Abstract
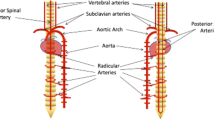
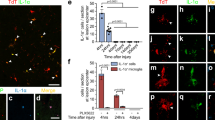
Blood vessels in the central nervous system (CNS) are controlled by neuronal activity. For example, widespread vessel constriction (vessel tone) is induced by brainstem neurons that release the monoamines serotonin and noradrenaline, and local vessel dilation is induced by glutamatergic neuron activity. Here we examined how vessel tone adapts to the loss of neuron-derived monoamines after spinal cord injury (SCI) in rats. We find that, months after the imposition of SCI, the spinal cord below the site of injury is in a chronic state of hypoxia owing to paradoxical excess activity of monoamine receptors (5-HT1) on pericytes, despite the absence of monoamines. This monoamine-receptor activity causes pericytes to locally constrict capillaries, which reduces blood flow to ischemic levels. Receptor activation in the absence of monoamines results from the production of trace amines (such as tryptamine) by pericytes that ectopically express the enzyme aromatic L-amino acid decarboxylase (AADC), which synthesizes trace amines directly from dietary amino acids (such as tryptophan). Inhibition of monoamine receptors or of AADC, or even an increase in inhaled oxygen, produces substantial relief from hypoxia and improves motoneuron and locomotor function after SCI.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Acker, T. & Acker, H. Cellular oxygen sensing need in CNS function: physiological and pathological implications. J. Exp. Biol. 207, 3171–3188 (2004).
Martirosyan, N.L. et al. Blood supply and vascular reactivity of the spinal cord under normal and pathological conditions. J. Neurosurg. Spine 15, 238–251 (2011).
Peña, F. & Ramirez, J.M. Hypoxia-induced changes in neuronal network properties. Mol. Neurobiol. 32, 251–283 (2005).
Hamilton, N.B., Attwell, D. & Hall, C.N. Pericyte-mediated regulation of capillary diameter: a component of neurovascular coupling in health and disease. Front. Neuroenergetics 2, 5 (2010).
Itoh, Y. & Suzuki, N. Control of brain capillary blood flow. J. Cereb. Blood Flow Metab. 32, 1167–1176 (2012).
Peppiatt, C.M., Howarth, C., Mobbs, P. & Attwell, D. Bidirectional control of CNS capillary diameter by pericytes. Nature 443, 700–704 (2006).
Reber, F., Gersch, U. & Funk, R.W. Blockers of carbonic anhydrase can cause increase of retinal capillary diameter, decrease of extracellular and increase of intracellular pH in rat retinal organ culture. Graefes Arch. Clin. Exp. Ophthalmol. 241, 140–148 (2003).
Barcroft, H., Bonnar, W.M., Edholm, O.G. & Effron, A.S. On sympathetic vasoconstrictor tone in human skeletal muscle. J. Physiol. (Lond.) 102, 21–31 (1943).
Westcott, E.B. & Segal, S.S. Perivascular innervation: a multiplicity of roles in vasomotor control and myoendothelial signaling. Microcirculation 20, 217–238 (2013).
Bonvento, G. et al. Evidence for differing origins of the serotonergic innervation of major cerebral arteries and small pial vessels in the rat. J. Neurochem. 56, 681–689 (1991).
Cohen, Z., Bonvento, G., Lacombe, P. & Hamel, E. Serotonin in the regulation of brain microcirculation. Prog. Neurobiol. 50, 335–362 (1996).
Cohen, Z., Molinatti, G. & Hamel, E. Astroglial and vascular interactions of noradrenaline terminals in the rat cerebral cortex. J. Cereb. Blood Flow Metab. 17, 894–904 (1997).
Lincoln, J. Innervation of cerebral arteries by nerves containing 5-hydroxytryptamine and noradrenaline. Pharmacol. Ther. 68, 473–501 (1995).
Hardebo, J.E. & Owman, C. Barrier mechanisms for neurotransmitter monoamines and their precursors at the blood-brain interface. Ann. Neurol. 8, 1–11 (1980).
Murray, K.C. et al. Recovery of motoneuron and locomotor function after spinal cord injury depends on constitutive activity in 5-HT2C receptors. Nat. Med. 16, 694–700 (2010).
Brown, A., Nabel, A., Oh, W., Etlinger, J.D. & Zeman, R.J. Perfusion imaging of spinal cord contusion: injury-induced blockade and partial reversal by β2-agonist treatment in rats. J. Neurosurg. Spine 20, 164–171 (2014).
Kang, C.E., Clarkson, R., Tator, C.H., Yeung, I.W. & Shoichet, M.S. Spinal cord blood flow and blood vessel permeability measured by dynamic computed tomography imaging in rats after localized delivery of fibroblast growth factor. J. Neurotrauma 27, 2041–2053 (2010).
Sinescu, C. et al. Molecular basis of vascular events following spinal cord injury. J. Med. Life 3, 254–261 (2010).
Kundi, S., Bicknell, R. & Ahmed, Z. The role of angiogenic and wound-healing factors after spinal cord injury in mammals. Neurosci. Res. 76, 1–9 (2013).
Murray, K.C. et al. Polysynaptic excitatory postsynaptic potentials that trigger spasms after spinal cord injury in rats are inhibited by 5-HT1B and 5-HT1F receptors. J. Neurophysiol. 106, 925–943 (2011).
Rank, M.M. et al. Adrenergic receptors modulate motoneuron excitability, sensory synaptic transmission and muscle spasms after chronic spinal cord injury. J. Neurophysiol. 105, 410–422 (2011).
Commissiong, J.W. The synthesis and metabolism of catecholamines in the spinal cord of the rat after acute and chronic transections. Brain Res. 347, 104–111 (1985).
Li, Y. et al. Synthesis, transport, and metabolism of serotonin formed from exogenously applied 5-HTP after spinal cord injury in rats. J. Neurophysiol. 111, 145–163 (2014).
Wienecke, J. et al. Spinal cord injury enables aromatic L-amino acid decarboxylase cells to synthesize monoamines. J. Neurosci. 34, 11984–12000 (2014).
Berry, M.D. Mammalian central nervous system trace amines. Pharmacologic amphetamines, physiologic neuromodulators. J. Neurochem. 90, 257–271 (2004).
Burchett, S.A. & Hicks, T.P. The mysterious trace amines: protean neuromodulators of synaptic transmission in mammalian brain. Prog. Neurobiol. 79, 223–246 (2006).
Gozal, E.A. et al. Anatomical and functional evidence for trace amines as unique modulators of locomotor function in the mammalian spinal cord. Front. Neural Circuits 8, 134 (2014).
Glaeser, B.S., Maher, T.J. & Wurtman, R.J. Changes in brain levels of acidic, basic, and neutral amino acids after consumption of single meals containing various proportions of protein. J. Neurochem. 41, 1016–1021 (1983).
Gessa, G.L., Biggio, G., Fadda, F., Corsini, G.U. & Tagliamonte, A. Effect of the oral administration of tryptophan-free amino acid mixtures on serum tryptophan, brain tryptophan and serotonin metabolism. J. Neurochem. 22, 869–870 (1974).
Hawkins, R.A., O'Kane, R.L., Simpson, I.A. & Viña, J.R. Structure of the blood-brain barrier and its role in the transport of amino acids. J. Nutr. 136 (Suppl. 1), 218S–226S (2006).
Boess, F.G. & Martin, I.L. Molecular biology of 5-HT receptors. Neuropharmacology 33, 275–317 (1994).
U'Prichard, D.C., Greenberg, D.A. & Snyder, S.H. Binding characteristics of a radiolabeled agonist and antagonist at central nervous system alpha noradrenergic receptors. Mol. Pharmacol. 13, 454–473 (1977).
Bunzow, J.R. et al. Amphetamine, 3,4-methylenedioxymethamphetamine, lysergic acid diethylamide, and metabolites of the catecholamine neurotransmitters are agonists of a rat trace amine receptor. Mol. Pharmacol. 60, 1181–1188 (2001).
Anwar, M.A., Ford, W.R., Broadley, K.J. & Herbert, A.A. Vasoconstrictor and vasodilator responses to tryptamine of rat-isolated perfused mesentery: comparison with tyramine and β-phenylethylamine. Br. J. Pharmacol. 165, 2191–2202 (2012).
Broadley, K.J., Fehler, M., Ford, W.R. & Kidd, E.J. Functional evaluation of the receptors mediating vasoconstriction of rat aorta by trace amines and amphetamines. Eur. J. Pharmacol. 715, 370–380 (2013).
Cohen, Z. et al. Multiple microvascular and astroglial 5-hydroxytryptamine receptor subtypes in human brain: molecular and pharmacologic characterization. J. Cereb. Blood Flow Metab. 19, 908–917 (1999).
Rennels, M.L. & Nelson, E. Capillary innervation in the mammalian central nervous system: an electron microscopic demonstration. Am. J. Anat. 144, 233–241 (1975).
Busija, D.W. & Leffler, C.W. Postjunctional alpha 2-adrenoceptors in pial arteries of anesthetized newborn pigs. Dev. Pharmacol. Ther. 10, 36–46 (1987).
Edvinsson, L., Degueurce, A., Duverger, D., MacKenzie, E.T. & Scatton, B. Central serotonergic nerves project to the pial vessels of the brain. Nature 306, 55–57 (1983).
Attwell, D. et al. Glial and neuronal control of brain blood flow. Nature 468, 232–243 (2010).
Winkler, E.A., Bell, R.D. & Zlokovic, B.V. Central nervous system pericytes in health and disease. Nat. Neurosci. 14, 1398–1405 (2011).
Xiong, Z. & Sperelakis, N. Regulation of L-type calcium channels of vascular smooth muscle cells. J. Mol. Cell. Cardiol. 27, 75–91 (1995).
Göritz, C. et al. A pericyte origin of spinal cord scar tissue. Science 333, 238–242 (2011).
Dalkara, T., Gursoy-Ozdemir, Y. & Yemisci, M. Brain microvascular pericytes in health and disease. Acta Neuropathol. 122, 1–9 (2011).
Hall, C.N. et al. Capillary pericytes regulate cerebral blood flow in health and disease. Nature 508, 55–60 (2014).
Burdyga, T. & Borysova, L. Calcium signalling in pericytes. J. Vasc. Res. 51, 190–199 (2014).
Di Narzo, A.F. et al. Decrease of mRNA editing after spinal cord injury is caused by down-regulation of ADAR2 that is triggered by inflammatory response. Sci. Rep. 5, 12615 (2015).
Unekawa, M. et al. RBC velocities in single capillaries of mouse and rat brains are the same, despite 10-fold difference in body size. Brain Res. 1320, 69–73 (2010).
Carreau, A., El Hafny-Rahbi, B., Matejuk, A., Grillon, C. & Kieda, C. Why is the partial oxygen pressure of human tissues a crucial parameter? Small molecules and hypoxia. J. Cell. Mol. Med. 15, 1239–1253 (2011).
Marina, N. et al. Brainstem hypoxia contributes to the development of hypertension in the spontaneously hypertensive rat. Hypertension 65, 775–783 (2015).
Schroeder, J.L., Highsmith, J.M., Young, H.F. & Mathern, B.E. Reduction of hypoxia by perfluorocarbon emulsion in a traumatic spinal cord injury model. J. Neurosurg. Spine 9, 213–220 (2008).
Wilson, R.J., Chersa, T. & Whelan, P.J. Tissue PO2 and the effects of hypoxia on the generation of locomotor-like activity in the in vitro spinal cord of the neonatal mouse. Neuroscience 117, 183–196 (2003).
van den Brand, R. et al. Restoring voluntary control of locomotion after paralyzing spinal cord injury. Science 336, 1182–1185 (2012).
Attwell, D., Mishra, A., Hall, C.N., O'Farrell, F.M. & Dalkara, T. What is a pericyte? J. Cereb. Blood Flow Metab. 36, 451–455 (2016).
Hill, R.A. et al. Regional blood flow in the normal and ischemic brain is controlled by arteriolar smooth muscle cell contractility and not by capillary pericytes. Neuron 87, 95–110 (2015).
Gorassini, M.A., Norton, J.A., Nevett-Duchcherer, J., Roy, F.D. & Yang, J.F. Changes in locomotor muscle activity after treadmill training in subjects with incomplete spinal cord injury. J. Neurophysiol. 101, 969–979 (2009).
Kapitza, S. et al. Tail spasms in rat spinal cord injury: changes in interneuronal connectivity. Exp. Neurol. 236, 179–189 (2012).
Beauparlant, J. et al. Undirected compensatory plasticity contributes to neuronal dysfunction after severe spinal cord injury. Brain 136, 3347–3361 (2013).
Navarrete-Opazo, A. & Mitchell, G.S. Therapeutic potential of intermittent hypoxia: a matter of dose. Am. J. Physiol. Regul. Integr. Comp. Physiol. 307, R1181–R1197 (2014).
Miller, G.M. The emerging role of trace amine-associated receptor 1 in the functional regulation of monoamine transporters and dopaminergic activity. J. Neurochem. 116, 164–176 (2011).
Acknowledgements
We thank F. Geddes and Y. Ma for technical assistance. This research was supported by the Canadian Institutes of Health Research (MOP 14697; D.J.B.) and the US National Institutes of Health (NIH, R01NS47567; D.J.B. and K.F.).
Author information
Authors and Affiliations
Contributions
Y.L. performed all in vitro rat experiments and in vivo pO2 measurements, contributed to all other rat studies and co-wrote the paper. R.V. and K.F. contributed to the rat in vivo locomotor experiments. I.R.W., K.F., R.V., L.S. and A.M.L.-O. contributed to immunolabeling experiments. I.R.W., L.S. and M.V.B. contributed to blood flow measurements. L.S. performed all sacral SCI surgeries. M.J.S., S.B. and K.K.F. contributed to analysis and editing. A.F.D.N. and S.D. performed mRNA-seq analysis. D.J.B. performed in vitro and in vivo rat experiments, directly supervised all the experiments and co-wrote the paper. K.F. and D.J.B. shared senior authorship.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–16 (PDF 5699 kb)
Rights and permissions
About this article
Cite this article
Li, Y., Lucas-Osma, A., Black, S. et al. Pericytes impair capillary blood flow and motor function after chronic spinal cord injury. Nat Med 23, 733–741 (2017). https://doi.org/10.1038/nm.4331
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.4331
This article is cited by
-
Blood-spinal cord barrier disruption in degenerative cervical myelopathy
Fluids and Barriers of the CNS (2023)
-
Oxygen therapy attenuates neuroinflammation after spinal cord injury
Journal of Neuroinflammation (2023)
-
Controlled delivery of a neurotransmitter–agonist conjugate for functional recovery after severe spinal cord injury
Nature Nanotechnology (2023)
-
The Provenance, Providence, and Position of Endothelial Cells in Injured Spinal Cord Vascular Pathology
Cellular and Molecular Neurobiology (2023)
-
Myelin Debris Impairs Tight Junctions and Promotes the Migration of Microvascular Endothelial Cells in the Injured Spinal Cord
Cellular and Molecular Neurobiology (2023)