Abstract
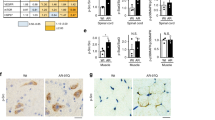
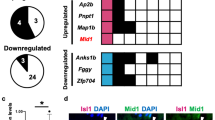
Spinal bulbar muscular atrophy (SBMA) is a motor neuron disease caused by toxic gain of function of the androgen receptor (AR). Previously, we found that co-regulator binding through the activation function-2 (AF2) domain of AR is essential for pathogenesis, suggesting that AF2 may be a potential drug target for selective modulation of toxic AR activity. We screened previously identified AF2 modulators for their ability to rescue toxicity in a Drosophila model of SBMA. We identified two compounds, tolfenamic acid (TA) and 1-[2-(4-methylphenoxy)ethyl]-2-[(2-phenoxyethyl)sulfanyl]-1H-benzimidazole (MEPB), as top candidates for rescuing lethality, locomotor function and neuromuscular junction defects in SBMA flies. Pharmacokinetic analyses in mice revealed a more favorable bioavailability and tissue retention of MEPB compared with TA in muscle, brain and spinal cord. In a preclinical trial in a new mouse model of SBMA, MEPB treatment yielded a dose-dependent rescue from loss of body weight, rotarod activity and grip strength. In addition, MEPB ameliorated neuronal loss, neurogenic atrophy and testicular atrophy, validating AF2 modulation as a potent androgen-sparing strategy for SBMA therapy.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Change history
08 January 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41591-023-02778-7
References
Kennedy, W.R., Alter, M. & Sung, J.H. Progressive proximal spinal and bulbar muscular atrophy of late onset. A sex-linked recessive trait. Neurology 18, 671–680 (1968).
Chahin, N., Klein, C., Mandrekar, J. & Sorenson, E. Natural history of spinal-bulbar muscular atrophy. Neurology 70, 1967–1971 (2008).
Poletti, A., Negri-Cesi, P. & Martini, L. Reflections on the diseases linked to mutations of the androgen receptor. Endocrine 28, 243–262 (2005).
Fratta, P. et al. Correlation of clinical and molecular features in spinal bulbar muscular atrophy. Neurology 82, 2077–2084 (2014).
La Spada, A.R., Wilson, E.M., Lubahn, D.B., Harding, A.E. & Fischbeck, K.H. Androgen receptor gene mutations in X-linked spinal and bulbar muscular atrophy. Nature 352, 77–79 (1991).
Sorarù, G. et al. Spinal and bulbar muscular atrophy: skeletal muscle pathology in male patients and heterozygous females. J. Neurol. Sci. 264, 100–105 (2008).
Finsterer, J. Perspectives of Kennedy's disease. J. Neurol. Sci. 298, 1–10 (2010).
Nedelsky, N.B. et al. Native functions of the androgen receptor are essential to pathogenesis in a Drosophila model of spinobulbar muscular atrophy. Neuron 67, 936–952 (2010).
Smith, C.L. & O'Malley, B.W. Coregulator function: a key to understanding tissue specificity of selective receptor modulators. Endocr. Rev. 25, 45–71 (2004).
Askew, E.B., Gampe, R.T. Jr., Stanley, T.B., Faggart, J.L. & Wilson, E.M. Modulation of androgen receptor activation function 2 2 by testosterone and dihydrotestosterone. J. Biol. Chem. 282, 25801–25816 (2007).
Chevalier-Larsen, E.S. et al. Castration restores function and neurofilament alterations of aged symptomatic males in a transgenic mouse model of spinal and bulbar muscular atrophy. J. Neurosci. 24, 4778–4786 (2004).
Katsuno, M. et al. Testosterone reduction prevents phenotypic expression in a transgenic mouse model of spinal and bulbar muscular atrophy. Neuron 35, 843–854 (2002).
Katsuno, M. et al. Leuprorelin rescues polyglutamine-dependent phenotypes in a transgenic mouse model of spinal and bulbar muscular atrophy. Nat. Med. 9, 768–773 (2003).
Katsuno, M. et al. Efficacy and safety of leuprorelin in patients with spinal and bulbar muscular atrophy (JASMITT study): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet Neurol. 9, 875–884 (2010).
Yang, Z. et al. ASC-J9 ameliorates spinal and bulbar muscular atrophy phenotype via degradation of androgen receptor. Nat. Med. 13, 348–353 (2007).
Banno, H. et al. Phase 2 trial of leuprorelin in patients with spinal and bulbar muscular atrophy. Ann. Neurol. 65, 140–150 (2009).
Axerio-Cilies, P. et al. Inhibitors of androgen receptor activation function-2 (AF2) site identified through virtual screening. J. Med. Chem. 54, 6197–6205 (2011).
Ban, F. et al. Discovery of 1H-indole-2-carboxamides as novel inhibitors of the androgen receptor binding function 3 3 (BF3). J. Med. Chem. 57, 6867–6872 (2014).
Estébanez-Perpiñá, E. et al. A surface on the androgen receptor that allosterically regulates coactivator binding. Proc. Natl. Acad. Sci. USA 104, 16074–16079 (2007).
Munuganti, R.S. et al. Targeting the binding function 3 3 (BF3) site of the androgen receptor through virtual screening. 2. development of 2-((2-phenoxyethyl) thio)-1H-benzimidazole derivatives. J. Med. Chem. 56, 1136–1148 (2013).
Lack, N.A. et al. Targeting the binding function 3 3 (BF3) site of the human androgen receptor through virtual screening. J. Med. Chem. 54, 8563–8573 (2011).
Munuganti, R.S. et al. Identification of a potent antiandrogen that targets the BF3 site of the androgen receptor and inhibits enzalutamide-resistant prostate cancer. Chem. Biol. 21, 1476–1485 (2014).
Rocchi, A. et al. Glycolytic-to-oxidative fiber-type switch and mTOR signaling activation are early-onset features of SBMA muscle modified by high-fat diet. Acta Neuropathol. 132, 127–144 (2016).
Cashman, N.R., Covault, J., Wollman, R.L. & Sanes, J.R. Neural cell adhesion molecule in normal, denervated, and myopathic human muscle. Ann. Neurol. 21, 481–489 (1987).
Gosztonyi, G., Naschold, U., Grozdanovic, Z., Stoltenburg-Didinger, G. & Gossrau, R. Expression of Leu-19 (CD56, N-CAM) and nitric oxide synthase (NOS) I in denervated and reinnervated human skeletal muscle. Microsc. Res. Tech. 55, 187–197 (2001).
Marbini, A. et al. Immunohistochemical study of muscle biopsy in children with cerebral palsy. Brain Dev. 24, 63–66 (2002).
Yu, Z. et al. Abnormalities of germ cell maturation and sertoli cell cytoskeleton in androgen receptor 113 CAG knock-in mice reveal toxic effects of the mutant protein. Am. J. Pathol. 168, 195–204 (2006).
Sun, J.H. & Lee, S.A. Association between CAG repeat polymorphisms and the risk of prostate cancer: a meta-analysis by race, study design and the number of (CAG)n repeat polymorphisms. Int. J. Mol. Med. 32, 1195–1203 (2013).
Albertelli, M.A. et al. Glutamine tract length of human androgen receptors affects hormone-dependent and -independent prostate cancer in mice. Hum. Mol. Genet. 17, 98–110 (2008).
Robins, D.M., Albertelli, M.A. & O'Mahony, O.A. Androgen receptor variants and prostate cancer in humanized AR mice. J. Steroid Biochem. Mol. Biol. 108, 230–236 (2008).
Buchanan, G. et al. Structural and functional consequences of glutamine tract variation in the androgen receptor. Hum. Mol. Genet. 13, 1677–1692 (2004).
Buchanan, G. et al. Corepressor effect on androgen receptor activity varies with the length of the CAG encoded polyglutamine repeat and is dependent on receptor/corepressor ratio in prostate cancer cells. Mol. Cell. Endocrinol. 342, 20–31 (2011).
Jehle, K. et al. Coregulator control of androgen receptor action by a novel nuclear receptor-binding motif. J. Biol. Chem. 289, 8839–8851 (2014).
Corell, T. Pharmacology of tolfenamic acid. Pharmacol. Toxicol. 75 (Suppl. 2), 14–21 (1994).
Hendel, J. The overall safety of tolfenamic acid. Pharmacol. Toxicol. 75 (Suppl. 2), 53–55 (1994).
Hendel, L., Larsen, E. & Bonnevie, O. A comparative study of the influence of tolfenamic acid (Clotam) and diclofenac sodium (Voltaren) on the gastrointestinal mucosa in patients with a history of NSAID-related dyspeptic symptoms. Pharmacol. Toxicol. 75 (Suppl. 2), 49–50 (1994).
Pedersen, S.B. Biopharmaceutical aspects of tolfenamic acid. Pharmacol. Toxicol. 75 (Suppl. 2), 22–32 (1994).
Yuan, H. et al. Suppression of the androgen receptor function by quercetin through protein-protein interactions of Sp1, c-Jun, and the androgen receptor in human prostate cancer cells. Mol. Cell. Biochem. 339, 253–262 (2010).
Hodgson, M.C., Shen, H.C., Hollenberg, A.N. & Balk, S.P. Structural basis for nuclear receptor corepressor recruitment by antagonist-liganded androgen receptor. Mol. Cancer Ther. 7, 3187–3194 (2008).
Bott, L.C. et al. A small-molecule Nrf1 and Nrf2 activator mitigates polyglutamine toxicity in spinal and bulbar muscular atrophy. Hum. Mol. Genet. 25, 1979–1989 (2016).
Glynn, M.W. & Glover, T.W. Incomplete processing of mutant lamin A in Hutchinson-Gilford progeria leads to nuclear abnormalities, which are reversed by farnesyltransferase inhibition. Hum. Mol. Genet. 14, 2959–2969 (2005).
Schindelin, J. et al. Fiji: an open-source platform for biological-image analysis. Nat. Methods 9, 676–682 (2012).
D'Argenio, D.Z., Schumitzky, A. & Wang, X. ADAPT 5 User's Guide: Pharmacokinetic/Pharmacodynamic Systems Analysis Software (Los Angeles: Biomedical Simulations Resource, 2009).
Beal, S.L. Ways to fit a PK model with some data below the quantification limit. J. Pharmacokinet. Pharmacodyn. 28, 481–504 (2001).
Brown, R.P., Delp, M.D., Lindstedt, S.L., Rhomberg, L.R. & Beliles, R.P. Physiological parameter values for physiologically based pharmacokinetic models. Toxicol. Ind. Health 13, 407–484 (1997).
Gargas, M.L. et al. Physiologically based pharmacokinetic modeling of chloroethane disposition in mice, rats, and women. Toxicol. Sci. 104, 54–66 (2008).
Kaliss, N. & Pressman, D. Plasma and blood volumes of mouse organs, as determined with radioactive iodoproteins. Proc. Soc. Exp. Biol. Med. 75, 16–20 (1950).
McIlwain, D.L., Hoke, V.B., Kopchick, J.J., Fuller, C.R. & Lund, P.K. Differential inhibition of postnatal brain, spinal cord and body growth by a growth hormone antagonist. BMC Neurosci. 5, 6 (2004).
Duhamel, G., Callot, V., Cozzone, P.J. & Kober, F. Spinal cord blood flow measurement by arterial spin labeling. Magn. Reson. Med. 59, 846–854 (2008).
Gibaldi, M. & Perrier, D. Pharmacokinetics 2nd edn (CRC Press, 1982).
Denney, W., Duvvuri, S. & Buckeridge, C. Simple, automatic noncompartmental analysis: the PKNCA R package. J. Pharmacokinet. Pharmacodyn. 42, S65 (2015).
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2016).
Brooks, B.P. et al. Characterization of an expanded glutamine repeat androgen receptor in a neuronal cell culture system. Neurobiol. Dis. 3, 313–323 (1997).
Acknowledgements
We thank N. Nedelsky for editorial assistance. We thank the transgenic core facility at St. Jude for production of AR121Q transgenic mice and ARC Technical Services at St. Jude for surgical and animal care assistance. We also thank W. Denney for guidance in use of the 'PKNCA' R package. This work was supported by the Howard Hughes Medical Institute (J.P.T.), the American-Lebanese-Syrian Associated Charities (J.P.T., H.T.), NIH R01 NS053825 (J.P.T.), NIH R01 NS100023 (A.R.L.), the Muscular Dystrophy Association (A.R.L.) and the Kennedy's Disease Association (H.C.M.).
Author information
Authors and Affiliations
Contributions
N.M.B., A.K., H.J.K., A.R.L. and J.P.T. designed the fruit fly, mouse and cell-based experiments. N.M.B., A.K. and H.C.M. performed the experiments and data analyses. P.K.V., Y.W. and B.B.F. performed the pharmacokinetics analyses. R.B.S., E.R.Q. and N.C.K. provided assistance in the fruit fly experiments. J.D., J. Messing, B.D.F. and P.-C.C. provided assistance in the mouse experiments. B.J.W. performed in silico docking of TA into the AR LBD and generated the structural depictions of the AR LBD. B.L.S. and A.P.K. performed the cloning and preparation of the constructs used to generate AR121Q transgenic mice. J. Moore and B.F. provided assistance in cell-based experiments for digital PCR. J. Moore provided assistance in mouse tissue and plasma collection for pharmacokinetics analysis. H.T. performed histopathologic analysis of AR121Q transgenic mice. Y.L. performed the sample size estimation (power analysis) and statistical QOL analysis. N.M.B., A.K., H.J.K. and J.P.T. wrote the manuscript. All of the authors provided scientific input and read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Figures & Table
Supplementary Figures 1-7 & Supplementary Table 1 (PDF 3158 kb)
Rights and permissions
About this article
Cite this article
Badders, N., Korff, A., Miranda, H. et al. Selective modulation of the androgen receptor AF2 domain rescues degeneration in spinal bulbar muscular atrophy. Nat Med 24, 427–437 (2018). https://doi.org/10.1038/nm.4500
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.4500
This article is cited by
-
LSD1/PRMT6-targeting gene therapy to attenuate androgen receptor toxic gain-of-function ameliorates spinobulbar muscular atrophy phenotypes in flies and mice
Nature Communications (2023)
-
Molecular Mechanisms and Therapeutics for SBMA/Kennedy's Disease
Neurotherapeutics (2019)
-
New strategy for SBMA therapy
Nature Reviews Drug Discovery (2018)