Abstract
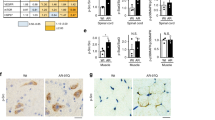
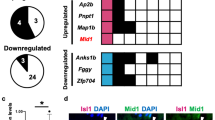
Spinal and bulbar muscular atrophy (SBMA) is a motor neuron disease caused by the expansion of the CAG triplet repeat within the androgen receptor (AR) gene. Here, we demonstrated that pathogenic AR upregulates the gene encoding calcitonin gene-related peptide α (CGRP1). In neuronal cells, overexpression of CGRP1 induced cellular damage via the activation of the c-Jun N-terminal kinase (JNK) pathway, whereas pharmacological suppression of CGRP1 or JNK attenuated the neurotoxic effects of pathogenic AR. The depletion of CGRP1 inactivated JNK and suppressed neurodegeneration in a mouse model of SBMA. Naratriptan, a serotonin 1B/1D (5-hydroxytryptamine 1B/1D, or 5-HT1B/1D) receptor agonist, decreased CGRP1 expression via the induction of dual-specificity protein phosphatase 1 (DUSP1), attenuated JNK activity and mitigated pathogenic AR-mediated neuronal damage in cellular and mouse SBMA models. These observations suggest that pharmacological activation of the 5-HT1B/1D receptor may be used therapeutically to treat SBMA and other polyglutamine-related neurodegenerative diseases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Accession codes
References
Ross, C.A. & Tabrizi, S.J. Huntington's disease: from molecular pathogenesis to clinical treatment. Lancet Neurol. 10, 83–98 (2011).
Gatchel, J.R. & Zoghbi, H.Y. Diseases of unstable repeat expansion: mechanisms and common principles. Nat. Rev. Genet. 6, 743–755 (2005).
Finsterer, J. Perspectives of Kennedy's disease. J. Neurol. Sci. 298, 1–10 (2010).
Katsuno, M. et al. Pathogenesis, animal models and therapeutics in spinal and bulbar muscular atrophy (SBMA). Exp. Neurol. 200, 8–18 (2006).
La Spada, A.R., Wilson, E.M., Lubahn, D.B., Harding, A.E. & Fischbeck, K.H. Androgen receptor gene mutations in X-linked spinal and bulbar muscular atrophy. Nature 352, 77–79 (1991).
Schmidt, B.J., Greenberg, C.R., Allingham-Hawkins, D.J. & Spriggs, E.L. Expression of X-linked bulbospinal muscular atrophy (Kennedy disease) in two homozygous women. Neurology 59, 770–772 (2002).
Sobue, G. et al. X-linked recessive bulbospinal neuronopathy. A clinicopathological study. Brain 112, 209–232 (1989).
Adachi, H. et al. Widespread nuclear and cytoplasmic accumulation of mutant androgen receptor in SBMA patients. Brain 128, 659–670 (2005).
Bauer, P.O. & Nukina, N. The pathogenic mechanisms of polyglutamine diseases and current therapeutic strategies. J. Neurochem. 110, 1737–1765 (2009).
Shao, J. & Diamond, M.I. Polyglutamine diseases: emerging concepts in pathogenesis and therapy. Hum. Mol. Genet. 16 Spec No. 2, R115–R123 (2007).
Katsuno, M. et al. Testosterone reduction prevents phenotypic expression in a transgenic mouse model of spinal and bulbar muscular atrophy. Neuron 35, 843–854 (2002).
Takeyama, K. et al. Androgen-dependent neurodegeneration by polyglutamine-expanded human androgen receptor in Drosophila. Neuron 35, 855–864 (2002).
Nedelsky, N.B. et al. Native functions of the androgen receptor are essential to pathogenesis in a Drosophila model of spinobulbar muscular atrophy. Neuron 67, 936–952 (2010).
Minamiyama, M. et al. Sodium butyrate ameliorates phenotypic expression in a transgenic mouse model of spinal and bulbar muscular atrophy. Hum. Mol. Genet. 13, 1183–1192 (2004).
Katsuno, M. et al. Reversible disruption of dynactin 1–mediated retrograde axonal transport in polyglutamine-induced motor neuron degeneration. J. Neurosci. 26, 12106–12117 (2006).
Ranganathan, S. et al. Mitochondrial abnormalities in spinal and bulbar muscular atrophy. Hum. Mol. Genet. 18, 27–42 (2009).
Katsuno, M. et al. Disrupted transforming growth factor-β signaling in spinal and bulbar muscular atrophy. J. Neurosci. 30, 5702–5712 (2010).
Steffan, J.S. et al. Histone deacetylase inhibitors arrest polyglutamine-dependent neurodegeneration in Drosophila. Nature 413, 739–743 (2001).
Butler, R. & Bates, G.P. Histone deacetylase inhibitors as therapeutics for polyglutamine disorders. Nat. Rev. Neurosci. 7, 784–796 (2006).
Luthi-Carter, R. et al. Decreased expression of striatal signaling genes in a mouse model of Huntington's disease. Hum. Mol. Genet. 9, 1259–1271 (2000).
Obrietan, K. & Hoyt, K.R. CRE-mediated transcription is increased in Huntington's disease transgenic mice. J. Neurosci. 24, 791–796 (2004).
Sugars, K.L. & Rubinsztein, D.C. Transcriptional abnormalities in Huntington disease. Trends Genet. 19, 233–238 (2003).
Mo, K. et al. Microarray analysis of gene expression by skeletal muscle of three mouse models of Kennedy disease/spinal bulbar muscular atrophy. PLoS ONE 5, e12922 (2010).
Ho, T.W., Edvinsson, L. & Goadsby, P.J. CGRP and its receptors provide new insights into migraine pathophysiology. Nat. Rev. Neurol. 6, 573–582 (2010).
Katsuno, M. et al. Leuprorelin rescues polyglutamine-dependent phenotypes in a transgenic mouse model of spinal and bulbar muscular atrophy. Nat. Med. 9, 768–773 (2003).
Popper, P. & Micevych, P.E. The effect of castration on calcitonin gene–related peptide in spinal motor neurons. Neuroendocrinology 50, 338–343 (1989).
Ma, W. et al. Localization and modulation of calcitonin gene-related peptide-receptor component protein-immunoreactive cells in the rat central and peripheral nervous systems. Neuroscience 120, 677–694 (2003).
Walker, C.S., Conner, A.C., Poyner, D.R. & Hay, D.L. Regulation of signal transduction by calcitonin gene–related peptide receptors. Trends Pharmacol. Sci. 31, 476–483 (2010).
Durham, P.L. & Russo, A.F. New insights into the molecular actions of serotonergic antimigraine drugs. Pharmacol. Ther. 94, 77–92 (2002).
Jhee, S.S., Shiovitz, T., Crawford, A.W. & Cutler, N.R. Pharmacokinetics and pharmacodynamics of the triptan antimigraine agents: a comparative review. Clin. Pharmacokinet. 40, 189–205 (2001).
Durham, P.L. & Russo, A.F. Serotonergic repression of mitogen-activated protein kinase control of the calcitonin gene–related peptide enhancer. Mol. Endocrinol. 12, 1002–1009 (1998).
Morfini, G. et al. JNK mediates pathogenic effects of polyglutamine-expanded androgen receptor on fast axonal transport. Nat. Neurosci. 9, 907–916 (2006).
Serra, H.G. et al. Gene profiling links SCA1 pathophysiology to glutamate signaling in Purkinje cells of transgenic mice. Hum. Mol. Genet. 13, 2535–2543 (2004).
Becanovic, K. et al. Transcriptional changes in Huntington disease identified using genome-wide expression profiling and cross-platform analysis. Hum. Mol. Genet. 19, 1438–1452 (2010).
Zheng, L.F. et al. Calcitonin gene–related peptide dynamics in rat dorsal root ganglia and spinal cord following different sciatic nerve injuries. Brain Res. 1187, 20–32 (2008).
Ringer, C., Weihe, E. & Schutz, B. Calcitonin gene–related peptide expression levels predict motor neuron vulnerability in the superoxide dismutase 1–G93A mouse model of amyotrophic lateral sclerosis. Neurobiol. Dis. 45, 547–554 (2012).
Ringer, C., Weihe, E. & Schutz, B. Pre-symptomatic alterations in subcellular betaCGRP distribution in motor neurons precede astrogliosis in ALS mice. Neurobiol. Dis. 35, 286–295 (2009).
Di Angelantonio, S., Giniatullin, R., Costa, V., Sokolova, E. & Nistri, A. Modulation of neuronal nicotinic receptor function by the neuropeptides CGRP and substance P on autonomic nerve cells. Br. J. Pharmacol. 139, 1061–1073 (2003).
Benemei, S., Nicoletti, P., Capone, J.A. & Geppetti, P. Pain pharmacology in migraine: focus on CGRP and CGRP receptors. Neurol. Sci. 28 (suppl. 2), S89–S93 (2007).
Disa, J., Parameswaran, N., Nambi, P. & Aiyar, N. Involvement of cAMP-dependent protein kinase and pertussis toxin–sensitive G-proteins in CGRP mediated JNK activation in human neuroblastoma cell line. Neuropeptides 34, 229–233 (2000).
Borsello, T. & Forloni, G. JNK signalling: a possible target to prevent neurodegeneration. Curr. Pharm. Des. 13, 1875–1886 (2007).
Perrin, V. et al. Implication of the JNK pathway in a rat model of Huntington's disease. Exp. Neurol. 215, 191–200 (2009).
Mehan, S., Meena, H., Sharma, D. & Sankhla, R. JNK: a stress-activated protein kinase therapeutic strategies and involvement in Alzheimer's and various neurodegenerative abnormalities. J. Mol. Neurosci. 43, 376–390 (2011).
Young, J.E. et al. Polyglutamine-expanded androgen receptor truncation fragments activate a Bax-dependent apoptotic cascade mediated by DP5/Hrk. J. Neurosci. 29, 1987–1997 (2009).
Edvinsson, L. & Goadsby, P.J. Neuropeptides in migraine and cluster headache. Cephalalgia 14, 320–327 (1994).
Katsuno, M. et al. for the Japan SBMA Interventional Trial for TAP-144-SR (JASMITT) study group. Efficacy and safety of leuprorelin in patients with spinal and bulbar muscular atrophy (JASMITT study): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet Neurol. 9, 875–884 (2010).
Fernández-Rhodes, L.E. et al. Efficacy and safety of dutasteride in patients with spinal and bulbar muscular atrophy: a randomised placebo-controlled trial. Lancet Neurol. 10, 140–147 (2011).
Niwa, H., Yamamura, K. & Miyazaki, J. Efficient selection for high-expression transfectants with a novel eukaryotic vector. Gene 108, 193–199 (1991).
Waza, M. et al. 17-AAG, an Hsp90 inhibitor, ameliorates polyglutamine-mediated motor neuron degeneration. Nat. Med. 11, 1088–1095 (2005).
Oh-hashi, Y. et al. Elevated sympathetic nervous activity in mice deficient in alphaCGRP. Circ. Res. 89, 983–990 (2001).
Adachi, H. et al. CHIP overexpression reduces mutant androgen receptor protein and ameliorates phenotypes of the spinal and bulbar muscular atrophy transgenic mouse model. J. Neurosci. 27, 5115–5126 (2007).
Tokui, K. et al. 17-DMAG ameliorates polyglutamine-mediated motor neuron degeneration through well-preserved proteasome function in an SBMA model mouse. Hum. Mol. Genet. 18, 898–910 (2009).
Acknowledgements
This work was supported by a Center-of-Excellence grant, a Grant-in-Aid for Scientific Research on Innovated Areas “Foundation of Synapse and Neurocircuit Pathology” (No. 22110005) and Grants-in-Aid from the Ministry of Education, Culture, Sports, Science and Technology, Japan (Nos. 21229011, 21689024 and 23390230); grants from the Ministry of Health, Labor and Welfare, Japan; Core Research for Evolutional Science and Technology (CREST) from Japan Science and Technology Agency (JST); and a grant from the Kennedy Disease Association.
Author information
Authors and Affiliations
Contributions
Project planning was performed by M.M., M.K., H.K. and G.S.; microarray analysis by M.M. and M.K.; cellular analysis by M.M., M.K., H.A., H.D., S.M. and Y.M.; primary motor neuron culture by M.K., S.I. and Y.F.; animal work by M.M., M.K., N.K. and M.I.; tissue staining by M.M., M.K. and M.I.; and data analysis by M.M., M.K., F.T. and G.S. M.M. and M.K. drafted the manuscript, and F.T., H.K. and G.S. revised it critically for intellectual content.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–15, Supplementary Table 1 and Supplementary Note (PDF 3248 kb)
Rights and permissions
About this article
Cite this article
Minamiyama, M., Katsuno, M., Adachi, H. et al. Naratriptan mitigates CGRP1-associated motor neuron degeneration caused by an expanded polyglutamine repeat tract. Nat Med 18, 1531–1538 (2012). https://doi.org/10.1038/nm.2932
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.2932
This article is cited by
-
Mid1 is associated with androgen-dependent axonal vulnerability of motor neurons in spinal and bulbar muscular atrophy
Cell Death & Disease (2022)
-
CGRP-Mediated Prolactin Upregulation: a Possible Pathomechanism in IgG4-Related Disease
Inflammation (2021)
-
Unveiling synapse pathology in spinal bulbar muscular atrophy by genome-wide transcriptome analysis of purified motor neurons derived from disease specific iPSCs
Molecular Brain (2020)
-
Src inhibition attenuates polyglutamine-mediated neuromuscular degeneration in spinal and bulbar muscular atrophy
Nature Communications (2019)
-
Gene expression analysis reveals early dysregulation of disease pathways and links Chmp7 to pathogenesis of spinal and bulbar muscular atrophy
Scientific Reports (2019)