Abstract
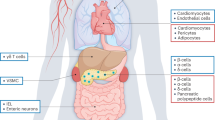
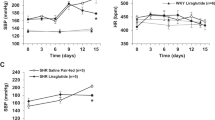
Glucagon-like peptide-1 receptor (GLP-1R) agonists exert antihypertensive actions through incompletely understood mechanisms. Here we demonstrate that cardiac Glp1r expression is localized to cardiac atria and that GLP-1R activation promotes the secretion of atrial natriuretic peptide (ANP) and a reduction of blood pressure. Consistent with an indirect ANP-dependent mechanism for the antihypertensive effects of GLP-1R activation, the GLP-1R agonist liraglutide did not directly increase the amount of cyclic GMP (cGMP) or relax preconstricted aortic rings; however, conditioned medium from liraglutide-treated hearts relaxed aortic rings in an endothelium-independent, GLP-1R–dependent manner. Liraglutide did not induce ANP secretion, vasorelaxation or lower blood pressure in Glp1r−/− or Nppa−/− mice. Cardiomyocyte GLP-1R activation promoted the translocation of the Rap guanine nucleotide exchange factor Epac2 (also known as Rapgef4) to the membrane, whereas Epac2 deficiency eliminated GLP-1R–dependent stimulation of ANP secretion. Plasma ANP concentrations were increased after refeeding in wild-type but not Glp1r−/− mice, and liraglutide increased urine sodium excretion in wild-type but not Nppa−/− mice. These findings define a gut-heart GLP-1R–dependent and ANP–dependent axis that regulates blood pressure.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Goldfine, A.B. Assessing the cardiovascular safety of diabetes therapies. N. Engl. J. Med. 359, 1092–1095 (2008).
Fonseca, V.A., Zinman, B., Nauck, M.A., Goldfine, A.B. & Plutzky, J. Confronting the type 2 diabetes epidemic: the emerging role of incretin-based therapies. Am. J. Med. 123, S2–S10 (2010).
Sivertsen, J., Rosenmeier, J., Holst, J.J. & Vilsboll, T. The effect of glucagon-like peptide 1 on cardiovascular risk. Nat. Rev. Cardiol. 9, 209–222 (2012).
Fonseca, V.A. Ongoing clinical trials evaluating the cardiovascular safety and efficacy of therapeutic approaches to diabetes mellitus. Am. J. Cardiol. 108, 52B–58B (2011).
Ussher, J.R. & Drucker, D.J. Cardiovascular biology of the incretin system. Endocr. Rev. 33, 187–215 (2012).
Drucker, D.J. & Nauck, M.A. The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet 368, 1696–1705 (2006).
Golpon, H.A., Puechner, A., Welte, T., Wichert, P.V. & Feddersen, C.O. Vasorelaxant effect of glucagon-like peptide7–36 amide and amylin on the pulmonary circulation of the rat. Regul. Pept. 102, 81–86 (2001).
Nyström, T. et al. Effects of glucagon-like peptide-1 on endothelial function in type 2 diabetes patients with stable coronary artery disease. Am. J. Physiol. Endocrinol. Metab. 287, E1209–E1215 (2004).
Chai, W. et al. Glucagon-like peptide 1 recruits microvasculature and increases glucose use in muscle via a nitric oxide–dependent mechanism. Diabetes 61, 888–898 (2012).
Vilsbøll, T., Christensen, M., Junker, A.E., Knop, F.K. & Gluud, L.L. Effects of glucagon-like peptide-1 receptor agonists on weight loss: systematic review and meta-analyses of randomised controlled trials. Br. Med. J. 344, d7771 (2012).
Crajoinas, R.O. et al. Mechanisms mediating the diuretic and natriuretic actions of the incretin hormone glucagon-like peptide-1. Am. J. Physiol. Renal Physiol. 301, F355–F363 (2011).
Hirata, K. et al. Exendin-4 has an anti-hypertensive effect in salt-sensitive mice model. Biochem. Biophys. Res. Commun. 380, 44–49 (2009).
Yu, M. et al. Antihypertensive effect of glucagon-like peptide 1 in Dahl salt-sensitive rats. J. Hypertens. 21, 1125–1135 (2003).
Gutzwiller, J.P. et al. Glucagon-like peptide 1 induces natriuresis in healthy subjects and in insulin-resistant obese men. J. Clin. Endocrinol. Metab. 89, 3055–3061 (2004).
Ban, K. et al. Cardioprotective and vasodilatory actions of glucagon-like peptide 1 receptor are mediated through both glucagon-like peptide 1 receptor-dependent and -independent pathways. Circulation 117, 2340–2350 (2008).
Drucker, D.J., Dritselis, A. & Kirkpatrick, P. Liraglutide. Nat. Rev. Drug Discov. 9, 267–268 (2010).
Scrocchi, L.A. et al. Glucose intolerance but normal satiety in mice with a null mutation in the glucagon-like peptide receptor gene. Nat. Med. 2, 1254–1258 (1996).
Holtwick, R. et al. Smooth muscle-selective deletion of guanylyl cyclase-A prevents the acute but not chronic effects of ANP on blood pressure. Proc. Natl. Acad. Sci. USA 99, 7142–7147 (2002).
Winquist, R.J. et al. Atrial natriuretic factor elicits an endothelium-independent relaxation and activates particulate guanylate cyclase in vascular smooth muscle. Proc. Natl. Acad. Sci. USA 81, 7661–7664 (1984).
Moore-Morris, T. et al. Identification of potential pharmacological targets by analysis of the comprehensive G protein–coupled receptor repertoire in the four cardiac chambers. Mol. Pharmacol. 75, 1108–1116 (2009).
Drucker, D.J., Philippe, J., Mojsov, S., Chick, W.L. & Habener, J.F. Glucagon-like peptide I stimulates insulin gene expression and increases cyclic AMP levels in a rat islet cell line. Proc. Natl. Acad. Sci. USA 84, 3434–3438 (1987).
Kang, G., Chepurny, O.G. & Holz, G.G. cAMP-regulated guanine nucleotide exchange factor II (Epac2) mediates Ca2+-induced Ca2+ release in INS-1 pancreatic β-cells. J. Physiol. (Lond.) 536, 375–385 (2001).
Shibasaki, T. et al. Essential role of Epac2/Rap1 signaling in regulation of insulin granule dynamics by cAMP. Proc. Natl. Acad. Sci. USA 104, 19333–19338 (2007).
Richards, A.M. et al. Effects of α-human atrial natriuretic peptide in essential hypertension. Hypertension 7, 812–817 (1985).
Carraro-Lacroix, L.R., Malnic, G. & Girardi, A.C. Regulation of Na+/H+ exchanger NHE3 by glucagon-like peptide 1 receptor agonist exendin-4 in renal proximal tubule cells. Am. J. Physiol. Renal Physiol. 297, F1647–F1655 (2009).
Kocinsky, H.S., Dynia, D.W., Wang, T. & Aronson, P.S. NHE3 phosphorylation at serines 552 and 605 does not directly affect NHE3 activity. Am. J. Physiol. Renal Physiol. 293, F212–F218 (2007).
Wei, Y. & Mojsov, S. Tissue-specific expression of the human receptor for glucagon-like peptide-I: brain, heart and pancreatic forms have the same deduced amino acid sequences. FEBS Lett. 358, 219–224 (1995).
Panjwani, N. et al. GLP-1 receptor activation indirectly reduces hepatic lipid accumulation but does not attenuate development of atherosclerosis in diabetic male ApoE−/− mice. Endocrinology 154, 127–139 (2013).
Smrcka, A.V., Brown, J.H. & Holz, G.G. Role of phospholipase Cɛ in physiological phosphoinositide signaling networks. Cell Signal. 24, 1333–1343 (2012).
Ballermann, B.J. A highly sensitive radioreceptor assay for atrial natriuretic peptide in rat plasma. Am. J. Physiol. 254, F159–F163 (1988).
Chattington, P.D. et al. Atrial natriuretic peptide in type 2 diabetes mellitus: response to a physiological mixed meal and relationship to renal function. Diabet. Med. 15, 375–379 (1998).
Noyan-Ashraf, M.H. et al. GLP-1R agonist liraglutide activates cytoprotective pathways and improves outcomes after experimental myocardial infarction in mice. Diabetes 58, 975–983 (2009).
Lønborg, J. et al. Exenatide reduces reperfusion injury in patients with ST-segment elevation myocardial infarction. Eur. Heart J. 33, 1491–1499 (2012).
Padmanabhan, S., Newton-Cheh, C. & Dominiczak, A.F. Genetic basis of blood pressure and hypertension. Trends Genet. 28, 397–408 (2012).
Moro, C. et al. Atrial natriuretic peptide contributes to physiological control of lipid mobilization in humans. FASEB J. 18, 908–910 (2004).
Birkenfeld, A.L. et al. Atrial natriuretic peptide induces postprandial lipid oxidation in humans. Diabetes 57, 3199–3204 (2008).
Bordicchia, M. et al. Cardiac natriuretic peptides act via p38 MAPK to induce the brown fat thermogenic program in mouse and human adipocytes. J. Clin. Invest. 122, 1022–1036 (2012).
Engeli, S. et al. Natriuretic peptides enhance the oxidative capacity of human skeletal muscle. J. Clin. Invest. 122, 4675–4679 (2012).
Ropero, A.B. et al. The atrial natriuretic peptide and guanylyl cyclase-A system modulates pancreatic β-cell function. Endocrinology 151, 3665–3674 (2010).
Zhang, J. et al. Nitro-oleic acid inhibits angiotensin II–induced hypertension. Circ. Res. 107, 540–548 (2010).
Yamamoto, H. et al. Glucagon-like peptide-1 receptor stimulation increases blood pressure and heart rate and activates autonomic regulatory neurons. J. Clin. Invest. 110, 43–52 (2002).
Shen, B., Ye, C.L., Ye, K.H., Zhuang, L. & Jiang, J.H. Doxorubicin-induced vasomotion and [Ca2+]i elevation in vascular smooth muscle cells from C57BL/6 mice. Acta Pharmacol. Sin. 30, 1488–1495 (2009).
Sambrano, G.R. et al. Navigating the signalling network in mouse cardiac myocytes. Nature 420, 712–714 (2002).
Wu, X. et al. MEK-ERK pathway modulation ameliorates disease phenotypes in a mouse model of Noonan syndrome associated with the Raf1L613V mutation. J. Clin. Invest. 121, 1009–1025 (2011).
Acknowledgements
We thank G. Kabir for assistance with mouse telemetry and G. Holz (State University of New York Upstate Medical University) for the provision of Epac2 virus constructs. These studies were carried out with support from the Heart and Stroke Foundation of Ontario HSFO NA6997, the Canada Research Chair in Regulatory Peptides, the Banting and Best Diabetes Centre–Novo Nordisk Chair in incretin biology, a grant from Novo Nordisk Inc. to D.J.D., Canadian Institutes of Health Research grant MOP 111159 to J.A.S. and grants to S.S. from the Japan Science and Technology Agency and the Ministry of Education, Culture, Sports, Science and Technology, Japan.
Author information
Authors and Affiliations
Contributions
M.K., M.J.P. and J.A.S. designed and carried out experiments, analyzed results and wrote the manuscript. M.K. was supported by a postdoctoral fellowship award from the Canadian Diabetes Association. S.S. provided Rapgef4−/− mice, interpreted results and wrote the manuscript. T.S. carried out experiments and reviewed the manuscript. S.E.Q. and P.H.B. helped design experiments and reviewed the manuscript. D.J.D. designed experiments, interpreted results and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
D.J.D. has served as a consultant to Amylin Pharmaceuticals Inc., Eli Lilly Inc., GlaxoSmithKline, Novo Nordisk Inc. and Sanofi Inc.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–8 (PDF 500 kb)
Rights and permissions
About this article
Cite this article
Kim, M., Platt, M., Shibasaki, T. et al. GLP-1 receptor activation and Epac2 link atrial natriuretic peptide secretion to control of blood pressure. Nat Med 19, 567–575 (2013). https://doi.org/10.1038/nm.3128
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.3128
This article is cited by
-
Chronic kidney outcomes associated with GLP-1 receptor agonists versus long-acting insulins among type 2 diabetes patients requiring intensive glycemic control: a nationwide cohort study
Cardiovascular Diabetology (2023)
-
Glucagon-like peptide 1 receptor agonists: cardiovascular benefits and mechanisms of action
Nature Reviews Cardiology (2023)
-
The expanding incretin universe: from basic biology to clinical translation
Diabetologia (2023)
-
Global trends and focuses of GLP-1RA in renal disease: a bibliometric analysis and visualization from 2005 to 2022
Naunyn-Schmiedeberg's Archives of Pharmacology (2023)
-
Association of glucagon-like peptide-1 receptor agonists with cardiac arrhythmias in patients with type 2 diabetes or obesity: a systematic review and meta-analysis of randomized controlled trials
Diabetology & Metabolic Syndrome (2022)