Abstract
Background:
Long-term maintenance treatment with an antipsychotic is often required to prevent relapse and mitigate functional deterioration in patients with schizophrenia.
Aims:
This study assessed the long-term safety, tolerability, and maintenance of the therapeutic effect of aripiprazole once-monthly 400 mg (AOM 400) in patients with schizophrenia.
Methods:
This 52-week, open-label study included patients previously enrolled in 1 of 2 AOM 400 randomized controlled trials (RCTs) and de novo patients. Safety endpoints included adverse events (AEs), suicidality, extrapyramidal symptoms, injection-site pain, and clinically relevant changes in clinical and laboratory values. The primary efficacy endpoint was the percentage of stable patients at baseline who remained stable at the last visit of the AOM 400 maintenance phase. All endpoints were assessed with descriptive statistics; there were no formal planned statistical analyses.
Results:
Of 1,247 patients screened, 1,178 enrolled in the study (194 de novo and 984 patients from the RCTs) and 1,081 received maintenance treatment with AOM 400. The maintenance phase completion rate was 79.4% at 52 weeks. Treatment-emergent AEs in ⩾5% of patients during open-label AOM 400 treatment were headache (7.6%), nasopharyngitis (7.0%), anxiety (6.8%), and insomnia (6.6%). There were no clinically relevant changes in safety parameters of interest. Ninety-five percent of stable patients at baseline remained stable at their last visit during the AOM 400 maintenance phase.
Conclusions:
The long-term safety and tolerability profile of AOM 400 was comparable to the RCTs, and the long-term therapeutic effect was maintained.
Similar content being viewed by others
Introduction
Schizophrenia is a chronic condition for which long-term maintenance treatment with antipsychotic medication is critical to prevent relapse and mitigate functional deterioration.1–4 In an effort to improve treatment adherence by eliminating the need for daily dosing, long-acting injectable (LAI) antipsychotic formulations have been developed and have demonstrated long-term improvements in relapse rates4,5 and may potentially minimize functional deterioration.2,6
Aripiprazole once-monthly 400 mg (AOM 400), an extended-release injectable suspension of aripiprazole, is the only dopamine D2 partial agonist7 available as an LAI. AOM 400 is approved for the treatment of schizophrenia. In two randomized controlled trials (RCTs), AOM 400 delayed time to impending relapse and reduced impending relapse rates versus placebo and a subtherapeutic dose of aripiprazole once-monthly, respectively.8,9
The current 52-week, multicenter, open-label study evaluated the long-term effectiveness of AOM 400 as maintenance treatment in patients with schizophrenia, some of whom had received AOM 400 in RCTs. The primary objective was to evaluate the long-term safety and tolerability of AOM 400, and the secondary objective was to assess long-term maintenance of the therapeutic effect.
Materials and methods
Study design and patients
Patients in this study (NCT00731549), conducted from February 2009 to October 2013, were de novo or had participated in 1 of 2 RCTs: a 52-week placebo-controlled study (NCT00705783) and a 38-week active-controlled study (NCT00706654) that assessed AOM 400 as maintenance treatment of schizophrenia.8,9 The 52-week study had four treatment phases, which included an oral conversion phase (4–6 weeks; patients were cross-titrated to oral aripiprazole monotherapy if they were currently treated with another antipsychotic), oral stabilization phase (4–12 weeks; patients were stabilized on oral aripiprazole 10–30 mg/day based on predefined stability criteria), AOM 400 stabilization phase (12–36 weeks; patients were exposed to single-blind treatment with AOM 400 with concomitant oral aripiprazole for the first 2 weeks), and then the maintenance treatment phase (up to 52 weeks, patients who met predefined stability criteria were randomized 2:1 to AOM 400 or placebo). The primary endpoint, time to impending relapse/exacerbation of psychotic symptoms, was significantly delayed in patients treated with AOM 400 compared with placebo.8 The 38-week study had three treatment phases that included an oral conversion phase (4–6 weeks; patients were cross-titrated to oral aripiprazole monotherapy if they were currently treated with another antipsychotic), oral stabilization (8–28 weeks; patients were stabilized on oral aripiprazole 10–30 mg/day based on predefined stability criteria), and the double-blind maintenance phase (up to 38 weeks; patients were randomized 2:2:1 to AOM 400, oral aripiprazole 10–30 mg/day (an active-control group), or AOM 50 mg (a subtherapeutic dose)). The primary endpoint, the Kaplan–Meier estimated impending relapse rate from randomization to week 26, was significantly lower in the AOM 400 mg group compared with the AOM 50 mg group, and non-inferiority between AOM 400 and oral aripiprazole treatment groups was established.9
Eligible patients aged 18 to 65 years had a current diagnosis of schizophrenia (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR)) for ⩾3 years before screening, and per the study investigator’s opinion, required chronic antipsychotic treatment and would benefit from continuing or initiating treatment with AOM 400. The assessment of potential benefit of initiating or continuing treatment with AOM 400 was made at the discretion of study investigators on a case-by-case basis. For de novo patients and patients with >30 days’ lapse since concluding participation in the RCTs, exclusion criteria were similar to those of the previous RCTs.8,9 All patients provided written informed consent prior to study participation, and the protocol and amendments were approved by the institutional review board or independent ethics committee for each respective trial site or country.
There were three consecutive treatment phases (Figure 1): an oral conversion phase (phase 1, 4–6 weeks; patients cross-titrated from their prior antipsychotic therapy to oral aripiprazole 10 or 15 mg/day and were seen weekly for assessments); an oral stabilization phase (phase 2, 4–16 weeks; patients received flexible dosing of oral aripiprazole 10–30 mg/day and were seen biweekly for assessments); and an open-label AOM 400 maintenance phase (phase 3, 52 weeks; patients were seen weekly for the first 4 weeks, biweekly for weeks 6–12, and every 4 weeks through week 52). After screening, patients who were not currently receiving oral aripiprazole (including de novo patients) and patients who had >30 days’ lapse since completion of or discontinuation from one of the RCTs entered the oral conversion phase and cross-titrated to oral aripiprazole. De novo patients currently receiving oral aripiprazole and patients from the RCTs with ⩽30 days’ lapse since concluding participation entered the current study in the oral stabilization phase and received flexible dosing of oral aripiprazole (10–30 mg).
Because the 52-week RCT was terminated after the interim analysis when the primary efficacy endpoint was met,8 patients who were in the conversion phase, oral stabilization phase, or single-blind AOM 400 stabilization phase of the 52-week study could enter the current study and remain in the same phase. However, all patients who were in the double-blind, placebo-controlled phase at the time of termination entered the current study in the oral stabilization phase and were restabilized on oral aripiprazole (10–30 mg), because some patients had been on placebo when the 52-week study was terminated.
All patients who met predefined stability criteria with oral aripiprazole therapy could enter the AOM 400 maintenance phase. As in the RCTs,8,9 stability was defined as patients meeting all of the following criteria on 1 occasion after receiving ⩾4 weeks of oral aripiprazole 10–30 mg: outpatient status; Positive and Negative Syndrome Scale (PANSS) total score ⩽80; lack of specific psychotic symptoms as measured by a score of ⩽4 on the conceptual disorganization, suspiciousness, hallucinatory behavior, and unusual thought content PANSS items; Clinical Global Impression-Severity10 (CGI-S) score ⩽4 (moderately ill); and a Clinical Global Impression-Severity of Suicidality11 (CGI-SS) score ⩽2 (mildly suicidal) on part 1 and ⩽5 (minimally worsened) on part 2.
During the maintenance phase, all patients initiated AOM 400 but could reduce their dose to 300 mg for tolerability and could return to 400 mg for efficacy, based on investigator judgment. Patients received oral aripiprazole 10–20 mg/day for the first 2 weeks after initiating AOM 400 to maintain therapeutic plasma concentrations. Thereafter, patients could receive oral aripiprazole for short-term rescue therapy and for ⩽3 episodes of impending relapse over the 52 weeks. No other antipsychotic medications were permitted during this period.
Assessments
Safety was assessed by adverse events (AEs), including frequency, severity, seriousness, and discontinuation due to AEs. AEs ongoing at the last visit of the RCTs that increased in severity or frequency were recorded as new AEs in the current study. Potentially clinically relevant changes in vital signs, routine laboratory tests, electrocardiograms, serum prolactin concentrations, and body weight were monitored. Extrapyramidal symptoms (EPS) were assessed using the Simpson-Angus Scale12 (SAS), Abnormal Involuntary Movement Scale13 (AIMS), and Barnes Akathisia Rating Scale14 (BARS). Risk of suicide was assessed with the CGI-SS and the Columbia Suicide Severity Rating Scale15 (C-SSRS). The Columbia Classification Algorithm of Suicide Assessment16 was used to classify potential suicidality events that were recorded as AEs. Patients evaluated injection site pain using a visual analog scale (VAS) with ratings that ranged from 0 mm (no pain) to 100 mm (unbearable pain). Study investigators rated injection site reactions (localized pain, swelling, redness, and induration) at the most recent injection site using a 4-point categorical scale ranging from absent to severe.17,18
The primary efficacy endpoint was the percentage of stable patients at baseline who met all of the predefined stability criteria at the last visit of the maintenance phase. The key secondary efficacy endpoint was the proportion of patients with impending relapse8,19 during the maintenance phase. Impending relapse was defined as meeting ⩾1 of the following four criteria: (1) Clinical Global Impression-Improvement (CGI-I) score ⩾5 (minimally worse) AND a score >4, with an absolute increase of ⩾2, for any of the PANSS items conceptual disorganization, hallucinatory behavior, suspiciousness, or unusual thought content OR CGI-I score ⩾5 (minimally worse) AND a score >4, with an absolute increase of ⩾4, on the same combined 4 PANSS items; (2) hospitalization due to worsening of psychotic symptoms (but not for psychosocial reasons); (3) CGI-SS score of 4 (severely suicidal) or 5 (attempted suicide) on part 1 and/or 6 (much worse) on part 2; and (4) violent behavior resulting in clinically relevant self-injury, injury to another person, or property damage.
Overall effectiveness (i.e., efficacy and tolerability) was measured with the Investigator’s Assessment Questionnaire (IAQ), a scale that includes 12 items that assess efficacy and tolerability: positive symptoms, negative symptoms, other symptoms, somnolence, weight gain, signs and symptoms of prolactin elevation, akathisia, extrapyramidal symptoms, other safety or tolerability issues, cognition, energy, and mood. Each item was rated by the investigator on a 5-point scale (range: much better1 to much worse5) relative to the patient’s antipsychotic medication prior to baseline (i.e., during the oral conversion phase or at screening for de novo patients) and summed for a total score (range, 12–60). The IAQ was only completed by patients who underwent cross-titration during the oral conversion phase or were de novo patients. For the items ‘other symptoms’ and ‘other safety or tolerability issues,’ if no such symptoms or issues occurred, then a response of ‘none’ was noted. Lower scores indicate greater improvement compared with prior medication.
Statistical analyses
The safety sample for the maintenance phase included all patients who received ⩾1 dose of AOM 400 during the maintenance phase. The efficacy sample included all patients who had ⩾1 postbaseline efficacy evaluation in the maintenance phase; baseline was defined as the last visit with available data before entering the open-label maintenance phase. Endpoints were summarized using descriptive statistics for all patients and by enrollment source. Because this was an open-label trial, no formal statistical analyses were planned. Descriptive statistics for the observed case (OC) data set were computed for selected safety endpoints in the maintenance phase: laboratory test results, vital sign parameters, electrocardiogram (ECG) parameters, SAS total score, BARS global score, AIMS movement scale score, CGI-SS severity of suicide score and change in suicidality score, and C-SSRS mean and mean change from baseline in suicidal ideation intensity score for most severe suicidal ideation.
The percentage of stable patients at baseline who remained stable at endpoint was calculated using the last visit of the maintenance phase with available data. Time to first impending relapse was plotted using a Kaplan–Meier curve. IAQ total scores and changes from baseline in PANSS total score during the maintenance phase were also assessed using descriptive statistics for the OC data set by visit for the efficacy sample.
Results
Patient disposition and characteristics
Of 1,247 patients screened, 1,178 enrolled in the study; and 858/1,081 patients (79.4%) entered the AOM 400 maintenance phase and completed the week 52 visit (Figure 1). Patients who entered from 1 of the previous RCTs were more likely to complete the current study than de novo patients; 52/143 (36.4%) de novo patients discontinued and 171/938 (18.2%) patients who entered from the RCTs discontinued (Figure 2).
Reasons for discontinuation during the aripiprazole once-monthly 400 mg maintenance phase. aIncluded patients who met any of the following criteria: experienced an AE, intercurrent illness, or laboratory abnormality that warranted withdrawal per investigator opinion; treated with prohibited concomitant medications; nonadherence; patient, investigator, study sponsor, or regulatory authority requested withdrawal; pregnancy; lost to follow-up; did not fulfill stability criteria on oral aripiprazole between weeks 4 and 16 of the oral stabilization phase; or met criteria for exacerbation of psychotic symptoms/impending relapse after three episodes of rescue therapy during the aripiprazole once-monthly maintenance phase. AE, adverse event.
Demographic and baseline characteristics were similar across phases (Table 1). At baseline of the maintenance phase, mean PANSS total score (54.5), mean CGI-S score (3.0), and mean CGI-SS score (1.0) indicated that patients were stable and not suicidal.
Treatment exposure and adherence
During the maintenance phase, 934/1,081 patients (86.4%) received AOM 400 mg for ⩾6 months (i.e., injections every 28 days for 7 injections) and 826/1,081 (76.4%) patients received treatment for ⩾12 months (i.e., injections every 28 days for 13 injections). In reviewing total exposure from the RCTs (i.e., including exposure during the 38-week and 52-week studies), there were 276 patients with ⩾20 months of aripiprazole once-monthly 300 or 400 mg exposure, including 36 patients with >2 years’ exposure and 1 patient who received AOM 400 for 28 months. In the current study, 92% of patients (990/1,081) initiated aripiprazole once-monthly at the 400-mg dose and had no dose change. The percentage of patients who initiated AOM 400 and had no dose change ranged from 84% for de novo patients to 92 and 93% for patients who entered from the 38-week and 52-week RCTs, respectively.
During the first 2 weeks of the maintenance phase, the mean (s.d.) dose of concomitant oral aripiprazole was 11.5 (2.8) mg/day. During the maintenance phase, 77/1,081 patients (7.1%) received oral aripiprazole as rescue therapy, including 17/143 (11.9%) de novo patients, 28/464 (6.0%) and 32/474 (6.8%) from the 52-week and 38-week RCTs. Few patients required two episodes (13/1,081, 1.2%) or 3 episodes (2/1,081, 0.2%) of rescue therapy. The mean (s.d.) dose of oral aripiprazole rescue therapy for the first episode was 10.7 (2.1) mg/day, and the mean duration was 19.2 (7.9) days. The percentage of patients who were stable at baseline and remained stable at the last visit of the maintenance treatment phase was higher for patients who did not receive oral aripiprazole as rescue therapy (967/996, 97.1%) compared with patients who were treated with oral aripiprazole rescue therapy (51/76, 67.1%).
Safety and tolerability
Adverse events
During the maintenance phase, 726/1,081 patients (67.2%) had treatment-emergent AEs (TEAEs; Table 2); most were mild or moderate in severity; 95/1,081 (8.8%) patients experienced a serious TEAE. Severe TEAEs occurred in 79/1,081 patients (7.3%): 12/143 (8%) de novo, 30/464 (7%) from the 52-week RCT, and 37/474 (8%) from the 38-week RCT. TEAEs led to study discontinuation in 68/1,081 patients (6.3%): 15/143 (11%) de novo, 29/464 (6%) from the 52-week study, and 24/474 (5%) from the 38-week study.
TEAEs that occurred in ⩾1% of patients and were classified as serious, severe, or leading to study discontinuation included psychotic disorder and schizophrenia (serious: 15/1,081 (1.4%) and 21/1,081 (1.9%), respectively; severe: 13/1,081 (1%) and 14/1,081 (1%); leading to study discontinuation: 14/1,081 (1.3%) and 18/1,081 (1.7%)). Eight deaths (8/1,081 (0.7%)) occurred during the maintenance phase; most were cardiovascular related, and none were related to study medication (myocardial infarction (n=2); arteriosclerosis (n=1); cardiorespiratory arrest due to hypovolemia, dehydration, and metastatic adenocarcinoma of the lung (n=1); cardiac arrest (n=1); ruptured cerebral aneurism (n=1); unexplained/natural causes (n=1); and metastatic renal cancer (n=1)).
Safety and tolerability parameters of interest
There were no clinically relevant mean changes from baseline in serum chemistry, hematology, urinalysis, insulin, fasting insulin, vital signs (including blood pressure, heart rate, body temperature, waist circumference, or body mass index), or ECG parameters during the AOM 400 maintenance phase. There was a moderately higher incidence of potentially clinically relevant weight gain or loss (⩾7% change from baseline) at the last visit in de novo patients compared with patients who were enrolled from the RCTs (Table 3). Mean weight slightly increased from baseline to last visit of the maintenance phase for the overall sample (Table 3). Mean changes from baseline in serum prolactin levels in the maintenance phase were small and comparable for all patients (Table 3). At the last visit of the maintenance phase, potentially clinically relevant prolactin concentrations (above the upper limit of normal) were reported in 2.1% (23/1,070) of all patients (3/138 (2.2%) de novo, 10/461 (2.2%) from the 52-week RCT, and 10/471 (2.1%) from the 38-week RCT). EPS rating scale scores remained stable throughout the maintenance phase (Table 3).
Mean CGI-SS scores were 1.0 (not at all suicidal) and mean CGI change in suicidality scores were at or near 4.0 (no change) at baseline of the maintenance phase and remained stable throughout treatment for all patients and by enrollment source. No patients completed suicide during the maintenance phase. Suicidal ideation was reported by 46/1,081 patients (4.3%). Mean (s.d.) score and change from baseline in C-SSRS suicidal ideation intensity scores were 0.2 (1.5) and 0.1 (1.4), respectively, for all patients at the last visit of the maintenance phase, indicating low severity of intensity; findings were similar by enrollment source.
Most patients rated injection site pain as minimal, and most investigators rated injection site reactions as absent from the first through the last injection. Overall, patient and investigator assessments of injection site pain and reactions (redness, swelling, and induration) improved between the first and last injections; ‘absent’ ratings (i.e., absence of pain or reaction) among patients and investigators ranged from 84.9 to 98.2% after the first injection and from 87.7 to 99.1% after the last injection.
Efficacy outcomes
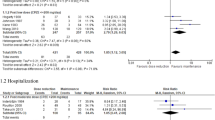
Ninety-five percent (1018/1072) of patients who were stable at baseline of the maintenance phase were also stable at their last visit. The percentage of patients who were stable at baseline and remained stable was high (i.e., 98%) for nearly all study weeks thereafter, regardless of enrollment source. For most visits of the maintenance phase, the percentage of patients meeting impending relapse criteria was ⩽1%. Overall, 8.3% of patients (89/1072) met criteria for impending relapse during the maintenance phase (Figure 3a). Mean CGI-S scores remained stable from baseline to the last visit of the maintenance phase (mean (s.d.) change, −0.14 (0.70)). The mean CGI-I score at last visit, 3.35 (1.10), also indicated that, on average, patients remained stable. PANSS total scores (possible range of 30–210, with higher scores indicating more severe symptoms) also remained relatively stable during the maintenance phase (Figure 3b); mean (s.d.) change from baseline to last visit was −1.72 (10.21) and ranged from −3.40 (10.41) to −0.19 (9.19) among enrollment source groups. The mean (s.d.) IAQ total score at week 12 (first assessment) was 30.85 (5.11) and was similar at last visit (30.22 (6.00)).
(a) Kaplan–Meier plot of time to first impending relapse during the aripiprazole once-monthly 400 mg maintenance phase. AOM 400, aripiprazole once-monthly 400 mg. (b) Mean PANSS total scores during the aripiprazole once-monthly 400 mg maintenance phase. Data are from observed cases. AOM 400, aripiprazole once-monthly 400 mg; PANSS, Positive and Negative Syndrome Scale.
Discussion
Main findings
Open-label maintenance treatment with AOM 400 for up to 52 weeks was safe, effective, and well tolerated in patients with schizophrenia. The completion rate was high (79.4%) and rates of metabolic abnormalities and extrapyramidal symptoms were low. The majority of patients who were stable at baseline remained stable. Most patients did not meet criteria for impending relapse, and PANSS, CGI-S, and CGI-I scores remained relatively stable, providing further evidence of the long-term maintenance of the therapeutic effect of AOM 400. Results from the current study, in which 92% of patients initiated or continued aripiprazole once-monthly therapy at 400 mg and had no dose change, confirm 400 mg20–22 as the effective starting and maintenance dose. Taking into account prior exposure from the RCTs, >200 patients were treated with AOM (400 mg or 300 mg) for >20 months, which provides further evidence for the well-established tolerability profile of AOM 400 in patients who remain on long-term treatment.
Interpretation of findings in relation to previously published work
The overall AE profile was consistent with the product labeling for AOM 400 and oral aripiprazole and with the AE profile in the RCTs.8,9 Consistent with the known safety profile of AOM 400, none of the EPS-related TEAEs reported as akathisia were considered serious or resulted in study discontinuation, the changes in prolactin levels were not clinically relevant, a low incidence of suicidal ideation was observed, and injection site reactions were mild or absent. Likewise, the modest mean increase in weight and the low rate of potentially clinically relevant weight gain further support the long-term favorable metabolic profile.
Although the current study had no placebo group for comparison, the percentage of stable patients at baseline who met stability criteria at the last visit was numerically higher with AOM 400 (95%) in the current study compared with the placebo group in the 52-week RCT (56%) and the subtherapeutic aripiprazole once-monthly 50-mg group in the 38-week RCT (75%). In the 52-week study, 40% of patients in the placebo group met impending relapse criteria at the final analysis time point, and 22% in the aripiprazole once-monthly 50-mg group met impending relapse criteria by week 38 in the 38-week study. In the current study, 8.3% of patients treated with AOM 400 met criteria for impending relapse, which is comparable with the rates for AOM 400-treated patients during double-blind treatment in both the 52-week (10.0%) and the 38-week study (8.3%). The comparatively high rates of stability and low rates of impending relapse in our open-label study, along with the low frequency of patients who required rescue therapy during the maintenance phase, confirm that the long-term therapeutic effect of AOM 400 was maintained. The all-cause discontinuation rate with AOM 400 in the current study (21%) was similar to those in the RCTs (25% in the 52-week trial and 26% in the 38-week trial).8,9 In comparison with other LAI antipsychotics, the rate of all-cause discontinuation in the current study (20.6%) was lower than rates reported in a 1-year naturalistic observational study with paliperidone palmitate and a 1-year, open-label trial with risperidone LAI (35% for both),23,24 and similar to the discontinuation rate in a 52-week, open-label extension study with paliperidone palmitate (22%).25 The 20.6% all-cause discontinuation rate in the current study was also lower than rates reported in short-term, open-label studies of oral aripiprazole in the US and EU (35.0 and 25.5%, respectively).26,27 The higher completion rates in this long-term open-label study may reflect the stability of patients at baseline of the maintenance phase, and the study population including patients who previously tolerated AOM 400 in the prior RCTs. Although the majority of patients in our study continued into this study after participating in one of the RCTs, the all-cause discontinuation rate was also comparatively low in the de novo patients (36%), indicating that AOM 400 is an effective long-term treatment option. The IAQ scores at week 12 and last visit indicate that investigators rated AOM 400 as about the same or slightly better on most efficacy, safety, and tolerability items, lending further support to the long-term effectiveness of AOM 400.
Strengths and limitations of the study
This study described the long-term clinical profile (i.e., >52 weeks in patients from RCTs) of AOM 400 as maintenance treatment in a large sample of patients with schizophrenia. The limitations of the current study, in addition to those noted in the RCTs,8,9 include lack of a control group, which limits the ability to attribute outcomes to treatment with AOM 400. Although self-selection of patients from the prior RCTs may limit the generalizability of our findings, we have reported all outcomes for the subpopulation of patients who entered the study de novo.
Conclusions
Open-label long-term treatment with AOM 400 was well tolerated in patients with schizophrenia, and the therapeutic effect was maintained. The high completion rate and low impending relapse rate confirm that AOM 400 is an effective, safe, and well-tolerated long-term treatment option for patients with schizophrenia.
References
Hasan A, Falkai P, Wobrock T, Lieberman J, Glenthoj B, Gattaz WF et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia, part 2: update 2012 on the long-term treatment of schizophrenia and management of antipsychotic-induced side effects. World J Biol Psychiatry 2013; 14: 2–44.
Harvey PD, Loewenstein DA, Czaja SJ . Hospitalization and psychosis: influences on the course of cognition and everyday functioning in people with schizophrenia. Neurobiol Dis 2013; 53: 18–25.
Caseiro O, Perez-Iglesias R, Mata I, Martinez-Garcia O, Pelayo-Teran JM, Tabares-Seisdedos R et al. Predicting relapse after a first episode of non-affective psychosis: a three-year follow-up study. J Psychiatr Res 2012; 46: 1099–1105.
Tandon R, Nasrallah HA, Keshavan MS . Schizophrenia, ‘just the facts’ 5. Treatment and prevention. Past, present, and future. Schizophr Res 2010; 122: 1–23.
Leucht C, Heres S, Kane JM, Kissling W, Davis JM, Leucht S . Oral versus depot antipsychotic drugs for schizophrenia—a critical systematic review and meta-analysis of randomised long-term trials. Schizophr Res 2011; 127: 83–92.
Kaplan G, Casoy J, Zummo J . Impact of long-acting injectable antipsychotics on medication adherence and clinical, functional, and economic outcomes of schizophrenia. Patient Prefer Adherence 2013; 7: 1171–1180.
Burris KD, Molski TF, Xu C, Ryan E, Tottori K, Kikuchi T et al. Aripiprazole, a novel antipsychotic, is a high-affinity partial agonist at human dopamine D2 receptors. J Pharmacol Exp Ther 2002; 302: 381–389.
Kane J, Sanchez R, Perry P, Jin N, Johnson B, Forbes R et al. Aripiprazole intramuscular depot as maintenance treatment in patients with schizophrenia: a 52-week multicenter, randomized, double-blind, placebo-controlled study. J Clin Psychiatry 2012; 73: 617–624.
Fleischhacker WW, Sanchez R, Perry PP, Jin N, Peters-Strickland T, Johnson BR et al. Aripiprazole once-monthly for treatment of schizophrenia: double-blind, randomised, non-inferiority study. Br J Psychiatry 2014; 205: 135–144.
Guy W . In: Clinical Global Impression Scale (CGI). US Dept. of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs: Rockville, MD, 1976, 217–222.
Meltzer HY, Alphs L, Green AI, Altamura AC, Anand R, Bertoldi A et al. Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT). Arch Gen Psychiatry 2003; 60: 82–91.
Simpson GM, Angus JW . A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl 1970; 212: 11–19.
Guy W . In: Abnormal Involuntary Movement Scale (AIMS). US Dept. of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs: Rockville, MD, 1976, 534–537.
Barnes TR . A rating scale for drug-induced akathisia. Br J Psychiatry 1989; 154: 672–676.
Posner K, Brent D, Lucas C, Gould M, Stanley B, Brown G et al. Columbia Suicide Severity Rating Scale. Available at http://cssrs.columbia.edu/docs/C-SSRS_1_14_09_Baseline.pdf Accessed on 23 April 2014.
Posner K, Oquendo MA, Gould M, Stanley B, Davies M . Columbia Classification Algorithm of Suicide Assessment (C-CASA): classification of suicidal events in the FDA's pediatric suicidal risk analysis of antidepressants. Am J Psychiatry 2007; 164: 1035–1043.
Kane JM, Eerdekens M, Lindenmayer JP, Keith SJ, Lesem M, Karcher K . Long-acting injectable risperidone: efficacy and safety of the first long-acting atypical antipsychotic. Am J Psychiatry 2003; 160: 1125–1132.
Lindenmayer JP, Jarboe K, Bossie CA, Zhu Y, Mehnert A, Lasser R . Minimal injection site pain and high patient satisfaction during treatment with long-acting risperidone. Int Clin Psychopharmacol 2005; 20: 213–221.
Biedermann F, Fleischhacker WW, Kemmler G, Ebenbichler CF, Lechleitner M, Hofer A . Sibutramine in the treatment of antipsychotic-induced weight gain: a pilot study in patients with schizophrenia. Int Clin Psychopharmacol 2014; 29: 181–184.
Abilify Maintena US (aripiprazole). Full Prescribing Information, Otsuka Pharmaceutical Co., Ltd: Tokyo, Japan, 2014.
Abilify Maintena EU (aripiprazole). Full Prescribing Information, Otsuka Pharmaceutical Europe Ltd: Wexham, UK, 2013.
Abilify Maintena CAN (aripiprazole). Full Prescribing Information, Otsuka Canada Pharmaceutical Inc.: Saint-Laurent, QC, Canada, 2014.
Attard A, Olofinjana O, Cornelius V, Curtis V, Taylor D . Paliperidone palmitate long-acting injection--prospective year-long follow-up of use in clinical practice. Acta Psychiatr Scand 2014; 130: 46–51.
Fleischhacker WW, Eerdekens M, Karcher K, Remington G, Llorca PM, Chrzanowski W et al. Treatment of schizophrenia with long-acting injectable risperidone: a 12-month open-label trial of the first long-acting second-generation antipsychotic. J Clin Psychiatry 2003; 64: 1250–1257.
Sliwa JK, Bossie CA, Fu DJ, Turkoz I, Alphs L . Long-term tolerability of once-monthly injectable paliperidone palmitate in subjects with recently diagnosed schizophrenia. Neuropsychiatr Dis Treat 2012; 8: 375–385.
Tandon R, Marcus RN, Stock EG, Riera LC, Kostic D, Pans M et al. A prospective, multicenter, randomized, parallel-group, open-label study of aripiprazole in the management of patients with schizophrenia or schizoaffective disorder in general psychiatric practice: Broad Effectiveness Trial With Aripiprazole (BETA). Schizophr Res 2006; 84: 77–89.
Wolf J, Janssen F, Lublin H, Salokangas RK, Allain H, Smeraldi E et al. A prospective, multicentre, open-label study of aripiprazole in the management of patients with schizophrenia in psychiatric practice in Europe: Broad Effectiveness Trial with Aripiprazole in Europe (EU-BETA). Curr Med Res Opin 2007; 23: 2313–2323.
Acknowledgements
Editorial support for the preparation of this manuscript was provided by Amy Roth Shaberman, PhD, of C4 MedSolutions, LLC (Yardley, PA, USA), a CHC Group company, with funding from Otsuka Pharmaceutical Development & Commercialization, Inc. and H. Lundbeck A/S. This research was supported by Otsuka Pharmaceutical Development & Commercialization, Inc. and H. Lundbeck A/S.
Author information
Authors and Affiliations
Contributions
All authors critically reviewed manuscript drafts and approved the final draft of the manuscript. In addition, NJ was responsible for data analysis and interpretation; AD was responsible for the clinical management of the study; and TP-S was the project lead and medical monitor for the study, and will act as the guarantor for this manuscript.
Corresponding author
Ethics declarations
Competing interests
TP-S, RAB, NJ, PP, BRJ, AD, and RS are employees of Otsuka Pharmaceutical Development & Commercialization, Inc. RDM is an employee of Otsuka America Pharmaceutical Inc. AE is an employee of Lundbeck LLC.
Additional information
Previous presentations of data: American Psychiatric Association (APA) Annual Meeting; May 3–7, 2014; New York, NY, USA. New Research Approaches for Mental Health Interventions (NCDEU) Annual Meeting; June 16–19, 2014; Hollywood, FL, USA. European College of Neuropsychopharmacology (ECNP) Congress; October 18–22, 2014; Berlin, Germany.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Peters-Strickland, T., Baker, R., McQuade, R. et al. Aripiprazole once-monthly 400 mg for long-term maintenance treatment of schizophrenia: a 52-week open-label study. npj Schizophr 1, 15039 (2015). https://doi.org/10.1038/npjschz.2015.39
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/npjschz.2015.39
This article is cited by
-
The use of long-acting Aripiprazole in a multi-center, prospective, uncontrolled, open-label, cohort study in Germany: a report on global assessment of functioning and the WHO wellbeing index
BMC Psychiatry (2020)
-
Pharmacokinetics, Safety, and Tolerability of a 2-Month Dose Interval Regimen of the Long-Acting Injectable Antipsychotic Aripiprazole Lauroxil: Results From a 44-Week Phase I Study
CNS Drugs (2020)