Abstract
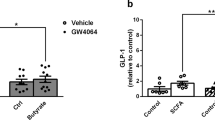
Type 2 diabetes is a major health problem worldwide, and one of its key features is the inability of elevated glucose to stimulate the release of sufficient amounts of insulin from pancreatic beta cells to maintain normal blood glucose levels1,2. New therapeutic strategies to improve beta cell function are therefore believed to be beneficial3,4. Here we demonstrate that the short-chain fatty acid receptors FFA2 (encoded by FFAR2) and FFA3 (encoded by FFAR3) are expressed in mouse and human pancreatic beta cells and mediate an inhibition of insulin secretion by coupling to Gi-type G proteins. We also provide evidence that mice with dietary-induced obesity and type 2 diabetes, as compared to non-obese control mice, have increased local formation by pancreatic islets of acetate, an endogenous agonist of FFA2 and FFA3, as well as increased systemic levels. This elevation may contribute to the insufficient capacity of beta cells to respond to hyperglycemia in obese states. Indeed, we found that genetic deletion of both receptors, either on the whole-body level or specifically in pancreatic beta cells, leads to greater insulin secretion and a profound improvement of glucose tolerance when mice are on a high-fat diet compared to controls. On the other hand, deletion of Ffar2 and Ffar3 in intestinal cells did not alter glucose tolerance in diabetic animals, suggesting these receptors act in a cell-autonomous manner in beta cells to regulate insulin secretion. In summary, under diabetic conditions elevated acetate acts on FFA2 and FFA3 to inhibit proper glucose-stimulated insulin secretion, and we expect antagonists of FFA2 and FFA3 to improve insulin secretion in type 2 diabetes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Nolan, C.J., Damm, P. & Prentki, M. Type 2 diabetes across generations: from pathophysiology to prevention and management. Lancet 378, 169–181 (2011).
Chen, L., Magliano, D.J. & Zimmet, P.Z. The worldwide epidemiology of type 2 diabetes mellitus–present and future perspectives. Nat. Rev. Endocrinol. 8, 228–236 (2012).
Tahrani, A.A., Bailey, C.J., Del Prato, S. & Barnett, A.H. Management of type 2 diabetes: new and future developments in treatment. Lancet 378, 182–197 (2011).
Vetere, A., Choudhary, A., Burns, S.M. & Wagner, B.K. Targeting the pancreatic β-cell to treat diabetes. Nat. Rev. Drug Discov. 13, 278–289 (2014).
Ashcroft, F.M. & Rorsman, P. Diabetes mellitus and the β cell: the last ten years. Cell 148, 1160–1171 (2012).
Rorsman, P. & Braun, M. Regulation of insulin secretion in human pancreatic islets. Annu. Rev. Physiol. 75, 155–179 (2013).
Ahrén, B. Islet G protein–coupled receptors as potential targets for treatment of type 2 diabetes. Nat. Rev. Drug Discov. 8, 369–385 (2009).
Sassmann, A. et al. The Gq/G11-mediated signaling pathway is critical for autocrine potentiation of insulin secretion in mice. J. Clin. Invest. 120, 2184–2193 (2010).
Ruiz de Azua, I., Gautam, D., Guettier, J.M. & Wess, J. Novel insights into the function of β-cell M3 muscarinic acetylcholine receptors: therapeutic implications. Trends Endocrinol. Metab. 22, 74–80 (2011).
Mancini, A.D. & Poitout, V. The fatty acid receptor FFA1/GPR40 a decade later: how much do we know? Trends Endocrinol. Metab. 24, 398–407 (2013).
Campbell, J.E. & Drucker, D.J. Pharmacology, physiology, and mechanisms of incretin hormone action. Cell Metab. 17, 819–837 (2013).
Rosengren, A.H. et al. Overexpression of α2A-adrenergic receptors contributes to type 2 diabetes. Science 327, 217–220 (2010).
Regard, J.B. et al. Probing cell type–specific functions of Gi in vivo identifies GPCR regulators of insulin secretion. J. Clin. Invest. 117, 4034–4043 (2007).
Stoddart, L.A., Smith, N.J. & Milligan, G. International Union of Pharmacology. LXXI. Free fatty acid receptors FFA1, -2, and -3: pharmacology and pathophysiological functions. Pharmacol. Rev. 60, 405–417 (2008).
Ulven, T. Short-chain free fatty acid receptors FFAR2/GPR43 and FFAR3/GPR41 as new potential therapeutic targets. Front. Endocrinol. (Lausanne) 3, 111 (2012).
Kebede, M.A., Alquier, T., Latour, M.G. & Poitout, V. Lipid receptors and islet function: therapeutic implications? Diabetes Obes. Metab. 11 (suppl. 4), 10–20 (2009).
Bjursell, M. et al. Improved glucose control and reduced body fat mass in free fatty acid receptor 2-deficient mice fed a high-fat diet. Am. J. Physiol. Endocrinol. Metab. 300, E211–E220 (2011).
Tolhurst, G. et al. Short-chain fatty acids stimulate glucagon-like peptide-1 secretion via the G-protein–coupled receptor FFAR2. Diabetes 61, 364–371 (2012).
Kimura, I. et al. The gut microbiota suppresses insulin-mediated fat accumulation via the short-chain fatty acid receptor GPR43. Nat. Commun. 4, 1829 (2013).
Samuel, B.S. et al. Effects of the gut microbiota on host adiposity are modulated by the short-chain fatty-acid binding G protein–coupled receptor, Gpr41. Proc. Natl. Acad. Sci. USA 105, 16767–16772 (2008).
Bellahcene, M. et al. Male mice that lack the G-protein-coupled receptor GPR41 have low energy expenditure and increased body fat content. Br. J. Nutr. 109, 1755–1764 (2013).
Lin, H.V. et al. Butyrate and propionate protect against diet-induced obesity and regulate gut hormones via free fatty acid receptor 3-independent mechanisms. PLoS ONE 7, e35240 (2012).
Zaibi, M.S. et al. Roles of GPR41 and GPR43 in leptin secretory responses of murine adipocytes to short chain fatty acids. FEBS Lett. 584, 2381–2386 (2010).
Ravassard, P. et al. A genetically engineered human pancreatic β cell line exhibiting glucose-inducible insulin secretion. J. Clin. Invest. 121, 3589–3597 (2011).
Brown, A.J. et al. The orphan G protein-coupled receptors GPR41 and GPR43 are activated by propionate and other short chain carboxylic acids. J. Biol. Chem. 278, 11312–11319 (2003).
Le Poul, E. et al. Functional characterization of human receptors for short chain fatty acids and their role in polymorphonuclear cell activation. J. Biol. Chem. 278, 25481–25489 (2003).
Buckley, B.M. & Williamson, D.H. Origins of blood acetate in the rat. Biochem. J. 166, 539–545 (1977).
Smith, R.F., Humphreys, S. & Hockaday, T.D. The measurement of plasma acetate by a manual or automated technique in diabetic and non-diabetic subjects. Ann. Clin. Biochem. 23, 285–291 (1986).
Todesco, T. et al. Plasma acetate levels in a group of obese diabetic, obese normoglycemic, and control subjects and their relationships with other blood parameters. Am. J. Gastroenterol. 88, 751–755 (1993).
Nøhr, M.K. et al. GPR41/FFAR3 and GPR43/FFAR2 as cosensors for short-chain fatty acids in enteroendocrine cells vs FFAR3 in enteric neurons and FFAR2 in enteric leukocytes. Endocrinology 154, 3552–3564 (2013).
Tazoe, H. et al. Roles of short-chain fatty acids receptors, GPR41 and GPR43 on colonic functions. J. Physiol. Pharmacol. 59 (suppl. 2), 251–262 (2008).
Madison, B.B. et al. Cis elements of the villin gene control expression in restricted domains of the vertical (crypt) and horizontal (duodenum, cecum) axes of the intestine. J. Biol. Chem. 277, 33275–33283 (2002).
Postic, C. et al. Dual roles for glucokinase in glucose homeostasis as determined by liver and pancreatic beta cell-specific gene knock-outs using Cre recombinase. J. Biol. Chem. 274, 305–315 (1999).
Wolever, T.M., Josse, R.G., Leiter, L.A. & Chiasson, J.L. Time of day and glucose tolerance status affect serum short-chain fatty acid concentrations in humans. Metabolism 46, 805–811 (1997).
Skutches, C.L., Holroyde, C.P., Myers, R.N., Paul, P. & Reichard, G.A. Plasma acetate turnover and oxidation. J. Clin. Invest. 64, 708–713 (1979).
Yamashita, H., Kaneyuki, T. & Tagawa, K. Production of acetate in the liver and its utilization in peripheral tissues. Biochim. Biophys. Acta 1532, 79–87 (2001).
Pouteau, E., Nguyen, P., Ballevre, O. & Krempf, M. Production rates and metabolism of short-chain fatty acids in the colon and whole body using stable isotopes. Proc. Nutr. Soc. 62, 87–93 (2003).
Layden, B.T., Yalamanchi, S.K., Wolever, T.M., Dunaif, A. & Lowe, W.L. Jr. Negative association of acetate with visceral adipose tissue and insulin levels. Diabetes Metab. Syndr. Obes. 5, 49–55 (2012).
Sakakibara, I. et al. Fasting-induced hypothermia and reduced energy production in mice lacking acetyl-CoA synthetase 2. Cell Metab. 9, 191–202 (2009).
Tiengo, A., Valerio, A., Molinari, M., Meneghel, A. & Lapolla, A. Effect of ethanol, acetaldehyde, and acetate on insulin and glucagon secretion in the perfused rat pancreas. Diabetes 30, 705–709 (1981).
Miyazaki, J. et al. Establishment of a pancreatic beta cell line that retains glucose-inducible insulin secretion: special reference to expression of glucose transporter isoforms. Endocrinology 127, 126–132 (1990).
Muyrers, J.P., Zhang, Y., Testa, G. & Stewart, A.F. Rapid modification of bacterial artificial chromosomes by ET-recombination. Nucleic Acids Res. 27, 1555–1557 (1999).
Ahmed, K. et al. An autocrine lactate loop mediates insulin-dependent inhibition of lipolysis through GPR81. Cell Metab. 11, 311–319 (2010).
van den Hoek, A.M. et al. Chronic PYY3-36 treatment promotes fat oxidation and ameliorates insulin resistance in C57BL6 mice. Am. J. Physiol. Endocrinol. Metab. 292, E238–E245 (2007).
Li, D.S., Yuan, Y.H., Tu, H.J., Liang, Q.L. & Dai, L.J. A protocol for islet isolation from mouse pancreas. Nat. Protoc. 4, 1649–1652 (2009).
Campbell, C.F. in Mouse Cell Culture: Methods and Protocols Vol. 633 (eds. Ward, A. & Tosh, D.) Ch. 14, 197–206 (Springer Science and Business Media, 2010).
Acknowledgements
The authors wish to thank S. Hümmer and S. Meaney-Gardian for secretarial help and K. Adolph and S. Kreutzer for technical support. H. Pijl (Leiden University Medical Centre) helped set up the hyperinsulinemic-euglycemic clamp, and P. Ravassard and R. Scharfmann (INSERM, Paris) provided EndoC-βH1 cells. This work was supported by funds through the Collaborative Research Center 1039 of the German Research Foundation and by the Max Planck Society.
Author information
Authors and Affiliations
Contributions
C.T. performed most of the experiments and analyzed and interpreted data; K.A. generated mice lacking Ffar2 and Ffar3; A.G. generated Ffar2 and Ffar3 reporter mice; S.L. helped with some of the in vivo experiments and with the histology; H.-J.G. performed histological analysis; S.T. performed expression analysis; S.O. analyzed and interpreted data, supervised the project and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Table 1 and Supplementary Figures 1–6 (PDF 3556 kb)
Rights and permissions
About this article
Cite this article
Tang, C., Ahmed, K., Gille, A. et al. Loss of FFA2 and FFA3 increases insulin secretion and improves glucose tolerance in type 2 diabetes. Nat Med 21, 173–177 (2015). https://doi.org/10.1038/nm.3779
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.3779
This article is cited by
-
Changes of the Concentration of Short-Chain Fatty Acids in the Intestines of Mice with Different Types of Obesity
Bulletin of Experimental Biology and Medicine (2024)
-
Can acetate via FFA receptors contribute to the diabetogenic effect of statins?
Naunyn-Schmiedeberg's Archives of Pharmacology (2024)
-
Non-target GC–MS analyses of fecal VOCs in NASH-hepatocellular carcinoma model STAM mice
Scientific Reports (2023)
-
Short-chain fatty acids: possible regulators of insulin secretion
Molecular and Cellular Biochemistry (2023)
-
A systematic review, meta-analysis, dose-response, and meta-regression of the effects of acarbose intake on glycemic markers in adults
Journal of Diabetes & Metabolic Disorders (2023)