Abstract
Background:
Many cases of chronic obstructive pulmonary disease (COPD) are diagnosed only after significant loss of lung function or during exacerbations.
Aims:
This study is part of a multi-method approach to develop a new screening instrument for identifying undiagnosed, clinically significant COPD in primary care.
Methods:
Subjects with varied histories of COPD diagnosis, risk factors and history of exacerbations were recruited through five US clinics (four pulmonary, one primary care). Phase I: Eight focus groups and six telephone interviews were conducted to elicit descriptions of risk factors for COPD, recent or historical acute respiratory events, and symptoms to inform the development of candidate items for the new questionnaire. Phase II: A new cohort of subjects participated in cognitive interviews to assess and modify candidate items. Two peak expiratory flow (PEF) devices (electronic, manual) were assessed for use in screening.
Results:
Of 77 subjects, 50 participated in Phase I and 27 in Phase II. Six themes informed item development: exposure (smoking, second-hand smoke); health history (family history of lung problems, recurrent chest infections); recent history of respiratory events (clinic visits, hospitalisations); symptoms (respiratory, non-respiratory); impact (activity limitations); and attribution (age, obesity). PEF devices were rated easy to use; electronic values were significantly higher than manual (P<0.0001). Revisions were made to the draft items on the basis of cognitive interviews.
Conclusions:
Forty-eight candidate items are ready for quantitative testing to select the best, smallest set of questions that, together with PEF, can efficiently identify patients in need of diagnostic evaluation for clinically significant COPD.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is one of the most common lung conditions seen in clinical practice and the fourth leading cause of death worldwide.1 Internationally, data suggest that only a fraction of those with COPD (9 to 22%) have been diagnosed.2 In the United States, analyses of data from the Third National Health and Nutrition Examination Survey (NHANES 2007–2010) found that fewer than 50% of adults with airflow obstruction have been told they have COPD.3
Goals of COPD management include relieving symptoms, improving exercise capacity and reducing the risk of acute exacerbations of COPD.4–6 Long-acting inhaled therapies, supplemental oxygen and pulmonary rehabilitation are particularly beneficial to symptomatic patients and to those with a forced expiratory volume in one second (FEV1) less than 60% predicted.6 Exacerbations are common and costly events associated with decline in lung function,7–9 impaired health-related quality of life10,11 and death.12 A history of acute exacerbations of COPD represents the most important risk factor for subsequent events,13 with treatments available to decrease frequency and improve outcomes.4,12
There is evidence suggesting that many patients are first diagnosed with COPD when their airway obstruction has progressed substantially or during an acute respiratory illness.14–19 Studies in primary care suggest that the proportion of newly diagnosed COPD patients with moderate-to-severe airway obstruction in primary care ranges from 43% (Scotland, Colorado)15 to 70% (Greece).16 A United States managed care database analysis suggested that 31% were GOLD III or IV,17 whereas a study in China found that 86% were moderate to severe and 34% had ⩾2 exacerbations the prior year.18 Exacerbation history is further exemplified by a study in France where investigators found that 96% of patients with newly diagnosed chronic bronchitis had been treated with antibiotics for similar episodes in the past year and 41% had at least two such episodes.19 Identifying individuals with undiagnosed clinically significant COPD (FEV1 <60% predicted or exacerbation risk) should set in motion effective medical treatment and improve short- and long-term health outcomes.
Several instruments have been proposed for COPD case identification, defined by airflow limitation (FEV1/FVC (forced vital capacity) <0.70) without reference to exacerbation risk.20–32 Methods used to develop these instruments vary widely. Target and test populations range from those with a history of cigarette smoking only21,25,29 to populations of smokers and non-smokers,20,22,26,27,30,32 and settings that include primary care, specialty clinics20–22,26,28,30 and general population screening.25,29,32 A few of these development studies have utilised qualitative research methods to inform and refine instrument structure and content22,27,28 or tested the use of peak expiratory flow (PEF) along with a questionnaire to enhance precision.29–32
A 2008 National Institutes of Health (NIH)-COPD Foundation workshop suggested a three-stage approach for identifying undiagnosed individuals with moderate-to-severe airflow obstruction (FEV1 <60%): a questionnaire to eliminate those unlikely to have severe disease, a simple measure of expiratory airflow to exclude those with normal or near-normal pulmonary function, and diagnostic evaluation, including clinical assessment and spirometry.33 Nelson et al.32 tested the effectiveness of this approach, by screening 5,638 diagnosed and undiagnosed individuals from the general population attending public events. In this setting, 6.3% of 3,791 with ⩾2 risk factors had abnormal PEF, suggesting that a more sensitive questionnaire is needed.
We are developing a new screening method for identifying cases of clinically significant COPD (FEV1 <60% and/or at risk for acute exacerbations of COPD) in primary care settings. The two-step process will include a questionnaire and pre-bronchodilator peak flow (PEF) to identify patients in need of further diagnostic evaluation. PEF will be measured using a familiar, inexpensive and widely available device for estimating the presence of airflow obstruction.31–33 Development methods for the questionnaire included a review of the literature,34 analyses of three existing COPD data sets using random forests methodology35 and qualitative research with individuals from the target population.
This paper presents the qualitative research used to inform thematic content, format, instructions and candidate items for the screening questionnaire. The intent was to develop a comprehensive pool of items for empirical testing, maximising content validity by using words and phrases easily understood by men and women in the target population. Ease of use and equivalence of two PEF metres were also assessed.
Materials and Methods
Study design
This was a two-phase qualitative study: Phase I (elicitation) included focus groups and interviews, and Phase II involved cognitive interviews (see Online Supplementary).
Sample
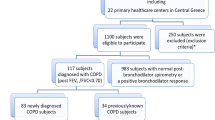
The Phase I sample included participants from one of four categories (see Table 1). COPD severity was based on airflow obstruction, defined by the Global Initiative for Chronic Obstructive Lung Disease (GOLD),36 and risk factors based on the literature and data mining. Subjects in categories (groups) 1 and 2 provided information on symptoms, risk factors, history and other breathing-related issues from the perspective of people recently diagnosed with clinically significant COPD—the target population. Groups 3 and 4 were designed to provide insight into how experienced (risk factor) but non-COPD (diagnosis naive) subjects describe their respiratory symptoms, risk factors, history and other breathing-related issues.
Inclusion criteria were as follows: ⩾40 years old; stable state spirometry (FEV1, FEV1% predicted, FEV1/FVC) in the past 12 months (on file or willing to undergo spirometry at the time of data collection); and able to attend a focus group or telephone interview, read and speak English and to provide written informed consent. Individuals were not eligible if they had physical or psychological impairments precluding participation or were hospitalised for a respiratory infection within the past 30 days. Current smokers (⩾10 pack-years), ex-smokers (history of ⩾10 pack-years) and never smokers (⩽100 cigarettes/pipes/cigars in a lifetime) were included.
Procedures
Participants were recruited from four pulmonary clinics and one primary care clinic in the United States. Convenience sampling was used; clinical members of the Study Group approached potential participants by phone or during clinic visits. Efforts were made to recruit a diverse sample in terms of age, smoking status and history, gender, race/ethnicity and educational level. The protocol was approved by a central Institutional Review Board and local Institutional Review Board at each site; written informed consent was obtained from all the participants.
Focus groups and interviews
Focus groups were held in a private room in the clinic; interviews were conducted by telephone. Experienced, trained research staff used a semi-structured interview guide to facilitate discussion. The guide included open-ended questions asking participants to describe their breathing-related symptoms and COPD risk-related experiences; COPD patients were also asked to consider these issues relative to their recent diagnosis. Sample questions for the COPD Groups (1 and 2) included the following: ‘Looking back, were there any ‘signals’ that suggested you might have a breathing condition?’ and ‘What symptoms or experiences did you have that led you to believe you might have a breathing problem?’ Sample questions for those without COPD (3 and 4) included the following: ‘Describe your breathing for us. Are there any other symptoms you associate with your breathing?’ and ‘Can you think of any other experiences related to the symptoms we just discussed?’
Two researchers were present during focus groups: one served as moderator (LTM), while the second observed and took field notes (KK or AWS). Groups lasted 1.5–2 h, with breaks taken as needed. Telephone interviews were 1:1 (LTM, KK or AWS), with the interviewer taking notes, and they lasted for 20–50 min. Focus groups and interviews were audio-recorded and transcribed verbatim, with the data cleaned and de-identified for analyses.
Peak expiratory flow
Following each focus group or interview, clinical staff performed PEF on each participant using electronic (Vitalograph Asma-1 USB, Lenexa, KS, USA) and manual (Vitalograph AsmaPlan mech PFM) devices. Order of administration was randomised; SafeTway disposable mouthpieces were used. Upon completion, participants and staff completed ease-of-use ratings (very easy, easy, neither difficult nor easy, difficult or very difficult to use).
Demographic and clinical measures
Participants also completed a sociodemographic and clinical history form, the RAND 36-Item Short Form Health Survey (SF-36)37 and the COPD Assessment Tool,38 a 10- to 15 -min activity following the focus group or interview. Spirometric values (FEV1, FEV1% predicted, FEV1/FVC) were obtained for all subjects, either from clinical charts (COPD groups) or by clinical site staff, at the time of the focus group or interview (no bronchodilation).
Data analysis
Using a content analysis approach, data (transcripts) were examined for key themes and constructs. A coding dictionary was developed and ATLAS.ti (version 7.1) was used to organise data. Two analysts independently coded the first transcript, and codes were compared and reconciled with senior scientific oversight. Terms and definitions in the coding dictionary were then refined for clarity. The remaining transcripts were coded thematically by one analyst and reviewed by a second analyst, with discrepancies resolved through discussion with the senior analyst. Saturation was defined by consistency of themes, construct descriptions or terms across groups and interviews.
Descriptive statistics were used to summarise sample characteristics, PEF values and PEF ease of use. A two-way analysis of variance was used to determine whether there was a significant difference between electronic and manual PEF values for participants with and without COPD. Paired-sample t-tests were used to compare PEF values between the electronic and manual devices within groups.
Item pool development and cognitive interviewing
Results were examined together with those from the literature review34 and data mining35 to inform the development of a pool of candidate questions for further evaluation and testing. Items were generated using an iterative process of development, review, revision, discussion and revision, with input from the High-Risk-COPD Screening Study Group. Candidate questions with instructions were formatted in a questionnaire layout and evaluated by a new set of subjects from the target population using cognitive interviewing methodology (see Online Supplementary).
Results
Eight focus groups (n=44) and six one-on-one telephone interviews (n=6) were conducted. Sample characteristics are summarised in Tables 2 and 3. For the COPD patients, mean post-bronchodilator FEV1 was 68% predicted (s.d.=10) (mean FEV1=2.2 l (s.d.=0.8)), and time since diagnosis averaged three months.
Spirometric values for three cases in the non-COPD groups suggested possible airway obstruction; these participants were referred to their physician for follow-up. In two cases, spirometry was performed after their focus groups. The third case was uncovered after screening and enrolment, and the decision was made to have him participate in the originally assigned no-COPD group so that he could share his experiences in an environment of people without COPD experience. Data from these three cases were also examined separately, comparing their responses with others.
Six major themes were identified in the data: (1) exposure to smoke and other pollutants (e.g., chemicals, paint, gasoline), either through a friend/relative, work environment or living condition; (2) personal and family history of respiratory health conditions, such as emphysema, pneumonia, frequent colds and sinus infections; (3) recent history of respiratory events, including factors that may trigger an event (perfumes, cigarette smoke, exertion) and recent clinic visits or hospitalisations owing to respiratory symptoms such as shortness of breath, coughing and chest tightness that continued to worsen; (4) symptoms, including respiratory (e.g., shortness of breath with and without exertion, sputum and phlegm production, wheezing, chest tightness and congestion) and nonrespiratory (e.g., feeling tired after slight exertion, low energy, sleeping problems such as waking up at night feeling short of breath); (5) impact of breathing-related problems on daily life (e.g., slowing down or stopping owing to breathlessness, unable to complete daily chores, unable to keep up with others); and (6) the attribution of symptoms or experiences (e.g., breathless, being tired or slowing down attributed to age or weight; cough attributed to smoking or smoke exposure).
Themes were consistent across COPD and non-COPD participants, with some cross-group variation in emphasis within each theme. Spontaneous symptom reporting rates were generally lowest for Group 3 (non-COPD ⩽2 risk factors); rates for Group 4 (non-COPD, ⩾4 risk factors) were similar to the COPD groups on sputum/phlegm (100%); tight, wheezy or noisy chest (90%); slowing down (40%); fatigue (50%); and sleep problems (40%). No qualitative differences were found between data provided by the three subjects with evidence of airway obstruction and other participants. Sample quotes for each theme are shown in Table 4. Candidate item content is shown in Table 5.
Electronic and manual PEF devices were rated as ‘easy’ or ‘very easy’ to use by participants (96%; 94%) and clinical site staff (80%; 84%). PEF values by device and group are shown in Table 6.
With the data analysed, a draft questionnaire with 48 candidate items was constructed and subjected to cognitive interviewing in a separate sample of 27 subjects. The instructions and item pool were easily understood and appropriately interpreted by the subjects; several adjustments were made to enhance clarity. PEF results were similar to those found in the elicitation sample (see Online Supplementary).
Discussion
Main findings
This qualitative study is part of a larger multi-method approach to develop a screening method for identifying patients with undiagnosed, clinically significant COPD in primary care. Six key themes were identified; candidate items were developed, using words and phrases easily understood by people in the target population. Although participants and clinical staff rated the two PEF devices easy to use, values produced by the electronic device were significantly higher than those provided by the manual device.
Strengths and limitations of this study
This is among the first known uses of qualitative data to inform the development of a screening tool for COPD case identification in a clinical setting. The study included men and women with varied COPD experiences, risk factors and education. The fact that all subjects were from the United States and most were white (70%) and not Hispanic or Latino (92%) is a limitation of the study. In addition, although a larger number of subjects with undiagnosed COPD would have been ideal, a study design that explicitly included screening and identifying subjects with undiagnosed clinically significant COPD (using methods not designed for this purpose) would have been cost-prohibitive. The fact that all moderators and interviewers were female may have influenced participant responses, although staff were experienced and trained to encourage discussion and minimise bias.
Interpretation of findings in relation to previously published work
The attribution theme offers insight into why certain symptoms are not reported or recognised as indicators of COPD. Participants who smoked often attributed their cough to smoking; others attributed slowing down, feeling tired or becoming breathless with exertion to ageing, weight or other health issues. These findings are consistent with descriptions of barriers to diagnosis;39 quantitative evidence that symptom-based diagnosis of COPD in primary care settings is unreliable, particularly if patients are overweight;40 and qualitative research suggesting that people minimise and negotiate the importance of symptoms and need to acknowledge ‘there must be something wrong’ as part of the diagnostic process.41
Most of the respiratory symptoms identified in this study were consistent with existing, symptom-based questionnaires for identifying undiagnosed COPD. Cough, phlegm, dyspnoea and wheeze,21–23 as well as history of chest infections, breathing-related disability or hospitalisations,23,24 for example, were broached and characterised by these participants. In addition, however, subjects described chest symptoms, including congestion, noisy or tight, as well as feelings of fatigue and sleep difficulties. Participant descriptions of family history of respiratory-related problems, symptoms, activity limitations and acute respiratory illnesses offer new insight into candidate items for identifying undiagnosed cases of clinically significant COPD.
Smokers and non-smokers were included to facilitate the use of the questionnaire in both groups. There is evidence to suggest that one-fourth to one-third of all COPD cases are non-smokers, with country-to-country variability.42 The international study of Lamprecht et al.42 found that 81% of never smokers with moderate-to-severe airway obstruction were undiagnosed. The study of Bednarek et al.2 in Poland suggested that detection of COPD is reduced by 26% when a ‘smokers only’ criterion is used, whereas in the Third US NHANES database, ‘never smokers’ accounted for 23% of airway obstruction cases, 69% of whom had no prior respiratory diagnosis.43
Sample clinical characteristics provide further qualitative insight into the challenges associated with variable selection for case identification. Descriptively, the frequency of breathing-related symptoms (e.g., cough, shortness of breath) and other risk factors (e.g., history of asthma, family history of breathing problems) were similar across groups. The COPD group reported more breathing events over the past year (e.g., cold, chest infection). Although there were no significant differences in health status between the two groups, the descriptively higher COPD Assessment Test scores for COPD subjects suggest a trend toward poorer health in areas specific to COPD, with the mean between-group difference exceeding the proposed two-point minimum clinically important difference.44 These exploratory results suggest that a small set of targeted questions may be more effective than a large number of general health questions for identifying people with COPD.
Implications for future research, policy and practice
As part of our screening tool development, we will be testing the added value of including PEF to increase sensitivity and specificity. To facilitate and optimise utilisation of PEF as part of the screening process, we evaluated the usability and comparability of electronic and manual devices. Most patients and clinic staff rated the devices easy or very easy to use, suggesting that either might be suitable. However, differences in PEF values indicate a need for standardisation to simplify the process by providing a single threshold for interpretation. With cost and availability in mind, the manual PEF device will be tested further during the next phase of screening tool development. The questionnaire’s sensitivity and specificity will be optimised independently of PEF, and thus those preferring to use FEV1 or PEF captured through an electronic/digital device would be free to do so, applying their preferred threshold for follow-up evaluation.
Conclusions
This qualitative study is part of a multi-method approach for developing a new screening method for identifying primary care patients who may have undiagnosed, clinically significant COPD. Six themes were identified: exposure, personal and family health, recent history of respiratory events, respiratory and non-respiratory symptoms, impact, and attribution. A pool of 48 candidate items was developed and revised based on cognitive interview results. Items will be tested and eliminated during the next phase of instrument development, with the intent of finding the best, smallest set of questions that, together with PEF, can identify patients in need of diagnostic evaluation for COPD.
References
Mathers CD, Loncar D . Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006; 3: e442.
Bednarek M, Maciejewski J, Wozniak M, Kuca P, Zielinski J . Prevalence, severity and underdiagnosis of COPD in the primary care setting. Thorax 2008; 63: 402–407.
Ford ES, Mannino DM, Wheaton AG, Giles WH, Presley-Cantrell L, Croft JB . Trends in the prevalence of obstructive and restrictive lung function among adults in the United States: findings from the National Health and Nutrition Examination surveys from 1988–1994 to 2007–2010. Chest 2013; 143: 1395–1406.
Gruffydd-Jones K, Loveridge C . The 2010 NICE COPD guidelines: how do they compare with the GOLD guidelines? Prim Care Respir J 2011; 20: 199–204.
Postma D, Anzueto A, Calverley P, Jenkins C, Make B, Sciurba F et al. A new perspective on optimal care for patients with COPD. Prim Care Respir J 2011; 20: 205–209.
Wilt T, Niewoehner D, MacDonald R, Kane R . Management of stable chronic obstructive pulmonary disease: a systematic review for a clinical practice guideline. Ann Int Med 2007; 147: 639–653.
Donaldson GC, Seemungal TA, Patel IS, Lloyd-Owen SJ, Wilkinson TM, Wedzicha JA . Longitudinal changes in the nature, severity and frequency of COPD exacerbations. Eur Respir J 2003; 22: 931–936.
Halpin DM, Decramer M, Celli B, Kesten S, Liu D, Tashkin DP . Exacerbation frequency and course of COPD. Int J Chron Obstruct Pulmon Dis 2012; 7: 653–661.
Vestbo J, Edwards LD, Scanlon PD, Yates JC, Agusti A, Bakke P et al. Changes in forced expiratory volume in 1 s over time in COPD. N Engl J Med 2011; 365: 1184–1192.
Bourbeau J, Ford G, Zackon H, Pinsky N, Lee J, Ruberto G . Impact on patients' health status following early identification of a COPD exacerbation. Eur Respir J 2007; 30: 907–913.
Xu W, Collet JP, Shapiro S, Lin Y, Yang T, Wang C et al. Negative impacts of unreported COPD exacerbations on health-related quality of life at 1 year. Eur Respir J 2010; 35: 1022–1030.
Anzueto A, Sethi S, Martinez FJ . Exacerbations of chronic obstructive pulmonary disease. Proc Am Thorac Soc 2007; 4: 554–564.
Hurst J, Vestbo J, Anzueto A, Locantore N, Mullerova H, Tal-Singer R et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med 2010; 363: 1128–1138.
Bastin AJ, Starling L, Ahmed R, Dinham A, Hill N, Stern M et al. High prevalence of undiagnosed and severe chronic obstructive pulmonary disease at first hospital admission with acute exacerbation. Chron Respir Dis 2010; 7: 91–97.
Tinkelman DG, Price D, Nordyke RJ, Halbert RJ . COPD screening efforts in primary care: what is the yield? Prim Care Respir J 2007; 16: 41–48.
Minas M, Hatzoglou C, Karetsi E, Papaioannou AI, Tanou K, Tsaroucha R et al. COPD prevalence and the differences between newly and previously diagnosed COPD patients in a spirometry program. Prim Care Respir J 2010; 19: 363–370.
Mapel DW, Dalal AA, Blanchette CM, Petersen H, Ferguson GT . Severity of COPD at initial spirometry-confirmed diagnosis: data from medical charts and administrative claims. Int J Chron Obstruct Pulmon Dis 2011; 6: 573–581.
Gao Y, Hou Q, Wang H . Assessment of health status in patients with newly diagnosed chronic obstructive pulmonary disease. PLoS One 2013; 8: e82782.
Roche N, Gaillat J, Garre M, Meunier J, Lemaire N, Bendjenana H . Acute respiratory illness as a trigger for detecting chronic bronchitis in adults at risk of COPD: a primary care survey. Prim Care Respir J 2010; 19: 371–377.
van Schayck C, Loozen J, Wagena E, Akkermans R, Wesseling G . Detecting patients at high risk of developing chronic obstructive pulmonary disease in general practice: cross sectional case finding study. BMJ 2002; 324: 1370–1375.
Freeman D, Nordyke R, Isonaka S, Nonikov V, Maroni J, Price D et al. Questions for COPD diagnostic screening in a primary care setting. Respir Med 2005; 99: 1311–1318.
Price D, Tinkelman D, Halbert R, Nordyke R, Isonaka S, Nonikov D et al. Symptom-based questionnaire for identifying chronic obstructive pulmonary disease in smokers. Respiration 2006; 73: 285–295.
Tinkelman D, Price D, Nordyke R, Halbert R, Isonaka S, Nonikov D et al. Symptom-based questionnaire for differentiating COPD and asthma. Respiration 2006; 73: 296–305.
Price D, Tinkelman D, Nordyke R, Isonaka S, Halbert R for the COPD Questionnaire Study Group. Scoring system and clininical application of COPD diagnostic questionnaires. Chest 2006; 129: 1531–1539.
Kotz D, Nelemans P, van Schayck C, Wesseling G . External validation of a COPD diagnostic questionnaire. Eur Respir J 2008; 31: 298–303.
Martinez F, Raczek A, Seifer F, Conoscenti C, Colice T, D'Eletto T et al. Development and initial validation of a self-scored COPD population screener questionnaire (COPD-PS). COPD 2008; 5: 85–95.
Yawn B, Mapel D, Mannino D, Martinez F, Donohue J, Hanania N et al. Development of the Lung Function Questionnaire (LFQ) to identify airflow obstruction. Int J Chron Obstruct Pulmon Dis 2010; 5: 1–10.
Hanania N, Mannino D, Yawn B, Mapel D, Martinez F, Donohue J et al. Predicting risk of airflow obstruction in primary care: validation of the lung function questionnaire (LFQ). Respir Med 2010; 104: 1160–1170.
Frith P, Crockett A, Beilby J, Marshall D, Attewell R, Ratnanesan A et al. Simplified COPD screening: validation of the Piko-6® in primary care. Prim Care Respir J 2011; 20: 190–198.
Sichletidis L, Spyratos D, Papaioannou M, Chloros D, Tsiotsios A, Tsagaraki V et al. A combination of the IPAG questionnaire and Piko-6® flow meter is a valuable screening tool for COPD in the primary care setting. Prim Care Respir J 2011; 20: 184–189.
Jithoo A, Enright PL, Burney P, Buist AS, Bateman ED, Tan WC et al. Case-finding options for COPD: results from the Burden of Obstructive Lung Disease study. Eur Respir J 2013; 41: 548–555.
Nelson SB, LaVange LM, Nie Y, Walsh JW, Enright PL, Martinez FJ et al. Questionnaires and pocket spirometers provide an alternative approach for COPD screening in the general population. Chest 2012; 142: 358–366.
Martinez FJ . NHLBI Workshop: A Case-finding Strategy for Moderate-to-Severe COPD in the United States Executive Summary. November 2009. http://www.nhlbi.nih.gov/research/reports/2009-case-finding-exesum.htm. Accessed 6 November 2014.
Han M, Steenrod A, Dansie EJ, Leidy N, Mannino D, Thomashow BM et al. Identifying patients with undiagnosed COPD in primary care settings: insight from screening tools and epidemiologic studies. J COPD F (in press).
Leidy N, Malley K, Steenrod A, Mannino D, Make B, Bowler R et al. Identifying best variables for COPD case identification in primary care: a random forests analysis (under review).
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for diagnosis, management and prevention of COPD. 2014. http://www.goldcopd.org. Accessed 6 November 2014.
Ware JE Jr, Sherbourne CD . The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992; 30: 473–483.
Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N . Development and first validation of the COPD Assessment Test. Eur Respir J 2009; 34: 648–654.
Fromer L . Diagnosing and treating COPD: understanding the challenges and finding solutions. Int J Gen Med 2011; 4: 729–739.
Walters JA, Walters EH, Nelson M, Robinson A, Scott J, Turner P et al. Factors associated with misdiagnosis of COPD in primary care. Prim Care Respir J 2011; 20: 396–402.
Lindgren S, Storli SL, Wiklund-Gustin L . Living in negotiation: patients' experiences of being in the diagnostic process of COPD. Int J Chron Obstruct Pulmon Dis 2014; 9: 441–451.
Lamprecht B, McBurnie MA, Vollmer WM, Gudmundsson G, Welte T, Nizankowska-Mogilnicka E et al. COPD in never smokers: results from the population-based burden of obstructive lung disease study. Chest 2011; 139: 752–763.
Celli BR, Halbert RJ, Nordyke RJ, Schau B . Airway obstruction in never smokers: results from the Third National Health and Nutrition Examination Survey. Am J Med 2005; 118: 1364–1372.
Kon SS, Canavan JL, Jones SE, Nolan CM, Clark AL, Dickson MJ et al. Minimum clinically important difference for the COPD Assessment Test: a prospective analysis. Lancet Respir Med 2014; 2: 195–203.
Acknowledgements
The authors thank Sarah Clifford for her comments during protocol development and Kathryn Miller for text editing and formatting the protocol and manuscript.
High-risk-COPD screening study group
Rebecca Copeland, University of Kentucky; Tim Dorius, University of Nebraska Medical Center; David Hengerer, Evidera; Patricia Jellen, New York Presbyterian Hospital; Marge Kurland, Olmsted Medical Center; Karen Malley, Evidera; Jason Shiffermiller, University of Nebraska Medical Center; Christina Schnell, National Jewish Health; Lori Silveira, National Jewish Health; Sonja Stringer, Evidera; Deb Sumnick, University of Nebraska; Randel Plant, COPD Foundation; Jennifer Underwood, National Jewish Health; Beth Whippo, New York Presbyterian Hospital.
Funding
Funding for this work was provided by the National Heart, Lung, and Blood Institute NHLBI: R01 HL 114055. Additional support was provided by NHLBI:R01 HL089856 and R01 HL089897.
Author information
Authors and Affiliations
Consortia
Contributions
Each named author participated in the study design and data analyses and interpretation. BPY, DMM, BMT, RGB, SIR, JFH, MKH, CAM, RPB and FM also participated in subject recruitment and data collection activities; LTM, KK and AWS served as focus group moderators, field note takers and interviewers. NKL, EDB, KK, AWS and LTM contributed to data management, analyses and interpretation. All the authors participated in manuscript development, review and/or editing. NKL, DMM and FM serve as co-investigators of the grant and, together with the co-authors, attest to the accuracy of the information contained in this manuscript.
Corresponding author
Ethics declarations
Competing interests
NKL, EDB, KK, AWS and LTM are employees of Evidera, a health care research firm that provides consulting and other research services to pharmaceutical, device, government and non-government organisations. In this salaried position, they work with a variety of companies and organisations and receive no payment or honoraria directly from these organisations for services rendered. BPY has received research funding from NIH, AHRQ, CDC and from BI for research on COPD. BPY has received compensation from Merck and Forrest for COPD advisory boards on COPD, and Grifols for advisory board on Alpha-1 antitrypsin deficiency states. DMM has received honoraria/consulting fees and served on speaker bureaus for GlaxoSmithKline PLC, Novartis Pharmaceuticals, Pfizer Inc., Boehringer-Ingelheim, AstraZeneca PLC, Forest Laboratories Inc., Merck, Amgen and Creative Educational Concepts. Furthermore, he has received royalties from UptoDate and is on the Board of Directors of the COPD Foundation. BMT has consulted for Boehringer-Ingelheim and has been on advisory boards for GlaxoSmithKline PLC, Novartis, AstraZeneca PLC and Forest. RGB received grant support from NIH, US-EPA and the Alpha1 Foundation; he has received royalties from UpToDate. SIR has had or currently has a number of relationships with companies who provide products and/or services relevant to outpatient management of chronic obstructive pulmonary disease, including AARC, American Board of Internal Medicine, Able Associates, Align2 Acton, Almirall, APT, AstraZeneca, American Thoracic Society, Beilenson, Boehringer Ingelheim, Chiesi, CIPLA, Clarus Acuity, CME Incite, COPD Foundation, Cory Paeth, CSA, CSL Behring, CTS Carmel, Dailchi Sankyo, Decision Resources, Dunn Group, Easton Associates, Elevation Pharma, FirstWord, Forest, GLG Research, Gilead, Globe Life Sciences, GlaxoSmithKline, Guidepoint, Health Advance, HealthStar, HSC Medical Education, Johnson and Johnson, Leerink Swan, LEK, McKinsey, Medical Knowledge, Medimmune, Merck, Navigant, Novartis, Nycomed, Osterman, Pearl, PeerVoice, Penn Technology, Pennside, Pfizer, Prescott, Pro Ed Communications, PriMed, Pulmatrix, Quadrant, Regeneron, Saatchi and Saatchi, Sankyo, Schering, Schlesinger Associates, Shaw Science, Strategic North, Summer Street Research, Synapse, Takeda, Telecon SC, ThinkEquity; these relationships include serving as a consultant, advising regarding clinical trials, speaking at continuing medical education programmes and performing funded research both at basic and clinical levels. SIR does not own any stock in any pharmaceutical companies. JFH declares no conflict of interest. MKH has consulted for GSK, Boehringer-Ingelheim and Regeneron. She has served on speaker bureaus for GSK, Novartis, Boehringer-Ingelheim, Forest and Grifols. CAM declares no conflict of interest. BJM has participated in research studies and/or served on medical advisory boards for AstraZeneca, Boehringer-Ingelheim, CSL Bering, GlaxoSmithKline, Forest, Novartis, Spiration and Sunovion. The work of RPB has been funded by the NIH, FAMRI, Butcher Foundation and John W. Carson Foundation. He participates in AstraZeneca- and GSK-sponsored clinical trials. He has received compensation as a member of scientific advisory boards of Boehringer Ingelheim Pharmaceutical. JWW declares no conflict of interest. FM has participated in Steering Committee in COPD or IPF sponsored by Bayer, Centocor, Forest, Gilead, Janssens, GSK, Nycomed/Takeda and Promedior. He has participated in advisory boards for COPD or IPF for Actelion, Amgen, AstraZeneca, Boehringer Ingelheim, Carden Jennings, CSA Medixcal, Ikaria, Forest, Genentech, GSK, Janssens, Merck, Pearl, Nycomed/Takeda, Pfizer, Roche, Sudler & Hennessey, Veracyte and Vertex. He has prepared or presented continuing medical presentations in COPD or IPF for the American College of Chest Physicians, the American Thoracic Society, CME Incite, Center for Health Care Education, Inova Health Systems, MedScape, Miller Medical, National Association for Continuing Education, Paradigm, Peer Voice, Projects in Knowledge, Spectrum Health System, St John’s Hospital, St Mary’s Hospital, University of Illinois Chicago, University of Texas Southwestern, University of Virginia, UpToDate and Wayne State University. FM has participated in data safety monitoring committees sponsored by GSK and Stromedix. He has aided with FDA presentations sponsored by Boehringer Ingelheim, GSK and Ikaria. He has spoken on COPD for Bayer, Forest, GSK and Nycomed/Takeda. He has participated in advisory teleconferences sponsored by the American Institute for Research, Axon, Grey Healthcare, Johnson & Johnson and Merion. He has received book royalties from Informa.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Leidy, N., Kim, K., Bacci, E. et al. Identifying cases of undiagnosed, clinically significant COPD in primary care: qualitative insight from patients in the target population. npj Prim Care Resp Med 25, 15024 (2015). https://doi.org/10.1038/npjpcrm.2015.24
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/npjpcrm.2015.24
This article is cited by
-
Case-finding for COPD clinic acceptability to patients in GPs across Hampshire: a qualitative study
npj Primary Care Respiratory Medicine (2021)
-
Development and validation of the Salzburg COPD-screening questionnaire (SCSQ): a questionnaire development and validation study
npj Primary Care Respiratory Medicine (2017)
-
A retrospective study of two populations to test a simple rule for spirometry
BMC Family Practice (2016)