history of binge-like drinking are different than the effects generated by models used to study dependence-like ethanol drinking.
In tissue from mice that had a history of three cycles of binge-like ethanol drinking and 24 h without ethanol access, NPY-induced inhibition of GABA transmission was enhanced, likely through activation of Y2R given the established role of the Y2R in modulating the effects of NPY on GABAergic transmission in the CeA (Gilpin et al, 2011). This finding was consistent with the IR results from mice in which ethanol was removed for 24 h after three cycles of binge-like ethanol drinking that also exhibited an upregulation of Y2R (and Y1R) in the CeA relative to the water drinking control group. When one considers the potential autoreceptor function of the Y2R, these changes, particularly the increase in Y2R IR, could be maladaptive, potentially leading to reduced levels of both NPY release and Y1R activation. Presynaptic Y2R also functions as a heteroreceptor that inhibits GABA release (Qian et al, 1997), which is the likely mechanism by which NPY inhibits GABAergic release here and in previous reports (Gilpin et al, 2011; Kash and Winder, 2006). When the heteroreceptor function is considered, it is possible that NPY-mediated inhibition of GABA release leads to increased excitability in downstream populations of neurons. The functional ramifications of increased downstream excitability are difficult to assess, as there are multiple populations of neurons in the lateral CeA (Haubensak et al, 2010). The present electrophysiology results complement the pharmacology and IR data, which together strongly suggest that NPY signaling in the CeA is compromised as a result of binge-like ethanol drinking in C57BL/6J mice.
It was recently reported that application of NPY to slice preparations from the CeA decreased baseline GABAergic transmission and inhibited ethanol-induced stimulation of GABAergic activity (Gilpin et al, 2011). Interestingly, although we observed increased NPY-induced inhibition of GABAergic activity in the CeA of mice with a history of binge-like ethanol drinking, Gilpin et al (2011) found no such differences between vapor-exposed and naive rats, which is additional evidence that the mechanisms that drive excessive ethanol intake in models of binge-like drinking and dependence-like drinking are not identical. Although we cannot rule out species differences as the cause of discrepant results, one striking dissimilarity between our study and that of Gilpin et al (2011) is that we studied excessive ethanol intake in rodents that voluntarily drank ethanol, whereas Gilpin et al (2011) studied excessive ethanol intake in animals that had prior forced ethanol exposure via vapor inhalation.
Importantly, Gilpin et al (2011) also found that prophylactic application of NPY during ethanol vapor exposure protected against the development of vapor-induced ethanol drinking. These observations, in tandem with data indicating that the direct application of NPY into the CeA protects against vapor-induced dependence-like drinking (Gilpin et al, 2008), further reinforce the hypothesis that the dysregulation of NPY signaling in the CeA contributes to uncontrolled and excessive ethanol intake (Koob, 2003; Koob and Le Moal, 2001). We propose that a similar (although not identical) dysregulation of NPY signaling occurs within the CeA during the course of a binge-like drinking episode. We speculate that blunted NPY signaling that unfolds during the course of a binge can motivate binge-like drinking in a manner similar to the role of blunted NPY signaling in motivating vapor-induced dependence-like drinking, and that dysregulation of NPY becomes rigid with repeated binge episodes, contributing to the transition to dependence. Viewed this way, in addition to being potential pharmaceutical targets for treating excessive ethanol intake resulting from dependence, the current data suggest that NPY compounds (Y1R agonists and Y2R antagonists) may also be useful for curbing and/or preventing binge drinking, ultimately protecting vulnerable individuals from progressing to the point of ethanol dependence. Because neuroplastic changes that develop in the brain with the development of dependence are thought to be longlasting and the underlying cause of uncontrolled excessive ethanol intake characteristic of dependent individuals (Koob, 2003; Koob and Le Moal, 2001), treating at-risk individuals suffering from alcohol abuse disorders before they have become dependent may be a more effective approach than treatments that are aimed at individuals who have already become dependent.
References
Bacchi F, Mathe AA, Jimenez P, Stasi L, Arban R, Gerrard P et al (2006). Anxiolytic-like effect of the selective neuropeptide Y Y2 receptor antagonist BIIE0246 in the elevated plus-maze. Peptides 27: 3202–3207.
Badia-Elder NE, Stewart RB, Powrozek TA, Murphy JM, Li TK (2003). Effects of neuropeptide Y on sucrose and ethanol intake and on anxiety-like behavior in high alcohol drinking (HAD) and low alcohol drinking (LAD) rats. Alcohol Clin Exp Res 27: 894–899.
Badia-Elder NE, Stewart RB, Powrozek TA, Roy KF, Murphy JM, Li TK (2001). Effect of neuropeptide Y (NPY) on oral ethanol intake in Wistar, alcohol-preferring (P), and -nonpreferring (NP) rats. Alcohol Clin Exp Res 25: 386–390.
Brumovsky P, Stanic D, Shuster S, Herzog H, Villar M, Hokfelt T (2005). Neuropeptide Y2 receptor protein is present in peptidergic and nonpeptidergic primary sensory neurons of the mouse. J Comp Neurol 489: 328–348.
Bulwa ZB, Sharlin JA, Clark PJ, Bhattacharya TK, Kilby CN, Wang Y et al (2011). Increased consumption of ethanol and sugar water in mice lacking the dopamine D2 long receptor. Alcohol 45: 631–639.
Chen X, DiMaggio DA, Han SP, Westfall TC (1997). Autoreceptor-induced inhibition of neuropeptide Y release from PC-12 cells is mediated by Y2 receptors. Am J Physiol 273 (4 Pt 2): H1737–H1744.
Criado JR, Liu T, Ehlers CL, Mathe AA (2011). Prolonged chronic ethanol exposure alters neuropeptide Y and corticotropin-releasing factor levels in the brain of adult Wistar rats. Pharmacol Biochem Behav 99: 104–111.
Doods H, Gaida W, Wieland HA, Dollinger H, Schnorrenberg G, Esser F et al (1999). BIIE0246: a selective and high affinity neuropeptide Y Y(2) receptor antagonist. Eur J Pharmacol 384: R3–R5.
Doods HN, Wieland HA, Engel W, Eberlein W, Willim KD, Entzeroth M et al (1996). BIBP 3226, the first selective neuropeptide Y1 receptor antagonist: a review of its pharmacological properties. Regul Peptides 65: 71–77.
Ehlers CL, Li TK, Lumeng L, Hwang BH, Somes C, Jimenez P et al (1998). Neuropeptide Y levels in ethanol-naive alcohol-preferring and nonpreferring rats and in Wistar rats after ethanol exposure. Alcohol Clin Exp Res 22: 1778–1782.
Feletou M, Levens NR (2005). Neuropeptide Y2 receptors as drug targets for the central regulation of body weight. Curr Opin Investig Drugs 6: 1002–1011.
Finn DA, Snelling C, Fretwell AM, Tanchuck MA, Underwood L, Cole M et al (2007). Increased drinking during withdrawal from intermittent ethanol exposure is blocked by the CRF receptor antagonist d-Phe-CRF(12-41). Alcohol Clin Exp Res 31: 939–949.
Franklin KBJ, Paxinos G (1997). The Mouse Brain in Stereotaxic Coordinates. Academic Press: San Diego, CA.
Funk CK, O′Dell LE, Crawford EF, Koob GF (2006). Corticotropin-releasing factor within the central nucleus of the amygdala mediates enhanced ethanol self-administration in withdrawn, ethanol-dependent rats. J Neurosci 26: 11324–11332.
Gehlert DR, Cippitelli A, Thorsell A, Le AD, Hipskind PA, Hamdouchi C et al (2007). 3-(4-Chloro-2-morpholin-4-yl-thiazol-5-yl)-8-(1-ethylpropyl)-2,6-dimethyl- imidazo[1,2-b]pyridazine: a novel brain-penetrant, orally available corticotropin-releasing factor receptor 1 antagonist with efficacy in animal models of alcoholism. J Neurosci 27: 2718–2726.
Gerald C, Walker MW, Criscione L, Gustafson EL, Batzlhartmann C, Smith KE et al (1996). A receptor subtype involved in neuropeptide-Y-induced food intake. Nature 382: 168–171.
Gilpin NW, Misra K, Herman MA, Cruz MT, Koob GF, Roberto M (2011). Neuropeptide Y opposes alcohol effects on gamma-aminobutyric acid release in amygdala and blocks the transition to alcohol dependence. Biol Psychiatry 69: 1091–1099.
Gilpin NW, Misra K, Koob GF (2008). Neuropeptide Y in the central nucleus of the amygdala suppresses dependence-induced increases in alcohol drinking. Pharmacol Biochem Behav 90: 475–480.
Gmel G, Bissery A, Gammeter R, Givel JC, Calmes JM, Yersin B et al (2006). Alcohol-attributable injuries in admissions to a swiss emergency room--an analysis of the link between volume of drinking, drinking patterns, and preattendance drinking. Alcohol Clin Exp Res 30: 501–509.
Gupta T, Syed YM, Revis AA, Miller SA, Martinez M, Cohn KA et al (2008). Acute effects of acamprosate and MPEP on ethanol Drinking-in-the-Dark in male C57BL/6J mice. Alcohol Clin Exp Res 32: 1992–1998.
Haubensak W, Kunwar PS, Cai H, Ciocchi S, Wall NR, Ponnusamy R et al (2010). Genetic dissection of an amygdala microcircuit that gates conditioned fear. Nature 468: 270–276.
Hayes DM, Knapp DJ, Breese GR, Thiele TE (2005). Comparison of basal NPY and CRF levels between the high ethanol drinking C57BL/6J and low ethanol drinking DBA/2J inbred mouse strains. Alcohol Clin Exp Res 29: 721–729.
Hendrickson LM, Zhao-Shea R, Tapper AR (2009). Modulation of ethanol drinking-in-the-dark by mecamylamine and nicotinic acetylcholine receptor agonists in C57BL/6J mice. Psychopharmacology (Berl) 204: 563–572.
Hingson R, Heeren T, Winter M, Wechsler H (2005). Magnitude of alcohol-related mortality and morbidity among U.S. college students ages 18–24: changes from 1998 to 2001. Annu Rev Public Health 26: 259–279.
Hingson RW, Heeren T, Winter MR (2006). Age of alcohol-dependence onset: associations with severity of dependence and seeking treatment. Pediatrics 118: e755–e763.
Kamdar NK, Miller SA, Syed YM, Bhayana R, Gupta T, Rhodes JS (2007). Acute effects of naltrexone and GBR 12909 on ethanol drinking-in-the-dark in C57BL/6J mice. Psychopharmacology (Berl) 192: 207–217.
Kash TL, Winder DG (2006). Neuropeptide Y and corticotropin-releasing factor bi-directionally modulate inhibitory synaptic transmission in the bed nucleus of the stria terminalis. Neuropharmacology 51: 1013–1022.
Kaur S, Ryabinin AE (2010). Ghrelin receptor antagonism decreases alcohol consumption and activation of perioculomotor urocortin-containing neurons. Alcohol Clin Exp Res 34: 1525–1534.
King PJ, Widdowson PS, Doods HN, Williams G (1999). Regulation of neuropeptide Y release by neuropeptide Y receptor ligands and calcium channel antagonists in hypothalamic slices. J Neurochem 73: 641–646.
King PJ, Williams G, Doods H, Widdowson PS (2000). Effect of a selective neuropeptide Y Y(2) receptor antagonist, BIIE0246 on neuropeptide Y release. Eur J Pharmacol 396: R1–R3.
Koob GF (2003). Alcoholism: allostasis and beyond. Alcohol Clin Exp Res 27: 232–243.
Koob GF, Le Moal M (2001). Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacology 24: 97–129.
Kopp J, Xu ZQ, Zhang X, Pedrazzini T, Herzog H, Kresse A et al (2002). Expression of the neuropeptide Y Y1 receptor in the CNS of rat and of wild-type and Y1 receptor knock-out mice. Focus on immunohistochemical localization. Neuroscience 111: 443–532.
Linsenbardt DN, Boehm 2nd SL (2009). Agonism of the endocannabinoid system modulates binge-like alcohol intake in male C57BL/6J mice: involvement of the posterior ventral tegmental area. Neuroscience 164: 424–434.
Lowery EG, Spanos M, Navarro M, Lyons AM, Hodge CW, Thiele TE (2010). CRF-1 antagonist and CRF-2 agonist decrease binge-like ethanol drinking in C57BL/6J mice independent of the HPA axis. Neuropsychopharmacology 35: 1241–1252.
Lyons AM, Thiele TE (2010). Neuropeptide Y conjugated to saporin alters anxiety-like behavior when injected into the central nucleus of the amygdala or basomedial hypothalamus in BALB/cJ mice. Peptides 31: 2193–2199.
Melon L, Boehm 2nd SL (2011). GABA(A) receptors in the posterior, but not anterior, ventral tegmental area mediate Ro15-4513-induced attenuation of binge-like ethanol consumption in C57BL/6J female mice. Behav Brain Res 220: 230–237.
Miller JW, Naimi TS, Brewer RD, Jones SE (2007). Binge drinking and associated health risk behaviors among high school students. Pediatrics 119: 76–85.
Moore EM, Boehm 2nd SL (2009). Site-specific microinjection of baclofen into the anterior ventral tegmental area reduces binge-like ethanol intake in male C57BL/6J mice. Behav Neurosci 123: 555–563.
Mullins D, Kirby D, Hwa J, Guzzi M, Rivier J, Parker E (2001). Identification of potent and selective neuropeptide Y Y(1) receptor agonists with orexigenic activity in vivo. Mol Pharmacol 60: 534–540.
Nakhate KT, Dandekar MP, Kokare DM, Subhedar NK (2009). Involvement of neuropeptide Y Y(1) receptors in the acute, chronic and withdrawal effects of nicotine on feeding and body weight in rats. Eur J Pharmacol 609: 78–87.
Navarro M, Cubero I, Knapp DJ, Breese GR, Thiele TE (2008). Decreased immunoreactivity of the melanocortin neuropeptide alpha-melanocyte-stimulating hormone (alpha-MSH) after chronic ethanol exposure in Sprague-Dawley rats. Alcohol Clin Exp Res 32: 266–276.
Naveilhan P, Neveu I, Arenas E, Ernfors P (1998). Complementary and overlapping expression of Y1, Y2 and Y5 receptors in the developing and adult mouse nervous system. Neuroscience 87: 289–302.
Okoro CA, Brewer RD, Naimi TS, Moriarty DG, Giles WH, Mokdad AH (2004). Binge drinking and health-related quality of life: do popular perceptions match reality? Am J Prev Med 26: 230–233.
Palmiter RD, Erickson JC, Hollopeter G, Baraban SC, Schwartz MW (1998). Life without neuropeptide Y. Recent Prog Horm Res 53: 163–199.
Pandey SC, Ugale R, Zhang H, Tang L, Prakash A (2008). Brain chromatin remodeling: a novel mechanism of alcoholism. J Neurosci 28: 3729–3737.
Pinto S, Roseberry AG, Liu H, Diano S, Shanabrough M, Cai X et al (2004). Rapid rewiring of arcuate nucleus feeding circuits by leptin. Science 304: 110–115.
Qian J, Colmers WF, Saggau P (1997). Inhibition of synaptic transmission by neuropeptide Y in rat hippocampal area CA1: modulation of presynaptic Ca2+ entry. J Neurosci 17: 8169–8177.
Rhodes JS, Best K, Belknap JK, Finn DA, Crabbe JC (2005). Evaluation of a simple model of ethanol drinking to intoxication in C57BL/6J mice. Physiol Behav 84: 53–63.
Roberto M, Madamba SG, Stouffer DG, Parsons LH, Siggins GR (2004). Increased GABA release in the central amygdala of ethanol-dependent rats. J Neurosci 24: 10159–10166.
Roy A, Pandey SC (2002). The decreased cellular expression of neuropeptide Y protein in rat brain structures during ethanol withdrawal after chronic ethanol exposure. Alcohol Clin Exp Res 26: 796–803.
Sajja RK, Rahman S (2011). Lobeline and cytisine reduce voluntary ethanol drinking behavior in male C57BL/6J mice. Prog Neuropsychopharmacol Biol Psychiatry 35: 257–264.
Sakharkar AJ, Zhang H, Tang L, Shi G, Pandey SC et al. Histone deacetylases (HDAC)-induced histone modifications in the amygdala: a role in rapid tolerance to the anxiolytic effects of ethanol. Alcohol Clin Exp Res; (e-pub ahead of print 25 July 2011).
Shepherd JP, Sutherland I, Newcombe RG (2006). Relations between alcohol, violence and victimization in adolescence. J Adolesc 29: 539–553.
Slawecki CJ, Jimenez-Vasquez P, Mathe AA, Ehlers CL (2005). Effect of ethanol on brain neuropeptides in adolescent and adult rats. J Stud Alcohol 66: 46–52.
Smith-White MA, Hardy TA, Brock JA, Potter EK (2001). Effects of a selective neuropeptide Y Y2 receptor antagonist, BIIE0246, on Y2 receptors at peripheral neuroeffector junctions. Br J Pharmacol 132: 861–868.
Sorensen G, Lindberg C, Wortwein G, Bolwig TG, Woldbye DP (2004). Differential roles for neuropeptide Y Y1 and Y5 receptors in anxiety and sedation. J Neurosci Res 77: 723–729.
Sparta DR, Sparrow AM, Lowery EG, Fee JR, Knapp DJ, Thiele TE (2008). Blockade of the corticotropin releasing factor type 1 receptor attenuates elevated ethanol drinking associated with drinking in the dark procedures. Alcohol Clin Exp Res 32: 259–265.
Thiele TE, Cubero I, van Dijk G, Mediavilla C, Bernstein IL (2000). Ethanol-induced c-Fos expression in catecholamine- and neuropeptide Y-producing neurons in rat brainstem. Alcohol Clin Exp Res 24: 802–809.
Thiele TE, Koh MT, Pedrazzini T (2002). Voluntary alcohol consumption is controlled via the neuropeptide Y Y1 receptor. J Neurosci 22: RC208.
Thiele TE, Naveilhan P, Ernfors P (2004). Assessment of ethanol consumption and water drinking by NPY Y2 receptor knockout mice. Peptides 25: 975–983.
Thiele TE, Sparta DR, Fee JR, Navarro M, Cubero I (2003). Central neuropeptide Y alters ethanol-induced sedation, but not ethanol intake, in C57BL/6 mice. Alcohol 31: 155–160.
Thorsell A, Rimondini R, Heilig M (2002). Blockade of central neuropeptide Y (NPY) Y2 receptors reduces ethanol self-administration in rats. Neurosci Lett 332: 1–4.
Valdez GR, Roberts AJ, Chan K, Davis H, Brennan M, Zorrilla EP et al (2002). Increased ethanol self-administration and anxiety-like behavior during acute ethanol withdrawal and protracted abstinence: regulation by corticotropin-releasing factor. Alcohol Clin Exp Res 26: 1494–1501.
Wahlestedt C, Yanaihara N, H:akanson R (1986). Evidence for different pre-and post-junctional receptors for neuropeptide Y and related peptides. Regul Peptides 13: 307–301.
Walker BM, Drimmer DA, Walker JL, Liu T, Mathe AA, Ehlers CL (2010). Effects of prolonged ethanol vapor exposure on forced swim behavior, and neuropeptide Y and corticotropin-releasing factor levels in rat brains. Alcohol 44: 487–493.
Zhang H, Pandey SC (2003). Effects of PKA modulation on the expression of neuropeptide Y in rat amygdaloid structures during ethanol withdrawal. Peptides 24: 1397–1402.
Zhang H, Sakharkar AJ, Shi G, Ugale R, Prakash A, Pandey SC (2010). Neuropeptide Y signaling in the central nucleus of amygdala regulates alcohol-drinking and anxiety-like behaviors of alcohol-preferring rats. Alcohol Clin Exp Res 34: 451–461.
Acknowledgements
This work was supported by NIH grants AA013573, AA015148, AA017818, AA017803, AA019839, AA017668, and AA019454, an ABMRF Research Grant, and an INIA-Stress Pilot Project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Neuropsychopharmacology website
Supplementary information
Rights and permissions
About this article
Cite this article
Sparrow, A., Lowery-Gionta, E., Pleil, K. et al. Central Neuropeptide Y Modulates Binge-Like Ethanol Drinking in C57BL/6J Mice via Y1 and Y2 Receptors. Neuropsychopharmacol 37, 1409–1421 (2012). https://doi.org/10.1038/npp.2011.327
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2011.327
Keywords
This article is cited by
-
Basolateral amygdala neuropeptide Y system modulates binge ethanol consumption
Neuropsychopharmacology (2024)
-
Kappa opioid receptor and dynorphin signaling in the central amygdala regulates alcohol intake
Molecular Psychiatry (2021)
-
Importance of sex and trauma context on circulating cytokines and amygdalar GABAergic signaling in a comorbid model of posttraumatic stress and alcohol use disorders
Molecular Psychiatry (2021)
-
Medial prefrontal cortex neuropeptide Y modulates binge-like ethanol consumption in C57BL/6J mice
Neuropsychopharmacology (2019)
-
Dynorphin-kappa opioid receptor activity in the central amygdala modulates binge-like alcohol drinking in mice
Neuropsychopharmacology (2019)