Abstract
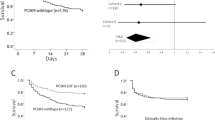
Liver disease is one of the leading causes of death worldwide1. Patients with cirrhosis display an increased predisposition to and mortality from infection due to multimodal defects in the innate immune system2,3,4; however, the causative mechanism has remained elusive. We present evidence that the cyclooxygenase (COX)-derived eicosanoid prostaglandin E2 (PGE2) drives cirrhosis-associated immunosuppression. We observed elevated circulating concentrations (more than seven times as high as in healthy volunteers) of PGE2 in patients with acute decompensation of cirrhosis. Plasma from these and patients with end-stage liver disease (ESLD) suppressed macrophage proinflammatory cytokine secretion and bacterial killing in vitro in a PGE2-dependent manner via the prostanoid type E receptor-2 (EP2), effects not seen with plasma from patients with stable cirrhosis (Child-Pugh score grade A). Albumin, which reduces PGE2 bioavailability, was decreased in the serum of patients with acute decompensation or ESLD (<30 mg/dl) and appears to have a role in modulating PGE2-mediated immune dysfunction. In vivo administration of human albumin solution to these patients significantly improved the plasma-induced impairment of macrophage proinflammatory cytokine production in vitro. Two mouse models of liver injury (bile duct ligation and carbon tetrachloride) also exhibited elevated PGE2, reduced circulating albumin concentrations and EP2-mediated immunosuppression. Treatment with COX inhibitors or albumin restored immune competence and survival following infection with group B Streptococcus. Taken together, human albumin solution infusions may be used to reduce circulating PGE2 levels, attenuating immune suppression and reducing the risk of infection in patients with acutely decompensated cirrhosis or ESLD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Lim, Y.S. & Kim, W.R. The global impact of hepatic fibrosis and end-stage liver disease. Clin. Liver Dis. 12, 733–746 (2008).
Fierer, J. & Finley, F. Deficient serum bactericidal activity against Escherichia coli in patients with cirrhosis of the liver. J. Clin. Invest. 63, 912–921 (1979).
Fernández, J. et al. Bacterial infections in cirrhosis: epidemiological changes with invasive procedures and norfloxacin prophylaxis. Hepatology 35, 140–148 (2002).
Moreau, R. et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 144, 1426–1437 (2013).
Fernández, J. et al. Prevalence and risk factors of infections by multiresistant bacteria in cirrhosis: a prospective study. Hepatology 55, 1551–1561 (2012).
O'Brien, A.J., Welch, C.A., Singer, M. & Harrison, D.A. Prevalence and outcome of cirrhosis patients admitted to UK intensive care: a comparison against dialysis-dependent chronic renal failure patients. Intensive Care Med. 38, 991–1000 (2012).
Hassner, A. et al. Impaired monocyte function in liver cirrhosis. Br. Med. J. (Clin. Res. Ed.) 282, 1262–1263 (1981).
Rajkovic, I.A. & Williams, R. Abnormalities of neutrophil phagocytosis, intracellular killing and metabolic activity in alcoholic cirrhosis and hepatitis. Hepatology 6, 252–262 (1986).
Shawcross, D.L. et al. Ammonia impairs neutrophil phagocytic function in liver disease. Hepatology 48, 1202–1212 (2008).
Fagiuoli, S. et al. Management of infections in cirrhotic patients: report of a consensus conference. Dig. Liver Dis. 46, 204–212 (2014).
Scher, J.U. & Pillinger, M.H. The anti-inflammatory effects of prostaglandins. J. Investig. Med. 57, 703–708 (2009).
Kalinski, P. Regulation of immune responses by prostaglandin E2. J. Immunol. 188, 21–28 (2012).
Fullerton, J.N., O'Brien, A.J. & Gilroy, D.W. Pathways mediating resolution of inflammation: when enough is too much. J. Pathol. 231, 8–20 (2013).
Fullerton, J.N., O'Brien, A.J. & Gilroy, D.W. Lipid mediators in immune dysfunction after severe inflammation. Trends Immunol. 35, 12–21 (2014).
Serezani, C.H. et al. Prostaglandin E2 suppresses bacterial killing in alveolar macrophages by inhibiting NADPH oxidase. Am. J. Respir. Cell Mol. Biol. 37, 562–570 (2007).
Bourdonnay, E., Serezani, C.H., Aronoff, D.M. & Peters-Golden, M. Regulation of alveolar macrophage p40phox: hierarchy of activating kinases and their inhibition by PGE2. J. Leukoc. Biol. 92, 219–231 (2012).
Aronoff, D.M., Canetti, C. & Peters-Golden, M. Prostaglandin E2 inhibits alveolar macrophage phagocytosis through an E-prostanoid 2 receptor-mediated increase in intracellular cyclic AMP. J. Immunol. 173, 559–565 (2004).
Medeiros, A.I., Serezani, C.H., Lee, S.P. & Peters-Golden, M. Efferocytosis impairs pulmonary macrophage and lung antibacterial function via PGE2/EP2 signaling. J. Exp. Med. 206, 61–68 (2009).
Bozyk, P.D. & Moore, B.B. Prostaglandin E2 and the pathogenesis of pulmonary fibrosis. Am. J. Respir. Cell Mol. Biol. 45, 445–452 (2011).
Yang, J., Petersen, C.E., Ha, C.E. & Bhagavan, N.V. Structural insights into human serum albumin-mediated prostaglandin catalysis. Protein Sci. 11, 538–545 (2002).
Wasmuth, H.E. et al. Patients with acute on chronic liver failure display “sepsis-like” immune paralysis. J. Hepatol. 42, 195–201 (2005).
Goss, J.A., Mangino, M.J. & Flye, M.W. Prostaglandin E2 production during hepatic regeneration downregulates Kupffer cell IL-6 production. Ann. Surg. 215, 553–559, discussion 559–560 (1992).
McAnulty, R.J., Hernandez-Rodriguez, N.A., Mutsaers, S.E., Coker, R.K. & Laurent, G.J. Indomethacin suppresses the anti-proliferative effects of transforming growth factor-beta isoforms on fibroblast cell cultures. Biochem. J. 321, 639–643 (1997).
Runyon, B.A. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology 57, 1651–1653 (2013).
Alves de Mattos, A. Current indications for the use of albumin in the treatment of cirrhosis. Ann. Hepatol. 10 (suppl. 1), S15–S20 (2011).
Mookerjee, R.P. et al. Neutrophil dysfunction in alcoholic hepatitis superimposed on cirrhosis is reversible and predicts the outcome. Hepatology 46, 831–840 (2007).
Garcia-Martinez, R. et al. Albumin: pathophysiologic basis of its role in the treatment of cirrhosis and its complications. Hepatology 58, 1836–1846 (2013).
Romanelli, R.G. et al. Long-term albumin infusion improves survival in patients with cirrhosis and ascites: an unblinded randomized trial. World J. Gastroenterol. 12, 1403–1407 (2006).
Georgiev, P. et al. Characterization of time-related changes after experimental bile duct ligation. Br. J. Surg. 95, 646–656 (2008).
Domenicali, M. et al. A novel model of CCl4-induced cirrhosis with ascites in the mouse. J. Hepatol. 51, 991–999 (2009).
Acknowledgements
We thank R. Mookerjee (Royal Free Hospital) for allowing use of samples from the DASIMAR study, N. Shah for collecting these samples and N. Davies for technical assistance. We also thank A. Healey for technical support and H. Antoniades for facilitating sample acquisition. E. coli and GBS clinical isolates were provided by V. Gant, University College London Hospitals. D.W.G. is a Wellcome Trust senior research fellow and support for work presented here was provided by the Wellcome Trust. Support was also provided by a grant from the National Institute of Health Research University College London Hospitals Biomedical Research Centre (A.J.O.).
Author information
Authors and Affiliations
Contributions
D.W.G. and A.J.O. conceived of the idea, and A.J.O. carried out the work. D.W.G. and A.J.O. cowrote the paper, and J.N.F. edited. J.N.F., G.S., J.N., S.J., E.K. and G.A. carried out biochemical assays, and W.A. (Royal London Hospitals), J.C. and R.G.-M. (both from ALFAE and MACHT clinical trials) supplied clinical samples. K.A.M. and A.N. carried out ESI/LC-MS/MS analysis, and A.W. carried out histological analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–5 and Supplementary Tables 1–4 (PDF 809 kb)
Rights and permissions
About this article
Cite this article
O'Brien, A., Fullerton, J., Massey, K. et al. Immunosuppression in acutely decompensated cirrhosis is mediated by prostaglandin E2. Nat Med 20, 518–523 (2014). https://doi.org/10.1038/nm.3516
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.3516
This article is cited by
-
Acute-on-chronic liver failure: far to go—a review
Critical Care (2023)
-
PPARγ-dependent hepatic macrophage switching acts as a central hub for hUCMSC-mediated alleviation of decompensated liver cirrhosis in rats
Stem Cell Research & Therapy (2023)
-
Cirrhosis-associated immune dysfunction
Nature Reviews Gastroenterology & Hepatology (2022)
-
Predictive accuracy of the modified SOFA score, SIRS criteria, and qSOFA score for uroseptic shock after mini-percutaneous nephrolithotomy
Urolithiasis (2022)
-
Use of human albumin infusion in cirrhotic patients: a systematic review and meta-analysis of randomized controlled trials
Hepatology International (2022)