Abstract
Background:
With a growing availability of different devices and types of medication, additional evidence is required to assist clinicians in prescribing the optimal medication in relation to chronic obstructive pulmonary disease (COPD) patients’ persistence with long-acting β2-agonists (LABAs).
Aims:
To assess the impact of the type of inhaler device (multiple-dose versus single-dose inhalers) on 1-year persistence and switching patterns with LABAs.
Methods:
A retrospective observational cohort study was performed comparing a cohort of patients initiating multiple-dose inhalers and a cohort initiating single-dose inhalers. The study population consisted of long-acting bronchodilator naive COPD patients, initiating inhalation therapy with mono-LABAs (formoterol, indacaterol or salmeterol). Analyses were performed using pharmacy dispensing data from 1994 to 2012, obtained from the IADB.nl database. Study outcomes were 1-year persistence and switching patterns. Results were adjusted for initial prescriber, initial medication, dosing regimen and relevant comorbidities.
Results:
In all, 575 patients initiating LABAs were included in the final study cohort. Among them, 475 (83%) initiated a multiple-dose inhaler and 100 (17%) a single-dose inhaler. Further, 269 (47%) initiated formoterol, 9 (2%) indacaterol and 297 (52%) salmeterol. There was no significant difference in persistence between users of multiple-dose or single-dose inhalers (hazard ratio: 0.98, 95% confidence interval: 0.76–1.26, P=0.99). Over 80% re-started or switched medication.
Conclusions:
There seems no impact of inhaler device (multiple-dose versus single-dose inhalers) on COPD patients’ persistence with LABAs. Over 80% of patients who initially seemed to discontinue LABAs, re-started their initial medication or switched inhalers or medication within 1 year.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) places a high burden on both public health and health-care budgets of patients and the government.1,2 Despite no curative treatment being available, inhaled medication has been shown to reduce disease symptoms.3,4 However, effectiveness of current medication has mainly been assessed in controlled clinical trial settings, which may not properly reflect real-life behavior of patients. Furthermore, these trial populations do not fully represent the characteristics of the average COPD population.5 Both factors contribute to a real-life adherence to COPD medication that is far beyond adherence reported in clinical trials.6,7 Recently, non-adherent patients were highlighted as a target for interventions because of the significant clinical and economic impact of non-adherence on patients with COPD.8 Factors associated with non-adherence with COPD medication include age, comorbidity, disease severity and class of medication.9,10 However, only a few factors may be modified by the prescribing clinician. Compared to the abundant number of adherence studies in asthma patients, studies on patients with COPD are limited.6,7,11–13 In particular, studies assessing the impact of the type of inhaler device on medication adherence in patients with COPD are lacking.14 With a growing availability of different types of medication and inhaler devices, additional evidence is required to assist clinicians in prescribing the optimal medication in relation to their patients’ adherence. Adherence does encompass compliance (the extent of acting according to the prescribers’ advice) and persistence (duration of time from initiation till discontinuation of therapy).15 The objective of this study is to assess the impact of the type of inhalation device on COPD patients’ persistence with, and switching between, long-acting respiratory medication. The focus on persistence was chosen as this could be objectively measured using a dispensing database, whereas compliance would require face-to-face assessment of patients. In particular, we focused on persistence with long-acting β2-agonists (LABAs), where we compared single-dose versus multiple-dose inhalers.
Materials and Methods
Data source
Data were obtained from the InterActionDatabase (IADB.nl, available from http://www.iadb.nl). The IADB.nl database covers pharmacy-dispensing data from over 500,000 patients from 55 community pharmacies located in the Northern Netherlands between 1994 and 2012. Dispensing data contain information on drug name, product specifications, anatomical therapeutic chemical code, prescriber, amount of delivered drug units, daily dose and patient characteristics such as date of birth, gender and socioeconomic status, regardless of health-care insurance status of the patients. Thus, the database is representative for the real-world situation in the Netherlands. Medication dispensed in hospitals is not included. The IADB.nl database has been validated for drug utilisation studies16 and has been used in previous persistence studies.17,18 In the Netherlands, patients usually redeem their prescriptions at the same pharmacy allowing a complete longitudinal follow-up.
Study population
As the database lacked data on clinical diagnosis, COPD patients were selected based on initiation of inhaled respiratory medication above the age of 55 years, in line with previous studies.7,12 Treatment initiation was defined as at least one prescription of LABAs for inhalation (salmeterol (R03AC12), formoterol (R03AC13), or indacaterol (R03AC18)). The group of LABAs was chosen as for this group both dry powder inhalers (DPIs) and pressurised metered dose inhalers are available. Moreover, within the DPI group, both single-dose as well as multiple-dose inhalers are available, making this the group of long-acting bronchodilators where the influence of inhaler device could be most extensively tested. Starters were defined as not having used any long-acting respiratory medications (LABAs, inhaled corticosteroids (ICS) or long-acting muscarinic antagonists) for at least 2 years before treatment initiation. To make sure that a complete overview of history and follow-up was available, patients needed to be registered in the database at least 2 years before and 1 year after initiation of therapy. We only included patients who started one type of inhaled medication at treatment initiation (that is, patients who started a LABA and at the same date ICS or long-acting muscarinic antagonist were excluded). To minimise the possibility to include (late onset) asthma patients, we excluded patients using typical asthma medication (antihistamines (R06), anti-allergics (R03BC), leukotriene receptor antagonists (R03DC), and omaluzimab (R03DX05)) within 1 year after long-acting beta agonist initiation.
Persistence
Continuous drug use in the first year was calculated by the total number of doses dispensed from therapy initiation, divided by the prescribed daily dose. A gap of maximal 60 days without medication coverage within the period of continuous use was allowed to consider a patient being still persistent to medication, that is, patients who did not have any gaps exceeding 60 days in the 1-year period after therapy initiation was considered persistent. This 60-day gap is a common cutoff and was used in various previous studies assessing persistence with COPD medication.6,7
Switching
Part of the nonpersistent patients were those who did discontinue their initial inhaler or medication but did not completely discontinue the use of any long-acting medication at all (that is, they switched therapy). Therefore, follow-up of non-persistent (to initial therapy) patients was monitored by assessing patients’ medication profiles after the date of discontinuation of their initial therapy. For all patients, follow-up was at least 1 year from the date of treatment initiation; however, to be able to assess switching patterns in the year after the date of treatment discontinuation, follow-up needed to be longer. Therefore, we defined a subcohort where patients needed to have a follow-up of at least 2 years. After discontinuation of initial treatment, we assessed the following possibilities: a switch to a different inhaler within the DPI class (that is, from single- to multiple-dose inhaler or vice versa), a switch to a LABA-pressurised metered dose inhaler, a switch to a different bronchodilator class (LABA/ICS or long-acting muscarinic antagonist), a restart with initial type of medication/inhaler or permanent discontinuation of any long-acting bronchodilator.
Defining the single-dose and multiple-dose cohorts
Two cohorts were defined based on the type of LABA-DPI initiated by the patients. We made a distinction between single-dose and multiple-dose DPI inhalers. Single-dose inhalers require loading of separate capsules before using the device.19,20 Examples include the Handihaler, the Cyclohaler, the Rotahaler and the Breezhaler. Multiple-dose inhalers contain a fixed amount of doses (usually between 60 and 120) that can be taken successively until the device runs out of doses. Examples include the Diskus, the Turbuhaler and the Novolizer. We hypothesised that the use of single-dose inhalers required more complex and time-consuming handlings in order to perform proper inhalation and would therefore decrease treatment persistence.
Covariates
Although this study focused on the medication and inhaler devices, persistence may be altered by several other parameters. The following parameters were compared between the two cohorts: age, gender, socioeconomic status, initial prescriber, comorbidity (described in more detail below), number of short courses of oral corticosteroids, use of short-acting bronchodilators, initial medication and dosing regimen. We performed a multivariate analysis to correct for parameters that significantly differed (P<0.05) between the two cohorts.
Comorbidity
Included comorbidities were selected based on frequently reported comorbidities from previous studies.21 If available, proxies from earlier studies were used to identify comorbidities based on medication use.22–24 Diabetes was identified by use of glucose-lowering drugs, that is, drugs with anatomical therapeutic chemical code ‘A10%’. Dyslipidaemia was identified by use of lipid-lowering drugs (C10). Heart failure and ischaemic heart disease were identified by prescription of digoxin or loop diuretics (C01AA05 or C03C) and C01DA, respectively. Patients not using previously mentioned anatomical therapeutic chemical codes but using other cardiovascular drugs (C02, C03, C07, C08 or C09) were classified as patients suffering from other cardiovascular disorders. Other diseases included osteoporosis (M05B), anxiety (N05B and N05C), dementia (N06B), depression (N06A), rheumatic arthritis (M01 and M02) and hypothyroid disease (H03). Patients needed to have at least two of these prescriptions within 1 year after COPD treatment initiation to be considered a chronic user of these comedications.
Statistics
Parameters of the two cohorts were compared using Fisher’s exact tests or Mann–Whitney U-tests, where appropriate.
Kaplan–Meier survival analyses were used to visualise patients’ persistence over a 1-year-time period, comparing patients initiating multiple-dose inhalers and single-dose inhalers. In multivariate Cox proportional hazard analyses, results were adjusted for parameters that differed between the two cohorts with a 95% confidence level (P<0.05). Statistics were performed with IBM SPSS Statistics 22 (IBM Corp., Armonk, NY, USA).
Handling of missing data
Patients without gender or date of birth information were excluded from the cohort, just as patients who died in the year after treatment initiation. In case of missing data on essential parameters such as dosing regimen or amount of inhalers dispensed, patients were also excluded.
Sensitivity analyses
In order to assess the sensitivity of the gap that was chosen to define persistence, we also performed an analysis with a 30- and a 90-day gap. These analyses will ease generalisability of results by allowing comparison with previous studies using different definitions of persistence. Sensitivity analyses were performed for patients with at least two prescriptions for long-acting bronchodilators (including LABA-ICS or long-acting muscarinic antagonist) in the year after treatment initiation, that is, one-time users (for example, in case of an incident exacerbation) were excluded.
Results
Population selection process
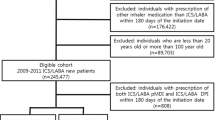
In all, 1,838 potential COPD patients initiated a LABA of interest (formoterol, indacaterol or salmeterol) between 1996 and 2011. After exclusion of likely asthma patients (223), 1,615 patients remained. Of these, 595 patients had no complete information records on essential parameters to calculate persistence (for example, dosing regimen or amount of inhalers) and were excluded, leaving 1,020 patients. Among them, 207 started two long-acting inhalers on the same date and were excluded, leaving 813 patients. Of those, 238 (29%) started with a pressurised metered dose inhaler and 575 (71%) started with a DPI. Of all the DPI users, 475 (83%) initiated a multiple-dose inhaler and 100 (17%) a single-dose inhaler.
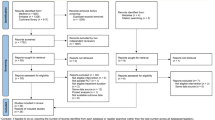
A flow diagram is provided in Figure 1. Patient characteristics, per cohort, are presented in Table 1. Parameters that significantly differed (P<0.05) were the initial prescriber, comorbidities (lipid-metabolism disorders and psychosis, in particular), the initial medication and the dosing regimen.
Flow diagram of the population selection process. Asthma patients, excluded based on use of antihistamines, anti-allergics, leukotriene receptor antagonists or omaluzimab; COPD, chronic obstructive pulmonary disease; double medication, initiating of two types of inhaled medication at the same date; DPI, dry powder inhaler; LABA, long-acting β2-agonist; pMDI, pressurised metered dose inhaler.
Analysis of persistence
Overall, 1-year persistence in the basecase scenario (60-day gap, minimal one prescription) was 14.4%. Persistence between users of multiple-dose and single-dose inhalers did not significantly differ (hazard ratio: 0.96, 95% confidence interval: 0.76–1.22, P=0.74). In the multivariate analysis, results did not change (hazard ratio: 0.98, 95% confidence interval: 0.76–1.26, P=0.99).
Sensitivity analyses
Impact of the gap
In sensitivity analyses, overall 1-year persistence changed when increasing or decreasing the gap allowed for being considered persistent. Decreasing to a 30-day gap reduced overall persistence to 9.6%, whereas increasing to a 90-day gap improved overall treatment persistence to 19%.
Excluding one-time users
Including only patients with two prescriptions or more resulted in a cohort of 375 patients initiating LABAs. Sixty-six (18%) patients initiated a single-dose inhaler and three hundred nine (82%) a multiple-dose inhaler. Overall persistence was 21.9%. There was no significant difference between persistence of users of single-dose or multiple-dose inhalers (25% vs. 21%, P=0.24). Persistence with initial medication over time is graphically shown in Figure 2. Note that in this figure patients were marked non-persistent when they did not redeem their next prescription of their initial inhaler within 60 days after the theoretical end date of their previous prescription (when used as prescribed). Take into account that the dosing regimen varied between one and four times per day. The time point of non-persistence is the theoretical end date of their last prescription before their first gap.
Allowing switching
In Figure 3, persistence with any long-acting medication over time is shown for a cohort that included only patients with two or more prescriptions and allowing switching, resulting in an overall persistence of 38.4%.
Switching patterns
Figure 4 shows the switching patterns of non-persistent patients after their first 60-days gap. Note that the switching analysis was performed in a subcohort (N=307) with at least two dispensings for long-acting bronchodilators (that is, one-time users are not included) and a follow-up of at least 2 years from treatment initiation. In this cohort, 38 out of 53 single-dose inhaler users were non-persistent and 203 out of 254 multiple-dose inhaler users. From Figure 4 it is shown that ~40% of all patients (disregarding their inhaler type) re-started their initial therapy within 1 year after their first gap. Less than 19% of the patients with a gap did permanently discontinue any type of long-acting respiratory therapy. A considerable percentage of patients switched to fixed dose inhalers of LABA and ICS. Of the single-dose inhaler users, 11% switched to multiple-dose inhalers of the same medication, whereas none of the multiple-dose inhaler users switched to single-dose inhalers with the same medication.
Switching patterns after the first 60-day gap in patients with at least two dispenses and 2 years follow-up: single-dose versus multiple-dose inhalers. LABA, long-acting β2-agonist; ICS, inhaled corticosteriod; LAMA, long-acting muscarinic antagonist; DPI, dry-powder inhaler; pMDI, pressurised metered-dose inhaler.
Discussion
Main findings
This study showed no significant impact of inhaler device on COPD patients’ persistence with LABAs: persistence of patients initiating multiple-dose inhalers was comparable to patients initiating single-dose inhalers. Whereas overall persistence with LABAs seemed relatively low at first sight, this study showed that ~40% of all patients (disregarding their inhaler type) re-started their initial therapy within 1 year. Only 15% of the patients who seemed to discontinue based on a 60-day treatment gap did indeed permanently discontinue any type of long-acting respiratory therapy. A considerable percentage of patients (about one-third) switched to fixed dose inhalers of LABA and ICS. Of the single-dose inhaler users, 11% switched to multiple-dose inhalers of the same medication, whereas none of the multiple-dose inhaler users switched to single-dose inhalers with the same medication.
Interpretation of findings in relation to previously published work
This study is the first describing the relationship between inhaler devices and persistence with COPD maintenance medication. In asthma, DPI devices have been linked to improved adherence compared with pressurised metered dose inhalers.25 Specific studies in COPD patients assessing the impact of inhaler device on adherence or persistence are lacking.14 In general, medication persistence in our study was far short of optimal, for both multiple-dose as well as single-dose inhalers. This relatively low persistence is in line with findings from previous studies;6,7 however, this study showed that over 80% of patients who initially seemed to discontinue LABAs, based on a 60-day treatment gap, re-started their initial medication or switched to different types of inhaler or medication within 1 year after discontinuation. The high percentage of switching may suggest that for some prescribers it takes some time to find the optimal inhaler and medication to suit their patients’ preferences regarding persistent use. However, whereas an optimal inhaler may favour patients’ persistence, improved disease control and better clinical outcomes are not guaranteed. Even though in controlled clinical trial settings comparing inhaler devices no differences in outcomes were observed,26 in daily practice, many problems with inhalers have been described.19,20,27 Main problems are related to poor inhalation technique,28 resulting in suboptimal deposition in the lungs, oropharyngeal side effects29 and ultimately poor disease control.30 Instruction on inhalation techniques has been shown to not only improve adherence but was also associated with better health-related quality of life.31 Apart from inhalation technique and lung deposition issues, one can argue whether improved health outcomes are solely achieved by adherence to respiratory medication or that COPD patients’ (self-management) skills and behaviour determine an important part of improved outcomes. Notably, good adherers with COPD placebo inhalers showed comparable outcomes on mortality and hospitalisation rates as good adherers to real medications.32 Vestbo et al.32 describe this phenomenon as the ‘healthy adherer effect’. It is suggested that COPD patients who are good adherers to their medication have a healthier lifestyle in general (similar to more awareness of the importance of smoking cessation, a healthy diet and intensity of exercise). In other words, medication non-adherence may be an indicator of patients’ shortage of disease- and self-management skills. This reveals an important opportunity for the health-care provider: actively search for non-adherent COPD patients (for example, by medication dispense records) and target your interventions to these patients. Using this strategy, not only health-care providers’ time is more efficiently spent but also the cost effectiveness of disease management interventions is expected to increase as non-adherence has a marked effect on worsened economic outcomes.8
Strengths and limitations
By using real-world and up-to-date data, the results of this study are expected to be representative for the current situation in the community. However, whereas relative results are expected to be generalisable between countries, absolute results may be less generalisable because of intensive monitoring and lung revalidation programmes currently running in the Netherlands, which may encourage more adherent behaviour. Some late onset asthma patients may be incorrectly classified as COPD patients as the database does not provide a diagnosis. In addition, some severe exacerbations (requiring hospital admission) may have been missed as the database only collects data from community pharmacies. Although we tried to use the dispensing of short courses of oral corticosteroids as a proxy for disease severity, findings could still be confounded by COPD severity, as neither lung function data nor a full set of proxies for COPD severity were available. The last two limitations are related to the size of the sample. It might be possible that the observed non-difference in persistence between the two inhaler types resulted from an insufficient power to detect the persistence difference. Another possibility is that the persistence difference might only exist, for example, in those COPD patients using their inhaler four times per day, and only a small proportion of the studied subjects used the inhaler at this high frequency.
Implications for future research, policy and practice
In order to optimise patients’ persistence with COPD medication, we recommend a choice of inhaler depending on patients’ individual abilities to handle the inhaler.33 Besides, factors relating to optimal prescription, taking into account patients’ preferences34 and interventions on behaviour modification (for example, stimulation of self-management and inhalation techniques), are equally important and may add to patients’ capacity of acting in a more adherent behaviour.35 In addition, enhancing health-care providers’ education and communication skills may be beneficial.36 Targeting these interventions on non-adherent patients is expected to improve cost effectiveness.8,37
Conclusions
The choice of an appropriate inhaler device is an important issue regarding COPD patients’ persistence; however, regarding the inhaler being a multi-dose or a single-dose device does not seem to affect patients’ persistence with LABAs. Over 80% of patients, who initially seemed to discontinue LABAs, re-started their initial medication or switched to a different type of inhaler or medication within 1 year.
References
Sullivan SD, Ramsey SD, Lee TA. The economic burden of COPD. Chest 2000; 117 (Suppl): 5S–9S.
van Boven JF, Vegter S, van der Molen T, Postma MJ. COPD in the working age population: the economic impact on both patients and government. COPD 2013; 10: 629–639.
Calverley P, Pauwels R, Vestbo J, Jones P, Pride N, Gulsvik A et al. Combined salmeterol and fluticasone in the treatment of chronic obstructive pulmonary disease: a randomised controlled trial. Lancet 2003; 361: 449–456.
Calverley PM, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med 2007; 356: 775–789.
Herland K, Akselsen JP, Skjonsberg OH, Bjermer L. How representative are clinical study patients with asthma or COPD for a larger "real life" population of patients with obstructive lung disease? Respir Med 2005; 99: 11–19.
Cramer JA, Bradley-Kennedy C, Scalera A. Treatment persistence and compliance with medications for chronic obstructive pulmonary disease. Can Respir J 2007; 14: 25–29.
Penning-van Beest F, van Herk-Sukel M, Gale R, Lammers JW, Herings R. Three-year dispensing patterns with long-acting inhaled drugs in COPD: a database analysis. Respir Med 2011; 105: 259–265.
van Boven JF, Chavannes NH, van der Molen T, Rutten-van Molken MP, Postma MJ, Vegter S. Clinical and economic impact of non-adherence in COPD: a systematic review. Respir Med 2014; 108: 103–113.
George J, Kong DC, Thoman R, Stewart K. Factors associated with medication nonadherence in patients with COPD. Chest 2005; 128: 3198–3204.
Khdour MR, Hawwa AF, Kidney JC, Smyth BM, McElnay JC . Potential risk factors for medication non-adherence in patients with chronic obstructive pulmonary disease (COPD). Eur J Clin Pharmacol 2012; 68: 1365–1373.
Blais L, Bourbeau J, Sheehy O, LeLorier J. Inhaled corticosteroids in COPD: Determinants of use and trends in patient persistence with treatment. Can Respir J 2004; 11: 27–32.
Breekveldt-Postma NS, Gerrits CM, Lammers JW, Raaijmakers JA, Herings RM. Persistence with inhaled corticosteroid therapy in daily practice. Respir Med 2004; 98: 752–759.
Rand CS, Nides M, Cowles MK, Wise RA, Connett J. Long-term metered-dose inhaler adherence in a clinical trial. the lung health study research group. Am J Respir Crit Care Med 1995; 152: 580–588.
Makela MJ, Backer V, Hedegaard M, Larsson K. Adherence to inhaled therapies, health outcomes and costs in patients with asthma and COPD. Respir Med 2013; 107: 1481–1490.
World Health Organization. Adherence to long-term therapies - evidence for action. available from Http://Apps.who.int/medicinedocs/pdf/s4883e/s4883e.pdf 2003.
Visser ST, Schuiling-Veninga CC, Bos JH, de Jong-van den Berg LT, Postma MJ . The population-based prescription database IADB.nl: Its development, usefulness in outcomes research and challenges. Expert Rev Pharmacoecon Outcomes Res 2013; 13: 285–292.
Vegter S, Nguyen NH, Visser ST, de Jong-van den Berg LT, Postma MJ, Boersma C . Compliance, persistence, and switching patterns for ACE inhibitors and ARBs. Am J Manag Care 2011; 17: 609–616.
van Boven JF, de Boer PT, Postma MJ, Vegter S . Persistence with osteoporosis medication among newly-treated osteoporotic patients. J Bone Miner Metab 2013; 31: 562–570.
Barrons R, Pegram A, Borries A. Inhaler device selection: Special considerations in elderly patients with chronic obstructive pulmonary disease. Am J Health Syst Pharm 2011; 68: 1221–1232.
Virchow JC, Crompton GK, Dal Negro R, Pedersen S, Magnan A, Seidenberg J et al. Importance of inhaler devices in the management of airway disease. Respir Med 2008; 102: 10–19.
Garcia-Olmos L, Alberquilla A, Ayala V, García-Sagredo P, Morales L, Carmona M et al. Comorbidity in patients with chronic obstructive pulmonary disease in family practice: a cross sectional study. BMC Fam Pract 2013; 14: 11.
Gray J, Majeed A, Kerry S, Rowlands G. Identifying patients with ischaemic heart disease in general practice: cross sectional study of paper and computerised medical records. BMJ 2000; 321: 548–550.
Tu K, Manuel D, Lam K, Kavanagh D, Mitiku TF, Guo H. Diabetics can be identified in an electronic medical record using laboratory tests and prescriptions. J Clin Epidemiol 2011; 64: 431–435.
Udris EM, Au DH, McDonell MB, Chen L, Martin DC, Tierney WM et al. Comparing methods to identify general internal medicine clinic patients with chronic heart failure. Am Heart J 2001; 142: 1003–1009.
Roy A, Battle K, Lurslurchachai L, Halm EA, Wisnivesky JP. Inhaler device, administration technique, and adherence to inhaled corticosteroids in patients with asthma. Prim Care Respir J 2011; 20: 148–154.
Dolovich MB, Ahrens RC, Hess DR, Anderson P, Dhand R, Rau JL et al. Device selection and outcomes of aerosol therapy: evidence-based guidelines: American college of chest physicians/american college of asthma, allergy, and immunology. Chest 2005; 127: 335–371.
Rau JL. Determinants of patient adherence to an aerosol regimen. Respir Care 2005; 50: 1346–1356.
Broeders ME, Sanchis J, Levy ML, Crompton GK, Dekhuijzen PN, ADMIT Working Group. The ADMIT series--issues in inhalation therapy. 2. improving technique and clinical effectiveness. Prim Care Respir J 2009; 18: 76–82.
van Boven JF, de Jong-van den Berg LT, Vegter S . Inhaled corticosteroids and the occurrence of oral candidiasis: a prescription sequence symmetry analysis. Drug Saf 2013; 36: 231–236.
Lindgren S, Bake B, Larsson S. Clinical consequences of inadequate inhalation technique in asthma therapy. Eur J Respir Dis 1987; 70: 93–98.
Takemura M, Mitsui K, Itotani R, Ishitoko M, Suzuki S, Matsumoto M et al. Relationships between repeated instruction on inhalation therapy, medication adherence, and health status in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 2011; 6: 97–104.
Vestbo J, Anderson JA, Calverley PM, Celli B, Ferguson GT, Jenkins C et al. Adherence to inhaled therapy, mortality and hospital admission in COPD. Thorax 2009; 64: 939–943.
Vincken W, Dekhuijzen PR, Barnes P, ADMIT Group. The ADMIT series - issues in inhalation therapy. 4) how to choose inhaler devices for the treatment of COPD. Prim Care Respir J 2010; 19: 10–20.
Price D, Lee AJ, Sims EJ, Kemp L, Hillyer EV, Chisholm A et al. Characteristics of patients preferring once-daily controller therapy for asthma and COPD: a retrospective cohort study. Prim Care Respir J 2013; 22: 161–168.
Broeders ME, Vincken W, Corbetta L, ADMIT Working Group. The ADMIT series-issues in inhalation therapy. 7. ways to improve pharmacological management of COPD: the importance of inhaler choice and inhalation technique. Prim Care Respir J 2011; 20: 338–343.
Lareau SC, Yawn BP. Improving adherence with inhaler therapy in COPD. Int J Chron Obstruct Pulmon Dis 2010; 5: 401–406.
Van Boven JF, Tommelein E, Boussery K, Mehuys E, Vegter S, Brusselle GG et al. Improving inhaler adherence in patients with Chronic Obstructive Pulmonary Disease: a cost-effectiveness analysis. Respir Res 2014; 15: 66.
Acknowledgements
We thank Bert Bijker for database assistance.
Author information
Authors and Affiliations
Contributions
JFMvB and TvM designed the study. JJvR and RvG prepared the database. JFMvB and SV performed the analyses. All the authors were involved in study methodology and interpretation of results. JFMvB wrote the first draft. All the authors commented on the manuscript and contributed to the final version. JFMvB is the guarantor of the study.
Corresponding author
Ethics declarations
Competing interests
TvdM has received research grants from AstraZeneca, GlaxoSmithKline, Nycomed, MSD, Almirall, consultancy fees for advisory boards from AstraZeneca, Nycomed, MSD, Novartis, Almirall and speaker fees from AstraZeneca, GlaxoSmithKline, Nycomed, Novartis and MSD. PNRD has received reimbursements for attending symposia, fees for speaking, organising educational events, funds for research or fees for consulting from AstraZeneca, Boehringer-Ingelheim, Chiesi, MSD, Mundipharma, Novartis, Takeda, Almirall and Teva. MJP has received grants, honoraria and travel stipends from various pharmaceutical companies including GlaxoSmithKline. The remaining authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
van Boven, J., van Raaij, J., van der Galiën, R. et al. Impact of multiple-dose versus single-dose inhaler devices on COPD patients’ persistence with long-acting β2-agonists: a dispensing database analysis. npj Prim Care Resp Med 24, 14069 (2014). https://doi.org/10.1038/npjpcrm.2014.69
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/npjpcrm.2014.69
This article is cited by
-
Patient’s awareness on COPD is the strongest predictor of persistence and adherence in treatment-naïve patients in real life: a prospective cohort study
BMC Pulmonary Medicine (2021)
-
Primary non-adherence to inhaled medications measured with e-prescription data from Poland
Clinical and Translational Allergy (2020)