Abstract
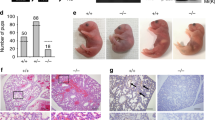
Although the lung is a defining feature of air-breathing animals, the pathway controlling the formation of type I pneumocytes, the cells that mediate gas exchange, is poorly understood. In contrast, the glucocorticoid receptor and its cognate ligand have long been known to promote type II pneumocyte maturation; prenatal administration of glucocorticoids is commonly used to attenuate the severity of infant respiratory distress syndrome (RDS). Here we show that knock-in mutations of the nuclear co-repressor SMRT (silencing mediator of retinoid and thyroid hormone receptors) in C57BL/6 mice (SMRTmRID) produces a previously unidentified respiratory distress syndrome caused by prematurity of the type I pneumocyte. Though unresponsive to glucocorticoids, treatment with anti–thyroid hormone drugs (propylthiouracil or methimazole) completely rescues SMRT-induced RDS, suggesting an unrecognized and essential role for the thyroid hormone receptor (TR) in lung development. We show that TR and SMRT control type I pneumocyte differentiation through Klf2, which, in turn, seems to directly activate the type I pneumocyte gene program. Conversely, mice without lung Klf2 lack mature type I pneumocytes and die shortly after birth, closely recapitulating the SMRTmRID phenotype. These results identify TR as a second nuclear receptor involved in lung development, specifically type I pneumocyte differentiation, and suggest a possible new type of therapeutic option in the treatment of RDS that is unresponsive to glucocorticoids.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Accession codes
References
Metzger, R.J., Klein, O.D., Martin, G.R. & Krasnow, M.A. The branching programme of mouse lung development. Nature 453, 745–750 (2008).
Stripp, B.R. Hierarchical organization of lung progenitor cells: is there an adult lung tissue stem cell? Proc. Am. Thorac. Soc. 5, 695–698 (2008).
Williams, M.C. Alveolar type I cells: molecular phenotype and development. Annu. Rev. Physiol. 65, 669–695 (2003).
Dobbs, L.G., Johnson, M.D., Vanderbilt, J., Allen, L. & Gonzalez, R. The great big alveolar TI cell: evolving concepts and paradigms. Cell. Physiol. Biochem. 25, 55–62 (2010).
Herzog, E.L., Brody, A.R., Colby, T.V., Mason, R. & Williams, M.C. Knowns and unknowns of the alveolus. Proc. Am. Thorac. Soc. 5, 778–782 (2008).
Evans, R. A transcriptional basis for physiology. Nat. Med. 10, 1022–1026 (2004).
Chen, J.D. & Evans, R.M. A transcriptional co-repressor that interacts with nuclear hormone receptors. Nature 377, 454–457 (1995).
Bookout, A.L. et al. Anatomical profiling of nuclear receptor expression reveals a hierarchical transcriptional network. Cell 126, 789–799 (2006).
Privalsky, M.L. The role of corepressors in transcriptional regulation by nuclear hormone receptors. Annu. Rev. Physiol. 66, 315–360 (2004).
Hu, X. & Lazar, M.A. The CoRNR motif controls the recruitment of corepressors by nuclear hormone receptors. Nature 402, 93–96 (1999).
Jepsen, K. & Rosenfeld, M.G. Biological roles and mechanistic actions of co-repressor complexes. J. Cell Sci. 115, 689–698 (2002).
Perissi, V., Jepsen, K., Glass, C.K. & Rosenfeld, M.G. Deconstructing repression: evolving models of co-repressor action. Nat. Rev. Genet. 11, 109–123 (2010).
Jones, P.L. & Shi, Y.B. N-CoR-HDAC corepressor complexes: roles in transcriptional regulation by nuclear hormone receptors. Curr. Top. Microbiol. Immunol. 274, 237–268 (2003).
Nofsinger, R.R. et al. SMRT repression of nuclear receptors controls the adipogenic set point and metabolic homeostasis. Proc. Natl. Acad. Sci. USA 105, 20021–20026 (2008).
Morrisey, E.E. & Hogan, B.L. Preparing for the first breath: genetic and cellular mechanisms in lung development. Dev. Cell 18, 8–23 (2010).
Mendelson, C.R. Role of transcription factors in fetal lung development and surfactant protein gene expression. Annu. Rev. Physiol. 62, 875–915 (2000).
Zhang, Y. et al. GATA and Nkx factors synergistically regulate tissue-specific gene expression and development in vivo. Development 134, 189–198 (2007).
Burrow, G.N., Fisher, D.A. & Larsen, P.R. Maternal and fetal thyroid function. N. Engl. J. Med. 331, 1072–1078 (1994).
Fraichard, A. et al. The T3Rα gene encoding a thyroid hormone receptor is essential for post-natal development and thyroid hormone production. EMBO J. 16, 4412–4420 (1997).
Wikström, L. et al. Abnormal heart rate and body temperature in mice lacking thyroid hormone receptor α 1. EMBO J. 17, 455–461 (1998).
Saltó, C. et al. Ablation of TRα2 and a concomitant overexpression of α1 yields a mixed hypo- and hyperthyroid phenotype in mice. Mol. Endocrinol. 15, 2115–2128 (2001).
Gauthier, K. et al. Genetic analysis reveals different functions for the products of the thyroid hormone receptor α locus. Mol. Cell. Biol. 21, 4748–4760 (2001).
Forrest, D. et al. Recessive resistance to thyroid hormone in mice lacking thyroid hormone receptor β: evidence for tissue-specific modulation of receptor function. EMBO J. 15, 3006–3015 (1996).
Hetzel, B.S. & Mano, M.T. A review of experimental studies of iodine deficiency during fetal development. J. Nutr. 119, 145–151 (1989).
Barish, G.D. et al. Bcl-6 and NF-κB cistromes mediate opposing regulation of the innate immune response. Genes Dev. 24, 2760–2765 (2010).
Wani, M.A., Wert, S.E. & Lingrel, J.B. Lung Kruppel-like factor, a zinc finger transcription factor, is essential for normal lung development. J. Biol. Chem. 274, 21180–21185 (1999).
Wani, M.A., Means, R.T. Jr. & Lingrel, J.B. Loss of LKLF function results in embryonic lethality in mice. Transgenic Res. 7, 229–238 (1998).
Kuo, C.T. et al. The LKLF transcription factor is required for normal tunica media formation and blood vessel stabilization during murine embryogenesis. Genes Dev. 11, 2996–3006 (1997).
Warburton, D. et al. The molecular basis of lung morphogenesis. Mech. Dev. 92, 55–81 (2000).
Whitsett, J.A., Wert, S.E. & Trapnell, B.C. Genetic disorders influencing lung formation and function at birth. Hum. Mol. Genet. 13 (Spec No 2), R207–R215 (2004).
Domyan, E.T. & Sun, X. Patterning and plasticity in development of the respiratory lineage. Dev. Dyn. 240, 477–485 (2011).
Sheppard, D. Functions of pulmonary epithelial integrins: from development to disease. Physiol. Rev. 83, 673–686 (2003).
Minoo, P., Su, G., Drum, H., Bringas, P. & Kimura, S. Defects in tracheoesophageal and lung morphogenesis in Nkx2.1−/− mouse embryos. Dev. Biol. 209, 60–71 (1999).
Chen, G. et al. SPDEF is required for mouse pulmonary goblet cell differentiation and regulates a network of genes associated with mucus production. J. Clin. Invest. 119, 2914–2924 (2009).
Tsao, P.N. et al. Notch signaling controls the balance of ciliated and secretory cell fates in developing airways. Development 136, 2297–2307 (2009).
Borges, M. et al. An achaete-scute homologue essential for neuroendocrine differentiation in the lung. Nature 386, 852–855 (1997).
Morimoto, M. et al. Canonical Notch signaling in the developing lung is required for determination of arterial smooth muscle cells and selection of Clara versus ciliated cell fate. J. Cell Sci. 123, 213–224 (2010).
Mendelsohn, C. et al. Function of the retinoic acid receptors (RARs) during development (II). Multiple abnormalities at various stages of organogenesis in RAR double mutants. Development 120, 2749–2771 (1994).
Gross, I. Regulation of fetal lung maturation. Am. J. Physiol. 259, L337–L344 (1990).
Merrill, J.D. & Ballard, R.A. Antenatal hormone therapy for fetal lung maturation. Clin. Perinatol. 25, 983–997 (1998).
NIH Consensus Development Panel on the Effect of Corticosteroids for Fetal Maturation on Perinatal Outcomes. Effect of corticosteroids for fetal maturation on perinatal outcomes. J. Am. Med. Assoc. 273, 413–418 (1995).
Bizzarro, M.J. & Gross, I. Effects of hormones on fetal lung development. Obstet. Gynecol. Clin. North Am. 31, 949–961 (2004).
Purdy, I.B. & Wiley, D.J. Perinatal corticosteroids: a review of research. Part I: antenatal administration. Neonatal Netw. 23, 15–30 (2004).
Ho, N.K. Factors affecting responses of infants with respiratory distress syndrome to exogenous surfactant therapy. Singapore Med. J. 34, 74–77 (1993).
Lim, B.K. et al. Coxsackievirus and adenovirus receptor (CAR) mediates atrioventricular-node function and connexin 45 localization in the murine heart. J. Clin. Invest. 118, 2758–2770 (2008).
Zhang, Y., Conrad, A.H. & Conrad, G.W. Detection and quantification of 3,5,3′-triiodothyronine and 3,3′,5′-triiodothyronine by electrospray ionization tandem mass spectrometry. J. Am. Soc. Mass Spectrom. 16, 1781–1786 (2005).
Yue, B. et al. Free thyroid hormones in serum by direct equilibrium dialysis and online solid-phase extraction–liquid chromatography/tandem mass spectrometry. Clin. Chem. 54, 642–651 (2008).
Hsiao, A., Ideker, T., Olefsky, J.M. & Subramaniam, S. VAMPIRE microarray suite: a web-based platform for the interpretation of gene expression data. Nucleic Acids Res. 33, W627–W632 (2005).
Pei, L. et al. NR4A orphan nuclear receptors are transcriptional regulators of hepatic glucose metabolism. Nat. Med. 12, 1048–1055 (2006).
Nelson, J.D., Denisenko, O. & Bomsztyk, K. Protocol for the fast chromatin immunoprecipitation (ChIP) method. Nat. Protoc. 1, 179–185 (2006).
Acknowledgements
We thank H. Juguilon, M. Karunasiri, S. Kaufman and Y. Dayn for technical support, J. Stubbs, C. Kintner, L. Nagy, S.-H. Hong, J. Jonker and J. Fitzpatrick for helpful discussions, M. Montminy of Salk Institute for GFP adenovirus, J. Simon, L. Grabowski and J. Belcovson for artistic work, and E. Ong and S. Ganley for administrative assistance. We appreciate the help and expertise from M. Wood for the electron microscopy study. We thank J. Codey and the Leona M. and Harry B. Helmsley Charitable Trust for their generous support. L.P. is a Parker B. Francis Fellow supported by the Francis Family Foundation. R.M.E. is an investigator of the Howard Hughes Medical Institute at the Salk Institute for Biological Studies and March of Dimes Chair in Molecular and Developmental Biology. This work was supported by the Howard Hughes Medical Institute and US National Institutes of Health grants 2RO1DK057978, 2RO1HL105278, 5U19DK062434 (R.M.E.) and RO1HL57281 (J.B.L.).
Author information
Authors and Affiliations
Contributions
L.P. led the project and designed and performed most of the experiments. M.L. is a pathologist who evaluated all the anatomy, histology and staining results. A.A. analyzed the blood T4 and rT3 levels in newborn pups using mass spectrometry. R.N. generated the SMRT knock-in mice. R.T.Y. analyzed the microarray data. H.-R.L. provided expertise in electron microscopy studies. G.B., J.W., D.G., M.H., K.K., M.D., H.C.P. and J.B.L. provided intellectual input and technical expertise. J.B.L. provided the Klf2−/− ES cells. R.M.E. supervised the project. L.P. and R.M.E. wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–12 and Supplementary Tables 1–4. (PDF 1106 kb)
Rights and permissions
About this article
Cite this article
Pei, L., Leblanc, M., Barish, G. et al. Thyroid hormone receptor repression is linked to type I pneumocyte–associated respiratory distress syndrome. Nat Med 17, 1466–1472 (2011). https://doi.org/10.1038/nm.2450
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.2450
This article is cited by
-
Stability selection enhances feature selection and enables accurate prediction of gestational age using only five DNA methylation sites
Clinical Epigenetics (2023)
-
RNA sequencing for global gene expression associated with muscle growth in a single male modern broiler line compared to a foundational Barred Plymouth Rock chicken line
BMC Genomics (2017)
-
Phycocyanin attenuates pulmonary fibrosis via the TLR2-MyD88-NF-κB signaling pathway
Scientific Reports (2017)
-
Piezo2 senses airway stretch and mediates lung inflation-induced apnoea
Nature (2017)
-
Two nested developmental waves demarcate a compartment boundary in the mouse lung
Nature Communications (2014)