Abstract
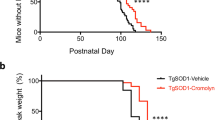
Mitochondria are particularly vulnerable to oxidative stress, and mitochondrial swelling and vacuolization are among the earliest pathologic features found in two strains of transgenic amyotrophic lateral sclerosis (ALS) mice with SOD1 mutations1,2. Mice with the G93A human SOD1 mutation have altered electron transport enzymes, and expression of the mutant enzyme in vitro results in a loss of mitochondrial membrane potential and elevated cytosolic calcium concentration3. Mitochondrial dysfunction may lead to ATP depletion, which may contribute to cell death. If this is true, then buffering intracellular energy levels could exert neuroprotective effects. Creatine kinase and its substrates creatine and phosphocreatine constitute an intricate cellular energy buffering and transport system connecting sites of energy production (mitochondria) with sites of energy consumption4, and creatine administration stabilizes the mitochondrial creatine kinase and inhibits opening of the mitochondrial transition pore5. We found that oral administration of creatine produced a dose-dependent improvement in motor performance and extended survival in G93A transgenic mice, and it protected mice from loss of both motor neurons and substantia nigra neurons at 120 days of age. Creatine administration protected G93A transgenic mice from increases in biochemical indices of oxidative damage. Therefore, creatine administration may be a new therapeutic strategy for ALS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others

References
Wong, P.C. et al. An adverse property of a familial ALS-linked SOD1 mutation causes motor neuron disease characterized by vacuolar degeneration of mitochondria. Neuron 14, 1105–1116 (1995).
Gurney, M.E. et al. Motor neuron degeneration in mice that express a human Cu,Zn superoxide dismutase mutation. Science 264, 1772–1775 (1994).
Carri, M.T. et al. Expression of a Cu,Zn superoxide dismutase typical of familial amyotrophic lateral sclerosis induces mitochondrial alteration and increase of cytosolic Ca2+ concentration in transfected neuroblastoma SH-SY5Y cells. FEBS Lett. 414, 365–368 (1997).
Hemmer, W. & Wallimann, T. Functional aspects of creatine kinase in brain. Dev. Neurosci. 15, 249–260 (1993).
O'Gorman, E., Beutner, G., Wallimann, T. & Brdiczka, D. Differential effects of creatine depletion on the regulation of enzyme activities and on creatine-stimulated mitochondrial respiration in skeletal muscle, heart, and brain. Biochim. Biophys. Acta 1276, 161–170 (1996).
Gurney, M.E. et al. Antioxidants and inhibitors of glutamatergic transmission have therapeutic benefit in a transgenic model of familial amyotrophic lateral sclerosis. Ann. Neurol. 39, 147–157 (1996).
Dugan, L.L. et al. Carboxyfullerenes as neuroprotective agents. Proc. Natl. Acad. Sci. USA 94, 9434–9439 (1997).
Hottinger, A.F., Fine, E.G., Gurney, M.E., Zurn, A.D. & Aebischer, P. The copper chelator d-penicillamine delays onset of disease and extends survival in a transgenic moouse model of familial amyotrophic lateral sclerosis. Eur. J. Neurosci. 9, 1548–1551 (1997).
Kostic, V. et al. Midbrain dopaminergic neuronal degeneration in a transgenic mouse model of familial amyotrophic lateral sclerosis. Ann. Neurol. 41, 497–504 (1997).
Ferrante, R.J. et al. Increased 3-nitrotyrosine and oxidative damage in mice with a human Cu, Zn superoxide dismutase mutation. Ann. Neurol. 42, 326–334 (1997).
Bogdanov, M.B., Ramos, L.E., Xu, X. & Beal, M.F. Elevated "hydroxyl radical" generation in vivo in an animal model of amyotrophic lateral sclerosis. J. Neurochem. 71, 1321–1324 (1998).
Sasaki, S., Maruyama, S., Yamane, K., Sakuma, H. & Takeishi, M. Ultrastructure of swollen proximal axons of anterior horn neurons in motor neuron disease. J. Neurol. Sci. 97, 233–240 (1990).
Siklos, L. et al. Ultrastructural evidence for altered calcium in motor nerve terminals in amyotrophic lateral sclerosis. Ann. Neurol. 39, 203–219 (1996).
White, R.J. & Reynolds, I.J. Mitochondrial depolarization in glutamate-stimulated neurons: an early signal specific to excitotoxin exposure. J. Neurosci. 16, 5688–5697 (1996).
O'Gorman, E. et al. The role of creatine kinase inhibition of mitochondrial permeability transition. FEBS Lett. 414, 253–257 (1997).
Sauter, A. & Rudin, M. Determination of creatine kinase parameters in rat brain by NMR magnetization transfer: correlation with brain function. J. Biol. Chem. 268, 13166–13171 (1993).
Corbett, R.J.T. & Laptook, A.R. Age-related changes in swine brain creatine kinase-catalyzed 31P exchange measured in vivo using 31P NMR magnetization transfer. J. Cereb. Blood Flow Metab. 14, 1070–1077 (1994).
Xu, C.J. et al. Phosphocreatine-dependent glutamate uptake by synaptic vesicles. J. Biol. Chem. 271, 13435–13440 (1996).
Rothstein, J.D., M., V.K., Levey, A.I., Martin, L. & Kuncl, R.W. Selective loss of glial glutamate transporter GLT-1 in amyotrophic lateral sclerosis. Ann. Neurol. 38, 73–84 (1995).
Sipila, I., Rapola, J., Simell, O. & Vannas, A. Supplementary creatine as a treatment for gyrate atrophy of the choroid and retina. N. Engl. J. Med. 304, 867–870 (1981).
Blanchard, V., Raisman-Vozari, R., Vyas, S., Michel, P.P., Javoy-Agid, F. & Uhl, G. Differential expression of tyrosine hydroxylase and membrane dopamine transporter genes in subpopulations of dopaminergic neurons of rat mesencephalon. Molec. Brain Res. 22, 29–40 (1994).
Matthews, R.T. et al. Neuroprotective effects of creatine and cyclocreatine in animal models of Huntington's disease. J. Neurosci. 18, 156–163 (1998).
Bogdanov, M.B., Ramos, L.E., Xu, X. & Beal, M.F. Elevated "hydroxyl radical" generation in vivo in an animal model of amyotrophic lateral sclerosis. J. Neurochem. 71, 1321–1324 (1998).
Acknowledgements
The secretarial assistance of S. Melanson is acknowledged. Photographic assistance was provided by S. Kuemmerle. This work was supported by NIH grant PO1 AG12292 (M.F.B. and R.J.F.), NS37102 (R.J.F.), the Veterans Administration (R.J.F.), the Muscular Dystrophy Association and the ALS Association, and NIMH grant MH11692 (A.M.K.).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Klivenyi, P., Ferrante, R., Matthews, R. et al. Neuroprotective effects of creatine in a transgenic animal model of amyotrophic lateral sclerosis. Nat Med 5, 347–350 (1999). https://doi.org/10.1038/6568
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/6568
This article is cited by
-
“Heads Up” for Creatine Supplementation and its Potential Applications for Brain Health and Function
Sports Medicine (2023)
-
FUS Mutation Causes Disordered Lipid Metabolism in Skeletal Muscle Associated with ALS
Molecular Neurobiology (2022)
-
Altered Bioenergetics and Metabolic Homeostasis in Amyotrophic Lateral Sclerosis
Neurotherapeutics (2022)
-
Energy metabolism in ALS: an underappreciated opportunity?
Acta Neuropathologica (2018)
-
AMPK Signalling and Defective Energy Metabolism in Amyotrophic Lateral Sclerosis
Neurochemical Research (2016)