Abstract
Sexual dysfunction is a major contributor to treatment discontinuation and nonadherence among patients treated with selective serotonin reuptake inhibitors (SSRIs). The mechanisms by which depressive symptoms in general, as well as SSRI exposure in particular, may worsen sexual function are not known. We examined genetic polymorphisms, including those of the serotonin and glutamate systems, for association with erectile dysfunction, anorgasmia, and decreased libido during citalopram treatment. Clinical data were drawn from a nested case–control cohort derived from the STAR*D study, a multicenter, prospective, effectiveness trial in outpatients with nonpsychotic major depressive disorder (MDD). Self-reports of erectile dysfunction, decreased libido, or difficulty achieving orgasm based on the Patient-Rated Inventory of Side Effects were examined among Caucasian subjects (n=1473) for whom DNA and adverse effect measures were available, and who were treated openly with citalopram for up to 14 weeks. Of 1473 participants, 799 (54%) reported decreased libido; 525 (36%) reported difficulty achieving orgasm. Of 574 men, 211 (37%) reported erectile dysfunction. Using a set-based test for association, single nucleotide polymorphisms in glutamatergic genes were associated with decreased libido (GRIA3; GRIK2), difficulty achieving orgasm (GRIA1), and difficulty achieving erection (GRIN3A) (experiment-wide permuted p<0.05 for each). Evidence of association persisted after adjustment for baseline clinical and sociodemographic differences. Likewise, evidence of association was similar when the cohort was limited to those who did not report a given adverse event at the first post-baseline visit (ie, those whose adverse events were known to be treatment emergent). These hypothesis-generating analyses suggest the potential for glutamatergic treatment targets for sexual dysfunction during major depressive episodes.
Similar content being viewed by others
INTRODUCTION
Sexual dysfunction is common among individuals with major depressive episodes and may be triggered or exacerbated by treatment with the selective serotonin reuptake inhibitors (SSRIs), with a prevalence of up to 50–70% in some studies when sexual functioning is specifically assessed (Angst et al, 2002; Fava and Rankin, 2002; Montejo et al, 2001). Common symptoms include decreased libido, difficulty in arousal, and delayed or absent orgasm (Angst et al, 2002). Beyond their impact on quality of life, these effects frequently lead to medication intolerance and discontinuation (Bull et al, 2002; Montejo et al, 2001). Indeed, sexual dysfunction may be the most clinically significant SSRI-related adverse event among individuals age 18–40 (Bishop et al, 2006; Clayton, 2001).
The mechanism by which depression itself, or treatments such as SSRIs, may induce sexual dysfunction is poorly understood. Because the proximal site of action of SSRIs is believed to be the serotonin transporter, some sexual effects have been presumed to relate to serotonergic neurotransmission (Murray, 1998). However, the neuroanatomy of sexual functioning in general offers some additional direction about which neurotransmitter systems might be most likely to mediate these symptoms. Specifically, other monoamines, as well as glutamate, appear to have a function in male and female sexual behavior (Clayton, 2003).
Because of their potential importance in antidepressant efficacy, common variations in serotonergic, glutamatergic, dopaminergic, and other pathways implicated in antidepressant mechanism of action have been examined recently in a genetic association study in the STAR*D cohort (McMahon et al, 2006; Paddock et al, 2007). To attempt to clarify the mechanism by which depression and its treatments may contribute to sexual dysfunction, we performed a hypothesis-generating secondary analysis in which we examined these genes for association with sexual dysfunction.
METHODS
Clinical Methods
In the STAR*D trial, all patients were initially treated with the SSRI citalopram. Those who were intolerant of citalopram, or who did not achieve remission, could then be randomized to a next-step treatment option. The methods of the STAR*D study are described in detail elsewhere (Fava et al, 2003; Rush et al, 2004; Trivedi et al, 2006b) and are summarized below.
Study Organization
The STAR*D study, overseen by 14 regional centers (RCs), provided treatment at 41 clinical sites (18 primary care and 23 psychiatric care settings) across the United States.
Research outcomes were collected by telephone interviews conducted by a small team of trained research outcome assessors (ROAs) masked to treatment. ROAs received extensive training in the administration of efficacy measures, with interrater reliability assessed periodically.
Study Population
The STAR*D clinical cohort consisted of 4041 subjects, of whom 1953 provided blood samples for extraction of DNA and 1910 were genotyped, including 1499 (78.5%) Caucasians. This report presents data from the 1473 Caucasians from this pool who returned for at least one follow-up visit (ie, a modified intent-to-treat cohort). As the study was designed to represent real-world clinical practice, only individuals who sought treatment at the clinical sites were recruited, and advertising was not permitted. Participants were informed of all risks, benefits, and adverse events associated with each study treatment and they provided written informed consent before study entry at each level, as well as for the genetic study. Participants could decline participation in the genetic protocol, which was initiated about 12 months after the clinical study initiation. The study protocol was approved by institutional review boards at all participating RCs, the National Coordinating Center, and the Data Coordinating Center. The study was overseen by an NIMH DSMB.
Participants met broadly inclusive and minimal exclusive criteria to enroll a representative sample. Male and female outpatients, age 18–75, with a DSM-IV diagnosis of nonpsychotic major depressive disorder (MDD), a baseline score ⩾14 on the 17-item Hamilton Rating Scale for Depression (HRSD) (Hamilton, 1960) by the clinical research coordinator (CRC), and for whom the treating clinician had determined that outpatient antidepressant treatment was safe and appropriate were enrolled. Exclusion criteria included a well-documented history of nonresponse or intolerability in the current major depressive episode to adequate doses (Fava, 2003) of one or more medications used in the first two treatment steps; lifetime diagnosis of MDD with psychotic features, schizophrenia, schizoaffective disorder, or bipolar disorder; a current primary diagnosis of eating disorder or obsessive-compulsive disorder; presence of severe, unstable concurrent psychiatric conditions likely to require hospitalization within 6 months (eg severe alcohol dependence with recent detoxification admissions); presence of concurrent medical or psychiatric conditions or concomitant medications that contraindicate a protocol treatment; and pregnancy or intent to conceive within the 9 months subsequent to study entry.
Research Outcome Assessments
The CRC at each study site completed the HRSD17 at baseline to determine eligibility, reviewed other inclusion/exclusion criteria, and completed the 16-item Quick Inventory of Depressive Symptomatology (QIDS-C16) (Rush et al, 2000, 2006a, 2003; Trivedi et al, 2004) at each treatment visit—a clinician-rated scale that assesses nine diagnostic symptoms/domains of MDD. The QIDS-C16 was used to guide treatment implementation and dose adjustment (Rush et al, 2006b; Trivedi et al, 2006a), and was selected as the primary outcome measure for STAR*D genetics reports. The CRC also completed the 14-item Cumulative Illness Rating Scale (Linn et al, 1968; Miller et al, 1992) that quantifies the severity/morbidity of general medical conditions relevant to different organ systems. Each of the 14 illness categories was scored 0 (no problem) to 4 (extremely severe/immediate treatment required/end organ failure/severe impairment in function). The present analysis examined total severity summed over all categories except psychiatry.
The ROA conducted a telephone interview with study participants within 72 h of the baseline and subsequent visits to complete the baseline blinded HRSD17 and the 30-item Inventory of Depressive Symptomatology, Clinician-Rated (IDS-C30) (Rush et al, 1996).
Individual adverse events were identified at each post-baseline clinical visit using the Patient-Rated Inventory of Side Effects (PRISE) (Rush et al, 2004), a nine-item patient-rated assessment of presence or absence of side effects in domains including gastrointestinal, cardiac, skin, nervous system, sensory organs, genital/urinary, sleep, sexual functioning, and other. In each domain, multiple symptoms may be endorsed. No standardized assessment of patient adherence to treatment was collected.
Intervention
Details of the STAR*D measurement-based care approach have been described elsewhere (Trivedi et al, 2006b). Following citalopram treatment at doses up to 60 mg per day for up to 14 weeks, participants who did not achieve remission (QIDS-C16⩽5) and/or who could not tolerate citalopram were encouraged to proceed to next-step treatments. Participants could discontinue citalopram and proceed to next-step treatment at any point in the event of intolerable side effects requiring change in medication, inability to increase to an optimal dose because of side effects or patient preference, or presence of significant depressive symptoms (defined as QIDS-C16 score ⩾9) after 9 weeks at maximum tolerated dose.
Concomitant treatments for current general medical conditions, for associated symptoms of depression including insomnia, anxiety, and agitation, and for antidepressant-associated side effects were permitted based on clinical judgment. However, stimulants, anticonvulsants, antipsychotics, alprazolam, nonprotocol antidepressants other than trazodone ⩽200 mg at bedtime for insomnia, and psychotherapies targeted at depressive symptoms were not permitted (Trivedi et al, 2006b).
Genotyping methods
The process for selecting candidate genes based on evidence of involvement in antidepressant mechanism of action, and selection of single nucleotide polymorphisms (SNPs) to capture common variation, has been described elsewhere (McMahon et al, 2006). In brief, based on expert consensus, genes were selected in serotonergic (n=20), glutamatergic (n=16), dopaminergic (n=3), adrenergic (n=4), and neurotrophic (n=4) systems, as well as other genes implicated in antidepressant mechanism of action (n=21). The full list of genes is available in Table 2 of McMahon et al (2006). Genotyping was performed using the Illumina BeadArray platform and genotypic data were cleaned using methods previously described.
Analytic methods
Decreased libido, difficulty achieving orgasm, and difficulty with erections are three correlated but nonidentical phenomena assessed by the PRISE. Therefore, three sets of primary analyses were performed examining each of these individually. Each symptom of sexual dysfunction was defined as report of that category of adverse event on the PRISE on at least one post-baseline visit. For follow-up analyses, we also defined ‘emergent’ symptoms (putative adverse events) as those that were absent at the initial post-baseline (ie the week 2) visit, but present on at least one subsequent visit.
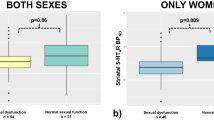
Primary analysis pooled men and women, which would maximize power to detect associations provided effects were similar within these two groups. For SNPs with nominal p<0.05 in any genes identified in the primary test of association described below, follow-up analysis examined heterogeneity between odds ratios within strata (men and women) using the Breslow–Day test. This approach was guided by the recommendations of a recent structured review of methodological constraints in detecting sex-specific effects (Patsopoulos et al, 2007).
Clinical analyses
Degree of overlap between the three categories of sexual symptoms was examined using cross-tabulation and Spearman's ρ. Individuals with and without each sexual symptom were compared on baseline sociodemographic and clinical features using χ2-test or unpaired t-test. Multiple logistic regression was then used to determine which of these to include in the multivariate models described below; any feature with p<0.05 in the multivariate regression model was included as a covariate in the association analyses. Symptom groups were also compared in terms of maximal citalopram dose, amount of decrease in QIDS-C16 from baseline to end point, achieving remission (QIDS-C16⩽5) at end point, number of study visits, medication tolerability (using an algorithm previously described), and presence or absence of sedative/hypnotic co-treatment.
Gene-based analyses
As suggested by Neale and Sham (2004) for analysis of association studies, we considered the unit of analysis in this study to be the single gene rather than SNP; that is, we were screening for association of a gene (understood as a SNP or set of SNPs) with the phenotype of interest using a set-based test (here, the ‘set’ in question includes the SNPs in a given gene). The set-based test provides a simple means of accounting for linkage disequilibrium between SNPs within a gene, and also will generally have greater power to detect associations if multiple SNPs within a gene are associated with the phenotype of interest. In brief, this test, analogous to that proposed by Ott and Hoh (2003), computes the test statistic (χ2 for dichotomous outcomes) for each individual SNP within a gene, then calculates the average test statistic for the best single SNP per region, for the best two SNPs per region, and for the best three SNPs per region. The significance of these set statistics is then estimat by permuting (swapping) individual identifiers to generate a ‘new’ data set. This method allows an estimate of how often, if no ‘true’ association exists, a set statistic this large or larger would be observed by chance. It allows a determination of gene-wise significance, allowing for correlation between SNPs and tests, while controlling type 1 error at the single-gene level.
Primary analysis screened for association using the set-based test as implemented in PLINK (Purcell et al, 2007) for each gene. Significance of SNP combinations including between one and three SNPs was estimated, using 20 000 permutations. To further control type 1 error, the same approach to permutation was also used to account for all tests in all genes (experiment-wise p-values)—here, how often would test statistics this extreme, or more extreme, be observed in the ‘permuted’ data sets. Where experiment-wise p<0.05 for a gene was observed, all single SNP associations in that gene were then examined. For the set-based tests, where pairs of SNPs were in linkage disequilibrium with r2>0.8, only one of the two, selected arbitrarily, was included in analysis, but all SNPs in a gene were included when follow-up analyses were conducted. Epistatic effects were not examined due to limited power to detect such associations.
To address the potential for confounding by associations with baseline clinical features or longitudinal outcomes, we also performed a series of planned follow-up analyses for any SNPs in genes with nominal evidence of association. First, we repeated single SNP association analyses with adjustment for individual baseline clinical and sociodemographic features, or longitudinal outcomes that were associated with a given sexual symptom. Efficacy and tolerability can be strongly correlated in clinical trials and can therefore confound observed associations. For example, individuals who derive less benefit from an intervention might receive greater dosing or longer trials, leading to greater emergence of dose-dependent symptoms or adverse events. A particular concern was confounding by symptomatic worsening, which led us to examine in a post hoc analysis SNPs with nominal evidence of association. In Cox regression, with emergence of a sexual symptom as the event of interest, we examined models including both genotype and visit-to-visit symptom change, the latter as a time-dependent covariate.
We further addressed the possibility of population admixture as previously reported, generating probabilities of ethnic group membership using the program STRUCTURE (McMahon et al, 2006; Pritchard et al, 2000) to cluster individuals based on ancestry-informative markers. Single SNP analyses were repeated with adjustment for factor loadings assuming a three-population (k=3) solution, previously found to represent the optimal number of populations in this cohort (McMahon et al, 2006).
RESULTS
Comparisons of the genetic cohort to the total clinical cohort in terms of baseline sociodemographic features have been presented elsewhere (McMahon et al, 2006). Of 1910 genotyped subjects, we excluded 36 subjects who failed to return for at least one post-baseline visit and therefore did not provide adverse event data, yielding a ‘modified intent-to-treat’ sample; a further 401 non-Caucasian subjects were excluded from primary analyses because allele frequencies for many of the genes in question differ across populations, resulting in 1473 evaluable Caucasian subjects.
Sexual Symptoms and Clinical Associations
Of 1473 participants, 799 (54%) reported decrease in libido, and 525 (36%) reported difficulty achieving orgasm; correlation between them was modest (Spearman's ρ=0.33). In all, 400 of 1473 (27%) reported both symptoms, and 524 of 1473 (36%) reported one symptom. Of 574 men, 211 (37%) reported erectile dysfunction (ED); Spearman's ρ=0.32 between ED and libido and 0.44 between ED and orgasm. Of 574, 133 (23%) reported two of three sexual symptoms, and 118 (21%) reported. Table 1 compares those who did or did not report each of the three sexual symptoms in terms of baseline clinical and sociodemographic features. For ED, greater age, duration of illness, severity of depression at study entry, severity of general medical comorbidity, and presence of an anxiety disorder were associated with greater risk. For decreased libido, earlier onset of illness, greater severity of depression, being married, and being male were associated with greater risk. For difficulty with orgasm, younger age and earlier age at onset, greater severity of general medical comorbidity, as well as being married, male, and treated in a specialty rather than primary care setting, were associated with greater risk (features of longitudinal course, including number of follow-up visits, symptomatic improvement or remission, medication tolerability, and use of concomitant sedative/hypnotic medication are similarly compared in Supplementary Table 1).
Genetic Associations
Erectile dysfunction in men
Supplementary Table 2 shows results from the set-based test for association between the included genes and presence of ED. GRIN3A was associated with difficulty achieving erection (experiment-wise permuted p<0.05 for rs1323427, rs1323423, and rs2050641) and met the threshold for further examination. Among serotonergic genes, greatest evidence of association was observed in HTR2A (rs6314, rs2770296, rs594242; gene-wise p=0.05, experiment-wise p=0.95). Table 2 includes all single SNP allelic results with nominal p<0.05 for association. Odds ratios for ED ranged from 1.51 to 1.56 for the three SNPs with greatest evidence of association, indicating overall risk ∼50–60% greater among individuals carrying these individual risk alleles. To address the possibility that the association was confounded by sociodemographic or clinical features, we repeated the single SNP analyses with adjustment for any variables significant in univariate analyses, yielding no evidence of confounding in terms of change in odds ratios (Table 2). Likewise, to examine the possibility of confounding by efficacy (eg patients with poorer response receiving greater citalopram doses), we repeated single SNP analyses with adjustment for maximum citalopram dose, again with little change in strength of association (Supplementary Table 5). In particular, incorporating a term for symptom change vs prior visit did not change any observed hazard ratios by greater than 10%, suggesting these associations are not confounded by symptom change (results not shown). Most, but not all, associations remained significant (p<0.05) following adjustment for population substructure (Table 4). Finally, when the cohort was limited to those individuals without ED at the first post-baseline visit (N=446), 87 (20%) reported new onset of ED (Table 2). Effect sizes, in terms of odds ratios, were similar to those observed in the full cohort.
Changes in libido
We examined changes in libido in a similar manner. Two genes, GRIA3 (rs2285127, rs2269551, rs550640) and GRIK2 (rs9404130, rs2518302, rs513216) showed experiment-wise evidence of association (permuted p<0.05; Supplementary Table 3). Single SNP tests are shown in Table 3. For the three top SNPs in GRIK2, risk of decreased libido was 30–40% greater among those with the risk allele, and for GRIA3, risk was 20–30% greater. No serotonergic genes were significantly associated with libido; the gene showing greatest evidence of association was SLC6A4 (rs7224199, rs2054847, rs2020942; gene-wise p=0.02, experiment-wise p=0.69). Once again, there was little change in odds ratios for association with decreased libido when analyses were adjusted for sociodemographic and clinical differences (Table 3), or features of longitudinal outcome (Supplementary Table 6). As above, in no case did adjustment for symptom change yield a change in hazard ratio of greater than 10% (results not shown). After adjustment for population substructure, most but not all SNPs remained significantly associated (Table 4). When the phenotype was restricted to those without the adverse event at the first post-baseline visit (N=937) who subsequently developed decrease in libido (272 of 937; 29%), effect sizes were similar to those observed in the cohort as a whole.
Difficulty with orgasm
One gene, GRIA1 (rs1994862, rs10515697, rs1864205), showed evidence of association with difficulty with orgasm (Supplementary Table 4). Among serotonergic genes, strongest association was again observed in the same SNPs in SLC6A4 (rs2054847, rs7224199, rs2020942; gene-wise p=0.003, experiment-wise p=0.162). Results from individual SNPs in this gene with nominal p<0.05 are given in Table 4. Overall, odds of difficulty with orgasm were ∼40–50% greater among those with the risk allele. Adjusting these association analyses for potential baseline (Table 4) or longitudinal (Supplementary Table 7) confounders yielded little change in odds ratios. Again, adjustment for symptom change did not change observed hazard ratios for single SNPs by 10% or greater (results not shown). The two top SNPs remained significantly associated with difficulty with orgasm after adjustment for ancestry-informative markers. Limiting the analysis to the subset without decreased orgasm at baseline (N=1153) also yielded similar results (Table 4).
DISCUSSION
This secondary analysis of data from a large-scale candidate gene study of antidepressant response found multiple genes of the glutamatergic system, but none from the serotonergic system, to be significantly associated with sexual dysfunction of three correlated but nonidentical types. Follow-up clinical analyses suggest that these associations are not confounded by clinical features that are independently associated with such symptoms, including general medical comorbidity, or by overall symptomatic worsening. This latter finding is notable in light of a prior STAR*D report that also identified association between glutamate genes and treatment-associated suicidality (Laje et al, 2007).
Although glutamate has not been studied as a mechanism of depression, or antidepressant-associated sexual dysfunction, rodent studies highlight its importance in sexual function. In males, the medial preoptic area (MPOA), which integrates and coordinates sexual behavior (Hull and Dominguez, 2006), receives glutamatergic input from the medial amygdala and bed nucleus of the stria terminalis, and in turn (acting through nitric oxide (NO)) increases dopamine release in the MPOA. Injecting dopamine antagonists will interfere with copulation among male rats, whereas agonists have the opposite (facilitating) effect (Dominguez and Hull, 2005). Treatment with glutamate agonists and antagonists has analogous effects (Dominguez et al, 2006, 2004).
The MPOA projects widely, including the paraventricular nucleus of the hypothalamus (PVN), which appears to mediate directly erection through oxytocinogenic neurons. Glutamate agonists induce erections when injected into the PVN; erections are blocked by injecting glutamate antagonists (Melis et al, 2000; Powell et al, 2003). Glutamate has also been implicated in animal models of female sexual behavior. For example, glutamate antagonists infused into the ventromedial hypothalamus increase lordosis among female rats (Georgescu and Pfaus, 2006), whereas glutamate agonists have the opposite effect.
Far less is known about the neurobiology underlying libido per se, which may be difficult to distinguish from sexual activity in animal models. Notably, however, at least one case report associates lamotrigine, which decreases glutamatergic neurotransmission, with spontaneous hypersexuality or improvement in sexual function or interest among epilepsy patients (Gil-Nagel et al, 2006; Grabowska-Grzyb et al, 2006).
In humans, a recent report using magnetic resonance spectroscopy demonstrated that citalopram administration increases a composite measure of glutamate and glutamine in vivo (Taylor et al, 2008). Indirect evidence in animal models or in vitro systems suggests that SSRIs may influence glutamatergic neurotransmission, though the mechanism is not known (Langman et al, 2006; Matrisciano et al, 2008; Shioda et al, 2004; Svenningsson et al, 2007). For example, an in vitro model of neurogenesis suggests synergy between SSRIs and glutamate receptor (mGluR2 and 3) agonists (Matrisciano et al, 2008).
To our knowledge, only one prior pharmacogenetic study examined SSRI-associated sexual dysfunction (Bishop et al, 2006); in that study of 89 outpatients, a noncoding polymorphism in the HTR2A gene (−1438GA; rs6311) was associated with sexual dysfunction in general, as well as difficulty with arousal. Although we did not directly genotype this polymorphism, for purposes of comparison we did examine rs1928040 in HTR2A which is reported to be in strong linkage disequilibrium with it (r2>0.8 in the International Haplotype Map Phase II data), and a two-SNP combination which is reported to be in perfect linkage disequilibrium with it (rs1928040, rs985933), but found no evidence of association either in the cohort as a whole, or among male or female cohorts (results not shown; nominal p>0.05 for all three sexual adverse effects). We likewise found no significant evidence of association on a gene-based test for association of HTR2A with any of these phenotypes (Supplementary Tables 1–3); although ED was nominally associated with some SNPs in HTR2A, these modest effects did not survive correction for multiple comparisons. We note that our phenotype differs from that previously examined because of the lack of baseline symptom assessment or sensitive measures of sexual function, so cannot exclude the possibility that a larger cohort or more detailed phenotyping might have detected a significant association. Alternatively, although modulation of postsynaptic 5HT2A may be clinically relevant to SSRI-mediated sexual dysfunction (Clayton and Montejo, 2006), there may simply not be a genetic basis for the observable pharmacodynamic variation.
A limitation of the present report is that no detailed and validated assessment of sexual function, such as the Changes in Sexual Functioning Questionnaire (Clayton et al, 1997), was used. Therefore, our sensitivity to sexual symptoms and ability to dissect individual components affected is limited. On the other hand, this would tend to bias our results toward the null, so it does not diminish confidence in the positive findings. In addition, details of medical comorbidity or their treatment are not available to us, although adjustment for summary measures of such comorbidity yields no evidence of confounding. Another caveat is that, because there is no PRISE completed at baseline, our findings do not necessarily indicate that these symptoms are treatment emergent. Rather, they may indicate risk for sexual dysfunction regardless of treatment. We nonetheless relied on this assessment as our primary phenotype because it allowed us to examine the largest possible cohort, we expected that most such reported symptoms would actually be treatment emergent, and we reasoned that any association detected, regardless of specificity, would be of interest. However, a secondary analysis examining only those symptoms clearly absent at initial post-baseline visit, and thus more likely to be truly treatment emergent, yielded similar results.
A further limitation is our inability to exclude fully the potential confounding effects of population stratification despite adjustment using ancestry-informative markers, and inability to exclude type I error in the absence of a replication cohort (Sullivan, 2007). Conversely, it is possible that pooling men and women obscured true sex-specific associations, resulting in type II error. We did not detect sex-specific effects for the genes showing main effects and therefore did not pursue within-sex analyses except for the SNP in HTR2A previously associated with sexual symptoms.
Finally, in the absence of a placebo or active comparator, we cannot address the specificity of the observed associations. The observed associations might indicate proneness to report sexual symptoms, regardless of treatment, or might be limited to SSRIs such as citalopram.
In sum, in this large-scale candidate gene-based study, we find preliminary evidence for association of glutamatergic but not serotonergic genes with sexual dysfunction among individuals with MDD treated with the SSRI citalopram. In all cases, the SNPs identified do not lie in known coding or regulatory regions. Still, these results suggest that glutamatergic strategies may merit further consideration for the management of SSRI-associated sexual dysfunction. By considering variation in glutamatergic genes, as well as clinical features associated with differential risk, it may be possible to identify individuals at greater risk for experiencing sexual dysfunction during depressive episodes.
References
Angst F, Stassen HH, Clayton PJ, Angst J (2002). Mortality of patients with mood disorders: follow-up over 34–38 years. J Affect Disord 68: 167–181.
Bishop JR, Moline J, Ellingrod VL, Schultz SK, Clayton AH (2006). Serotonin 2A-1438 G/A and G-protein Beta3 subunit C825T polymorphisms in patients with depression and SSRI-associated sexual side-effects. Neuropsychopharmacology 31: 2281–2288.
Bull SA, Hunkeler EM, Lee JY, Rowland CR, Williamson TE, Schwab JR et al (2002). Discontinuing or switching selective serotonin-reuptake inhibitors. Ann Pharmacother 36: 578–584.
Clayton AH (2001). Recognition and assessment of sexual dysfunction associated with depression. J Clin Psychiatry 62 (Suppl 3): 5–9.
Clayton AH (2003). Sexual function and dysfunction in women. Psychiatr Clin North Am 26: 673–682.
Clayton AH, McGarvey EL, Clavet GJ (1997). The Changes in Sexual Functioning Questionnaire (CSFQ): development, reliability, and validity. Psychopharmacol Bull 33: 731–745.
Clayton AH, Montejo AL (2006). Major depressive disorder, antidepressants, and sexual dysfunction. J Clin Psychiatry 67 (Suppl 6): 33–37.
Dominguez JM, Gil M, Hull EM (2006). Preoptic glutamate facilitates male sexual behavior. J Neurosci 26: 1699–1703.
Dominguez JM, Hull EM (2005). Dopamine, the medial preoptic area, and male sexual behavior. Physiol Behav 86: 356–368.
Dominguez JM, Muschamp JW, Schmich JM, Hull EM (2004). Nitric oxide mediates glutamate-evoked dopamine release in the medial preoptic area. Neuroscience 125: 203–210.
Fava M (2003). Diagnosis and definition of treatment-resistant depression. Biol Psychiatry 53: 649–659.
Fava M, Rankin M (2002). Sexual functioning and SSRIs. J Clin Psychiatry 63 (Suppl 5): 13–16; discussion 23–5.
Fava M, Rush AJ, Trivedi MH, Nierenberg AA, Thase ME, Sackeim HA et al (2003). Background and rationale for the sequenced treatment alternatives to relieve depression (STAR*D) study. Psychiatr Clin North Am 26: 457–494, x.
Georgescu M, Pfaus JG (2006). Role of glutamate receptors in the ventromedial hypothalamus in the regulation of female rat sexual behaviors. II. Behavioral effects of selective glutamate receptor antagonists AP-5, CNQX, and DNQX. Pharmacol Biochem Behav 83: 333–341.
Gil-Nagel A, Lopez-Munoz F, Serratosa JM, Moncada I, Garcia-Garcia P, Alamo C (2006). Effect of lamotrigine on sexual function in patients with epilepsy. Seizure 15: 142–149.
Grabowska-Grzyb A, Naganska E, Wolanczyk T (2006). Hypersexuality in two patients with epilepsy treated with lamotrigine. Epilepsy Behav 8: 663–665.
Hamilton M (1960). A rating scale for depression. J Neurol Neurosurg Psychiatry 23: 56–62.
Hull EM, Dominguez JM (2006). Getting his act together: roles of glutamate, nitric oxide, and dopamine in the medial preoptic area. Brain Res 1126: 66–75.
Laje G, Paddock S, Manji H, Rush AJ, Wilson AF, Charney D et al (2007). Genetic markers of suicidal ideation emerging during citalopram treatment of major depression. Am J Psychiatry 164: 1530–1538.
Langman NJ, Smith CG, Whitehead KJ (2006). Selective serotonin re-uptake inhibition attenuates evoked glutamate release in the dorsal horn of the anaesthetised rat in vivo. Pharmacol Res 53: 149–155.
Linn BS, Linn MW, Gurel L (1968). Cumulative Illness Rating Scale. J Am Geriatr Soc 16: 622–626.
Matrisciano F, Zusso M, Panaccione I, Turriziani B, Caruso A, Iacovelli L et al (2008). Synergism between fluoxetine and the mGlu2/3 receptor agonist, LY379268, in an in vitro model for antidepressant drug-induced neurogenesis. Neuropharmacology 54: 428–437.
McMahon FJ, Buervenich S, Charney D, Lipsky R, Rush AJ, Wilson AF et al (2006). Variation in the gene encoding the serotonin 2A receptor is associated with outcome of antidepressant treatment. Am J Hum Genet 78: 804–814.
Melis MR, Succu S, Spano MS, Argiolas A (2000). Effect of excitatory amino acid, dopamine, and oxytocin receptor antagonists on noncontact penile erections and paraventricular nitric oxide production in male rats. Behav Neurosci 114: 849–857.
Miller MD, Paradis CF, Houck PR, Mazumdar S, Stack JA, Rifai AH et al (1992). Rating chronic medical illness burden in geropsychiatric practice and research: application of the Cumulative Illness Rating Scale. Psychiatry Res 41: 237–248.
Montejo AL, Llorca G, Izquierdo JA, Rico-Villademoros F (2001). Incidence of sexual dysfunction associated with antidepressant agents: a prospective multicenter study of 1022 outpatients. Spanish Working Group for the Study of Psychotropic-Related Sexual Dysfunction. J Clin Psychiatry 62 (Suppl 3): 10–21.
Murray JB (1998). Physiological mechanisms of sexual dysfunction side effects associated with antidepressant medication. J Psychol 132: 407–416.
Neale BM, Sham PC (2004). The future of association studies: gene-based analysis and replication. Am J Hum Genet 75: 353–362.
Ott J, Hoh J (2003). Set association analysis of SNP case–control and microarray data. J Comput Biol 10: 569–574.
Paddock S, Laje G, Charney D, Rush AJ, Wilson AF, Sorant AJ et al (2007). Association of GRIK4 with outcome of antidepressant treatment in the STAR*D cohort. Am J Psychiatry 164: 1181–1188.
Patsopoulos NA, Tatsioni A, Ioannidis JP (2007). Claims of sex differences: an empirical assessment in genetic associations. JAMA 298: 880–893.
Powell WS, Dominguez JM, Hull EM (2003). An NMDA antagonist impairs copulation and the experience-induced enhancement of male sexual behavior in the rat. Behav Neurosci 117: 69–75.
Pritchard JK, Stephens M, Donnelly P (2000). Inference of population structure using multilocus genotype data. Genetics 155: 945–959.
Purcell S, Neale BM, Todd-Brown K, Thomas L, Ferreira MAR, Bender D et al (2007). PLINK: a toolset for whole genome association and population-based linkage analyses. Am J Hum Genet 81: 559–575.
Rush A, Carmody T, Reimitz P (2000). The Inventory of Depressive Symptomatology (IDS): Clinician (IDS-C) and Self-Report (IDS-SR) ratings of depressive symptoms. Int J Methods Psychiatr Res 9: 45–59.
Rush AJ, Bernstein IH, Trivedi MH, Carmody TJ, Wisniewski S, Mundt JC et al (2006a). An evaluation of the Quick Inventory of Depressive Symptomatology and the Hamilton Rating Scale for Depression: a Sequenced Treatment Alternatives to Relieve Depression trial report. Biol Psychiatry 59: 493–501.
Rush AJ, Fava M, Wisniewski SR, Lavori PW, Trivedi MH, Sackeim HA et al (2004). Sequenced Treatment Alternatives to Relieve Depression (STAR*D): rationale and design. Control Clin Trials 25: 118–141.
Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH (1996). The Inventory of Depressive Symptomatology (IDS): psychometric properties. Psychol Med 26: 477–486.
Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN et al (2003). The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), Clinician Rating (QIDS-C), and Self-Report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry 54: 573–583.
Rush AJ, Trivedi MH, Wisniewski SR, Stewart JW, Nierenberg AA, Thase ME et al (2006b). Bupropion-SR, sertraline, or venlafaxine-XR after failure of SSRIs for depression. N Engl J Med 354: 1231–1242.
Shioda K, Nisijima K, Yoshino T, Kato S (2004). Extracellular serotonin, dopamine and glutamate levels are elevated in the hypothalamus in a serotonin syndrome animal model induced by tranylcypromine and fluoxetine. Prog Neuropsychopharmacol Biol Psychiatry 28: 633–640.
Sullivan PF (2007). Spurious genetic associations. Biol Psychiatry 61: 1121–1126.
Svenningsson P, Bateup H, Qi H, Takamiya K, Huganir RL, Spedding M et al (2007). Involvement of AMPA receptor phosphorylation in antidepressant actions with special reference to tianeptine. Eur J Neurosci 26: 3509–3517.
Taylor M, Murphy SE, Selvaraj S, Wylezinkska M, Jezzard P, Cowen PJ et al (2008). Differential effects of citalopram and reboxetine on cortical Glx measured with proton MR spectroscopy. J Psychopharmacol 22: 473–476.
Trivedi MH, Fava M, Wisniewski SR, Thase ME, Quitkin F, Warden D et al (2006a). Medication augmentation after the failure of SSRIs for depression. N Engl J Med 354: 1243–1252.
Trivedi MH, Rush AJ, Ibrahim HM, Carmody TJ, Biggs MM, Suppes T et al (2004). The Inventory of Depressive Symptomatology, Clinician Rating (IDS-C) and Self-Report (IDS-SR), and the Quick Inventory of Depressive Symptomatology, Clinician Rating (QIDS-C) and Self-Report (QIDS-SR) in public sector patients with mood disorders: a psychometric evaluation. Psychol Med 34: 73–82.
Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L et al (2006b). Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry 163: 28–40.
Acknowledgements
The Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study is supported by federal funds from NIMH under contract N01 MH-90003 to the University of Texas Southwestern Medical Center at Dallas (AJ Rush, principal investigator). Dr Perlis is supported by NIMH K23MH67060, a NARSAD Young Investigator/Sidney R Baer Jr Foundation Award, and a Bowman Family Foundation award. Additional support provided by NIMH Intramural program. We thank Rutgers Cell and DNA Repository for extracting DNA and providing samples. We appreciate the support of Forest Laboratories for providing citalopram at no cost to the STAR*D study. We thank Stephen Wisniewski and Heather Eng for providing the clinical data. We thank the STAR*D Research Team for conducting the clinical study and obtaining clinical data and the blood samples for these analyses. Finally, we thank the study participants without whom this study would not have been possible.
Author information
Authors and Affiliations
Corresponding author
Additional information
DISCLOSURE/CONFLICT OF INTEREST
Roy Perlis
Research support: Eli Lilly and Company, Elan/Eisai, National Institute of Mental Health, NARSAD, Bowman Family Foundation, American Philosophical Society.
Advisory/Consulting: AstraZeneca, Bristol-Myers Squibb, Eli Lilly and Company, Pfizer Inc.
Speaking: AstraZeneca, Bristol-Myers Squibb Eli Lilly and Company, GlaxoSmithKline, Pfizer Inc.
Equity holdings: None.
Royalty/patent, other income: None.
Maurizio Fava
Research support: Abbott Laboratories, Alkermes, Aspect Medical Systems, AstraZeneca, Bristol-Myers Squibb, Cephalon, Eli Lilly and Company, Forest Pharmaceuticals Inc., GlaxoSmithKline, J and J Pharmaceuticals, Lichtwer Pharma GmbH, Lorex Pharmaceuticals, Novartis, Organon Inc., Pamlab LLC, Pfizer Inc., Pharmavite, Roche, Sanofi/Synthelabo, Solvay Pharmaceuticals Inc., Wyeth-Ayerst Laboratories.
Advisory/Consulting: Aspect Medical Systems, AstraZeneca, Bayer AG, Biovail Pharmaceuticals Inc., BrainCells Inc. Bristol-Myers Squibb, Cephalon, Compellis, Cypress Pharmaceuticals, Dov Pharmaceuticals, Eli Lilly and Company, EPIX Pharmaceuticals, Fabre-Kramer Pharmaceuticals Inc., Forest Pharmaceuticals Inc., GlaxoSmithKline, Grunenthal GmBH, Janssen Pharmaceutica, Jazz Pharmaceuticals, J and J Pharmaceuticals, Knoll Pharmaceutical Company, Lundbeck, MedAvante Inc., Neuronetics, Novartis, Nutrition 21, Organon Inc., Pamlab LLC, Pfizer Inc., PharmaStar, Pharmavite, Roche, Sanofi/Synthelabo, Sepracor, Solvay Pharmaceuticals Inc., Somaxon, Somerset Pharmaceuticals, Wyeth-Ayerst Laboratories.
Speaking: AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Cephalon, Eli Lilly and Company, Forest Pharmaceuticals Inc., GlaxoSmithKline, Novartis, Organon Inc., Pfizer Inc., PharmaStar, Wyeth-Ayerst Laboratories.
Equity Holdings: Compellis, MedAvante.
Royalty/patent, other income: None.
Madhukar Trivedi
Research Support: Bristol-Myers Squibb; Cephalon Inc.; Corcept Therapeutics Inc.; Cyberonics Inc.; Eli Lilly and Company; Forest Pharmaceuticals; GlaxoSmithKline; Janssen Pharmaceutica; Merck; National Institute of Mental Health; National Alliance for Research in Schizophrenia and Depression; Novartis; Pfizer Inc.; Predix Pharmaceuticals; Wyeth-Ayerst Laboratories.
Advisory/Consulting: Abbott Laboratories Inc.; Akzo (Organon Inc.); Bayer; Bristol-Myers Squibb; Cyberonics Inc.; Forest Pharmaceuticals; GlaxoSmithKline; Janssen Pharmaceutica; Johnson & Johnson PRD; Eli Lilly & Company; Meade Johnson; Parke-Davis Pharmaceuticals, Inc.; Pfizer, Inc.; Pharmacia & Upjohn; Sepracor; Solvay Pharmaceuticals Inc.; Wyeth-Ayerst Laboratories.
Speaking: Akzo (Organon Inc.); Bristol-Myers Squibb; Cyberonics Inc.; Forest Pharmaceuticals; Janssen Pharmaceutica Products, LP; Eli Lilly and Company; Pharmacia and Upjohn; Solvay Pharmaceuticals Inc.; Wyeth-Ayerst Laboratories.
Equity Holdings: None (exclude mutual funds/blinded trusts).
Royalty/patent, other income: None.
A John Rush
Speaker's Bureau: Cyberonics Inc.; Forest Pharmaceuticals Inc.; GlaxoSmithKline.
Advisory Boards/Consultant: Advanced Neuromodulation Systems Inc.; Best Practice Project Management Inc.; Bristol-Myers Squibb; Cyberonics Inc.; Eli Lilly and Company; Forest Pharmaceuticals Inc.; Gerson Lehman Group; GlaxoSmithKline; Healthcare Technology Systems; Jazz Pharmaceuticals; Merck; Neuronetics; Ono Pharmaceuticals; Organon Inc.; Personality Disorder Research Corp.; Urban Institute; Wyeth-Ayerst Laboratories.
Research Support: Robert Wood Johnson Foundation, National Institute of Mental Health, Stanley Medical Research Institute.
Royalties: Guilford Publications, Healthcare Technology Systems.
Stock: Pfizer Inc.
Jordan Smoller
Dr Smoller has received honoraria from Hoffman-La Roche Inc. and has served on an advisory board for Roche Diagnostics Corporation. He has received research funding from the National Institute of Mental Health and the National Alliance for Research in Schizophrenia and Depression.
The other authors have no financial competing interests to disclose.
Supplementary Information accompanies the paper on the Neuropsychopharmacology website (http://www.nature.com/npp)
Rights and permissions
About this article
Cite this article
Perlis, R., Laje, G., Smoller, J. et al. Genetic and Clinical Predictors of Sexual Dysfunction in Citalopram-Treated Depressed Patients. Neuropsychopharmacol 34, 1819–1828 (2009). https://doi.org/10.1038/npp.2009.4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2009.4
Keywords
This article is cited by
-
Paraphilic disorders, psychopathy, and those who sexually offend: a narrative review of treatment modalities
International Journal of Impotence Research (2023)
-
Association between serotonin 2A receptor (HTR2A), serotonin transporter (SLC6A4) and brain-derived neurotrophic factor (BDNF) gene polymorphisms and citalopram/sertraline induced sexual dysfunction in MDD patients
The Pharmacogenomics Journal (2020)
-
TRAILR1 (rs20576) and GRIA3 (rs12557782) are not associated with interferon-β response in multiple sclerosis patients
Molecular Biology Reports (2020)
-
Post-finasteride syndrome and post-SSRI sexual dysfunction: two sides of the same coin?
Endocrine (2018)
-
Sexual Function Across Aging
Current Psychiatry Reports (2016)