Abstract
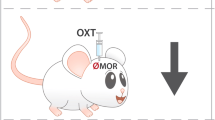
Prolactin-releasing peptide (PrRP) and its receptor G protein–coupled receptor 10 (GPR10) are expressed in brain areas involved in the processing of nociceptive signals. We investigated the role of this new neuropeptidergic system in GPR10-knockout mice. These mice had higher nociceptive thresholds and stronger stress-induced analgesia than wild-type mice, differences that were suppressed by naloxone treatment. In addition, potentiation of morphine-induced antinociception and reduction of morphine tolerance were observed in mutants. Intracerebroventricular administration of PrRP in wild-type mice promoted hyperalgesia and reversed morphine-induced antinociception. PrRP administration had no effect on GPR10-mutant mice, showing that its effects are mediated by GPR10. Anti-opioid effects of neuropeptide FF were found to require a functional PrRP-GPR10 system. Finally, GPR10 deficiency enhanced the acquisition of morphine-induced conditioned place preference and decreased the severity of naloxone-precipitated morphine withdrawal syndrome. Altogether, our data identify the PrRP-GPR10 system as a new and potent negative modulator of the opioid system.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Inturrisi, C.E. Clinical pharmacology of opioids for pain. Clin. J. Pain 18, S3–13 (2002).
Noble, F. & Roques, B.P. CCK-B receptor: chemistry, molecular biology, biochemistry and pharmacology. Prog. Neurobiol. 58, 349–379 (1999).
Panula, P. et al. Neuropeptide FF and modulation of pain. Brain Res. 848, 191–196 (1999).
Calo, G., Guerrini, R., Rizzi, A., Salvadori, S. & Regoli, D. Pharmacology of nociceptin and its receptor: a novel therapeutic target. Br. J. Pharmacol. 129, 1261–1283 (2000).
Meunier, J.C. Utilizing functional genomics to identify new pain treatments: the example of nociceptin. Am. J. Pharmacogenomics 3, 117–130 (2003).
Mollereau, C., Roumy, M. & Zajac, J.M. Opioid-modulating peptides: mechanisms of action. Curr. Top. Med. Chem. 5, 341–355 (2005).
Allard, M., Labrouche, S., Nosjean, A. & Laguzzi, R. Mechanisms underlying the cardiovascular responses to peripheral administration of NPFF in the rat. J. Pharmacol. Exp. Ther. 274, 577–583 (1995).
Sundblom, D.M., Heikman, P., Naukkarinen, H. & Fyhrquist, F. Blood concentrations of vasopressin, neuropeptide FF and prolactin are increased by high-dose right unilateral ECT. Peptides 20, 319–326 (1999).
Roumy, M. & Zajac, J.M. Neuropeptide FF, pain and analgesia. Eur. J. Pharmacol. 345, 1–11 (1998).
Hinuma, S. et al. A prolactin-releasing peptide in the brain. Nature 393, 272–276 (1998).
Lawrence, C.B., Celsi, F., Brennand, J. & Luckman, S.M. Alternative role for prolactin-releasing peptide in the regulation of food intake. Nat. Neurosci. 3, 645–646 (2000).
Samson, W.K., Resch, Z.T. & Murphy, T.C. A novel action of the newly described prolactin-releasing peptides: cardiovascular regulation. Brain Res. 858, 19–25 (2000).
Maruyama, M. et al. Prolactin-releasing peptide as a novel stress mediator in the central nervous system. Endocrinology 142, 2032–2038 (2001).
Maruyama, M. et al. Central administration of prolactin-releasing peptide stimulates oxytocin release in rats. Neurosci. Lett. 276, 193–196 (1999).
Roland, B.L. et al. Anatomical distribution of prolactin-releasing peptide and its receptor suggests additional functions in the central nervous system and periphery. Endocrinology 140, 5736–5745 (1999).
Passik, S.D. & Weinreb, H.J. Managing chronic nonmalignant pain: overcoming obstacles to the use of opioids. Adv. Ther. 17, 70–83 (2000).
Lin, S.H., Leslie, F.M. & Civelli, O. Neurochemical properties of the prolactin releasing peptide (PrRP) receptor expressing neurons: evidence for a role of PrRP as a regulator of stress and nociception. Brain Res. 952, 15–30 (2002).
Kalliomaki, M.L. et al. Prolactin-releasing peptide affects pain, allodynia and autonomic reflexes through medullary mechanisms. Neuropharmacology 46, 412–424 (2004).
Mogil, J.S., Sternberg, W.F., Balian, H., Liebeskind, J.C. & Sadowski, B. Opioid and nonopioid swim stress-induced analgesia: a parametric analysis in mice. Physiol. Behav. 59, 123–132 (1996).
Semenova, S., Kuzmin, A. & Zvartau, E. Strain differences in the analgesic and reinforcing action of morphine in mice. Pharmacol. Biochem. Behav. 50, 17–21 (1995).
Lin, S.H., Leslie, F.M. & Civelli, O. Neurochemical properties of the prolactin releasing peptide (PrRP) receptor expressing neurons: evidence for a role of PrRP as a regulator of stress and nociception. Brain Res. 952, 15–30 (2002).
Pacak, K. et al. In vivo hypothalamic release and synthesis of catecholamines in spontaneously hypertensive rats. Hypertension 22, 467–478 (1993).
Lawrence, C.B., Ellacott, K.L. & Luckman, S.M. PRL-releasing peptide reduces food intake and may mediate satiety signaling. Endocrinology 143, 360–367 (2002).
Ueda, H., Inoue, M. & Mizuno, K. New approaches to study the development of morphine tolerance and dependence. Life Sci. 74, 313–320 (2003).
Solomon, R.L. & Corbit, J.D. An opponent-process theory of motivation. I. Temporal dynamics of affect. Psychol. Rev. 81, 119–145 (1974).
Malin, D.H. et al. FMRF-NH2-like mammalian peptide precipitates opiate-withdrawal syndrome in the rat. Peptides 11, 277–280 (1990).
Panula, P. et al. Neuropeptide FF and modulation of pain. Brain Res. 848, 191–196 (1999).
Murphy, N.P., Lee, Y. & Maidment, N.T. Orphanin FQ/nociceptin blocks acquisition of morphine place preference. Brain Res. 832, 168–170 (1999).
King, M.A., Rossi, G.C., Chang, A.H., Williams, L. & Pasternak, G.W. Spinal analgesic activity of orphanin FQ/nociceptin and its fragments. Neurosci. Lett. 223, 113–116 (1997).
Ueda, H., Inoue, M., Takeshima, H. & Iwasawa, Y. Enhanced spinal nociceptin receptor expression develops morphine tolerance and dependence. J. Neurosci. 20, 7640–7647 (2000).
Ueda, H. et al. Partial loss of tolerance liability to morphine analgesia in mice lacking the nociceptin receptor gene. Neurosci. Lett. 237, 136–138 (1997).
Noble, F., Derrien, M. & Roques, B.P. Modulation of opioid antinociception by CCK at the supraspinal level: evidence of regulatory mechanisms between CCK and enkephalin systems in the control of pain. Br. J. Pharmacol. 109, 1064–1070 (1993).
Noble, F. & Roques, B.P. The role of CCK2 receptors in the homeostasis of the opioid system. Drugs Today (Barc.) 39, 897–908 (2003).
Pommier, B. et al. Deletion of CCK2 receptor in mice results in an upregulation of the endogenous opioid system. J. Neurosci. 22, 2005–2011 (2002).
Langmead, C.J. et al. Characterization of the binding of [(125)I]-human prolactin releasing peptide (PrRP) to GPR10, a novel G protein coupled receptor. Br. J. Pharmacol. 131, 683–688 (2000).
Laorden, M.L., Castells, M.T. & Milanes, M.V. Effects of morphine and morphine withdrawal on brainstem neurons innervating hypothalamic nuclei that control the pituitary-adrenocortical axis in rats. Br. J. Pharmacol. 136, 67–75 (2002).
Dayas, C.V., Buller, K.M., Crane, J.W., Xu, Y. & Day, T.A. Stressor categorization: acute physical and psychological stressors elicit distinctive recruitment patterns in the amygdala and in medullary noradrenergic cell groups. Eur. J. Neurosci. 14, 1143–1152 (2001).
Delfs, J.M., Zhu, Y., Druhan, J.P. & Aston-Jones, G. Noradrenaline in the ventral forebrain is critical for opiate withdrawal-induced aversion. Nature 403, 430–434 (2000).
Martin, M., Ledent, C., Parmentier, M., Maldonado, R. & Valverde, O. Involvement of CB1 cannabinoid receptors in emotional behaviour. Psychopharmacology (Berl.) 159, 379–387 (2002).
Simonin, F., Valverde, O., Smadja, C., Slowe, S., Kitchen, I., Dierich, A., Le Meur, M., Roques, B.P., Maldonado, R. & Kieffer, B.L. Disruption of the kappa-opioid receptor gene in mice enhances sensitivity to chemical visceral pain, impairs pharmacological actions of the selective kappa-agonist U-50,488H and attenuates morphine withdrawal. EMBO J. 17, 886–897 (1998).
Acknowledgements
We thank C. Contet, L. Cuvelier and D. Houtteman for technical assistance and F. Simonin for helpful discussion. M.P. and S.N.S. were supported by the Fondation Médicale Reine Elisabeth and the Fonds de la Recherche Scientifique Médicale. M.P. was also supported by the Belgian 'Interuniversity Attraction Poles' program, initiated by the Belgian State, Prime Minister's Office, Science Policy Programming and the LifeSciHealth (grant LSHB-CT-2003-503337) programs of the European Community. O.V. and R.M. were supported by the Spanish Ministry of Science and Technology (SAF 2001-0745 to O.V. and GEN2003-20651-C06-04 to R.M). P.L. was supported by fellowships from the Fonds pour la Recherche dans l'Industrie et l'Agriculture and Télévie. C.L and A. de K. are Chercheurs Qualifiés of the Fonds National de la Recherche Scientifique. Scientific responsibility is assumed by the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Fig. 1
Corticosterone supplementation. (PDF 221 kb)
Supplementary Fig. 2
Lower incidence of somatic signs of withdrawal in KO mice. (PDF 240 kb)
Supplementary Fig. 3
Morphine-induced regulation of NPFF and PrRP transcript levels. (PDF 320 kb)
Supplementary Table 1
[35S]GTPγS binding assay of the μ-opioid receptor. (PDF 26 kb)
Rights and permissions
About this article
Cite this article
Laurent, P., Becker, J., Valverde, O. et al. The prolactin-releasing peptide antagonizes the opioid system through its receptor GPR10. Nat Neurosci 8, 1735–1741 (2005). https://doi.org/10.1038/nn1585
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nn1585
This article is cited by
-
Behavioral sensitization induced by methamphetamine causes differential alterations in gene expression and histone acetylation of the prefrontal cortex in rats
BMC Neuroscience (2021)
-
The hindbrain is a site of energy balance action for prolactin-releasing peptide: feeding and thermic effects from GPR10 stimulation of the nucleus tractus solitarius/area postrema
Psychopharmacology (2018)
-
Candidate gene polymorphisms predicting individual sensitivity to opioids
Naunyn-Schmiedeberg's Archives of Pharmacology (2008)