Abstract
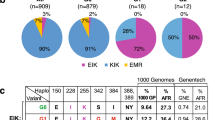
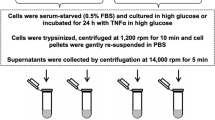
Soluble urokinase plasminogen activator receptor (suPAR) independently predicts chronic kidney disease (CKD) incidence and progression. Apolipoprotein L1 (APOL1) gene variants G1 and G2, but not the reference allele (G0), are associated with an increased risk of CKD in individuals of recent African ancestry. Here we show in two large, unrelated cohorts that decline in kidney function associated with APOL1 risk variants was dependent on plasma suPAR levels: APOL1-related risk was attenuated in patients with lower suPAR, and strengthened in those with higher suPAR levels. Mechanistically, surface plasmon resonance studies identified high-affinity interactions between suPAR, APOL1 and αvβ3 integrin, whereby APOL1 protein variants G1 and G2 exhibited higher affinity for suPAR-activated avb3 integrin than APOL1 G0. APOL1 G1 or G2 augments αvβ3 integrin activation and causes proteinuria in mice in a suPAR-dependent manner. The synergy of circulating factor suPAR and APOL1 G1 or G2 on αvβ3 integrin activation is a mechanism for CKD.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Chen, T.K., Estrella, M.M. & Parekh, R.S. The evolving science of apolipoprotein-L1 and kidney disease. Curr. Opin. Nephrol. Hypertens. 25, 217–225 (2016).
Tzur, S. et al. Missense mutations in the APOL1 gene are highly associated with end stage kidney disease risk previously attributed to the MYH9 gene. Hum. Genet. 128, 345–350 (2010).
Genovese, G. et al. Association of trypanolytic ApoL1 variants with kidney disease in African Americans. Science 329, 841–845 (2010).
Kao, W.H. et al. MYH9 is associated with nondiabetic end-stage renal disease in African Americans. Nat. Genet. 40, 1185–1192 (2008).
Parsa, A. et al. APOL1 risk variants, race, and progression of chronic kidney disease. N. Engl. J. Med. 369, 2183–2196 (2013).
Nichols, B. et al. Innate immunity pathways regulate the nephropathy gene Apolipoprotein L1. Kidney Int. 87, 332–342 (2015).
Papeta, N. et al. APOL1 variants increase risk for FSGS and HIVAN but not IgA nephropathy. J. Am. Soc. Nephrol. 22, 1991–1996 (2011).
Kopp, J.B. et al. APOL1 genetic variants in focal segmental glomerulosclerosis and HIV-associated nephropathy. J. Am. Soc. Nephrol. 22, 2129–2137 (2011).
Bruggeman, L.A. et al. APOL1-G0 or APOL1-G2 transgenic models develop preeclampsia but not kidney disease. J. Am. Soc. Nephrol. 27, 3600–3610 (2016).
Anderson, B.R. et al. In vivo modeling implicates APOL1 in nephropathy: evidence for dominant negative effects and epistasis under anemic stress. PLoS Genet. 11, e1005349 (2015).
Thunø, M., Macho, B. & Eugen-Olsen, J. suPAR: the molecular crystal ball. Dis. Markers 27, 157–172 (2009).
Sidenius, N. et al. Serum level of soluble urokinase-type plasminogen activator receptor is a strong and independent predictor of survival in human immunodeficiency virus infection. Blood 96, 4091–4095 (2000).
Ostrowski, S.R. et al. High plasma levels of intact and cleaved soluble urokinase receptor reflect immune activation and are independent predictors of mortality in HIV-1-infected patients. J. Acquir. Immune Defic. Syndr. 39, 23–31 (2005).
Hayek, S.S. et al. Soluble urokinase receptor and chronic kidney disease. N. Engl. J. Med. 373, 1916–1925 (2015).
Hahm, E. et al. Bone marrow–derived immature myeloid cells are a main source of circulating suPAR contributing to proteinuric kidney disease. Nat. Med. 23, 100–106 (2017).
Wei, C. et al. Modification of kidney barrier function by the urokinase receptor. Nat. Med. 14, 55–63 (2008).
Wei, C. et al. Circulating urokinase receptor as a cause of focal segmental glomerulosclerosis. Nat. Med. 17, 952–960 (2011).
Weckerle, A. et al. Characterization of circulating APOL1 protein complexes in African Americans. J. Lipid Res. 57, 120–130 (2016).
Ni, H., Li, A., Simonsen, N. & Wilkins, J.A. Integrin activation by dithiothreitol or Mn2+ induces a ligand-occupied conformation and exposure of a novel NH2-terminal regulatory site on the beta1 integrin chain. J. Biol. Chem. 273, 7981–7987 (1998).
Bruggeman, L.A. et al. Plasma apolipoprotein L1 levels do not correlate with CKD. J. Am. Soc. Nephrol. 25, 634–644 (2014).
Lan, X. et al. APOL1 risk variants enhance podocyte necrosis through compromising lysosomal membrane permeability. Am. J. Physiol. Renal Physiol. 307, F326–F336 (2014).
Wan, G. et al. Apolipoprotein L1, a novel Bcl-2 homology domain 3-only lipid-binding protein, induces autophagic cell death. J. Biol. Chem. 283, 21540–21549 (2008).
Tanida, I., Ueno, T. & Kominami, E. LC3 and autophagy. Methods Mol. Biol. 445, 77–88 (2008).
Sever, S. et al. Proteolytic processing of dynamin by cytoplasmic cathepsin L is a mechanism for proteinuric kidney disease. J. Clin. Invest. 117, 2095–2104 (2007).
Yaddanapudi, S. et al. CD2AP in mouse and human podocytes controls a proteolytic program that regulates cytoskeletal structure and cellular survival. J. Clin. Invest. 121, 3965–3980 (2011).
Shukha, K. et al. Most ApoL1 is secreted by the liver. J. Am. Soc. Nephrol. 28, 1079–1083 (2016).
Fu, Y. et al. APOL1–G1 in nephrocytes induces hypertrophy and accelerates cell death. J. Am. Soc. Nephrol. 28, 1106–1116 (2017).
Ma, L. et al. APOL1 renal-risk variants induce mitochondrial dysfunction. J. Am. Soc. Nephrol. 28, 1093–1105 (2017).
Friedman, D.J. & Pollak, M.R. Apolipoprotein L1 and kidney disease in African Americans. Trends Endocrinol. Metab. 27, 204–215 (2016).
Kruzel-Davila, E. et al. APOL1-mediated cell injury involves disruption of conserved trafficking processes. J. Am. Soc. Nephrol. 28, 1117–1130 (2017).
Cortese, K., Sahores, M., Madsen, C.D., Tacchetti, C. & Blasi, F. Clathrin and LRP-1-independent constitutive endocytosis and recycling of uPAR. PLoS One 3, e3730 (2008).
Czekay, R.P., Kuemmel, T.A., Orlando, R.A. & Farquhar, M.G. Direct binding of occupied urokinase receptor (uPAR) to LDL receptor-related protein is required for endocytosis of uPAR and regulation of cell surface urokinase activity. Mol. Biol. Cell 12, 1467–1479 (2001).
Yu, C.H. et al. Integrin-β3 clusters recruit clathrin-mediated endocytic machinery in the absence of traction force. Nat. Commun. 6, 8672 (2015).
Kobayashi, N. et al. Podocyte injury-driven intracapillary plasminogen activator inhibitor type 1 accelerates podocyte loss via uPAR-mediated β1-integrin endocytosis. Am. J. Physiol. Renal Physiol. 308, F614–F626 (2015).
Outinen, T.K. et al. Urine soluble urokinase-type plasminogen activator receptor levels correlate with proteinuria in Puumala hantavirus infection. J. Intern. Med. 276, 387–395 (2014).
Gavrilovskaya, I.N., Shepley, M., Shaw, R., Ginsberg, M.H. & Mackow, E.R. β3 Integrins mediate the cellular entry of hantaviruses that cause respiratory failure. Proc. Natl. Acad. Sci. USA 95, 7074–7079 (1998).
Beckerman, P. et al. Transgenic expression of human APOL1 risk variants in podocytes induces kidney disease in mice. Nat. Med. 23, 429–438 (2017).
Patel, R.S. et al. Circulating CD34+ progenitor cells and risk of mortality in a population with coronary artery disease. Circ. Res. 116, 289–297 (2015).
Eapen, D.J. et al. Soluble urokinase plasminogen activator receptor level is an independent predictor of the presence and severity of coronary artery disease and of future adverse events. J. Am. Heart Assoc. 3, e001118 (2014).
Levey, A.S. et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 150, 604–612 (2009).
Lee, H. et al. Reducing agents affect inhibitory activities of compounds: results from multiple drug targets. Anal. Biochem. 423, 46–53 (2012).
Saleem, M.A. et al. A conditionally immortalized human podocyte cell line demonstrating nephrin and podocin expression. J. Am. Soc. Nephrol. 13, 630–638 (2002).
Wu, M.J. et al. Rapamycin promotes podocyte migration through the up-regulation of urokinase receptor. Transplant. Proc. 46, 1226–1228 (2014).
Li, Y. et al. An anti-urokinase plasminogen activator receptor (uPAR) antibody: crystal structure and binding epitope. J. Mol. Biol. 365, 1117–1129 (2007).
Foster, M.C. et al. APOL1 variants associate with increased risk of CKD among African Americans. J. Am. Soc. Nephrol. 24, 1484–1491 (2013).
Harrell, F. Regression Modeling Strategies: with Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis (Springer, 2015).
Acknowledgements
We would like to acknowledge the members of the Emory Biobank Team, Emory Clinical Cardiovascular Research Institute (ECCRI) and Atlanta Clinical and Translational Science Institute for the recruitment of participants, compilation of data and preparation of samples. Specifically, we would like to acknowledge M. Awad, T. Varghese, W. Schultz, J. Patrick, M. Namara and A. Samman Tahhan (Emory University Department of Medicine) for assisting in data collection. We also appreciate A. Arnaout and B. Adair for the discussion of APOL1 and suPAR interaction. We are grateful to A.P. Mazar for providing anti-suPAR antibody ATN615. We thank R. Shemer, (Technion, Israel Institute of Technology) and A. Ofir (Rambam Medical Center, Haifa, Israel) for discussions and technical help.
Author information
Authors and Affiliations
Contributions
S.S.H., K.H.K. and C.W. designed and performed experiments, and wrote the paper; M.E.G. and Y.-A.K. contributed to data analysis; J.L., B.S., H.L., R.R.D., H.W.L., E.H., V.P., M.T., N.J.T., G.G. and N.S. contributed to experiments; K.S. participated in formulating aspects of study design relating to suPAR–APOL1 interaction and developing novel enabling reagents, and collaborated in the writing of the manuscript; V.G., M.M.A., C.A.W., M.S.L., A.T., L.A.I., A.S.L., M.Z., B.I.F., J.B.K. and J.C. contributed to the interpretation of data and manuscript revision; A.A.Q. established the Emory Cardiovascular Biobank that contributed all clinical samples and assisted in manuscript preparation; J.R. and S.S. designed and supervised the study, and wrote the paper. J.R. is supported by grants 5R01DK101350-03 (NIDDK) and 1R01DK106051 (NIDDK). A.A.Q. is supported by grants 5P01HL101398-02, 1P20HL113451-01, 1R56HL126558-01, 1RF1AG051633-01, R01 NS064162-01, R01 HL89650-01, HL095479-01, 1U10HL110302-01, 1DP3DK094346-01, 2P01HL086773-06A1 (NIH). M.E.G., J.C., A.S.L., L.A.I. and A.T. are supported by grants R01DK108803 (NIH) and U01DK085689 (NIDDK). J.C., A.S.L. and L.A.I. are supported by grant R01DK087961 (NIH). E.H. was supported by grant 1RO1 DK106051. Funding for the collection and management of samples was received from the Robert W. Woodruff Health Sciences Center Fund (Atlanta, GA), Emory Heart and Vascular Center (Atlanta, GA), Katz Family Foundation Preventive Cardiology Grant (Atlanta, GA), and National Institutes of Health (NIH) Grants UL1 RR025008 from the Clinical and Translational Science Award program and the Intramural Research Programs of NCI and NIDDK, NIH. This project has also been funded in part with federal funds from the National Cancer Institute, National Institutes of Health, under contract HHSN26120080001E. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does the mention of trade names, commercial products or organizations imply endorsement by the US Government. This research was supported in part by the Intramural Research Program of the NIH, National Cancer Institute, Center for Cancer Research.
Corresponding authors
Ethics declarations
Competing interests
J.R. and S.S. are cofounders of the biotech TRISAQ, and hold patents and stock in the space of proteinuric kidney disease. C.W. has a pending patent on suPAR in diabetic kidney disease. J.R., S.S., C.W. and E.H. are inventors on pending and issued patents related to anti-proteinuric therapies. They stand to gain royalties from present and future commercialization. J.C., A.S.L. and L.I. have a patent pending on GFR estimation and a collaboration agreement with Metabolon. Wake Forest University Health Sciences and B.F have filed for a patent related to APOL1 genetic testing. B.F receives research support from Novartis Pharmaceuticals and is a consultant for Ionis and AstraZeneca Pharmaceuticals.
Supplementary information
Supplementary Figures and Table
Supplementary Figures 1–7 and Supplementary Table 1 (PDF 1452 kb)
Rights and permissions
About this article
Cite this article
Hayek, S., Koh, K., Grams, M. et al. A tripartite complex of suPAR, APOL1 risk variants and αvβ3 integrin on podocytes mediates chronic kidney disease. Nat Med 23, 945–953 (2017). https://doi.org/10.1038/nm.4362
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.4362
This article is cited by
-
Role of biophysics and mechanobiology in podocyte physiology
Nature Reviews Nephrology (2024)
-
Gut Microbiota and Its Role in the Brain-Gut-Kidney Axis in Hypertension
Current Hypertension Reports (2023)
-
Role of Soluble Urokinase-Type Plasminogen Activator Receptor in Cardiovascular Disease
Current Cardiology Reports (2023)
-
SuPAR mediates viral response proteinuria by rapidly changing podocyte function
Nature Communications (2023)
-
The evolving story of apolipoprotein L1 nephropathy: the end of the beginning
Nature Reviews Nephrology (2022)