Abstract
Visuo-spatial deficits are the most consistently reported cognitive abnormalities in Parkinson's disease (PD), and they are frequently associated to motor symptoms in the early stages of the disease when dopamine loss is moderate and still restricted to the caudate–putamen. The metabotropic glutamate receptor 5 (mGluR5) antagonist, 2-methyl-6-(phenylethynyl)-pyridine (MPEP), has beneficial effects on motor symptoms in animal models of PD. However, the effects of MPEP on the cognitive deficits of the disease have never been investigated. Thus, the purpose of this study was to explore its therapeutic potentials by investigating its effects on the visuo-spatial deficits induced by 6-hydroxydopamine (6-OHDA) lesions of dorsal striatum in CD1 mice. The results demonstrated that systemic injections of MPEP (6, 12, and 24 mg/kg, i.p.) impair visuo-spatial discrimination in intact mice at high concentrations, whereas lower doses (1.5 and 3 mg/kg, i.p.) were void of effects. Nevertheless, when an ineffective dose (MPEP 3 mg/kg) was injected, either acutely or subchronically (8 days), it antagonized the visuo-spatial discrimination deficit induced by bilateral dopamine lesion of the striatum. Furthermore, the same treatment increased contralateral turning induced by L-DOPA in mice bearing unilateral 6-OHDA lesion. These results confirm the therapeutic potential of mGluR5 blockade on motor symptoms induced by reduced striatal dopamine function. Further, they demonstrate that mGluR5 blockade may also have beneficial effects on cognitive deficits induced by dopamine depletion.
Similar content being viewed by others
INTRODUCTION
It is widely recognized that motor symptoms are accompanied by cognitive deficits in Parkinsonian patients even at the early stages of the disease, when dopamine (DA) depletion is restricted to the striatal complex (Owen et al, 1997; Pillon et al, 1997, 1998). On the basis of recent evidence, visuo-spatial memory impairments seem to be the most constantly reported cognitive deficit in Parkinson's disease (PD) patients (Berger et al, 2004; Cools et al, 2002, 2007; Giraudo et al, 1997; Lewis et al, 2003; Owen et al, 1998; Pillon et al, 1997, 1998). Consistently, extensive DA lesions, obtained through either medial forebrain bundle or dorsal striatum 6-hydroxydopamine (6-OHDA) administrations, have been found to impair memory in the spatial version of the Morris water maze in rats (Miyoshi et al, 2002; Mura and Feldon, 2003; Whishaw and Dunnett, 1985). Furthermore, it has been recently shown that partial bilateral DA depletion of the dorsal striatum impairs spatial discrimination in the object–place association task in mice, and that this effect is specific for spatial information (De Leonibus et al, 2007), thus providing an useful animal model of cognitive deficit in the early stages of PD.
On the basis of current theories, which consider the imbalance between DA and glutamate in the basal ganglia (BG) one of the major consequence of PD-related pathogenic cascade (Breysse et al, 2003; Greenamyre and O'Brien, 1991; Klockgether et al, 1991), metabotropic glutamate receptors (mGluRs) have been suggested as suitable targets to modulate parkinsonian motor symptoms. Accordingly, mGluR5 blockade ameliorates motor abnormalities induced by lesions of the nigrostriatal dopaminergic system, or by dopaminergic receptor antagonists in animal models of PD (Breysse et al, 2002; Coccurello et al, 2004; Dekundy et al, 2006; Domenici et al, 2005; Ossowska et al, 2001, 2002, 2005; Oueslati et al, 2005; Phillips et al, 2006; Popoli et al, 2001; Turle-Lorenzo et al, 2005). However, to our knowledge, none of the studies in the literature investigated the possible therapeutic potentials of mGluR5 antagonists in the treatment of the cognitive symptoms of the disease. It is worth noting in this regard, that experimental findings using pharmacological approaches or mGluR5 KO mice demonstrate an involvement of mGluR5 in neural plasticity, as well as in learning and memory processes (Ballard et al, 2005; Campbell et al, 2004; Gravius et al, 2005; Gubellini et al, 2003; Homayoun et al, 2004; Lu et al, 1997; Manahan-Vaughan and Braunewell, 2005; Simonyi et al, 2005), suggesting that mGluR5 blockade could impair learning and memory in intact animals. Nevertheless, glutamate overactivity as a consequence of striatal DA depletion, might have a causal role in the cognitive deficits of Parkinson's patients; in addition to motor dysfunction. Thus, mGluR5 blockade might improve, rather than impair, spatial memory in DA lesioned animals. Therefore, the present study was undertaken to determine whether the beneficial effects of mGluR5 blockade apply to both motor and cognitive deficits observed in animal models of PD.
For this purpose, we first tested the effects of systemic acute injection of different doses of 2-methyl-6-(phenylethynyl)-pyridine (MPEP), a selective mGluR5 antagonist, on naïve mice in the object–place association task (Lenck-Santini et al, 2005; Roullet et al, 2001). Afterward, we selected a dose of MPEP (3 mg/kg) that was void of any effect on naïve animals and that in previous studies was demonstrated to reverse motor deficits in an animal model of PD (Breysse et al, 2002) and tested its acute or subchronic (8 days) effects on the spatial deficit induced by bilateral dorsal striatal 6-OHDA lesions. Finally, we tested the effects of acute and subchronic (8 days) systemic injections of MPEP (3 mg/kg) on contralateral turning induced by the DA precursor L-DOPA on animals unilaterally injected with 6-OHDA in the caudate–putamen.
MATERIALS AND METHODS
Animals
The subjects were adult CD1 male outbred mice obtained from Charles River (Calco, Italy). Upon arrival mice were housed in groups of 12 in standard breeding cages (46 × 26 × 21.8 cm), placed in a rearing room at a constant temperature (22±1°C) and maintained on a 12 h light/dark cycle with food and water available ad libitum. At the time of surgery they were 8–10 weeks old. Every possible effort was made to minimize animal suffering, and all procedures were in strict accordance with the European Communities Council directives (86/609/EEC) and regulations on the use of animals in research and NIH guidelines on animal care.
Dopamine Lesion
Mice were anaesthetized with i.p. injection of chloral hydrate (500 mg/kg; Fluka Co., Milan, Italy) and placed in a stereotaxic apparatus (David Kopf Instruments, Tujunga, CA, USA) with mouse adaptor and lateral ear bars. The head skin was cut longitudinally and an injector (0.09 mm internal and 0.20 mm external diameter), connected with a polyethylene tubing to a 2 μl Hamilton syringe, was lowered bilaterally into the dorsal striatum. The following stereotaxic coordinates were used: +0.3 mm anterior to bregma, ±2 mm lateral to midline, −3.0 mm ventral from the skull surface, according to Franklin and Paxinos mouse brain atlas (1997). In the experiments 2 and 3 lesioned animals (Les) were bilaterally injected with 6-OHDA hydrochloride (0.3 μl per side of 1.5 μg/0.1 μl solution containing Na-metabisulfite 0.1 M; Sigma, Milan, Italy), although the sham controls were bilaterally injected with a corresponding volume of saline (NaCl 9%). In experiment 4, the same procedure was used but mice were injected unilaterally with 6-OHDA whereas the contralateral side was injected with saline solution. To protect noradrenergic terminals mice were given desipramine (35 mg/kg; Sigma). Mice were then allowed to recover from the operation for at least 10 days.
Behavioral Apparati and Procedures
Experiments 1, 2, and 3: spatial memory studies
The apparatus (Figure 1) was a circular open field (for a detailed description refer to Roullet et al, 2001). The behavioral procedure was similar to that previously described (Roullet et al, 2001). Mice were individually submitted to seven consecutive, 6-min sessions. Intersession interval was 3 min. During session 1 (S1), mice were placed into the empty open field. In sessions 2–4 (S2–S4), five objects were positioned into the open field as shown in Figure 1 (habituation phase). During the spatial test session (S5) the objects configuration was changed by displacing two of the objects (Figure 1). After spatial test session the animals were submitted to two additional sessions: S6 and S7. In session 6, the configuration of the objects was kept unchanged as compared to S5. In the last session (session 7), one of the familiar objects was replaced by a new object. In the dose–response study (experiment 1) the last two sessions (S6 and S7) were omitted.
Drug injections (vehicle or MPEP) were performed 30 min before the first training session (S1). For the subchronic experiment (experiment 3), animals received daily injection of MPEP or vehicle for 7 days, and immediately after they were returned to their home cage. On the eighth day 30 min after the injection they were submitted to the spatial task.
Experiment 4: rotational study
The apparatus was a vase with a diameter of 18 and 18 cm high. Approximately 7 days after surgery animals were injected with 4 mg/kg of amphetamine, placed in the rotameter and screened for the following 60 min. Rotation was defined as a 360° rotation of the body axes in the same direction. Only those animals that made more than 200 ipsilateral turns, and showed a ratio ((number of ipsilateral rotations/total number of rotations) × 100) of ipsilateral rotations greater than 70% were included in the experiment. Approximately 7 days after screening, the animals received one injection of vehicle or MPEP (3 mg/kg) per day for 8 consecutive days. On the first (acute) and on the eighth (subchronic) day immediately after MPEP injection, animals were placed in the rotameter for 30 min (habituation). After this habituation phase they were injected with saline or L-DOPA (25 mg/kg) and benserazide (20 mg/kg, 30 min before L-DOPA) and tested for further 40 min. Turning behavior was recorded on a videotape and screened off line by an observer blind to the treatments. The effects of injections two through six were not recorded, and after the injection the animals were immediately returned to their home cages.
Experimental Groups
Experiment 1: MPEP dose–response on spatial discrimination in the object–place association task
Six groups of naïve animals were used. Each group was injected (i.p.) with one of the doses of MPEP (vehicle, 1.5, 3, 6, 12, 24 mg/kg) 30 min before testing.
Experiment 2: acute MPEP administration in the object–place association task, in 6-OHDA lesioned mice
Lesioned and sham animals were divided into two subgroups approximately 15 days after surgery. The two groups were treated with either vehicle or 3 mg/kg MPEP 30 min before the visuo-spatial task.
Experiment 3: subchronic MPEP administrations in the object–place association task, in 6-OHDA lesioned mice
Lesioned and sham animals were divided into two subgroups approximately 15 days after surgery. The two groups were treated with either vehicle or 3 mg/kg MPEP for 8 consecutive days. On the eighth day, 30 min after the injection of vehicle or MPEP the animals were submitted to the visuo-spatial task.
Experiment 4: acute and subchronic MPEP administrations on rotations induced by L-DOPA in unilateral 6-OHDA lesioned animals
After the screening with amphetamine, mice were divided into four groups: 1. saline pretreated (from day 1 to day 8) and challenged with vehicle on days 1 and 8; 2. saline pretreated (from day 1 to day 8) and challenged with L-DOPA on days 1 and 8; 3. MPEP pretreated (from day 1 to day 8) and challenged with vehicle on days 1 and 8; 4. MPEP pretreated (from day 1 to day 8) and challenged with L-DOPA on days 1 and 8.
Lesion Verification
To assess striatal DA levels in lesioned and sham animals (experiments 2 and 3), biochemical analyses were performed ex vivo on tissue samples. Mice were killed and the brain frozen at −10°C before punching. Punches were obtained from brain slices (frontal sections) no thicker than 1 mm. Stainless steel tubes 1 mm internal diameter were used to punch the dorsal striatum. DA was determined by means of reverse high-performance liquid chromatography (HPLC) coupled with electrochemical detection. Frozen samples were weighed and homogenized in 150 μl of HClO4 (75 mM). The homogenates were centrifuged at 14 000 rpm for 20 min at 4°C. Aliquots of the supernatant were transferred in the HPLC system. DA and NE levels were determined simultaneously using an HPLC coupled with electrochemical detection (Alexys 100 LC-EC; Antec Leyden, Alfatech, Italy). Electrochemical detection was accomplished using an amperometric detector with a glassy carbon working electrode (VT-03 flow cell, 3 mm GC WE) and a Ag/AgCl reference electrode (ISAAC) at a potential of +600 mV. The method sensitivity was set at 20 nA. Separation was achieved on a Reprosil-Pur 120 C18-AQ-5UM column (150 × 4 mm) protected by guard column (10 × 4 mm) with the same feature (Chebios, Roma, Italy). The flow rate was 1.2 ml/min. The mobile phase consisted of 3% acetonitrile in 0.1 M Na-phosphate buffer, pH 3, 0.1 mM Na2EDTA, 4 mM KCl, and 0.1 mM sodium 1-heptanesulfonate (Sigma). Tissue levels of DA and noradrenaline (NE; pg/mg wet weight) were used for statistical analyses.
Data Collection and Statistics
Data collection was performed using video recordings (for details see Roullet et al, 2001). In all sessions, locomotor activity was recorded by counting the number of sector crossings. From sessions 2 to 7, object exploration was evaluated on the basis of the mean time spent by the animal in contact with the different objects. A contact was defined as the snout of the subject actually touching an object. Habituation to the objects was assessed by averaging the duration of contacts with the five objects during sessions 2, 3, and 4 in each group. In sessions 4 and 5, the exploration time was considered also as the mean time of exploration for the two object categories: displaced object (DO) and nondisplaced object (NDO). The animals' ability to selectively react to the spatial change was analyzed by calculating the spatial re-exploration index (DO (S5)−DO (S4)=DO and NDO (S5)−NDO (S4)=NDO). Finally, in session 7, a NDO was substituted with a new one in the same location. In sessions 6 and 7, the exploration time was considered as the mean time of exploration of the two object categories: substituted object (SO) and nonsubstituted object (NSO). The animals' ability to selectively react to the nonspatial change (novel object) was analyzed by calculating the nonspatial re-exploration index (SO (S7)−SO (S6)=SO and NSO (S7)−NSO (S6)=NSO).
The effects of MPEP treatment on the variable measured in the visuo-spatial task (experiment 1) were analyzed by using two-way ANOVA for repeated measure, with MPEP doses (six levels: vehicle, 1.5, 3, 6, 12, 24 mg/kg) as the between factor. The effects of lesions on DA and NE tissue levels were analyzed by using a one-way ANOVA, lesion (two levels: sham and lesion) as between factors. The effects of acute or subchronic (experiment 4) treatment with MPEP in the 6-OHDA lesioned animals on the rotations induced by saline or L-DOPA were analyzed by using a four-way ANOVA for repeated measure with MPEP dose (two levels: vehicle and 3 mg/kg) and L-DOPA (two levels: vehicle and L-DOPA) as between factors, days of treatment (two levels: day 1 and day 8), and direction of rotation (two levels: ipsilateral and contralateral) as repeated measures. Tukey honestly significant difference post-hoc analysis was used when appropriate.
RESULTS
Experiment 1: Effects of MPEP Administrations on Spatial Discrimination in the Object–Place Association Task
Table 1 shows the mean number of sector crossing during all sessions and the mean time of objects exploration during the habituation phase for animals treated with the different doses of MPEP. All groups progressively reduced locomotor activity in a similar way over the consecutive sessions (main effect of session (F4,240=299.632; p<0.05)). Furthermore, the ANOVA revealed a significant interaction between dose and session (F20,240=1.842; p<0.05). The post hoc analysis showed a reduction (p<0.05) in locomotor activity from S1 to S5, but no differences among groups in any of the sessions.
Independently on the dose of MPEP, the animals showed a similar pattern of objects exploration during the habituation phase (from S2 to S4 in Table 1), namely a high level of exploration in session 2, and a progressive reduction in the following sessions (main effect of session (F2,120=200.573; p<0.05)). Systemic administration of MPEP affected the pattern of objects exploration in a dose dependent manner (main effect of dose (F5,60=8.509; p<0.05), interaction between MPEP dose and sessions (F10,120=2.714; p<0.05)). This effect was mainly due to the lowest dose of MPEP (1.5 mg/kg), which increased (p<0.05) objects exploration in all three sessions, and to a reduction (p<0.05) in objects exploration in the group injected with the highest dose of MPEP in session 1 (Table 1), as compared to vehicle injected animals.
Figure 2 illustrates the effect of systemic injection of MPEP on the spatial re-exploration index after objects displacement. Vehicle injected animals selectively re-explored the DOs far more than the NDOs, thus demonstrating that they were able to discriminate and selectively react to the spatial change. Acute MPEP injections impaired spatial discrimination at the two highest doses. Mice injected with the low doses or the vehicle showed intact spatial discrimination by differentially exploring the two object categories. The ANOVA revealed a significant main effect of object category (F1,60=67.92; p<0.05) and an interaction between object category and MPEP doses (F5,60=2.679; p<0.05).
Effects of systemic acute pretraining injection of 2-methyl-6-(phenylethynyl)-pyridine (MPEP; 0, 1.5, 3, 6, 12, 24 mg/kg, i.p.) on animal's ability to react to a spatial novelty. The histograms illustrate the mean time (s±SEM) spent exploring displaced object (DO) and nondisplaced object (NDO) in S5 minus the time spent exploring the same object category in S4, spatial re-exploration index. (*) p<0.05 DO vs NDO, within treatment.
Experiments 2 and 3: Effects of Acute and Subchronic MPEP Administrations on Spatial Discrimination in 6-OHDA Lesioned Mice
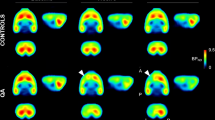
Lesion verification
The biochemical analysis, performed in the sham and the lesioned animals tested in the behavioral experiments, revealed comparable levels of DA depletion in the two lesioned groups as compared to their sham controls. The reduction in DA levels observed in 6-OHDA lesioned groups being approximately 50% of tissue levels in controls mice (sham=8792±520.6 pg/mg tissue; lesioned=4776.5±376.8 pg/mg tissue). One-way ANOVA for repeated measure revealed in both experiments only an effect of the lesion (F1,30=61.7; p<0.05; F1,44=19.474; p<0.05). On the contrary, striatal tissue levels of NE did not differ in lesioned compared with sham animals (F1,51=1.943; p=NS; 6-OHDA lesioned=179±35 pg/mg tissue; sham=249±35 pg/mg tissue).
Experiment 2: Effects of acute administration of MPEP on the spatial deficit induced by bilateral dorsal striatal 6-OHDA lesions
On the basis of dose–response experiment to test the effects of the mGluR5 antagonist in lesioned animals we chose the dose of 3 mg/kg. Table 2 reports the number of sectors crossing in all sessions and the mean time of objects exploration during the habituation phase for sham and lesioned animals pretreated with either vehicle or MPEP (3 mg/kg) 30 min before S1. All groups progressively reduced locomotor activity across sessions (main effect sessions (F6,192=131.933; p<0.05)). Although there was a slight difference in the pattern of locomotor activity across sessions between the different groups (MPEP × lesion × sessions interaction (F6,192=2.732; p<0.05)), post hoc analysis revealed a significant reduction of the locomotor activity in all groups and no significant differences among groups in the different sessions (Table 2). Similarly, all groups progressively reduced objects exploration in a similar way across sessions (main effect of session (F2,64=153.548; p<0.05)).
Figure 3a represents the spatial re-exploration indexes for all groups. As expected, sham animals re-explored DO more than NDO, independent of the pretreatment, thus confirming the results obtained in naïve animals (experiment 1) indicating that acute injection of 3 mg/kg of MPEP does not affect spatial discrimination. On the contrary, 6-OHDA lesioned animals re-explored the two object categories for a similar amount of time, thus demonstrating an impairing effect of the lesion on spatial discrimination. However, pretreating lesioned animals with MPEP re-established the spatial discrimination ability, as shown by the selective re-exploration of DO as compared to NDO in the lesioned group pretreated with 3 mg/kg of MPEP. The ANOVA revealed a significant main effect of the object category (F1,32=49.444; p<0.05) and that the lesion effect almost approached statistical significance (F1,32=3.437; p=0.07).
Effects of acute vehicle or 2-methyl-6-(phenylethynyl)-pyridine (MPEP; 3 mg/kg) administrations in sham and 6-hydroxydopamine (6-OHDA) lesioned animals on their ability to react to a spatial novelty in S5 and to a novel object in S7. (a) The histograms illustrate the mean time (s±SEM) spent exploring displaced object (DO) and nondisplaced object (NDO) in S5 minus the time spent exploring the same object category in S4, spatial re-exploration index. (*) p<0.05 DO vs NDO, within group. (b) The histograms illustrate the mean time (s±SEM) spent exploring substituted object (SO) and nonsubstituted object (NSO) in S7 minus the time spent exploring the same object category in S6, nonspatial re-exploration index. (*) p<0.05 SO vs NSO, within group.
Figure 3b represents the re-exploration index for the SO and theNSO after vehicle and MPEP injections in sham and lesioned groups. 6-OHDA lesions did not affect the ability of the animals to detect and react to the novel object. All groups explored the new object much more than the familiar ones (main effect of object category (F1,32=51.139; p<0.05)). The post hoc comparisons confirmed that sham animals re-explored the SO significantly more than NSO independently on the pretreatment. Lesioned animals also re-explored SO more than NSO, however, when pretreated with MPEP a reduction in SO re-exploration index was observed.
Experiment 3: Effects of subchronic MPEP administrations on the spatial deficit induced by bilateral dorsal striatal 6-OHDA lesions
Table 2 reports the number of sectors crossing during all sessions and the mean time of objects exploration during the habituation phase for sham and lesioned animals pretreated with vehicle or MPEP (3 mg/kg) for 7 days and challenged with either saline or MPEP (3 mg/kg) 30 min before S1. Also in this case neither the lesion nor the pretreatment affected the pattern of sectors crossing (main effect of session (F6,282=167.629; p<0.05) and session × lesion interaction (F6,282=3.343; p<0.05)). The post hoc analysis confirmed that all groups reduced the number of sector crossings across sessions (p<0.05) and that there were no differences among groups.
Similarly, all groups reduced objects exploration (Table 2) across sessions (main effect of session (F2,94=203.807; p<0.05), session × lesion interaction (F2,94=6.768; p<0.05) and session × MPEP dose interaction (F2,94=4.913; p<0.05)). The post hoc analysis confirmed that there were no significant differences among groups.
Figure 4a shows the spatial re-exploration index for all groups. Sham animals showed a clear preference for DOs as compared to NDOs. MPEP subchronic treatment did not affect the mice ability to selectively re-explore the DO. Lesioned animals were once again impaired in DO re-exploration. On the contrary, lesioned mice, subchronically administered with MPEP demonstrated higher levels of re-exploration of DO as compared to NDO, thus demonstrating a recovery of the spatial discrimination deficit induced by the lesion, similar to that observed after acute treatment. Three-way ANOVA revealed a significant main effect of the object category (F1,47=46.149; p<0.05) and of object category × MPEP dose (F1,47=4.372; p<0.05). The post hoc analyses revealed a significant difference in the re-exploration levels of the two object categories only for the sham groups independently of the treatment and in the lesioned animals pretreated with MPEP. No significant difference was found in the lesioned animals pretreated with vehicle.
Effects of subchronic administrations (8 days) of vehicle or 2-methyl-6-(phenylethynyl)-pyridine (MPEP; 3 mg/kg) in sham or 6-hydroxydopamine (6-OHDA) lesioned animals on their ability to react to a spatial novelty in S5 and to a novel object in S7. (a) The histograms illustrate the mean time (s±SEM) spent exploring displaced object (DO) and nondisplaced object (NDO) in S5 minus the time spent exploring the same object category in S4, spatial re-exploration index. (*) p<0.05 DO vs NDO, within group. (b) The histograms illustrate the mean time (s±SEM) spent exploring substituted object (SO) and nonsubstituted object (NSO) in S7 minus the time spent exploring the same object category in S6, nonspatial re-exploration index. (*) p<0.05 SO vs NSO, within group.
As illustrated in Figure 4b, all groups re-explored SO more than NSO (main effect of object category (F1,47=123.624; p<0.05)). Although, the interaction between MPEP dose × object category approached statistical significance (F1,47=5.179; p=0.05), post hoc analysis demonstrated that the difference between SO and NSO was significant in all groups, and there were no significant differences between groups in the re-exploration of any of the object categories.
Experiment 4: Effects of Acute and Subchronic MPEP Administrations on Rotational Behavior Induced by L-DOPA in Unilateral 6-OHDA Lesioned Animals
Injection of D-amphetamine (4 mg/kg) induced a net preference for rotations ipsilateral to the lesioned site (rotation direction (F1,42=140.442; p<0.05)), in the animals subsequently assigned to one of the four experimental groups. The mean ipsilateral rotation±SEM in 60 min being 554.71±39.6 (turns per 40 min), whereas the mean contralateral rotation reached 60.5±8.7. The experimental groups in the subsequent experiments were equated for rotational behavior induced by amphetamine.
Figure 5 illustrates the effects of acute (day 1) and subchronic (day 8) administrations of MPEP on rotational behavior induced by L-DOPA 25 mg/kg in unilateral 6-OHDA lesioned animals. As shown in Figure 5 L-DOPA treatment induced a preferential contralateral turning on day 1 (vehicle/L-DOPA group). This effect diminished across test sessions (day 8). Pretreatment with MPEP increased L-DOPA induced contralateral rotations after a single injection as well as after repeated administrations, the effect being more robust after 8 days of treatment. The three-way ANOVA for repeated measure, demonstrated that the effect of the direction of rotation (F1,42=3.964; p=0.053) and the interaction between MPEP dose × L-DOPA × day (F1,42=3.905; p=0.054) approached statistical significance. Furthermore, it revealed a significant effect of the interaction L-DOPA × direction of the rotation (F1,42=18.779; p<0.05), MPEP × day × direction of the rotation (F1,42=4.843; p<0.05) and between MPEP × L-DOPA × day × direction of the rotation (F1,42=4.624; p<0.05). The post hoc analysis confirmed that, on day 1, L-DOPA treatment increased contralateral as compared to ipsilateral rotations, independently on whether the animals where pretreated with vehicle or MPEP. This effect habituated across testing days when the animals were preinjected with vehicle, but it dramatically increased when the animals were subchronically (day 8) treated with MPEP.
Effects of acute (day 1) and subchronic administrations (day 8) of vehicle or 2-methyl-6-(phenylethynyl)-pyridine (MPEP; 3 mg/kg) on ipsilateral and contralateral rotations induced by L-DOPA or vehicle in 6-hydroxydopamine (6-OHDA) injected lesioned mice. (*) p<0.05 ipsilateral vs contralateral, within treatment, within day and within pretreatment; ($) p<0.05 vehicle vs MPEP, within treatment, within day and within direction of the rotation; (#) p<0.05 day 1 vs day 8, within pretreatment, within treatment and within direction of the rotation.
DISCUSSION
In this study we investigated whether the mGluR5 antagonist MPEP, which has been recently found to reverse motor symptoms in animal models of PD, could also improve the spatial memory deficit induced by DA loss in the striatum. The results confirmed previous findings that mild (about 50%) striatal DA depletion impairs animals' ability to discriminate a spatial change, but does not affect their ability to discriminate a new object (De Leonibus et al, 2007). Furthermore, it was also found that acute injections of high doses of MPEP impair spatial discrimination in intact animals. However, the most intriguing finding of this study was that MPEP at a low dose, though ineffective in sham animals, was able to reverse the spatial discrimination deficit induced by 6-OHDA lesions of the striatum. Interestingly, the same dose of MPEP that improved the visuo-spatial memory deficits in this model potentiated contralateral turning induced by L-DOPA, thereby confirming its antiparkinsonian action.
Acute systemic injections of high doses of MPEP impaired spatial discrimination in the object–place association task. The impairment was not secondary to motor or object exploration deficits, as doses of the drug which affected locomotion or objects exploration (ie 1.5 mg/kg) did not affect spatial discrimination. These data are consistent with previous findings in the literature showing that low doses of MPEP have no effect on spatial learning and memory (Ballard et al, 2005; Campbell et al, 2004; Homayoun et al, 2004; Manahan-Vaughan and Braunewell, 2005; Naie and Manahan-Vaughan, 2004; Petersen et al, 2002; Steckler et al, 2005).
As any potential antiparkinsonian drug needs to be repeatedly administered, we also tested the effects of subchronic injections of MPEP on the same task. Interestingly, lesioned animals treated with MPEP for 7 days and challenged with a further dose of the drug before testing, could discriminate the spatial change, thus demonstrating that the acute effect induced by MPEP in 6-OHDA lesioned mice is maintained after repeated injections. Furthermore, we report that repeated administration of MPEP 3 mg/kg did not affect spatial or novel object discrimination in sham animals. As MPEP has recently been investigated in studies related to anxiety, depression, and psychotic disorders (Belozertseva et al, 2007; Homayoun et al, 2004; Pilc et al, 2002), the results of this experiment, by showing no major cognitive impairments after repeated systemic injections of the drug, provide experimental evidence in favor of future clinical investigation. However, the route of administration is a critical point as repeated intracerebroventricular injections of MPEP have been reported to impair neural plasticity and spatial memory in naïve animals (Manahan-Vaughan and Braunewell, 2005; Naie and Manahan-Vaughan, 2004). These opposite results after systemic or brain focal administration of the drug could be due to the low solubility of MPEP compound. Intracerebral infusion of MPEP solution at low pH may produce deleterious effects on behavior that would not be observed after systemic injections.
The effects of mGluR5 blockade on spatial discrimination in DA lesioned animals cannot be attributed to a general enhancing effect on an animal's ability to detect or to react to novel information. Indeed, acute administrations of MPEP did not affect novel object discrimination in sham controls and worsened, rather then improved, novel object discrimination in lesioned animals; this latter effect disappeared after repeated administration and was never evident in sham animals. These data are in agreement with previous findings demonstrating that the same or higher doses of MPEP has no effect on short-term novel object discrimination in intact animals (Barker et al, 2006). A further caveat to be considered is that high doses of MPEP have been demonstrated to act also as NMDA receptor antagonists (O'Leary et al, 2000). However, NMDA receptor antagonism is achieved at brain concentrations higher than those reached after the doses used in the present study (Cosford et al, 2003; O'Leary et al, 2000). Moreover, NMDA antagonists alone or in combination with a reduced DA activity impair rather than improve mice performance in an object–place association tasks (Roullet et al, 1996). Therefore, it seems unlikely that the effect observed in these experiments could be due to NMDA receptors blockade.
On the basis of these results we verified the effects of acute and repeated systemic injection of MPEP (3 mg/kg) on rotational behavior induced by L-DOPA, in 6-OHDA unilaterally lesioned mice, a classical animal model of motor symptoms in PD. Consistent with previous studies, MPEP administration increased contralateral turning induced by L-DOPA. This effect was further potentiated after 7 days treatment. These results on the one hand confirm and extend previous findings in rats showing that chronic, but not acute, injection of low doses of MPEP can reverse the akinetic deficit induced by partial DA lesions of the dorsal striatum (Breysse et al, 2002, 2003). On the other hand, they contradict other experimental evidence showing that systemic acute or subchronic injection of MPEP, at low or high doses, reduces contralateral turning induced by L-DOPA in unilaterally 6-OHDA lesioned animals (Domenici et al, 2005; Spooren et al, 2000). This apparent discrepancy may be explained by the different site and extent of the lesion (Breysse et al, 2003; Domenici et al, 2005). In summary, we showed that MPEP, at low dose, has beneficial effects on cognitive as well as on motor deficits induced by partial DA depletion of the dorsal striatum, with no additional behavioral side effects.
There are several potential mechanisms and possible brain sites at which MPEP might have acted after its systemic administration. Recent autoradiographic studies with PET ligand show high concentrations of mGluR5 in the striatum, cortex and hippocampus (Wyss et al. 2007). However, in 6-OHDA lesioned rats, MPEP binding was increased in comparison to controls. Although mGluR5 up-regulation was observed in different brain regions, such as hippocampus and frontal cortex, it was more robust in the striatum. Further, in this structure it was accompanied by enhanced mGluR5 expression, as assessed by western blot analysis (Pellegrino et al, 2007). These findings support the existence compensatory mechanisms, at the striatal level, after nigrostriatal DA degeneration. In functional terms, one possibility is a direct effect of the mGluR5 antagonist on DA release in the striatum, by a presynaptic modulatory action on residual DA nerve terminals. However, MPEP (within the same dose range used in this study) has been reported to have no effect on extracellular DA in the prefrontal cortex and in the nucleus accumbens, and even reduce DA extracellular levels in the striatum in intact animals (Golembiowska et al, 2003; Homayoun et al, 2004). More likely, MPEP could modulate striatal glutamate release. Although mGluR5 are located predominantly postsynaptically, a presynaptical localization has recently been reported on corticostriatal glutamatergic afferents (Rodrigues et al, 2005). Consistently, it has been shown that MPEP could regulate glutamate release within the striatum (Rodrigues et al, 2005; Thomas et al, 2001). Hence, MPEP might act by reducing the availability of extracellular glutamate in the striatum, which in turn would lead to a reduced stimulation not only of mGluR5 but also of ionotropic glutamate postsynaptic receptors. Finally, mGluR5 blockade in the output nuclei of the BG, in addition to the striatum, might be responsible for the effects observed. In line with this, recent findings showed that DA lesion of the striatum is associated with overactivity of the subthalamic nucleus and substantia nigra pars reticulata, which are normalized by MPEP in parallel to the beneficial effect of MPEP on motor symptoms (Breysse et al, 2003; Phillips et al, 2006). It should be mentioned that the above-hypothesized mechanisms are not necessarily mutually exclusive and MPEP might act at different levels to revert 6-OHDA induced deficits. Additional studies using integrated approaches will help to elucidate these issues.
In conclusion, the most interesting finding of this study was the demonstration that, in an animal model of PD, systemic pharmacological treatments with potential therapeutic efficacy on motor symptoms not only do not have any detrimental effects on spatial learning and novelty exploration but on the contrary can also reverse the spatial discrimination deficit associated to the DA loss in the striatum. Therefore, regardless of the possible neural mechanisms underlying these beneficial effects, mGlu5 receptors may prove to be interesting potential targets for the development of possible treatments of PD.
References
Ballard TM, Woolley ML, Prinssen E, Huwyler J, Porter R, Spooren W (2005). The effect of the mGlu5 receptor antagonist MPEP in rodent tests of anxiety and cognition: a comparison. Psychopharmacology 179: 218–229.
Barker GR, Bashir ZI, Brown MW, Warburton EC (2006). A temporally distinct role for group I and group II metabotropic glutamate receptors in object recognition memory. Learn Mem 13: 178–186.
Belozertseva IV, Kos T, Popik P, Danysz W, Bespalov AY (2007). Antidepressant-like effects of mGluR1 and mGluR5 antagonists in the rat forced swim and the mouse tail suspension tests. Eur Neuropsychopharmacol 17: 172–179.
Berger HJ, Cools AR, Horstink MW, Oyen WJ, Verhoeven EW, van der Werf SP (2004). Striatal dopamine and learning strategy—an (123)I-FP-CIT SPECT study. Neuropsychologia 42: 1071–1078.
Breysse N, Amalric M, Salin P (2003). Metabotropic glutamate 5 receptor blockade alleviates akinesia by normalizing activity of selective basal-ganglia structures in parkinsonian rats. J Neurosci 23: 8302–8309.
Breysse N, Baunez C, Spooren W, Gasparini F, Amalric M (2002). Chronic but not acute treatment with a metabotropic glutamate 5 receptor antagonist reverses the akinetic deficits in a rat model of parkinsonism. J Neurosci 22: 5669–5678.
Campbell UC, Lalwani K, Hernandez L, Kinney GG, Conn PJ, Bristow LJ (2004). The mGluR5 antagonist 2-methyl-6-(phenylethynyl)-pyridine (MPEP) potentiates PCP-induced cognitive deficits in rats. Psychopharmacology 175: 310–318.
Coccurello R, Breysse N, Amalric M (2004). Simultaneous blockade of adenosine A2A and metabotropic glutamate mGlu5 receptors increase their efficacy in reversing Parkinsonian deficits in rats. Neuropsychopharmacology 29: 1451–1461.
Cools R, Lewis SJ, Clark L, Barker RA, Robbins TW (2007). -DOPA disrupts activity in the nucleus accumbens during reversal learning in Parkinson's disease. Neuropsychopharmacology 32: 180–189.
Cools R, Stefanova E, Barker RA, Robbins TW, Owen AM (2002). Dopaminergic modulation of high-level cognition in Parkinson's disease: the role of the prefrontal cortex revealed by PET. Brain 125: 584–594.
Cosford ND, Tehrani L, Roppe J, Schweiger E, Smith ND, Anderson J et al (2003). 3-[(2-Methyl-1,3-thiazol-4-yl)ethynyl]-pyridine: a potent and highly selective metabotropic glutamate subtype 5 receptor antagonist with anxiolytic activity. J Med Chem 46: 204–206.
De Leonibus E, Pascucci T, Lopez S, Oliverio A, Amalric M, Mele A (2007). Spatial deficit in a mouse model of Parkinson disease. Psychopharmacology 194: 517–525.
Dekundy A, Pietraszek M, Schaefer D, Cenci MA, Danysz W (2006). Effects of group I metabotropic glutamate receptors blockade in experimental models of Parkinson's disease. Brain Res Bull 69: 318–326.
Domenici MR, Potenza RL, Martire A, Coccurello R, Pezzola A, Reggio R et al (2005). Chronic treatment with the mGlu5R antagonist MPEP reduces the functional effects of the mGlu5R agonist CHPG in the striatum of 6-hydroxydopamine-lesioned rats: possible relevance to the effects of mGlu5R blockade in Parkinson's disease. J Neurosci Res 80: 646–654.
Franklin KBJ, Paxinos G (1997). The mouse brain in stereotaxic coordinates. Academic Press, San Diego.
Giraudo MD, Gayraud D, Habib M (1997). Visuospatial ability of parkinsonians and elderly adults in location memory tasks. Brain Cogn 34: 259–273.
Golembiowska K, Konieczny J, Wolfarth S, Ossowska K (2003). Neuroprotective action of MPEP, a selective mGluR5 antagonist, in methamphetamine-induced dopaminergic neurotoxicity is associated with a decrease in dopamine outflow and inhibition of hyperthermia in rats. Neuropharmacology 45: 484–492.
Gravius A, Pietraszek M, Schafer D, Schmidt WJ, Danysz W (2005). Effects of mGlu1 and mGlu5 receptor antagonists on negatively reinforced learning. Behav Pharmacol 16: 113–121.
Greenamyre JT, O'Brien CF (1991). N-methyl-D-aspartate antagonists in the treatment of Parkinson's disease. Arch Neurol 48: 977–981.
Gubellini P, Saulle E, Centonze D, Costa C, Tropepi D, Bernardi G et al (2003). Corticostriatal LTP requires combined mGluR1 and mGluR5 activation. Neuropharmacology 44: 8–16.
Homayoun H, Stefani MR, Adams BW, Tamagan GD, Moghaddam B (2004). Functional interaction between NMDA and mGlu5 receptors: effects on working memory, instrumental learning, motor behaviors, and dopamine release. Neuropsychopharmacology 29: 1259–1269.
Klockgether T, Turski L, Honore T, Zhang ZM, Gash DM, Kurlan R et al (1991). The AMPA receptor antagonist NBQX has antiparkinsonian effects in monoamine-depleted rats and MPTP-treated monkeys. Ann Neurol 30: 717–723.
Lenck-Santini PP, Rivard B, Muller RU, Poucet B (2005). Study of CA1 place cell activity and exploratory behavior following spatial and nonspatial changes in the environment. Hippocampus 15: 356–369.
Lewis SJ, Dove A, Robbins TW, Barker RA, Owen AM (2003). Cognitive impairments in early Parkinson's disease are accompanied by reductions in activity in frontostriatal neural circuitry. J Neurosci 23: 6351–6356.
Lu YM, Jia Z, Janus C, Henderson JT, Gerlai R, Wojtowicz JM et al (1997). Mice lacking metabotropic glutamate receptor 5 show impaired learning and reduced CA1 long-term potentiation (LTP) but normal CA3 LTP. J Neurosci 17: 5196–5205.
Manahan-Vaughan D, Braunewell KH (2005). The metabotropic glutamate receptor, mGluR5, is a key determinant of good and bad spatial learning performance and hippocampal synaptic plasticity. Cereb Cortex 15: 1703–1713.
Miyoshi E, Wietzikoski S, Camplessei M, Silveira R, Takahashi RN, Da Cunha C (2002). Impaired learning in a spatial working memory version and in a cued version of the water maze in rats with MPTP-induced mesencephalic dopaminergic lesions. Brain Res Bull 58: 41–47.
Mura A, Feldon J (2003). Spatial learning in rats is impaired after degeneration of the nigrostriatal dopaminergic system. Mov Disord 18: 860–871.
Naie K, Manahan-Vaughan D (2004). Regulation by metabotropic glutamate receptor 5 of LTP in the dentate gyrus of freely moving rats: relevance for learning and memory formation. Cereb Cortex 14: 189–198.
O'Leary DM, Movsesyan V, Vicini S, Faden AI (2000). Selective mGluR5 antagonists MPEP and SIB-1893 decrease NMDA or glutamate-mediated neuronal toxicity through actions that reflect NMDA receptor antagonism. Br J Pharmacol 131: 1429–1437.
Ossowska K, Konieczny J, Wardas J, Golembiowska K, Wolfarth S, Pilc A (2002). The role of striatal metabotropic glutamate receptors in Parkinson's disease. Amino Acids 23: 193–198.
Ossowska K, Konieczny J, Wolfarth S, Pilc A (2005). MTEP, a new selective antagonist of the metabotropic glutamate receptor subtype 5 (mGluR5), produces antiparkinsonian-like effects in rats. Neuropharmacology 49: 447–455.
Ossowska K, Konieczny J, Wolfarth S, Wieronska J, Pilc A (2001). Blockade of the metabotropic glutamate receptor subtype 5 (mGluR5) produces antiparkinsonian-like effects in rats. Neuropharmacology 41: 413–420.
Oueslati A, Breysse N, Amalric M, Kerkerian-Le Goff L, Salin P (2005). Dysfunction of the cortico–basal ganglia–cortical loop in a rat model of early parkinsonism is reversed by metabotropic glutamate receptor 5 antagonism. Eur J Neurosci 22: 2765–2774.
Owen AM, Doyon J, Dagher A, Sadikot A, Evans AC (1998). Abnormal basal ganglia outflow in Parkinson's disease identified with PET. Implications for higher cortical functions. Brain 121: 949–965.
Owen AM, Iddon JL, Hodges JR, Summers BA, Robbins TW (1997). Spatial and non-spatial working memory at different stages of Parkinson's disease. Neuropsychologia 35: 519–532.
Pellegrino D, Cicchetti F, Wang X, Zhu A, Yu M, Saint-Pierre M et al. (2007). Modulation of dopaminergic and glutamatergic brain function: PET studies on parkinsonian rats. J Nucl Med 48: 1147–1153.
Petersen S, Bomme C, Baastrup C, Kemp A, Christoffersen GR (2002). Differential effects of mGluR1 and mGlur5 antagonism on spatial learning in rats. Pharmacol Biochem Behav 73: 381–389.
Phillips JM, Lam HA, Ackerson LC, Maidment NT (2006). Blockade of mGluR glutamate receptors in the subthalamic nucleus ameliorates motor asymmetry in an animal model of Parkinson's disease. Eur J Neurosci 23: 151–160.
Pilc A, Klodzinska A, Branski P, Nowak G, Palucha A, Szewczyk B et al (2002). Multiple MPEP administrations evoke anxiolytic- and antidepressant-like effects in rats. Neuropharmacology 43: 181–187.
Pillon B, Deweer B, Vidailhet M, Bonnet AM, Hahn-Barma V, Dubois B (1998). Is impaired memory for spatial location in Parkinson's disease domain specific or dependent on ‘strategic’ processes? Neuropsychologia 36: 1–9.
Pillon B, Ertle S, Deweer B, Bonnet AM, Vidailhet M, Dubois B (1997). Memory for spatial location in ‘de novo’ parkinsonian patients. Neuropsychologia 35: 221–228.
Popoli P, Pezzola A, Torvinen M, Reggio R, Pintor A, Scarchilli L et al (2001). The selective mGlu(5) receptor agonist CHPG inhibits quinpirole-induced turning in 6-hydroxydopamine-lesioned rats and modulates the binding characteristics of dopamine D(2) receptors in the rat striatum: interactions with adenosine A(2a) receptors. Neuropsychopharmacology 25: 505–513.
Rodrigues RJ, Alfaro TM, Rebola N, Oliveira CR, Cunha RA (2005). Co-localization and functional interaction between adenosine A(2A) and metabotropic group 5 receptors in glutamatergic nerve terminals of the rat striatum. J Neurochem 92: 433–441.
Roullet P, Mele A, Ammassari-Teule M (1996). Involvement of glutamatergic and dopaminergic systems in the reactivity of mice to spatial and non-spatial change. Psychopharmacology 126: 55–61.
Roullet P, Sargolini F, Oliverio A, Mele A (2001). NMDA and AMPA antagonist infusions into the ventral striatum impair different steps of spatial information processing in a nonassociative task in mice. J Neurosci 21: 2143–2149.
Simonyi A, Schachtman TR, Christoffersen GR (2005). The role of metabotropic glutamate receptor 5 in learning and memory processes. Drug News Perspect 18: 353–361.
Spooren WP, Gasparini F, Bergmann R, Kuhn R (2000). Effects of the prototypical mGlu(5) receptor antagonist 2-methyl-6-(phenylethynyl)-pyridine on rotarod, locomotor activity and rotational responses in unilateral 6-OHDA-lesioned rats. Eur J Pharmacol 406: 403–410.
Steckler T, Oliveira AF, Van Dyck C, Van Craenendonck H, Mateus AM, Langlois X et al (2005). Metabotropic glutamate receptor 1 blockade impairs acquisition and retention in a spatial Water maze task. Behav Brain Res 164: 52–60.
Thomas LS, Jane DE, Gasparini F, Croucher MJ (2001). Glutamate release inhibiting properties of the novel mGlu(5) receptor antagonist 2-methyl-6-(phenylethynyl)-pyridine (MPEP): complementary in vitro and in vivo evidence. Neuropharmacology 41: 523–527.
Turle-Lorenzo N, Breysse N, Baunez C, Amalric M (2005). Functional interaction between mGlu 5 and NMDA receptors in a rat model of Parkinson's disease. Psychopharmacology 179: 117–127.
Whishaw IQ, Dunnett SB (1985). Dopamine depletion, stimulation or blockade in the rat disrupts spatial navigation and locomotion dependent upon beacon or distal cues. Behav Brain Res 18: 11–29.
Wyss MT, Ametamey SM, Treyer V, Bettio A, Blagoev M, Kessler LJ et al (2007). Quantitative evaluation of 11C-ABP688 as PET ligand for the measurement of the metabotropic glutamate receptor subtype 5 using autoradiographic studies and a β-scintillator. Neuroimage 35: 1086–1092.
Acknowledgements
The present study has been supported by a Galileo grant (to AM and MA), PRIN and FIRB grants from MIUR (to AO and AM) and grants DCMC and SaC from ASI (to AO and AM). We thankful to Dr Fabrizio Gasparini (Novartis Pharma AG, Basel, Switzerland) for the generous gift of MPEP, and to Dr Agu Pert for his useful comments on a previous version of the article.
Author information
Authors and Affiliations
Corresponding author
Additional information
DISCLOSURE/CONFLICT OF INTEREST
We declare that there is no conflict of interest for any of the authors.
Rights and permissions
About this article
Cite this article
De Leonibus, E., Managò, F., Giordani, F. et al. Metabotropic Glutamate Receptors 5 Blockade Reverses Spatial Memory Deficits in a Mouse Model of Parkinson's Disease. Neuropsychopharmacol 34, 729–738 (2009). https://doi.org/10.1038/npp.2008.129
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2008.129
Keywords
This article is cited by
-
Negative versus positive allosteric modulation of metabotropic glutamate receptors (mGluR5): indices for potential pro-cognitive drug properties based on EEG network oscillations and sleep-wake organization in rats
Psychopharmacology (2015)
-
Therapeutic potential of targeting glutamate receptors in Parkinson’s disease
Journal of Neural Transmission (2014)
-
Interaction between the mGlu receptors 5 antagonist, MPEP, and amphetamine on memory and motor functions in mice
Psychopharmacology (2013)
-
The effects of pergolide on memory and oxidative stress in a rat model of Parkinson’s disease
Journal of Physiology and Biochemistry (2012)
-
Targeting Glutamate Receptors to Tackle the Pathogenesis, Clinical Symptoms and Levodopa-Induced Dyskinesia Associated with Parkinson’s Disease
CNS Drugs (2012)