Abstract
Preclinical studies suggest that lithium may exert neurotrophic effects that counteract pathological processes in the brain of patients with bipolar disorder (BD). To describe and compare the course and magnitude of gray matter volume changes in patients with BD who are treated with lithium or valproic acid (VPA) compared to healthy comparison subjects, and to assess clinical relationships to gray matter volume changes induced by lithium in patients with BD, we conducted longitudinal brain imaging and clinical evaluations of treatment response in 22 mood-stabilizing and antipsychotic medications-naive patients with BD who were randomly assigned to either lithium or VPA treatment after baseline assessment. Fourteen healthy comparison subjects did not take any psychotropic medications during follow-up. Longitudinal data analyses of 93 serial magnetic resonance images revealed lithium-induced increases in gray matter volume, which peaked at week 10–12 and were maintained through 16 weeks of treatment. This increase was associated with positive clinical response. In contrast, VPA-treated patients with BD or healthy comparison subjects did not show gray matter volume changes over time. Results suggest that lithium induces sustained increases in cerebral gray matter volume in patients with BD and that these changes are related to the therapeutic efficacy of lithium.
Similar content being viewed by others
INTRODUCTION
Lithium, a monovalent cation, remains one of the first-line drugs for acute and maintenance treatment of bipolar disorder (BD) (Schou, 1997). Lithium is hypothesized to exert complex neuroprotective or neurotrophic effects that counteract pathological processes in the brain of patients with BD (Drevets et al, 1997; Rajkowska, 2000), most importantly by increasing cellular resilience and altering synaptic plasticity and neuronal morphology (Manji et al, 1999).
In vivo studies have also suggested protective and potentially regenerative brain effects of lithium in BD (Kempton et al, 2008; Bearden et al, 2007; Sassi et al, 2002; Kessing et al, 2008; Moore et al, 2000; Moore et al, 2009). Two cross-sectional brain magnetic resonance imaging (MRI) studies have reported that patients with BD on lithium treatment had greater gray matter (GM) volumes compared to patients with BD who were not (Bearden et al, 2007; Sassi et al, 2002). A recent meta-analysis suggested associations between lithium treatment in patients with BD and GM volume increases (Kempton et al, 2008). Lithium has also been reported to have a protective effect against dementia development in patients with BD (Kessing et al, 2008).
Moore et al (2000) have first reported that lithium treatment over a 4-week period increased GM volume by about 3% in 10 patients with BD. The same group has recently replicated this finding in 28 patients with BD who went through a 4-week lithium treatment (Moore et al, 2009). GM volume increases were primarily confined to treatment responders and prefrontal GM volume increases were also noted.
To date, it has not been shown whether acute increases in GM volume in response to short-term lithium administration persist during longer duration of treatment or its temporal relationship with clinical improvement. A study design that includes a comparison therapy in drug-naive BD and the control data to evaluate the stability of GM volume measurements over time would be more desirable in further characterizing the nature of lithium-related GM changes.
In an effort to address these questions, a longitudinal brain imaging study was conducted to assess brain GM and white matter (WM) volume changes and clinical improvement in medication-free patients with BD, naive to mood-stabilizers and antipsychotic medications. Valproic acid (VPA), a mood-stabilizing medication with clinical efficacy similar to lithium and a potentially different mechanism of action, was used as a comparison treatment. Age and sex-matched healthy comparison subjects (n=14) were longitudinally scanned to assess measurement variations in GM and WM volumes over time.
MATERIALS AND METHODS
Participants
Subjects were recruited from the University of Washington (UW) Center for Anxiety and Depression and the Bipolar Research Programs at McLean Hospital and Massachusetts General Hospital (MGH). This sample has been described in detail in prior magnetic resonance spectroscopy (MRS) studies of brain chemical alterations at baseline (Dager et al, 2004) and in response to treatment (Friedman et al, 2004). Among subjects who took part in previous MRS studies (Dager et al, 2004; Friedman et al, 2004), 25 medication-free patients with BD and 27 healthy comparison subjects were initially enrolled in this study. Of these subjects, 22 patients with BD and 14 healthy comparison subjects had usable baseline and at least one follow-up MRI scans for inclusion in data analyses for the longitudinal study (Table 1).
All subjects provided written informed consent that was approved by the institutional review boards of the participating institutions. Patients with BD had no other Axis I psychiatric diagnosis, including lifetime history of alcohol and/or other drug dependence or abuse. None of the patients with BD had ever been treated with mood-stabilizing or antipsychotic medications. Nine patients with BD had previously been prescribed antidepressants, but all were medication-free for a minimum of 2 months before enrollment.
Healthy comparison subjects had no current or previous DSM-IV Axis I diagnosis, including history of alcohol and/or other drug dependence or abuse within 6 months of study entrance. A history of significant psychiatric disorders in first-degree relatives was also an exclusion criterion. Any subject with clinically significant medical problems, including cerebral vascular disease, pulmonary disease, endocrine disorders, severe sensory or motor impairments, documented head trauma, or metal implants was excluded from the study.
Patients with BD were randomly assigned to receive lithium (n=13) or VPA (n=9) in a flexible dosing schedule. Four lithium-treated patients and five VPA-treated patients had one additional MR examinations during treatment; four lithium-treated patients and one VPA-treated patient had two additional MR examinations; five lithium-treated patients and three VPA-treated patients had three additional MR examinations. The mean duration of treatment for patients with BD was 81.8 days (SD, 23.0; range, 46–112 days) for the lithium-treated group and 52.6 days (SD, 35.9; range, 12–112 days) for the VPA-treated group. Healthy comparison subjects underwent additional MR scans at 64.8 days (SD, 18.9; range, 29–99 days) subsequent to baseline scans.
Assessment
Mood state at baseline and before each MR examination was assessed using the 17-item Hamilton Depression Rating Scale (HDRS) (Hamilton, 1960) and the Young Mania Rating Scale (YMRS) (Young et al, 1978).
Urine toxicology screens obtained before each MR scan were required to be negative for psychoactive substances, other than the treatment medication. Serum lithium and VPA levels were obtained at each MR scan or more frequently as clinically warranted, and dosing for lithium and VPA was adjusted to achieve serum levels of 0.6–0.8 mEq/l and 50–100 ng/ml, respectively. Mean blood levels of lithium and VPA during the study period were 0.65 mEq/l (SD 0.19) and 56.3 ng/ml (SD 24.5), respectively. No subject was on concomitant medications during the study.
MRI Acquisition and Tissue Segmentation
Participants underwent MRI scanning on clinical 1.5 T SIGNA whole-body scanners (GE Medical Systems, Milwaukee, WI), equipped at both sites with version 5.8 Genesis operating software. Identical protocols for MRI acquisition were used at the study sites. Custom-made receive-only linear birdcage coils with approximately 40% improved signal-to-noise ratio and enhanced coil homogeneity over conventional quadrature head coils (Dager et al, 2004) were used at both sites.
A three-dimensional spoiled gradient echo pulse sequence was used to acquire 124 1.5-mm-thick contiguous coronal images (echo time (TE)=5 ms, repetition time (TR)=35 ms, 256 × 192 matrix, field of view=24 cm, flip angle=45°, number of excitations=1) for baseline scans. Axial proton density and T2-weighted images were obtained for all baseline and follow-up scans (TE=30/80 ms; TR=3000 ms; 256 × 192 matrix; field of view=24 cm; flip angle=45°; 0.5 number of excitations, 3-mm-thick slices, no skip).
All image analyses were performed under blinded conditions. T2 axial image series were used for segmentation to maximize longitudinal data availability. A series of semiautomatic processing steps were applied to baseline and follow-up scans before tissue segmentation. All images were corrected for intensity nonuniformity. Follow-up images of an individual were aligned to his/her baseline image using a nine-parameter linear spatial transformation (Ashburner et al, 2003; Ashburner and Friston, 2001).
Segmentations of baseline and aligned follow-up scans into images of GM, WM, and cerebrospinal fluid (CSF) were performed on the basis of voxel intensity and spatial information with a cluster analysis of the Statistical Parametric Mapping application (SPM; Wellcome Department of Imaging Neuroscience, London). Non-brain tissues and brain stem below the level of the foramen magnum were manually removed. Probability maps for GM, WM, and CSF were then processed to quantify volume by multiplying the number of voxels with probability values for each tissue by the voxel volume. This SPM-based method to estimate GM and WM volumes has been shown to be robust, with acceptable reliability and reproducibility for quantitative analysis of MRI (Ananth et al, 2002; Chard et al, 2002). Validation of this SPM-based tissue classification methodology using T2 image data is presented in Supplementary Material.
Statistical Analysis
Demographic and clinical variables of continuous and categorical nature were compared between groups using an unpaired t-test and a χ2-test, respectively. Nonparametric statistics were used as appropriate.
For baseline assessments, we compared the GM and WM volumes of patients with BD and healthy comparison subjects using an analysis of covariance controlling for age, sex, and intracranial volume (ICV).
A mixed-model regression analysis was used to test whether there was a significant difference in clinical improvement as assessed by HDRS or YMRS scores between the lithium- and VPA-treated groups. A linear model for the effect of time was constructed with age, sex, and baseline HDRS or YMRS scores as covariates. The interaction term between the treatment group and time was also tested.
Longitudinal image data analyses were conducted using a mixed-model regression analysis with imaging data of 93 scans from 36 subjects (13 lithium-treated patients with BD, 9 VPA-treated patients with BD, and 14 healthy comparison subjects) in an effort to obtain the best fit for GM/WM trajectories. Mixed-model regression analysis permits the use of data with different observations per subject and irregular intervals (Gueorguieva and Krystal, 2004; Hennen, 2003).
Change values for GM and WM volumes, calculated by subtracting the baseline GM and WM volumes from each follow-up value and then dividing by the baseline values, were used in all longitudinal analyses. For a realistic and flexible assumption for the effects of medications on changes in GM and WM volumes, we used polynomial models, including linear-order and quadratic-order trends, for the effects of time. The likelihood ratio test was performed to compare models, then the best-fitting model with the smallest number of terms was selected.
First, we estimated within-group changes in GM and WM volumes in each group over time using a polynomial mixed-model regression analysis. Age, sex, and study site (UW or Mclean Hospital/MGH) were included as covariates. Second, to assess whether the pattern of changes in the GM and WM volumes over time would differ between the three groups (lithium vs VPA vs control groups), trend lines plotted during the follow-up period were compared with an interaction term between time and the group as an indicator. The time term was allowed to vary between individuals as a random effect. All analyses were conducted adjusting for age, sex, and study sites.
To assess the clinical relevance of GM volume changes induced by lithium treatment, we used Spearman correlation analyses to examine the relationship between slopes for HDRS scores and GM volume changes in lithium- and VPA-treated patients with BD. Slopes for the GM volume were also calculated using the baseline and follow-up scans on the presumption that changes in GM volumes were linear. Although GM changes in lithium-treated subjects were fitted with a quadratic model, this assumption of linearity helps make the interpretation of the relationship to be easier and intuitive (Keller et al, 2003).
Statistical significances were defined at an α level of <0.05 with two-tailed tests.
RESULTS
Characteristics of Study Participants
There were no significant differences in age or sex composition between patients with BD and healthy comparison subjects or between lithium- and VPA-treated patients with BD. There was no significant difference between lithium- and VPA-treated patients with BD in clinical characteristics of bipolar subtype, age at onset, duration of illness or baseline YMRS scores. With the use of the structured psychiatric interview, 9 (5 men, 4 women; mean age 32.1 years, SD 6.4) and 13 (5 men, 8 women; mean age 28.8 years, SD 10.3) patients with BD were classified as bipolar I and II disorders, respectively. Average illness duration was 13.4 years (SD, 6.9) and mean onset age for BD was 16.7 years (SD, 8.5; range, 8.4–38.4 years).
On the basis of clinical evaluation and YMRS scores at baseline, no subjects with BD were assessed as being in a manic phase at study entrance. Among 22 patients with BD, 19 subjects (86.4%) were in the depressed mood state and 3 (13.6%) were in the euthymic mood state at the time of baseline examination. Although randomly assigned, lithium-treated patients with BD had lower HDRS scores than VPA-treated patients with BD (16.3±10.1 vs 24.1±3.9, respectively, p=0.05) (Table 1). There were no significant differences in baseline global cerebral measures of GM, WM, or CSF between groups (Table 1).
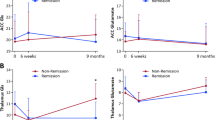
GM and WM Volume Change Over Time: Within-Group Changes
First, GM and WM volume longitudinal changes were examined for each group. In lithium-treated patients with BD, a significant increase in GM volume over time was found with a linear term for the time variable (z=4.22, p<0.001). Because the addition of a quadratic term improved the model fit for predicting GM volume changes (p<0.001), a quadratic mixed-model regression analysis for time and time-squared effects was used to estimate GM volume changes. Both linear (z=5.98, p<0.001) and quadratic terms (z=−4.40, p<0.001) for time were significant in the model. A similar pattern of changes was observed when GM ratio measures were used (GM volume/ICV) in lithium-treated patients (linear and quadratic time terms, z=5.54, p<0.001 and z=−3.91, p<0.001, respectively).
A quadratic regression model was not significantly better than a linear regression fit in assessing the time effect on WM volume changes, so a linear model was used to estimate WM changes. WM volumes did not significantly change over time with lithium treatment (z=−1.05, p=0.30).
There were no significant changes in GM or WM volumes during the study period in VPA-treated patients with BD (GM and WM changes, z=0.68, p=0.50 and z=−0.36, p=0.72, respectively) or in healthy controls (GM and WM changes, z=−0.16, p=0.88 and z=0.92, p=0.36, respectively).
GM and WM Volume Change Over Time: Between-Group Comparisons
We next constructed a multivariable mixed-effect regression model to estimate differential trends in GM and WM volume changes between the three groups. There was an interaction effect between group and time with regard to the GM volume changes. As shown in Figure 1a, the pattern of changes in GM volume during the 16-week follow-up period in lithium-treated patients with BD differed from VPA-treated patients with BD (p for interaction=0.02), as well as from healthy controls (p for interaction=0.001). There was no difference between VPA-treated with BD and healthy control groups. For lithium-treated patients with BD, the estimated GM volume increase that peaked at 11.5 weeks was 2.56% (95% CI=2.43–2.69) and equivalent to 17.6 cm3 (95% CI=16.7–18.5) (Figure 2a).
Estimated gray and white matter volume changes for participants during 16 weeks of study period. (a) Trend lines of gray matter volume changes from baseline were fitted by use of quadratic mixed-effect regression modeling (blue line for Li-treated patients with BD, green line for VPA-treated patients with BD, and gray line for healthy comparison subjects). The trend of changes in gray matter volume in Li-treated patients with BD differed significantly from that in VPA-treated patients (p for interaction=0.02) and from that in healthy comparison subjects (p for interaction=0.001). Age, sex, and study site were included as covariates in these models. (b) Trend lines of white matter volume changes from baseline were fitted by use of linear mixed-effect regression modeling (blue line for Li-treated bipolar patients, green line for VPA-treated bipolar patients, and gray line for healthy comparison subjects). The trend of changes in white matter volume in Li-treated patients with BD did not differ from that in VPA-treated patients (p for interaction=0.99) and from that in healthy comparison subjects (p for interaction=0.18). Age, sex, and study site were included as covariates in these models. GM, gray matter; Li, lithium; VPA, valproic acid; WM, white matter. See online version for colour information.
Individual trajectories in gray and white matter volumes and their fitted trend lines for lithium-treated (a) and valproic acid-treated (b) bipolar disorder patients. Trend lines of gray matter volume changes from baseline were fitted by use of quadratic mixed-effect regression modeling (blue dotted line). White matter volume changes were fitted by use of linear mixed-effect regression modeling (gray dotted line). Age, sex, and study site were included as covariates in these models. GM, gray matter; ICV, intracranial volume; WM, white matter. See online version for colour information.
There were no significant differences in WM volume changes between the three groups during the study period (lithium- vs VPA-treated patients with BD, p for interaction=0.99; lithium-treated patients with BD vs healthy comparison subjects, p for interaction=0.18) (Figure 1b). Changes in GM and WM volumes, and ICV of each patient during the follow-up period in lithium- and VPA-treated groups with BD are shown in Figure 2.
When analyses were conducted adjusting for bipolar subtype and baseline HDRS scores, there was still a difference in the patterns of temporal GM, but not WM, volume changes between the lithium- and VPA-treated groups with BD (p for interaction=0.02).
Lithium-Induced GM Volume Change and Clinical Measures
There was an overall improvement in HDRS scores over time for all patients with BD (z=−4.02, p<0.001). There was no significant difference in the rate of improvement, as assessed by decreases in HDRS scores, between lithium- and VPA-treated patients with BD (p for interaction=0.08) controlling for baseline HDRS scores. Changes in YMRS scores over time were not significant (z=0.05, p=0.96) and the rate of changes in YMRS scores did not differ between lithium- and VPA-treated patients with BD (p for interaction=0.77).
Improvement in depressive symptoms was associated with the rate of GM volume increases in lithium-treated patients with BD (n=13, Spearman ρ=−0.59, p=0.03), but not in the VPA-treated patients with BD (n=9, Spearman ρ=0.44, p=0.23).
DISCUSSION
In this study, lithium's effect on GM volume changes was first tested in mood-stabilizing and antipsychotic medications-naive patients with BD relative to VPA-treated patients with BD and control subjects. Lithium-induced GM volume increases, which reached peak levels after 10–12 weeks of treatment, and were sustained over 16 weeks during ongoing treatment. These robust GM volume increases correlated with clinical improvements. This suggests that lithium's effects on GM volume may be associated with therapeutic efficacy. Interestingly, however, GM volume increases were not observed in VPA-treated patients with BD although there was a clinical improvement similar to that in lithium-treated patients with BD. This suggests that lithium-induced GM changes are not likely to be epiphenomena of symptom improvement. This finding is consistent with hypothesized lithium-induced neurotrophic changes (Manji et al, 1999), which may be related to neuronal regeneration or axonal/dendritic sprouting (Moore et al, 2000; Moore et al, 2009).
The observed relationship between symptom abatement and GM volume increases suggests that lithium's effects on GM volume may be associated with therapeutic efficacy (Lagace and Eisch, 2005). The current findings may have implications for developing new treatment strategies for patients with BD. Considering that GM deficits were associated with clinical severity in BD (Lyoo et al, 2006), drugs that target GM volume increases may work as effectively as lithium in treating patients with BD without lithium-related side effects. Biomarkers for the neurotrophic system, such as genetic polymorphism in brain-derived neurotrophic factors, may be studied as potential predictors of lithium response (Martinowich et al, 2007).
Patients with BD have been reported to have a higher risk for dementia (Kessing and Nilsson, 2003). This increased risk seems to be reduced with continuous lithium, but not anticonvulsant, treatment (Kessing et al, 2008). This protective effect of lithium against dementia development may be associated with the current finding of sustained increases in GM volume with lithium treatment (Wada et al, 2005).
The maximum lithium-induced GM volume increase (approximately 2.56%, equivalent to 17.6 cm3) in this study is comparable in magnitude to the GM volume changes in a previous 4-week longitudinal study in BD (Moore et al, 2000; Moore et al, 2009). The current effect size for GM volume increase is also similar to that of brain structural changes caused by psychotropic medications in patients with other psychiatric disorders (Gilbert et al, 2000; Scherk and Falkai, 2006). ICV, in contrast, did not change over time in this study. This is consistent with a prior study that examined the total cerebral volume changes after long-term lithium treatment in patients with BD (Yücel et al, 2007).
GM volume increases in lithium-treated patients with BD could theoretically arise from osmotic changes (Phatak et al, 2006). However, metabolite T2-relaxation changes, which could reflect GM edematous changes, were not different between treatment groups over time in the same BD cohort (Friedman et al, 2004). The current findings are, therefore, unlikely to be confounded by osmotic effects of lithium. In this context, our finding of sustained GM volume increases in the lithium-treated patients with BD is most likely to reflect lithium-induced neurotrophic changes. This conclusion is also supported by preclinical and clinical studies (Coyle and Duman, 2003; Chuang and Manji, 2007).
Although clinical improvement in VPA-treated patients with BD was comparable to that of lithium-treated ones, VPA treatment was not associated with either GM or WM changes. Because similar neurotrophic mechanisms have been suggested to mediate the effects of lithium and VPA in preclinical studies (Coyle and Manji, 2002; Williams et al, 2002; Einat et al, 2003; Chen et al, 1999b; Chen et al, 1999a), this observation was somewhat unexpected. These results suggest that lithium and VPA may potentially have different, to some extent, mechanisms of action in the human brain.
Several brain imaging studies have reported that lithium and VPA cause different functional and neurochemical changes in the brain of patients with BD (Silverstone et al, 2003) as well as in healthy subjects (Bell et al, 2005). Cerebral levels of n-acetyl aspartate (NAA), a putative neuronal marker, increased in lithium-treated patients with BD but not in VPA-treated patients with BD (Silverstone et al, 2003). In our previous longitudinal MRS study in the same cohort, lithium, but not VPA, was associated with changes in cerebral levels of GM Glx (glutamate+glutamine) and myo-inositol (Friedman et al, 2004). This also indicates potential differences in the underlying mechanisms and modulatory consequences between the two drugs. The possibility of different mechanisms of action for lithium and VPA has also been raised by some preclinical studies (Gurvich and Klein, 2002; Hennion et al, 2002; Jorda et al, 2004; Li et al, 2002). It is also possible that VPA may affect regional cortical or subcortical, not overall, brain structures.
However, small sample size and relatively shorter mean treatment duration for the VPA group may contribute to the risk of type II error for the results of the VPA group. Difference in sex composition between groups may also be another confounding factor although sex and group interaction effect on the GM volume changes was not found.
Further studies with larger sample size, longer treatment duration, and balanced sample characteristics are necessary to confirm whether VPA treatment is associated with GM volume changes reflecting a potential neuroplastic effect.
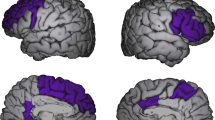
Considering the relatively small effect size of GM change of 2.56%, it could not be ruled out that changes in GM volumes in this study may potentially be driven by those in particular brain regions, for example, the prefrontal cortex where bipolar subjects have been affected (Kempton et al, 2008; Lyoo et al, 2006; Drevets et al, 1997; Moore et al, 2009), rather than the whole brain.
Healthy comparison subjects were examined twice, at baseline and approximately 9.3 weeks after baseline scans, whereas patients underwent MRI scanning up to 4 times. Further studies with more balanced data with larger sample size would be necessary for more robust results although this schedule for comparison scans allowed us to evaluate the stability of global GM volume measurements over time and our statistical model permits the different number of data points per subjects.
Given reports that antipsychotic and mood-stabilizing medications alter brain structures (Phillips et al, 2008), the fact that our patients with BD had never been treated with these medications, and were medication-free for at least 2 months before the scanning, provides an advantage over other studies where these important confounders were not controlled or reported (Phillips et al, 2008).
To summarize, this longitudinal imaging study of a medication-free BD cohort, naive to mood-stabilizing or antipsychotic medications, suggests that lithium treatment in patients with BD induce sustained increases in GM volume and that this effect may mediate the long-term efficacy of lithium. In contrast, changes in global brain GM volumes were not evident in VPA-treated patients with BD, suggesting a potential difference in the underlying mechanism of action for these drugs. Previous findings suggest that lithium's effect on GM volume changes would be most predominant in the ventromedial prefrontal cortical regions (Moore et al, 2009). Future studies that provide improved regional specificity particularly in the ventromedial prefrontal cortical regions in larger samples are needed to evaluate neural and biochemical differences, as well as commonalities, between these mood-stabilizing agents.
References
Ananth H, Popescu I, Critchley HD, Good CD, Frackowiak RS, Dolan RJ (2002). Cortical and subcortical gray matter abnormalities in schizophrenia determined through structural magnetic resonance imaging with optimized volumetric voxel-based morphometry. Am J Psychiatry 159: 1497–1505.
Ashburner J, Csernansky JG, Davatzikos C, Fox NC, Frisoni GB, Thompson PM (2003). Computer-assisted imaging to assess brain structure in healthy and diseased brains. Lancet Neurol 2: 79–88.
Ashburner J, Friston KJ (2001). Why voxel-based morphometry should be used. Neuroimage 14: 1238–1243.
Bearden CE, Thompson PM, Dalwani M, Hayashi KM, Lee AD, Nicoletti M et al (2007). Greater cortical gray matter density in lithium-treated patients with bipolar disorder. Biol Psychiatry 62: 7–16.
Bell EC, Willson MC, Wilman AH, Dave S, Silverstone PH (2005). Differential effects of chronic lithium and valproate on brain activation in healthy volunteers. Hum Psychopharmacol 20: 415–424.
Chard DT, Parker GJ, Griffin CM, Thompson AJ, Miller DH (2002). The reproducibility and sensitivity of brain tissue volume measurements derived from an SPM-based segmentation methodology. J Magn Reson Imaging 15: 259–267.
Chen G, Huang LD, Jiang YM, Manji HK (1999a). The mood-stabilizing agent valproate inhibits the activity of glycogen synthase kinase-3. J Neurochem 72: 1327–1330.
Chen G, Zeng WZ, Yuan PX, Huang LD, Jiang YM, Zhao ZH et al (1999b). The mood-stabilizing agents lithium and valproate robustly increase the levels of the neuroprotective protein bcl-2 in the CNS. J Neurochem 72: 879–882.
Chuang DM, Manji HK (2007). In search of the Holy Grail for the treatment of neurodegenerative disorders: has a simple cation been overlooked? Biol Psychiatry 62: 4–6.
Coyle JT, Duman RS (2003). Finding the intracellular signaling pathways affected by mood disorder treatments. Neuron 38: 157–160.
Coyle JT, Manji HK (2002). Getting balance: drugs for bipolar disorder share target. Nat Med 8: 557–558.
Dager SR, Friedman SD, Parow A, Demopulos C, Stoll AL, Lyoo IK et al (2004). Brain metabolic alterations in medication-free patients with bipolar disorder. Arch Gen Psychiatry 61: 450–458.
Drevets WC, Price JL, Simpson Jr JR, Todd RD, Reich T, Vannier M et al (1997). Subgenual prefrontal cortex abnormalities in mood disorders. Nature 386: 824–827.
Einat H, Yuan P, Gould TD, Li J, Du J, Zhang L et al (2003). The role of the extracellular signal-regulated kinase signaling pathway in mood modulation. J Neurosci 23: 7311–7316.
Friedman SD, Dager SR, Parow A, Hirashima F, Demopulos C, Stoll AL et al (2004). Lithium and valproic acid treatment effects on brain chemistry in bipolar disorder. Biol Psychiatry 56: 340–348.
Gilbert AR, Moore GJ, Keshavan MS, Paulson LA, Narula V, Mac Master FP et al (2000). Decrease in thalamic volumes of pediatric patients with obsessive-compulsive disorder who are taking paroxetine. Arch Gen Psychiatry 57: 449–456.
Gueorguieva R, Krystal JH (2004). Move over ANOVA: progress in analyzing repeated-measures data and its reflection in papers published in the Archives of General Psychiatry. Arch Gen Psychiatry 61: 310–317.
Gurvich N, Klein PS (2002). Lithium and valproic acid: parallels and contrasts in diverse signaling contexts. Pharmacol Ther 96: 45–66.
Hamilton M (1960). A rating scale for depression. J Neurol Neurosurg Psychiatry 23: 56–62.
Hennen J (2003). Statistical methods for longitudinal research on bipolar disorders. Bipolar Disord 5: 156–168.
Hennion JP, el-Masri MA, Huff MO, el-Mailakh RS (2002). Evaluation of neuroprotection by lithium and valproic acid against ouabain-induced cell damage. Bipolar Disord 4: 201–206.
Jorda EG, Verdaguer E, Morano A, Jimenez A, Canudas AM, Camins A et al (2004). Lithium prevents colchicine-induced apoptosis in rat cerebellar granule neurons. Bipolar Disord 6: 144–149.
Keller A, Castellanos FX, Vaituzis AC, Jeffries NO, Giedd JN, Rapoport JL (2003). Progressive loss of cerebellar volume in childhood-onset schizophrenia. Am J Psychiatry 160: 128–133.
Kempton MJ, Geddes JR, Ettinger U, Williams SC, Grasby PM (2008). Meta-analysis, database, and meta-regression of 98 structural imaging studies in bipolar disorder. Arch Gen Psychiatry 65: 1017–1032.
Kessing LV, Nilsson FM (2003). Increased risk of developing dementia in patients with major affective disorders compared to patients with other medical illnesses. J Affect Disord 73: 261–269.
Kessing LV, Sondergard L, Forman JL, Andersen PK (2008). Lithium treatment and risk of dementia. Arch Gen Psychiatry 65: 1331–1335.
Lagace DC, Eisch AJ (2005). Mood-stabilizing drugs: are their neuroprotective aspects clinically relevant? Psychiatr Clin North Am 28: 399–414.
Li X, Ketter TA, Frye MA (2002). Synaptic, intracellular, and neuroprotective mechanisms of anticonvulsants: are they relevant for the treatment and course of bipolar disorders? J Affect Disord 69: 1–14.
Lyoo IK, Sung YH, Dager SR, Friedman SD, Lee JY, Kim SJ et al (2006). Regional cerebral cortical thinning in bipolar disorder. Bipolar Disord 8: 65–74.
Manji HK, Moore GJ, Chen G (1999). Lithium at 50: have the neuroprotective effects of this unique cation been overlooked? Biol Psychiatry 46: 929–940.
Martinowich K, Manji H, Lu B (2007). New insights into BDNF function in depression and anxiety. Nat Neurosci 10: 1089–1093.
Moore GJ, Bebchuk JM, Wilds IB, Chen G, Manji HK (2000). Lithium-induced increase in human brain grey matter. Lancet 356: 1241–1242.
Moore GJ, Cortese BM, Glitz DA, Zajac-Benitez C, Quiroz JA, Uhde TW et al (2009). A longitudinal study of the effects of lithium treatment on prefrontal gray matter volume in treatment-responsive bipolar disorder patients. J Clin Psychiatry 70: 699–705.
Phatak P, Shaldivin A, King LS, Shapiro P, Regenold WT (2006). Lithium and inositol: effects on brain water homeostasis in the rat. Psychopharmacology (Berl) 186: 41–47.
Phillips ML, Travis MJ, Fagiolini A, Kupfer DJ (2008). Medication effects in neuroimaging studies of bipolar disorder. Am J Psychiatry 165: 313–320.
Rajkowska G (2000). Postmortem studies in mood disorders indicate altered numbers of neurons and glial cells. Biol Psychiatry 48: 766–777.
Sassi RB, Nicoletti M, Brambilla P, Mallinger AG, Frank E, Kupfer DJ et al (2002). Increased gray matter volume in lithium-treated bipolar disorder patients. Neurosci Lett 329: 243–245.
Scherk H, Falkai P (2006). Effects of antipsychotics on brain structure. Curr Opin Psychiatry 19: 145–150.
Schou M (1997). Forty years of lithium treatment. Arch Gen Psychiatry 54: 9–13.
Silverstone PH, Wu RH, O'Donnell T, Ulrich M, Asghar SJ, Hanstock CC (2003). Chronic treatment with lithium, but not sodium valproate, increases cortical N-acetyl-aspartate concentrations in euthymic bipolar patients. Int Clin Psychopharmacol 18: 73–79.
Wada A, Yokoo H, Yanagita T, Kobayashi H (2005). Lithium: potential therapeutics against acute brain injuries and chronic neurodegenerative diseases. J Pharmacol Sci 99: 307–321.
Williams RS, Cheng L, Mudge AW, Harwood AJ (2002). A common mechanism of action for three mood-stabilizing drugs. Nature 417: 292–295.
Young RC, Biggs JT, Ziegler VE, Meyer DA (1978). A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry 133: 429–435.
Yücel K, McKinnon MC, Taylor VH, MacDonald K, Alda M, Young LT et al (2007). Bilateral hippocampal volume increases after long-term lithium treatment in patients with bipolar disorder: a longitudinal MRI study. Psychopharmacology (Berl) 195: 357–367.
Acknowledgements
This study received financial support from the National Alliance for Schizophrenia and Depression (Independent Investigator Awards, Dr Lyoo and Dr Renshaw), the National Institute of Mental Health (RO1 MH58681, Dr Renshaw), the Poitras Foundation (Dr Renshaw), the Korean Ministry of Science and Technology (2009K001272, Dr Lyoo), and the National Research Foundation of Korea (2009-0074584, Dr Kim and 2009-0066915, Dr Yoon). We thank all study participants; the whole international collaborative team, including James Anderson, Sujin Bae, Carolyn Bea, Chris Budech, Marie Domsalla, Denise Echelard, Charlotte Haws, Jaeuk Hwang, Kyehyen Kim, and Gerald Ortiz for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Lyoo has received research support from Eli Lilly, AstraZeneca, GSK, and Lundbeck. Dr Dunner has been a consultant for Eli Lilly, Pfizer, GSK, Wyeth, Bristol-Myers Squibb, Forest, Roche Diagnostics, Cypress, Corcept, Janssen, Novartis, Shire, Somerset, Cyberonics, Otsuka, Jazz Pharma and Healthcare Technology Systems; received research support from Eli Lilly, Pfizer, GSK, Wyeth, Bristol-Myers Squibb, Forest, Janssen, Cyberonics, and Novartis; and has been on the speaker's bureau of Eli Lilly, Pfizer, GSK, Wyeth, Bristol-Myers Squibb, and Organon. Dr Renshaw is a consultant for Novartis, Roche, and Kyowa Hakko, and has received research support from Roche, GSK, and Eli Lilly. Dr Dager, Dr Kim, Dr Yoon, and Dr Friedman have no conflict of interest to declare.
Additional information
Supplementary Information accompanies the paper on the Neuropsychopharmacology website
Supplementary information
PowerPoint slides
Rights and permissions
About this article
Cite this article
Lyoo, I., Dager, S., Kim, J. et al. Lithium-Induced Gray Matter Volume Increase As a Neural Correlate of Treatment Response in Bipolar Disorder: A Longitudinal Brain Imaging Study. Neuropsychopharmacol 35, 1743–1750 (2010). https://doi.org/10.1038/npp.2010.41
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2010.41
Keywords
This article is cited by
-
Autophagy and autophagy signaling in Epilepsy: possible role of autophagy activator
Molecular Medicine (2023)
-
Mania-related effects on structural brain changes in bipolar disorder – a narrative review of the evidence
Molecular Psychiatry (2023)
-
Lithium as a Neuroprotective Agent for Bipolar Disorder: An Overview
Cellular and Molecular Neurobiology (2022)
-
Endothelial dysfunction in neuroprogressive disorders—causes and suggested treatments
BMC Medicine (2020)
-
Integrative analysis of lithium treatment associated effects on brain structure and peripheral gene expression reveals novel molecular insights into mechanism of action
Translational Psychiatry (2020)