Abstract
Failures in cortical control of fronto-striatal neural circuits may underpin impulsive and compulsive acts. In this narrative review, we explore these behaviors from the perspective of neural processes and consider how these behaviors and neural processes contribute to mental disorders such as obsessive–compulsive disorder (OCD), obsessive–compulsive personality disorder, and impulse-control disorders such as trichotillomania and pathological gambling. We present findings from a broad range of data, comprising translational and human endophenotypes research and clinical treatment trials, focussing on the parallel, functionally segregated, cortico-striatal neural projections, from orbitofrontal cortex (OFC) to medial striatum (caudate nucleus), proposed to drive compulsive activity, and from the anterior cingulate/ventromedial prefrontal cortex to the ventral striatum (nucleus accumbens shell), proposed to drive impulsive activity, and the interaction between them. We suggest that impulsivity and compulsivity each seem to be multidimensional. Impulsive or compulsive behaviors are mediated by overlapping as well as distinct neural substrates. Trichotillomania may stand apart as a disorder of motor-impulse control, whereas pathological gambling involves abnormal ventral reward circuitry that identifies it more closely with substance addiction. OCD shows motor impulsivity and compulsivity, probably mediated through disruption of OFC-caudate circuitry, as well as other frontal, cingulate, and parietal connections. Serotonin and dopamine interact across these circuits to modulate aspects of both impulsive and compulsive responding and as yet unidentified brain-based systems may also have important functions. Targeted application of neurocognitive tasks, receptor-specific neurochemical probes, and brain systems neuroimaging techniques have potential for future research in this field.
Similar content being viewed by others
INTRODUCTION
Whereas acts with impulsive or compulsive features may contribute specifically to creativity and endurance and generally to adaptive human behavior, disordered regulation of impulsive or compulsive behavior may be associated with adverse consequences and have a function in the development of mental disorder. Impulsivity may be defined as ‘a predisposition toward rapid, unplanned reactions to internal or external stimuli with diminished regard to the negative consequences of these reactions to the impulsive individual or to others’ (Chamberlain and Sahakian, 2007; Potenza, 2007b). In contrast, compulsivity represents a tendency to perform unpleasantly repetitive acts in a habitual or stereotyped manner to prevent perceived negative consequences, leading to functional impairment (WHO, 1992; Hollander and Cohen, 1996; Chamberlain et al, 2006b). These two constructs may be viewed as diametrically opposed, or alternatively, as similar, in that each implies a dysfunction of impulse control (Stein and Hollander, 1995). Each potentially involves alteration within a wide range of neural processes, including attention, perception, and coordination of motor or cognitive responses.
Neuroanatomical models posit the existence of separate but intercommunicating ‘compulsive’ and ‘impulsive’ cortico-striatal circuits, differentially modulated by neurotransmitters (Robbins, 2007; Brewer and Potenza, 2008). In the compulsive circuit, a striatal component (caudate nucleus) may drive compulsive behaviors and a prefrontal component (orbitofrontal cortex, OFC) may exert inhibitory control over them. Similarly, in the impulsive circuit, a striatal component (ventral striatum/nucleus accumbens shell) may drive impulsive behaviors and a prefrontal component (anterior cingulate/ventromedial prefrontal cortex, VMPFC) may exert inhibitory control. Thus, in this model, there exist at least two striatal neural circuitries (one compulsive and one impulsive) that drive these behaviors, and two corresponding prefrontal circuitries that restrain these behaviors. Hyperactivity within the striatal components or abnormalities (presumably hypoactivity) in the prefrontal components may thus result in an increased automatic tendency for executing impulsive or compulsive behaviors, depending on the sub-component afflicted. Other possible abnormalities within cortico-striatal circuits (eg related to diminished striatal activation to rewards) may also contribute to seemingly impulsive or compulsive behaviors during engagement in reward-related behaviors. These pathologies can be explored using tasks of cognitive performance that tap into these specific functions and/or by functional imaging studies that measure activity within these neural systems. Overlap between these functional systems, so that what starts out as a problem in the impulsive circuit may end up as a problem in the compulsive circuit and vice versa, may contribute toward the impulsive–compulsive diathesis model proposed by Hollander and Wong (1995) (Brewer and Potenza, 2008).
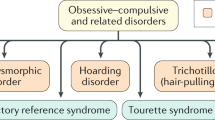
There exist certain mental disorders for which impulsive and compulsive behaviors seem, at least on phenotypic grounds, to be the core and most damaging ingredient. These often highly heritable disorders, currently classified across several DSM-IV-TR (APA) diagnostic categories, include obsessive–compulsive disorder (OCD), body dysmorphic disorder, Tourette's syndrome, trichotillomania, attention deficit hyperactivity disorder (ADHD), pathological gambling, and substance addictions (SAs). Of interest, autism is characterized by both compulsive behavior (as one of the three core symptom domains) as well as impulsive behavior (as one of the associated symptom domains).
Traditionally, compulsive and impulsive disorders have been viewed at opposite ends of a single dimension; the former driven by a desire to avoid harm and the latter by reward-seeking behavior. However, convergent evidence from translational studies suggests that a shared tendency toward behavioral disinhibition, presumably resulting from failures in ‘top–down’ cortical control of fronto-striatal circuits, or alternatively from overactivity within striatal circuitry, may crucially underpin both impulsive and compulsive disorders. Thus, rather than polar opposites, compulsivity and impulsivity may represent key orthogonal factors that each contribute to varying degrees across these disorders.
Many of these disorders tend to occur together, either within the same individual or clustering within families, implying the possibility of shared pathophysiological mechanisms (Hollander et al, 2007b). Moreover, there is evidence of overlap in the treatment-response across some disorders. OCD typically responds to serotonin reuptake inhibitors (SRIs; clomipramine and selective SRIs, SSRIs) and to SSRIs combined with antipsychotic agents (Fineberg et al, 2005). Antipsychotics represent first-line treatment for Tourette's syndrome, and it is, therefore, interesting that their combination with SSRIs shows greater efficacy in tic-related OCD (Bloch et al, 2006). Compulsions associated with autistic disorders may also respond to low-dose SSRI and to antipsychotics (Kolevzon et al, 2006). Trichotillomania may respond to SRIs and to antipsychotics, though confirmation in controlled studies is required (Chamberlain et al, 2007d). ADHD, on the other hand, responds to noradrenergic reuptake inhibitors as well as dopaminergic agents (eg amphetamine), pathological gambling, and substance abuse disorders may also share a therapeutic response to opiate antagonists (Brewer et al, 2008).
Attribution of cause and effect, using clinical data alone, may be confounded by the multiplicity of associated symptom domains that occur within complex mental disorders. Indeed, this group of disorders is characterized by considerable phenotypic heterogeneity and overlap. For example, some cases with autism show no symptoms of ADHD or compulsive behavior, others show ADHD, others OCD, and yet others show repetitive motor behaviors that do not resemble OCD. Translational research investigates from the perspective of underlying mechanisms, and may thus be capable of pinpointing neural contributions driving specific aspects of mental disorder. Endophenotypes are measurable, heritable traits, theoretically situated in an intermediate position between the clinical phenotype and the disease-susceptibility genotype. Such ‘intermediate phenotypes’ are hypothesized to be more directly related to genetic risk for polygenic mental disorders than clinically expressed behaviors (Gottesman and Gould, 2003; Chamberlain and Menzies, 2009). Endophenotypic models of disease may be helpful for clarifying our understanding of the genetic basis of complex brain disorders and thus for informing diagnostic classification. Currently, impulsive and compulsive disorders are classified within disparate DSM-IV categories. As the American Psychiatric Association considers the re-classification of OCD, anxiety disorders and impulse-control disorders (ICDs) for the forthcoming DSM-V revision (Fineberg et al, 2007a), it is timely to review the underpinning mechanisms of these disorders.
In this narrative review, we consider the neural and neuropsychological mechanisms associated with impulsive and compulsive acts and their contribution toward examples of impulsive and compulsive disorders. We assemble relevant findings from a broad range of complementary data, comprising recently published and as yet unpublished translational studies, human endophenotypic research, and clinical treatment trials, including ongoing work from our own units in the United Kingdom and the United States. Our analysis focusses on probing the parallel, functionally segregated, cortico-striatal neural projections from OFC to medial striatum (caudate nucleus), proposed to drive compulsive activity, and from the anterior cingulate/VMPFC to the ventral striatum (nucleus accumbens shell), proposed to drive impulsive activity, and the cross-talk between them (Robbins, 2007; Brewer and Potenza, 2008) (Figure 1).
Compulsivity and impulsivity: candidate neural processes contributing to mental disorders. Although impulsive and compulsive disorders can be thought of as polar opposites, failures in cortical control of fronto-striatal neural circuits may underpin both compulsivity (orbitofrontal cortex (OFC)—caudate) and impulsivity (right inferior frontal cortex (RIFC)—globus pallidus and anterior cingulate cortex (ACC)/ventromedial prefrontal cortex (VMPFC)—ventral striatum/nucleus accumbens (NA) shell), and contribute to these disorders.
Using these data, we attempt to address key questions including: (i) how much do compulsivity and impulsivity contribute to these disorders, (ii) to what extent do they depend on shared or separate neural circuitry, (iii) what are the mediating monoaminergic mechanisms, (iv) do impulsive or compulsive behavioral components have any prognostic value related to clinical treatment, and (v) is there a unifying-dimensional model that fully accommodates these data? We also draw attention to prospects for future research we believe may most fruitfully advance the field.
TRANSLATIONAL MODELS OF IMPULSIVITY AND COMPULSIVITY
Objective neurocognitive tests hold potential for elucidating the mechanisms by which pharmacological agents exert their beneficial clinical effects and for predicting clinical outcomes (Chamberlain et al, 2007e; Brewer and Potenza, 2008). Using sensitive and domain-specific neurocognitive tasks, impulsivity and compulsivity may be fractionated into separate and quantifiable neurobiologically specific domains in human beings and experimental animals, with specific aspects involving dissociable components of fronto-striatal circuitry (Winstanley et al, 2006).
Data indicate that impulsivity may derive from one or more distinct neurocognitive mechanisms. These include a tendency to pre-potent motor disinhibition, measured by the stop signal reaction time (SSRT) task (Aron and Poldrack, 2005), mediated in human beings through activation of right inferior frontal (RIF) cortex and its subcortical connections (Rubia et al, 2003) and modulated in rats and human beings by norepinephrine (Chamberlain et al, 2006c, 2007a; Cottrell et al, 2008), but not serotonin (Clark et al, 2005; Chamberlain et al, 2006d). Another aspect involves difficulty in delaying gratification and choosing immediate small rewards despite negative long-term consequences, measured by decision making or gambling tasks such as the Cambridge Gambling Task (CANTAB), mediated through orbitofrontal and related cortical circuitry under probable serotonergic modulation (Rogers et al, 1999b), and subcortical circuitry under joint dopaminergic and serotonergic control (Winstanley et al, 2006). A third component comprises insufficient information sampling before making a choice, measured by information sampling tasks such as the Reflection Task (Clark et al, 2006) and possibly the 5-Choice Serial Reaction Time Task (5-CSRTT) (Robbins, 2002) (Table 1).
Compulsivity is, perhaps, less well understood. Failures in (i) reversal learning (ie the ability to adapt behavior after negative feedback, measured by specific reversal learning tasks) and (ii) extra-dimensional (ED) attentional set-shifting, may each contribute toward its expression (Dias et al, 1996; Clarke et al, 2005). Both deficits constitute measures of cognitive inflexibility, but each seems subserved by separate neural circuitry.
Reversal learning is impaired by lesions to the OFC (but not dorsolateral prefrontal cortex, DLPFC) across species (Dias et al, 1996; Berlin et al, 2004; Hornak et al, 2004; Boulougouris et al, 2007). In human beings, the OFC activates selectively during reversal learning (Hampshire and Owen, 2006). In contrast, lesions to the lateral PFC impair ED set-shifting in primates (Dias et al, 1996), and in human beings performance of the task is associated with selective activation of the bilateral ventrolateral prefrontal cortex (VLPFC) (Hampshire and Owen, 2006) (Table 1).
There is now considerable evidence linking reversal learning with 5-HT mechanisms, including in rodents (Masaki et al, 2006; Boulougouris et al, 2008; Lapiz-Bluhm et al, 2009), non-human primates (Clarke et al, 2004, 2005; Walker et al, 2009), and human beings (Park et al, 1994; Rogers et al, 1999a; Evers et al, 2005) based on pharmacological, neurochemical and dietary manipulations, and evidence of genetic polymorphisms in rhesus monkeys (Izquierdo et al, 2007). Generally, reducing brain serotonin, especially in specific regions such as the OFC (eg Clarke et al, 2004), impairs reversal learning. Systemic administration of a 5-HT-2A receptor antagonist has also been shown to impair spatial reversal learning (Boulougouris et al, 2008). A 5-HT6 receptor antagonist has also been shown to enhance both reversal learning and attentional shifting in rats (Hatcher et al, 2005). However, there have been some failures to find effects on reversal learning, often after tryptophan depletion, in human beings (Talbot et al, 2006) and rats (van der Plasse and Feenstra, 2008), and serotonin transporter deficiency in rats also does not seem to affect simple spatial reversal (Homberg et al, 2007).
5-HT2 RECEPTOR SUBTYPES MAY UNDERPIN COMPULSIVE BEHAVIORS
A multiplicity of 5-HT receptors has been identified for which specific ligands are under development. Preliminary evidence from animal and human studies suggests a function for 5-HT2 receptors in compulsive behaviors. Transgenic mice lacking 5-HT2C receptors develop compulsive behavior patterns that constitute a plausible model for OCD (Chou-Green et al, 2003). However, there is an apparent mismatch of data obtained from this genetic preparation with other data, possibly because of unspecified developed compensatory processes in the transgenic preparation, as recent pharmacological data indicate the opposite finding that 5-HT2C receptor activation is associated with increased compulsivity. Thus, in a rewarded T-maze alternation rat model of OCD, Tsaltas et al (2005) found that administration of m-chlorophenylpiperazine (mCPP), a mixed serotonin agonist with potent 5-HT2C agonist effects, increased persistence or compulsivity of responding, whereas chronic pretreatment with an SSRI (fluoxetine), but not a benzodiazepine or desipramine, abolished the effects of mCPP. Challenge with the 5-HT1B receptor agonist naratriptan had no effect on compulsivity within this model, suggesting a specific function for the 5-HT2C receptor, which may be down-regulated by chronic SSRI treatment. In OCD patients, acute pharmacological challenge with mCPP exacerbated OCD symptomatology (Hollander et al, 1991b). This effect was also attenuated by pretreatment with fluoxetine (Hollander et al, 1991a) and clomipramine (Zohar et al, 1988). Moreover, consistent with these findings, Boulougouris et al (2008) found that a 5-HT2C receptor antagonist improved reversal learning. On the other hand, activation of prefrontal 5-HT2A receptors has been proposed to underpin the anticompulsive effect of SSRIs (Westenberg et al, 2007). Second generation antipsychotics may exacerbate compulsive behaviors in patients with schizophrenia, and it has been proposed that this occurs through potent 5-HT2A antagonism (Poyurovsky et al, 2008), though dopamine (DA) receptor antagonism represents another possible mechanism. Moreover, second and first generation antipsychotics show clinical efficacy when combined with SSRIs in OCD (Fineberg and Gale, 2005), perhaps by increasing DA activity within the frontal cortex (Denys et al, 2004).
PHARMACOLOGICAL DIFFERENTIATION OF IMPULSIVITY AND COMPULSIVITY; RECEPTOR LIGANDS
In animal models, an intriguing dissociation between the effects of 5-HT2A and 5-HT2C receptor antagonists on measures of impulsivity and compulsivity has been observed. On the 5-CSRTT, systemic administration of a 5-HT2C receptor antagonist (SB24284) exacerbated the enhanced impulsivity normally observed after global 5-HT depletion produced by intracerebroventricular administration of 5,7-dihydroxytryptamine; a similar SB24284-related enhancement in impulsivity was seen in sham-operated rats (Winstanley et al, 2004). In contrast, systemic administration of a selective 5-HT2A receptor antagonist (M100907) had opposite actions, remediating impulsivity in both sham-operated and 5-HT-depleted rats. These contrasting influences of the 5-HT2A and 5-HT2C receptor antagonists were mimicked by infusions of the drugs into the nucleus accumbens, but not the mPFC, in intact animals (Cottrell et al, 2008). However, in variations of the 5-CSRTT, it was possible to detect significant reductions in impulsivity after intra-mPFC infusion of the 5-HT2A receptor antagonist. The latter findings were consistent with observations that, in a population of Lister hooded rats, it was generally the most impulsive animals that had the greatest concentrations of 5-HT in the mPFC, indicating that individual differences and regional specificity are important considerations in understanding the relationship between 5-HT and behavioral disinhibition.
The effects of central 5-HT manipulations on impulsivity stand in some contrast to their actions on attentional function per se in the 5-CSRTT. Several papers have observed either no effects or actual enhancement of attentional accuracy when impulsive behavior is enhanced (Harrison et al, 1997) or after treatment with systemic or intra-PFC 5-HT2A receptor antagonists such as ketanserin or M100907 (Passetti et al, 2003; Winstanley et al, 2003) as well as the 5-HT1A receptor agonist 8-OHDPAT (Winstanley et al, 2003). These findings are compatible with the hypothesis that inhibitory control over impulsive behavior and attentional function are only loosely coupled in this test situation and suggests that there will be no simple relationship between the two in such syndromes as ADHD.
An additional element of complexity is introduced when considering the influences of these same drugs on measures of compulsivity. Using a simple serial spatial reversal test that is sensitive to lesions of the OFC (Boulougouris et al, 2007), it was found that 5-HT2C receptor antagonism (produced by systemic administration) facilitated reversal learning. M1000907 had the opposite effect of impairing it (Tsaltas et al, 2005). Note that in terms of remediation, this is opposite to what that was found for measures of impulsivity. Similar enhancements of reversal learning after treatment with the 5-HT2C antagonist were also found after infusion into the OFC (Boulougouris, Glennon, Robbins, unpublished results) (Table 2).
Regardless of precise elucidation of mechanism, these data pharmacologically dissociate these forms of impulsivity and compulsivity, suggesting that they cannot hinge on a common process of behavioral inhibition. The dissociation cannot easily be explained in terms of differences in species, drug, or dose of receptor antagonist used or the form of motivation used; they must be task–dependent—as both tasks require response inhibition for efficient performance. Thus, we conclude that there is some other aspect of the processes engaged by the task, which differentiates them. These results also imply that impulsivity and compulsivity are functionally separate and reciprocally yoked, lending support to the impulsive–compulsive diathesis model (Hollander and Wong, 1995). They also suggest that impulsivity and compulsivity can be dissociated by selective 5-HT2 receptor ligands and hint at new clinical applications for such agents. However, it will be important to resolve how these data fit with the consistent finding that 5-HT depletion in the OFC impairs visual object reversal learning in marmoset monkeys (Clarke et al, 2004, 2005; Yucel et al, 2007). In addition, it would seem likely that these seemingly opposed effects are mediated through separate neural pathways: in the case of impulsivity, through projections from the infralimbic VMPFC (area 25), an area richly innervated by 5-HT2A receptors and strongly implicated in affective regulation, toward the shell of the nucleus accumbens (Vertes, 2004) and, in the case of compulsivity, in connections between the OFC and the caudate nucleus (or the dorsomedial striatum in the rat) (Schilman et al, 2008).
DISSOCIATING IMPULSIVE AND COMPULSIVE DISORDERS USING NEUROPSYCHOLOGICAL TASKS
Impulsive and compulsive disorders usually involve a relatively diminished ability to delay or inhibit repetitive thoughts or behaviors. Thus, problems suppressing or inhibiting inappropriate behavior could underpin both impulsive and compulsive symptomatology (Chamberlain et al, 2005; Stein et al, 2006). ADHD is a disorder of early onset characterized by poorly conceived, impulsive actions and robust impairment in motor inhibition as measured on tasks such as the SSRT (Aron et al, 2003; Lijffijt et al, 2005). Administration of cognition-enhancing agents such as atomoxetine and methylphenidate improves symptoms and ameliorates SSRT deficits in adults with ADHD, presumably acting through increased noradrenergic (or possibly dopaminergic) neurotransmission (Chamberlain et al, 2007a).
Studies in OCD patients have revealed SSRT impairment and poor performance on ED-shifting tasks (Chamberlain et al, 2006a, 2007c; Menzies et al, 2007a), implying both impulsive and compulsive contributions to the disorder. Unaffected first-degree relatives of OCD probands share similar impairment on SSRT and ED-shifting tasks (Chamberlain et al, 2007c) and thus seem to exhibit similar levels of motor impulsivity and cognitive inflexibility, despite a lack of OCD symptoms. In contrast to OCD, application of a similar neurocognitive test battery to individuals with trichotillomania showed a more focal and selective impairment in motor inhibition, consistent with its DSM-IV classification as an ICD (Chamberlain et al, 2006b, 2007b). Whole-brain MRI in unmedicated trichotillomania identified increased gray-matter density in the left putamen and multiple cortical regions (Chamberlain et al, 2008b). Increased gray matter in striatal regions has also been reported in studies of Tourette syndrome (Bohlhalter et al, 2006; Garraux et al, 2006) and OCD (Menzies et al, 2008a). On the other hand, patients with Tourette's syndrome were found to share cognitive inflexibility and to be significantly more impaired than OCD patients on decision-making tasks, but less impaired on a task of motor inhibition (Watkins et al, 2005), though another study investigating adolescents with Tourette's did not find evidence of impaired reward learning compared with controls on a gamble task (Crawford et al, 2005). Li et al (2006) failed to show performance deficits compared with controls on the SSRT in 30 children with Tourette's syndrome.
The overlap of compulsive and impulsive responding within OCD raises the question whether impulsivity normally drives compulsivity, and thus whether it is possible to show pathological compulsivity without motor impulsivity. If so, which disorders might show ‘pure’ compulsivity? Individuals with obsessive–compulsive personality disorder comorbid with OCD showed increased impairment specifically in the domain of ED shifting. This finding is consistent with the clinical presentation of obsessive–compulsive personality disorder, which is characterized by excessive cognitive and behavioral inflexibility, but does not involve repetitive behaviors (ie obsessions or compulsions). Thus, obsessive–compulsive personality disorder may constitute a prototypic-compulsive disorder (Fineberg et al, 2007b). Confirmatory studies using individuals with non-comorbid OCPD would be welcomed.
NEUROCOGNITIVE ENDOPHENOTYPES, OCD, AND BEYOND
Whereas neurocognitive tasks may be used to identify fairly specific neuropsychological domains, complementary neuroimaging may be used to visualize the anatomical substrates and neural circuits underlying genetic risk for a disorder. By integrating neurocognitive and structural MRI parameters, using a whole-brain multivariate analysis (technique of partial least squares, McIntosh and Lobaugh, 2004) and a novel permutation test, Menzies et al (2007a) identified familial effects on performance on a motor-inhibition task (the SSRT) that were associated with variation in multiple anatomical sites. Both OCD patients and their unaffected first-degree relatives exhibited impaired motor inhibitory control, indexed by prolonged latency of the SSRT and longer latency was associated with both decreased gray-matter volume in the OFC and RIF cortex (areas conventionally associated with OCD and SSRT activation, respectively) and increased gray-matter volume in areas of the striatum, cingulate, and parietal cortex. These results argue for the first structural MRI endophenotype-mediating familial, and possibly genetic, risk for OCD-related impulsivity. Future studies might profitably test for specific genetic effects on variability in such intermediate phenotypes, as an alternative to classical association designs, for discovery of susceptibility alleles.
The findings with the SSRT, a relatively disease-non-specific task of motor impulsivity, raise the possibility that such an endophenotype may not be restricted to OCD, but in addition relate to other disorders within, and perhaps outside, the impulsive–compulsive disorders spectrum. For example, individuals with ADHD and their relatives seem impaired on motor-inhibition tasks (Crosbie and Schachar, 2001), but it is not yet clear whether the anatomical correlates of impairment for those with familial risk for ADHD are the same or differ from people with familial risk for OCD.
The within-subject correlation between decreased gray-matter volumes within frontal areas of cortex and increased volumes in the striatum resonates with empirical OCD models derived from early functional imaging studies (Baxter et al, 1987) and later structural and functional MRI studies (for review see, Menzies et al, 2008a). Preliminary findings from a subsequent study using diffusion tensor imaging within OCD family members (Menzies et al, 2008b) identified evidence of white-matter abnormalities in complementary brain areas including the right medial frontal (adjacent to anterior cingulate cortex, ACC) and right inferior parietal (adjacent to parietal cortex) zones, compatible with results from a prior study involving OCD patients (Szeszko et al, 2005). However, by extending this study to include unaffected OCD family members, we have proposed these findings as possible white-matter endophenotypes for OCD (Menzies et al, 2008b).
In addition to structural brain abnormalities in patients with OCD and their relatives, research has started to probe functional integrity of fronto-striatal circuitry using fMRI paradigms adapted for this purpose. Using an fMRI cognitive flexibility paradigm, it was shown that patients with OCD and their unaffected first-degree relatives exhibited under-activation of the bilateral lateral OFC during reversal of responses; they also tended to underactivate lateral aspects of the PFC during ED shifting at trend levels (Chamberlain et al, 2008a).
Together, these findings indicate that neuroimaging techniques can provide a rich source of candidate endophenotypes for OCD. The results are compatible with theories implicating failure of top–down cortical inhibition of striatally mediated behaviors. They suggest that the idiosyncratic obsessive ruminations and compulsive rituals that characterize OCD are accompanied by more general propensities toward rigid and disinhibited behavior that are shared among non-affected family members. Thus, difficulties in ‘cognitive inhibition and flexibility’ may causally contribute to the development of symptoms of OCD. Future work should examine whether this approach can be successfully generalized to other disorders on the impulsive–compulsive spectrum. The clinical relevance of putative endophenotypes requires additional investigation to determine whether (and how) unaffected relatives who share trait markers with OCD probands might be differentiated from non-OCD-related controls. An improved understanding is needed of mechanisms by which environmental factors might elicit OCD in genetically vulnerable individuals, and whether or how treatments could help modify disease onset.
ICDS AND MODELS OF REWARD
In contrast to compulsive disorders such as OCD, some ICDs, such as pathological gambling, are characterized by choosing short-term gratification irrespective of negative long-term consequences. Berlin et al (2008) compared individuals with and without pathological gambling on a selected neuropsychological battery (Berlin et al, 2008). Individuals with pathological gambling who scored more highly on self-reported measures of impulsivity such as the Barratt Impulsivity Scale had on average a faster subjective sense of time (overestimated time) compared with controls and showed deficits measured by a frontal behavior questionnaire considered to reflect prefrontal-cortical dysfunction. Subjects with pathological gambling also showed disadvantageous decision making on the Iowa Gamble Task (Bechara et al, 1994) and executive planning deficits (eg on Spatial Planning and Stockings of Cambridge subtests of CANTAB), implicating prefrontal circuitry including the OFC/VMPFC region. In contrast to OCD (Watkins et al, 2005; Chamberlain et al, 2006b), set-shifting was unimpaired in pathological gambling. However, other studies indicate that individuals with pathological gambling score highly on specific measures of compulsivity or harm avoidance, and that measures of impulsivity and compulsivity may change over time (eg, during the course of treatment (Potenza, 2007a; Blanco et al, 2009). These findings suggest that impulsivity and compulsivity are not diametrically opposed and share a complex, orthogonal relationship, with specific disorders showing a predominance of one construct over the other that may shift in a temporally dynamic manner.
Hollander et al (2007a) compared three groups of age- and gender-matched individuals, comprising pathological gambling (predominantly impulsive) and OCD and autism (predominantly compulsive) disorders, using a battery of clinical, cognitive, and functional imaging tasks. During execution of response-inhibition tasks (go/no-go) that normally activate fronto-striatal circuitry, all three spectrum-disorder groups showed abnormal fMRI activation in dorsal (cognitive) and ventral (emotional) regions of the ACC compared with healthy controls. There were no significant performance differences between the four groups. However, between-group analyses showed decreased dorsal ACC activation in all three patient groups relative to healthy controls. Thus, during response inhibition, both compulsive and impulsive disorders were characterized by diminished dorsal ACC activation, which may contribute toward failure to properly inhibit motoric behaviors across these disorders.
When individual activation patterns of the ventral ACC were correlated with measures of impulsivity or compulsivity, disorder-specific between-group differences emerged. Within the pathological gambling group, increased ventral ACC/ventral striatum activation correlated positively with clinical measures of increased impulsive reward-seeking behavior (as measured by TCI Impulsiveness and Total Harm Avoidance, NEO-FFI Extraversion, Total Time Estimation, and the Iowa Gambling Task). Furthermore, gamblers with increased activation in the ventral ACC (area 25) showed lower compulsivity scores on tasks of cognitive set-shifting (ID/ED stages completed). In contrast, in the autistic (compulsive) group, increased ventral ACC/ventral striatum activity correlated with increased severity of compulsive distress-relieving (reinforcing) habits, and increased activation within the same areas of the ventral ACC (area 25) correlated with increased compulsivity (ID/ED shift total errors adjusted) and decreased impulsivity on the Time Estimation task.
This ‘double-dissociation’ suggests that in pathological gambling and autism, prevailing differences in neuromodulation impact on ventral corticostriatal pathways during behavioral inhibition, which in pathological gambling may primarily drive impulsivity and in autism drive compulsivity. It is also reminiscent of data from rats described elsewhere here showing opposing effects of 5-HT2C and 5-HT2A receptor antagonists on impulsivity in the 5-CSRTT and compulsivity (spatial serial reversal learning) (Tsaltas et al, 2005; Boulougouris et al, 2007)—and also of the doubly dissociable findings of Carli et al—that infusions of the 5-HT1A agonist into the infralimbic region reduced perseverative behavior (on the 5-CSRTT) without influencing impulsive responding, with a 5-HT2A receptor antagonist having the opposite effect (Chambers et al, 2004). Together, these findings suggest that the same neural circuitry may drive impulsive or compulsive aspects of human behavior and that 5-HT subtypes in VMPFC (5-HT2A) and OFC (5-HT2C), and dorsal ACC deficits, may have a function in the failure of response inhibition in predominantly impulsive (pathological gambling) and compulsive (OCD, autism) disorders.
REWARD, REINFORCEMENT, AND DA
DA pathways in the mesolimbic system have an important function in reward and reinforcement (Wise, 2002). In disorders of impulse control, increased ventral ACC activation during response inhibition may be related to increased reward-seeking behavior. Preliminary results suggest that pathological gamblers are less sensitive to reward on the TCI reward dependence inventory than healthy controls and seek higher levels of stimulation (novelty seeking) (Berlin et al, 2008). However, other studies of subjects with pathological gambling have found relatively diminished activation of ACC, particularly in its ventral component, during appetitive states and cognitive-control experiments (Potenza et al, 2003a, 2003b). With respect to compulsive disorders, the positive correlation between increased ventral ACC activation during response-inhibition tasks and increased compulsivity on ID/ED stages and total errors adjusted may reflect increased dopaminergic activity from a relative deficit, in line with a mesolimbic DA model of OCD (Joel, 2006).
Hypothetically, intermittent and repeated stimulation of mesolimbic DA pathways may ‘sensitize’ the reward system and lead to escalation in reward seeking (Robinson and Berridge, 1993), which, if combined with poor prefrontal-cortex-mediated inhibitory control, may facilitate DA related and seemingly impulsive-motivated behaviors. Excessive DA release and stimulation may deplete DA stores and lead to anhedonia and depression (Koob and Le Moal, 1997). Indeed, in substance abusers, decreased activity of the mesolimbic/mesocortical DA system, as measured by electrophysiological recordings and in vivo microdialysis, intensifies after escalations in drug intake. This may generate an urge (compulsion) to seek stronger rewards to ‘replenish’ the DA deficiency. The demonstration of decreased striatal D2-like receptors in chronic cocaine users, by PET imaging (Volkow et al, 1999), suggests down-regulation in response to persistently elevated postsynaptic DA concentrations, consistent with the hypothesis of a dysregulated DA system after repeated stimulation of DA release. Thus, what starts as increased DA release leading to increased ventral ACC activity and increased reward seeking (Wise, 2002) may end as a compulsive drive toward increased levels of reward stimulation to restore a resultant DA deficiency. This compulsive drive may be exacerbated by deficient impulse control and decision making, linked to the orbitofrontal, ventromedial prefrontal, and ACC (Adinoff, 2004). However, the extent to which this hypothesis relates to specific ICDs requires direct investigation.
INTEGRATING MECHANISMS OF INHIBITORY CONTROL, REWARD, AND DA
Models of compulsivity and impulsivity posit a balance between 5-HT (2A, 2C) receptor activity in VMPFC/OFC regions regulating aspects of response inhibition, and DA tone in the ventral loops linking ventral ACC with ventral striatum/nucleus accumbens regulating reward and reinforcement behavior. DA neurotransmission, particularly phasic release, in the nucleus accumbens has been associated with reward seeking and reinforcement (Schultz, 2002). Unexpected punishment (monetary loss) has been proposed to result in a dip in central dopaminergic activity, reversal learning, and diminished reward seeking (Frank et al, 2007). Pro-dopamanergic drugs, including levo-dopa and pramipexole (a D2-like DA receptor agonist), have been associated with altering reversal learning to unexpected punishment and ICDs in patients with Parkinson's disease (Cools, 2006; Cools et al, 2006). Pramipexole has also been associated with impaired acquisition of reward-related behavior in healthy participants, consistent with data suggesting that phasic DA signaling is relevant to reinforcing actions leading to reward (Pizzagalli et al, 2008). However, other data indicate that pramipexole, when administered to healthy adults, does not alter behavioral impulsivity, compulsivity, or related constructs including delay-discounting, risk-taking, response inhibition, or perserveration (Hamidovic et al, 2008). Furthermore, olanzapine, a drug with antagonist properties at the D2-like receptor family of DA receptors, has not showed superiority to placebo in two controlled trials involving subjects with pathological gambling (Fong et al, 2008; McElroy et al, 2008), and another D2-like antagonist, haloperidol, has been found to increase gambling-related motivations and behaviors in individuals with pathological gambling (Zack and Poulos, 2007). Radioligand studies are important to clarify potential functions for D3 and D2 receptors in the pathophysiology of pathological gambling, and such studies are complicated by these receptors sharing affinities for existing radioligands.
Taking these findings into account, more research is needed to better understand the relationship between impulsivity, compulsivity, and DA function as they relate to specific psychiatric disorders such as pathological gambling. Impulsive or compulsive disorders may potentially derive from a mesolimbic DA deficiency. However, D2-like antagonists have shown a therapeutic benefit in some (OCD), but not other (pathological gambling) disorders characterized by impulsive and/or compulsive features. Probing both the ventral and dorsal striatal circuitry in human subjects with specific impulsive and compulsive disorders using receptor-specific serotonergic and dopaminergic ligands would be an important next step in understanding these conditions. It may be of particular interest to explore the effects of 5-HT2A and 2C antagonists on DA transmission in this circuitry. These investigations could provide additional insight into aspects such as diminished ventral striatal and VMPFC activation seen across studies involving disorders sharing impulsive and compulsive features, such as pathological gambling and SAs (Reuter et al, 2005; Potenza, 2007a).
Our earlier definition of compulsivity (a tendency to perform repetitive acts in a habitual/stereotyped manner to attempt to prevent adverse consequences) and the current definition (the alleviation of an aversive contingency such as withdrawal) are conceptually related. For example, responding habitually to drug cues may be construed as a mechanism to automatically anticipate a potentially aversive withdrawal syndrome and avert it before it actually happens. Data link these habitual learning mechanisms (or compulsivity) to parts of the dorsal striatum (the caudate for instance), as reviewed earlier. More recent evidence now links the dorsal striatum (its posterior part) to aversive motivational learning (Seymour et al, 2007). Hence, from a neural perspective, evidence supports an overlap between these two concepts of compulsivity.
IMPULSIVITY AND ‘BEHAVIORAL’ ADDICTIONS
Pathological gambling and SAs share many features. The disorders frequently co-occur and show similarities with respect to symptom profiles, gender differences, natural histories, and familial propensities (Grant and Potenza, 2006). Pathological gambling and SA show high levels of impulsivity on reward-discounting tasks, which correlate with poor measures of functioning (Bechara, 2003) and poor treatment outcome (Krishnan-Sarin et al, 2007) for individuals with SAs and thus may have prognostic value for pathological gambling and other ICDs. Neurocognitive and fMRI data suggest pathological gambling and SAs share similar mediating neurocircuitry, in which, as compared with control subjects, relatively diminished activation of the ventral striatum and VMPFC has been observed in reward processing and other paradigms (Potenza et al, 2003a, 2003b). Abnormal fMRI activation of the ventral striatum during reward processing has been identified in the families of individuals with SA and may represent a candidate functional endophenotype for addictive disorders, although this hypothesis requires direct examination in unaffected relatives of pathological gambling probands.
Over time, impulsive habitual responding in pathological gambling and SA may shift toward a more compulsive pattern of behavior, and it has been hypothesized that progressive recruitment of neighboring parallel and increasingly dorsal, cortico-striatal loops occurs in a spiraling manner (Brewer and Potenza, 2008) reminiscent of elaborately spiraling striato-nigrostriatal circuitry identified in primate (Lynd-Balta and Haber, 1994) and rodent (Belin et al, 2008) models of motivated behaviors mapping transitional processes from ventral to dorsal striatum. Prospective, longitudinal studies after these changes within individuals over time will be informative and clinically relevant. Promising research from treating individuals with pathological gambling with opioid antagonists (Brewer et al, 2008) not only discriminate pathological gambling from OCD, in which opioid antagonists such as naloxone have been shown to make OCD worse (Insel and Pickar, 1983), but also suggest a therapeutic function for opioid antagonists in other related ICDs (Grant et al, 2007).
NEW NEURAL TARGETS
To fully understand the neurobiology of impulsivity and compulsivity and the potential for developing new treatments, we may need to explore beyond the neural circuitries discussed in this article to include other neural structures, such as the insula. Data suggest that the insula is important in coordinating ‘conscious’ urges. Lesions of the insula, for instance after stroke, have been associated with rapid smoking cessation (Naqvi et al, 2007). Exposure to cues in the environment, or homeostatic states such as withdrawal, stress, or anxiety, may evoke ‘interoceptive’ representations in the insula that translate into consciously perceived ‘urges’. The insula is anatomically and functionally connected to the aforementioned neural systems implicated in impulsivity, compulsivity, and inhibitory control. Conceivably, the insula interacts with mechanisms of impulsivity and compulsivity by relaying signals (from the environment or the viscera) to 5-HT 2C vs 5-HT 2A receptors in the prefrontal cortex. Thus, interoceptive signals mediated through the insula may, on the one hand, sensitize the neural circuits driving impulsivity or compulsivity. On the other hand, insula activity may ‘hijack’ the inhibitory-control mechanisms of the prefrontal cortex and subvert attention, reasoning, planning, and decision-making processes away from foreseeing the negative consequences of a given action, and toward formulating plans to seek and procure rewarding stimuli such as drugs (Naqvi et al, 2007).
CONCLUSION
Returning, then, to our motivating questions: (i) how much do compulsivity and impulsivity contribute to these disorders, (ii) to what extent do they depend on shared or separate neural circuitry, (iii) what are the mediating monoaminergic mechanisms, (iv) do impulsive or compulsive behavioral components have any prognostic value related to treatment, and (v) is there a unifying-dimensional model that fits the data? According to the available evidence, impulsivity, and compulsivity, each seem to be multidimensional and underpin at least some of the impulsive and compulsive disorders, although the disorders show overlapping, but also distinct profiles. Thus, overarching failures within cortico-striatal neurocircuitry regulating aspects of inhibitory control have been observed in cognitive and imaging studies of all the disorders under review, though for some disorders the data remains tantalizingly incomplete. Trichotillomania may stand apart as a disorder of motor-impulse control and dysfunction within the RIF cortex and its cortico-subcortical connections, whereas pathological gambling has been associated with impulsivity linked to poor decision making and abnormal ventral cortico-striatal circuitry, particularly involving the VMPFC and ventral striatum, that identifies it more closely with SAs. High levels of reward-related impulsivity correlate with poor treatment outcome for SAs and may have prognostic significance for pathological gambling and other ICDs. Compulsive behaviors occurring with autism are associated with similar abnormalities in ventral reward circuitry. OCD, on the other hand, shows motor impulsivity and compulsivity, presumably mediated through disruption of OFC-caudate circuitry, as well as VLPFC, RIF cortex, cingulate, and parietal connections. For these disorders, inter-relating serotonin, DA, and noradrenaline projections are likely to have important modulating functions, as well as other systems as yet incompletely characterized. Over time, impulsivity may evolve into compulsivity and vice versa.
Thus, the picture seems far from a simple linear diathesis with impulsivity and compulsivity occupying opposite poles, and the ‘model’ probably involves a complicated interaction of multiple, orthogonally related diatheses, variably expressed across these circuits and disorders. Impulsive and compulsive disorders are conspicuously heterogeneous, sharing aspects of impulsivity and compulsivity, and become even more complex and thus more difficult to disentangle over time. For example, for impulsive and addictive disorders, tolerance to reward may develop and the behaviors may persist as a method of reducing discomfort (ie they become more compulsive). For compulsive disorders, it is possible that the performance of the repetitive behaviors themselves becomes reinforcing over time, despite their adverse long-term consequences (ie they become more impulsively driven). Mapping these disorders using an agreed-on battery of candidate endophenotypic markers may further clarify their relationship with each other, and future collaborative research enterprises across centers with complementary expertise should be encouraged. Novel approaches may be needed to investigate adequately through ‘triangulating’ approaches such as complex interactions. In this respect, techniques for identifying brain functional systems in neuroimaging data, such as the method of partial least squares (which also allows exploration of multiple behavioral and imaging variables), may have significant potential as procedures for the future in this field. We may also make further progress in dissecting the receptor mechanisms implicated in controlling compulsive and impulsive behavior by use of transgenic mouse preparations in the same tasks devised as for rats (eg 5-CSRTT and reversal learning) and exploration of the full range of 5-HT receptors using new pharmacological ligands.
References
Adinoff B (2004). Neurobiologic processes in drug reward and addiction. Harv Rev Psychiatry 12: 305–320.
Aron AR, Dowson JH, Sahakian BJ, Robbins TW (2003). Methylphenidate improves response inhibition in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry 54: 1465–1468.
Aron AR, Poldrack RA (2005). The cognitive neuroscience of response inhibition: relevance for genetic research in attention-deficit/hyperactivity disorder. Biol Psychiatry 57: 1285–1292.
Baxter Jr LR, Phelps ME, Mazziotta JC, Guze BH, Schwartz JM, Selin CE (1987). Local cerebral glucose metabolic rates in obsessive-compulsive disorder. A comparison with rates in unipolar depression and in normal controls. Arch Gen Psychiatry 44: 211–218.
Bechara A (2003). Risky business: emotion, decision-making, and addiction. J Gambl Stud 19: 23–51.
Bechara A, Damasio AR, Damasio H, Anderson SW (1994). Insensitivity to future consequences following damage to human prefrontal cortex. Cognition 50: 7–15.
Belin D, Mar AC, Dalley JW, Robbins TW, Everitt BJ (2008). High impulsivity predicts the switch to compulsive cocaine-taking. Science 320: 1352–1355.
Berlin HA, Hamilton H, Hollander E (2008). Neurocognition and Temperament in Pathological Gambling. American Psychiatric Association, conference poster: Washington DC.
Berlin HA, Rolls ET, Kischka U (2004). Impulsivity, time perception, emotion and reinforcement sensitivity in patients with orbitofrontal cortex lesions. Brain 127 (Pt 5): 1108–1126.
Blanco C, Potenza MN, Kim SW, Ibanez A, Zaninelli R, Saiz-Ruiz J et al (2009). A pilot study of impulsivity and compulsivity in pathological gambling. Psychiatry Res 167: 161–168.
Bloch MH, Landeros-Weisenberger A, Kelmendi B, Coric V, Bracken MB, Leckman JF (2006). A systematic review: antipsychotic augmentation with treatment refractory obsessive-compulsive disorder. Mol Psychiatry 11: 622–632.
Bohlhalter S, Goldfine A, Matteson S, Garraux G, Hanakawa T, Kansaku K et al (2006). Neural correlates of tic generation in Tourette syndrome: an event-related functional MRI study. Brain 129 (Pt 8): 2029–2037.
Boulougouris V, Dalley JW, Robbins TW (2007). Effects of orbitofrontal, infralimbic and prelimbic cortical lesions on serial spatial reversal learning in the rat. Behav Brain Res 179: 219–228.
Boulougouris V, Glennon JC, Robbins TW (2008). Dissociable effects of selective 5-HT2A and 5-HT2C receptor antagonists on serial spatial reversal learning in rats. Neuropsychopharmacology 33: 2007–2019.
Brewer JA, Grant JE, Potenza MN (2008). The treatment of pathological gambling. Addict Disord Treat 7: 1–14.
Brewer JA, Potenza MN (2008). The neurobiology and genetics of impulse control disorders: relationships to drug addictions. Biochem Pharmacol 75: 63–75.
Chamberlain SR, Blackwell AD, Fineberg NA, Robbins TW, Sahakian BJ (2005). The neuropsychology of obsessive compulsive disorder: the importance of failures in cognitive and behavioural inhibition as candidate endophenotypic markers. Neurosci Biobehav Rev 29: 399–419.
Chamberlain SR, Blackwell AD, Fineberg NA, Robbins TW, Sahakian BJ (2006a). Strategy implementation in obsessive-compulsive disorder and trichotillomania. Psychol Med 36: 91–97.
Chamberlain SR, Del Campo N, Dowson J, Muller U, Clark L, Robbins TW et al (2007a). Atomoxetine improved response inhibition in adults with attention deficit/hyperactivity disorder. Biol Psychiatry 62: 977–984.
Chamberlain SR, Fineberg NA, Blackwell AD, Clark L, Robbins TW, Sahakian BJ (2007b). A neuropsychological comparison of obsessive-compulsive disorder and trichotillomania. Neuropsychologia 45: 654–662.
Chamberlain SR, Fineberg NA, Blackwell AD, Robbins TW, Sahakian BJ (2006b). Motor inhibition and cognitive flexibility in obsessive-compulsive disorder and trichotillomania. Am J Psychiatry 163: 1282–1284.
Chamberlain SR, Fineberg NA, Menzies LA, Blackwell AD, Bullmore ET, Robbins TW et al (2007c). Impaired cognitive flexibility and motor inhibition in unaffected first-degree relatives of patients with obsessive-compulsive disorder. Am J Psychiatry 164: 335–338.
Chamberlain SR, Menzies L (2009). Endophenotypes of obsessive-compulsive disorder: rationale, evidence and future potential. Expert Rev Neurother 9: 1133–1146.
Chamberlain SR, Menzies L, Hampshire A, Suckling J, Fineberg NA, del Campo N et al (2008a). Orbitofrontal dysfunction in patients with obsessive-compulsive disorder and their unaffected relatives. Science 321: 421–422.
Chamberlain SR, Menzies L, Sahakian BJ, Fineberg NA (2007d). Lifting the veil on trichotillomania. Am J Psychiatry 164: 568–574.
Chamberlain SR, Menzies LA, Fineberg NA, Del Campo N, Suckling J, Craig K et al (2008b). Grey matter abnormalities in trichotillomania: morphometric magnetic resonance imaging study. Br J Psychiatry 193: 216–221.
Chamberlain SR, Muller U, Blackwell AD, Clark L, Robbins TW, Sahakian BJ (2006c). Neurochemical modulation of response inhibition and probabilistic learning in humans. Science 311: 861–863.
Chamberlain SR, Muller U, Deakin JB, Corlett PR, Dowson J, Cardinal R et al (2006d). Lack of deleterious effects of buspirone on cognition in healthy male volunteers. J Psychopharmacol 21: 210–215.
Chamberlain SR, Robbins TW, Sahakian BJ (2007e). The neurobiology of attention-deficit/hyperactivity disorder. Biol Psychiatry 61: 1317–1319.
Chamberlain SR, Sahakian BJ (2007). The neuropsychiatry of impulsivity. Curr Opin Psychiatry 20: 255–261.
Chambers MS, Atack JR, Carling RW, Collinson N, Cook SM, Dawson GR et al (2004). An orally bioavailable, functionally selective inverse agonist at the benzodiazepine site of GABAA alpha5 receptors with cognition enhancing properties. J Med Chem 47: 5829–5832.
Chou-Green JM, Holscher TD, Dallman MF, Akana SF (2003). Compulsive behavior in the 5-HT2C receptor knockout mouse. Physiol Behav 78: 641–649.
Clark L, Robbins TW, Ersche KD, Sahakian BJ (2006). Reflection impulsivity in current and former substance users. Biol Psychiatry 60: 515–522.
Clark L, Roiser JP, Cools R, Rubinsztein DC, Sahakian BJ, Robbins TW (2005). Stop signal response inhibition is not modulated by tryptophan depletion or the serotonin transporter polymorphism in healthy volunteers: implications for the 5-HT theory of impulsivity. Psychopharmacology (Berl) 182: 570–578.
Clarke HF, Dalley JW, Crofts HS, Robbins TW, Roberts AC (2004). Cognitive inflexibility after prefrontal serotonin depletion. Science 304: 878–880.
Clarke HF, Walker SC, Crofts HS, Dalley JW, Robbins TW, Roberts AC (2005). Prefrontal serotonin depletion affects reversal learning but not attentional set shifting. J Neurosci 25: 532–538.
Clarke HF, Walker SC, Dalley JW, Robbins TW, Roberts AC (2007). Cognitive inflexibility after prefrontal serotonin depletion is behaviorally and neurochemically specific. Cereb Cortex 17: 18–27.
Cools R (2006). Dopaminergic modulation of cognitive function-implications for L-DOPA treatment in Parkinson's disease. Neurosci Biobehav Rev 30: 1–23.
Cools R, Altamirano L, D'Esposito M (2006). Reversal learning in Parkinson's disease depends on medication status and outcome valence. Neuropsychologia 44: 1663–1673.
Cottrell S, Tilden D, Robinson P, Bae J, Arellano J, Edgell E et al (2008). A modeled economic evaluation comparing atomoxetine with stimulant therapy in the treatment of children with attention-deficit/hyperactivity disorder in the United Kingdom. Value Health 11: 376–388.
Crawford S, Channon S, Robertson MM (2005). Tourette's syndrome: performance on tests of behavioural inhibition, working memory and gambling. J Child Psychol Psychiatry 46: 1327–1336.
Crosbie J, Schachar R (2001). Deficient inhibition as a marker for familial ADHD. Am J Psychiatry 158: 1884–1890.
Denys D, Zohar J, Westenberg HG (2004). The role of dopamine in obsessive-compulsive disorder: preclinical and clinical evidence. J Clin Psychiatry 65 (Suppl 14): 11–17.
Dias R, Robbins TW, Roberts AC (1996). Dissociation in prefrontal cortex of affective and attentional shifts. Nature 380: 69–72.
Evers EA, Cools R, Clark L, van der Veen FM, Jolles J, Sahakian BJ et al (2005). Serotonergic modulation of prefrontal cortex during negative feedback in probabilistic reversal learning. Neuropsychopharmacology 30: 1138–1147.
Fineberg NA, Gale TM (2005). Evidence-based pharmacotherapy of obsessivecompulsive disorder. Int J Neuropsychopharmacol 8: 107–129.
Fineberg NA, Saxena S, Zohar J, Craig KJ (2007a). Obsessive-compulsive disorder: boundary issues. CNS Spectr 12: 359–364, 367–375.
Fineberg NA, Sharma P, Sivakumaran T, Sahakian B, Chamberlain SR (2007b). Does obsessive-compulsive personality disorder belong within the obsessive-compulsive spectrum? CNS Spectr 12: 467–482.
Fineberg NA, Sivakumaran T, Roberts A, Gale T (2005). Adding quetiapine to SRI in treatment-resistant obsessive-compulsive disorder: a randomized controlled treatment study. Int Clin Psychopharmacol 20: 223–226.
Fong T, Kalechstein A, Bernhard B, Rosenthal R, Rugle L (2008). A double-blind, placebo-controlled trial of olanzapine for the treatment of video poker pathological gamblers. Pharmacol Biochem Behav 89: 298–303.
Frank MJ, Moustafa AA, Haughey HM, Curran T, Hutchison KE (2007). Genetic triple dissociation reveals multiple roles for dopamine in reinforcement learning. Proc Natl Acad Sci USA 104: 16311–16316.
Garraux G, Goldfine A, Bohlhalter S, Lerner A, Hanakawa T, Hallett M (2006). Increased midbrain gray matter in Tourette's syndrome. Ann Neurol 59: 381–385.
Gottesman II, Gould TD (2003). The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry 160: 636–645.
Grant JE, Odlaug BL, Potenza MN (2007). Addicted to hair pulling? How an alternate model of trichotillomania may improve treatment outcome. Harv Rev Psychiatry 15: 80–85.
Grant JE, Potenza MN (2006). Compulsive aspects of impulse-control disorders. Psychiatr Clin North Am 29: 539–551.
Hamidovic A, Kang UJ, de Wit H (2008). Effects of low to moderate acute doses of pramipexole on impulsivity and cognition in healthy volunteers. J Clin Psychopharmacol 28: 45–51.
Hampshire A, Owen AM (2006). Fractionating attentional control using event-related fMRI. Cereb Cortex 16: 1679–1689.
Harrison AA, Everitt BJ, Robbins TW (1997). Central 5-HT depletion enhances impulsive responding without affecting the accuracy of attentional performance: interactions with dopaminergic mechanisms. Psychopharmacology (Berl) 133: 329–342.
Hatcher PD, Brown VJ, Tait DS, Bate S, Overend P, Hagan JJ et al (2005). 5-HT6 receptor antagonists improve performance in an attentional set shifting task in rats. Psychopharmacology (Berl) 181: 253–259.
Hollander E, Berlin HA, Bartz J, Anagnostou E, Pallanti S, Simeon D et al (2007a). The impulsive-compulsive spectrum: neurocognitive, functional imaging and treatment findings inform the phenotype. ACNP presentation. Scientific Abstracts ACNP 2007 Annual Meeting, p 50.
Hollander E, Cohen LJ (1996). Impulsivity and Compulsivity. American Psychiatric Press Inc, Washington DC.
Hollander E, DeCaria C, Gully R, Nitescu A, Suckow RF, Gorman JM et al (1991a). Effects of chronic fluoxetine treatment on behavioral and neuroendocrine responses to meta-chlorophenylpiperazine in obsessive-compulsive disorder. Psychiatry Res 36: 1–17.
Hollander E, DeCaria C, Nitescu A, Cooper T, Stover B, Gully R et al (1991b). Noradrenergic function in obsessive-compulsive disorder: behavioral and neuroendocrine responses to clonidine and comparison to healthy controls. Psychiatry Res 37: 161–177.
Hollander E, Kim S, Khanna S, Pallanti S (2007b). Obsessive-compulsive disorder and obsessive-compulsive spectrum disorders: diagnostic and dimensional issues. CNS Spectr 12 (2 Suppl 3): 5–13.
Hollander E, Wong CM (1995). Obsessive-compulsive spectrum disorders. J Clin Psychiatry 56 (Suppl 4): 3–6; discussion 53–5.
Homberg JR, Pattij T, Janssen MC, Ronken E, De Boer SF, Schoffelmeer AN et al (2007). Serotonin transporter deficiency in rats improves inhibitory control but not behavioural flexibility. Eur J Neurosci 26: 2066–2073.
Hornak J, O'Doherty J, Bramham J, Rolls ET, Morris RG, Bullock PR et al (2004). Reward-related reversal learning after surgical excisions in orbito-frontal or dorsolateral prefrontal cortex in humans. J Cogn Neurosci 16: 463–478.
Insel TR, Pickar D (1983). Naloxone administration in obsessive-compulsive disorder: report of two cases. Am J Psychiatry 140: 1219–1220.
Izquierdo A, Newman TK, Higley JD, Murray EA (2007). Genetic modulation of cognitive flexibility and socioemotional behavior in rhesus monkeys. Proc Natl Acad Sci USA 104: 14128–14133.
Joel D (2006). Current animal models of obsessive compulsive disorder: a critical review. Prog Neuropsychopharmacol Biol Psychiatry 30: 374–388.
Kolevzon A, Mathewson KA, Hollander E (2006). Selective serotonin reuptake inhibitors in autism: a review of efficacy and tolerability. J Clin Psychiatry 67: 407–414.
Koob GF, Le Moal M (1997). Drug abuse: hedonic homeostatic dysregulation. Science 278: 52–58.
Krishnan-Sarin S, Reynolds B, Duhig AM, Smith A, Liss T, McFetridge A et al (2007). Behavioral impulsivity predicts treatment outcome in a smoking cessation program for adolescent smokers. Drug Alcohol Depend 88: 79–82.
Lapiz-Bluhm MD, Soto-Pina AE, Hensler JG, Morilak DA (2009). Chronic intermittent cold stress and serotonin depletion induce deficits of reversal learning in an attentional set-shifting test in rats. Psychopharmacology (Berl) 202: 329–341.
Li CS, Chang HL, Hsu YP, Wang HS, Ko NC (2006). Motor response inhibition in children with Tourette's disorder. J Neuropsychiatry Clin Neurosci 18: 417–419.
Lijffijt M, Kenemans JL, Verbaten MN, van Engeland H (2005). A meta-analytic review of stopping performance in attention-deficit/hyperactivity disorder: deficient inhibitory motor control? J Abnorm Psychol 114: 216–222.
Lynd-Balta E, Haber SN (1994). The organization of midbrain projections to the ventral striatum in the primate. Neuroscience 59: 609–623.
Masaki D, Yokoyama C, Kinoshita S, Tsuchida H, Nakatomi Y, Yoshimoto K et al (2006). Relationship between limbic and cortical 5-HT neurotransmission and acquisition and reversal learning in a go/no-go task in rats. Psychopharmacology (Berl) 189: 249–258.
McElroy SL, Nelson EB, Welge JA, Kaehler L, Keck Jr PE (2008). Olanzapine in the treatment of pathological gambling: a negative randomized placebo-controlled trial. J Clin Psychiatry 69: 433–440.
McIntosh AR, Lobaugh NJ (2004). Partial least squares analysis of neuroimaging data: applications and advances. Neuroimage 23 (Suppl 1): S250–S263.
Menzies L, Achard S, Chamberlain SR, Fineberg N, Chen CH, del Campo N et al (2007a). Neurocognitive endophenotypes of obsessive-compulsive disorder. Brain 130 (Pt 12): 3223–3236.
Menzies L, Chamberlain SR, Laird AR, Thelen SM, Sahakian BJ, Bullmore ET (2008a). Integrating evidence from neuroimaging and neuropsychological studies of obsessive-compulsive disorder: The orbitofronto-striatal model revisited. Neurosci Biobehav Rev 32: 525–549.
Menzies L, Williams GB, Chamberlain SR, Ooi C, Fineberg N, Suckling J et al (2008b). White matter abnormalities in patients with obsessive-compulsive disorder and their first-degree relatives. Am J Psychiatry 165: 1308–1315.
Naqvi NH, Rudrauf D, Damasio H, Bechara A (2007). Damage to the insula disrupts addiction to cigarette smoking. Science 315: 531–534.
Park SB, Coull JT, McShane RH, Young AH, Sahakian BJ, Robbins TW et al (1994). Tryptophan depletion in normal volunteers produces selective impairments in learning and memory. Neuropharmacology 33: 575–588.
Passetti F, Dalley JW, Robbins TW (2003). Double dissociation of serotonergic and dopaminergic mechanisms on attentional performance using a rodent five-choice reaction time task. Psychopharmacology (Berl) 165: 136–145.
Pizzagalli DA, Evins AE, Schetter EC, Frank MJ, Pajtas PE, Santesso DL et al (2008). Single dose of a dopamine agonist impairs reinforcement learning in humans: behavioral evidence from a laboratory-based measure of reward responsiveness. Psychopharmacology (Berl) 196: 221–232.
Potenza MN (2007a). Impulsivity and compulsivity in pathological gambling and obsessive-compulsive disorder. Rev Bras Psiquiatr 29: 105–106.
Potenza MN (2007b). To do or not to do? The complexities of addiction, motivation, self-control, and impulsivity. Am J Psychiatry 164: 4–6.
Potenza MN, Leung HC, Blumberg HP, Peterson BS, Fulbright RK, Lacadie CM et al (2003a). An FMRI Stroop task study of ventromedial prefrontal cortical function in pathological gamblers. Am J Psychiatry 160: 1990–1994.
Potenza MN, Steinberg MA, Skudlarski P, Fulbright RK, Lacadie CM, Wilber MK et al (2003b). Gambling urges in pathological gambling: a functional magnetic resonance imaging study. Arch Gen Psychiatry 60: 828–836.
Poyurovsky M, Faragian S, Shabeta A, Kosov A (2008). Comparison of clinical characteristics, co-morbidity and pharmacotherapy in adolescent schizophrenia patients with and without obsessive-compulsive disorder. Psychiatry Res 159: 133–139.
Reuter J, Raedler T, Rose M, Hand I, Glascher J, Buchel C (2005). Pathological gambling is linked to reduced activation of the mesolimbic reward system. Nat Neurosci 8: 147–148.
Robbins TW (2002). The 5-choice serial reaction time task: behavioural pharmacology and functional neurochemistry. Psychopharmacology (Berl) 163: 362–380.
Robbins TW (2007). Shifting and stopping: fronto-striatal substrates, neurochemical modulation and clinical implications. Philos Trans R Soc Lond B Biol Sci 362: 917–932.
Robinson TE, Berridge KC (1993). The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Brain Res Rev 18: 247–291.
Rogers RD, Blackshaw AJ, Middleton HC, Matthews K, Hawtin K, Crowley C et al (1999a). Tryptophan depletion impairs stimulus-reward learning while methylphenidate disrupts attentional control in healthy young adults: implications for the monoaminergic basis of impulsive behaviour. Psychopharmacology (Berl) 146: 482–491.
Rogers RD, Everitt BJ, Baldacchino A, Blackshaw AJ, Swainson R, Wynne K et al (1999b). Dissociable deficits in the decision-making cognition of chronic amphetamine abusers, opiate abusers, patients with focal damage to prefrontal cortex, and tryptophan-depleted normal volunteers: evidence for monoaminergic mechanisms. Neuropsychopharmacology 20: 322–339.
Rubia K, Smith AB, Brammer MJ, Taylor E (2003). Right inferior prefrontal cortex mediates response inhibition while mesial prefrontal cortex is responsible for error detection. Neuroimage 20: 351–358.
Schilman EA, Uylings HB, Galis-de Graaf Y, Joel D, Groenewegen HJ (2008). The orbital cortex in rats topographically projects to central parts of the caudate-putamen complex. Neurosci Lett 432: 40–45.
Schultz W (2002). Getting formal with dopamine and reward. Neuron 36: 241–263.
Seymour B, Daw N, Dayan P, Singer T, Dolan R (2007). Differential encoding of losses and gains in the human striatum. J Neurosci 27: 4826–4831.
Stein DJ, Chamberlain SR, Fineberg N (2006). An A-B-C model of habit disorders: hair-pulling, skin-picking, and other stereotypic conditions. CNS Spectr 11: 824–827.
Stein DJ, Hollander E (1995). Obsessive-compulsive spectrum disorders. J Clin Psychiatry 56: 265–266.
Szeszko PR, Ardekani BA, Ashtari M, Malhotra AK, Robinson DG, Bilder RM et al (2005). White matter abnormalities in obsessive-compulsive disorder: a diffusion tensor imaging study. Arch Gen Psychiatry 62: 782–790.
Talbot PS, Watson DR, Barrett SL, Cooper SJ (2006). Rapid tryptophan depletion improves decision-making cognition in healthy humans without affecting reversal learning or set shifting. Neuropsychopharmacology 31: 1519–1525.
Tsaltas E, Kontis D, Chrysikakou S, Giannou H, Biba A, Pallidi S et al (2005). Reinforced spatial alternation as an animal model of obsessive-compulsive disorder (OCD): investigation of 5-HT2C and 5-HT1D receptor involvement in OCD pathophysiology. Biol Psychiatry 57: 1176–1185.
van der Plasse G, Feenstra MG (2008). Serial reversal learning and acute tryptophan depletion. Behav Brain Res 186: 23–31.
Vertes RP (2004). Differential projections of the infralimbic and prelimbic cortex in the rat. Synapse 51: 32–58.
Volkow ND, Fowler JS, Wang GJ (1999). Imaging studies on the role of dopamine in cocaine reinforcement and addiction in humans. J Psychopharmacol 13: 337–345.
Walker SC, Robbins TW, Roberts AC (2009). Differential contributions of dopamine and serotonin to orbitofrontal cortex function in the marmoset. Cereb Cortex 19: 889–898.
Watkins LH, Sahakian BJ, Robertson MM, Veale DM, Rogers RD, Pickard KM et al (2005). Executive function in Tourette's syndrome and obsessive-compulsive disorder. Psychol Med 35: 571–582.
Westenberg HG, Fineberg NA, Denys D (2007). Neurobiology of obsessive-compulsive disorder: serotonin and beyond. CNS Spectr 12 (2 Suppl 3): 14–27.
Winstanley CA, Chudasama Y, Dalley JW, Theobald DE, Glennon JC, Robbins TW (2003). Intra-prefrontal 8-OH-DPAT and M100907 improve visuospatial attention and decrease impulsivity on the five-choice serial reaction time task in rats. Psychopharmacology (Berl) 167: 304–314.
Winstanley CA, Eagle DM, Robbins TW (2006). Behavioral models of impulsivity in relation to ADHD: translation between clinical and preclinical studies. Clin Psychol Rev 26: 379–395.
Winstanley CA, Theobald DE, Dalley JW, Glennon JC, Robbins TW (2004). 5-HT2A and 5-HT2C receptor antagonists have opposing effects on a measure of impulsivity: interactions with global 5-HT depletion. Psychopharmacology (Berl) 176: 376–385.
Wise RA (2002). Brain reward circuitry: insights from unsensed incentives. Neuron 36: 229–240.
World Health Organisation (1992). International Classification of Diseases, 10th edition (ICD-10). World Health Organisation, Geneva.
Yucel M, Harrison BJ, Wood SJ, Fornito A, Wellard RM, Pujol J et al (2007). Functional and biochemical alterations of the medial frontal cortex in obsessive-compulsive disorder. Arch Gen Psychiatry 64: 946–955.
Zack M, Poulos CX (2007). A D2 antagonist enhances the rewarding and priming effects of a gambling episode in pathological gamblers. Neuropsychopharmacology 32: 1678–1686.
Zohar J, Insel TR, Zohar-Kadouch RC, Hill JL, Murphy DL (1988). Serotonergic responsivity in obsessive-compulsive disorder. Effects of chronic clomipramine treatment. Arch Gen Psychiatry 45: 167–172.
Acknowledgements
Dr Fineberg has consulted for Lundbeck, Glaxo-Smith Kline, Servier, and Bristol Myers Squibb; has received research support from Lundbeck, Glaxo-SmithKline, Astra Zeneca, Wellcome; has received honoraria and support to lecture at scientific meetings from Janssen, Jazz, Lundbeck, Servier, Astra Zeneca, Wyeth. Dr Potenza consults for and has advised to Boehringer Ingelheim; has consulted for and has financial interests in Somaxon; has received research support from the National Institutes of Health, Veteran's Administration, Mohegan Sun Casino, the National Center for Responsible Gambling and the Institute for Research on Gambling Disorders, and Glaxo-SmithKline, Forest Laboratories, Ortho-McNeil and Oy-Control/Biotie pharmaceuticals; has participated in surveys, mailings, or telephone consultations related to drug addiction, ICDs or other health topics; has consulted for law offices and the federal public defender's office in issues related to ICDs and drug addiction; has performed grant reviews for the National Institutes of Health and other agencies; has given academic lectures in grand rounds, CME events, and other clinical or scientific venues; has guest-edited sections of journals; has generated books or book chapters for publishers of mental health texts; and provides clinical care in the Connecticut Department of Mental Health and Addiction Services Problem Gambling Services Program. Dr Chamberlain consults for Cambridge Cognition, Shire, and P1Vital. Dr Menzies has received financial compensation resulting from the transfer of a technology not relating to the subject matter of this article between Cambridge Enterprise Limited, University of Cambridge, Cambridge, UK, and Cypress Bioscience, Inc, San Diego. Dr Bechara receives royalties from PAR, Inc. Dr Sahakian holds shares in CeNeS; has consulted for Cambridge Cognition, Novartis, Shire, GlaxoSmithKline, and Lilly; and has received honoraria for grand rounds in psychiatry at Massachusetts General Hospital (CME credits) and for speaking at the International Conference on Cognitive Dysfunction in Schizophrenia and Mood Disorders (2007). Dr Robbins consults for Cambridge Cognition, E. Lilly, GlaxoSmithKline, and Allon Therapeutics. Dr Bullmore is an employee of GlaxoSmithKline (50%) and the University of Cambridge (50%) and a shareholder in GlaxoSmithKline. Dr Bullmore has received financial compensation resulting from the transfer of a technology not relating to the subject matter of this article between Cambridge Enterprise Limited, University of Cambridge, Cambridge, UK, and Cypress Bioscience, Inc, San Diego. Dr Hollander has consulted to Somaxon, Neuropharm, Transcept, and Nastech. Dr Hollander has consulted to law offices and testified in the Mirapex Product Liability case. He has received research support from the National Institutes of Health, Orphan Products Division of the Food and Drug Administration, National Alliance for Research in Schizophrenia and Affective Disorders, Autism Speaks, the Seaver Foundation, and Solvay, Oy Contral, and Somaxon. This work was supported in part by a Wellcome Trust Programme Grant (076274/Z/04/Z) to Dr Robbins, Dr Sahakian, BJ Everitt, and AC Roberts. The Behavioural and Clinical Neuroscience Institute is supported by a joint award from the Medical Research Council (MRC) and Wellcome Trust (G001354). Supported by the National Alliance for Research on Schizophrenia and Depression (RG37920 Distinguished Investigator Award to Dr Bullmore), the Harnett Fund and James Baird Fund (University of Cambridge) and the University of Cambridge School of Clinical Medicine, (MB/PhD studentship to Dr Menzies), and the Medical Research Council (MB/PhD studentship to Dr Chamberlain). Dr Bechara receives grant support from the National Institutes on Health (NIDA R01 DA023051, DA11779, DA12487, and DA1670), (NINDS P01 NS019632), and the National Science Foundation (NSF IIS 04-42586). Dr Potenza receives grant support from the National Institutes of Health (R01 s DA019039, DA020908, DA015757, DA020709; R37 DA15969; RL1 AA017539; P50 s DA09241, AA12870, AA015632), the VA (VISN1 MIRECC and REAP), and Women's Health Research at Yale. Dr Robbins consults for pfizer, Dr Menzies has received honoraria for presenting at the 8th Annual conference on Research of psychopathology and for work on the UK Government Foresight Project on mental capital and wellbeing.
Author information
Authors and Affiliations
Corresponding author
Additional information
DISCLOSURE
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Fineberg, N., Potenza, M., Chamberlain, S. et al. Probing Compulsive and Impulsive Behaviors, from Animal Models to Endophenotypes: A Narrative Review. Neuropsychopharmacol 35, 591–604 (2010). https://doi.org/10.1038/npp.2009.185
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2009.185
Keywords
This article is cited by
-
Repeated Δ-9-Tetrahydrocannabinol administration dose dependently increases stablished schedule-induced drinking
Psychopharmacology (2024)
-
Chronic ∆-9-tetrahydrocannabinol administration delays acquisition of schedule-induced drinking in rats and retains long-lasting effects
Psychopharmacology (2022)
-
A systematic review of resting-state functional connectivity in obesity: Refining current neurobiological frameworks and methodological considerations moving forward
Reviews in Endocrine and Metabolic Disorders (2022)
-
Brain 5-HT2A receptor binding and its neural network related to behavioral inhibition system
Brain Imaging and Behavior (2022)
-
Memantine treatment does not affect compulsive behavior or frontostriatal connectivity in an adolescent rat model for quinpirole-induced compulsive checking behavior
Psychopharmacology (2022)