Abstract
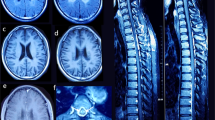
Leukoencephalopathy with brain stem and spinal cord involvement and lactate elevation (LBSL) has recently been defined based on a highly characteristic constellation of abnormalities observed by magnetic resonance imaging and spectroscopy1. LBSL is an autosomal recessive disease, most often manifesting in early childhood. Affected individuals develop slowly progressive cerebellar ataxia, spasticity and dorsal column dysfunction, sometimes with a mild cognitive deficit or decline. We performed linkage mapping with microsatellite markers in LBSL families and found a candidate region on chromosome 1, which we narrowed by means of shared haplotypes. Sequencing of genes in this candidate region uncovered mutations in DARS2, which encodes mitochondrial aspartyl-tRNA synthetase, in affected individuals from all 30 families. Enzyme activities of mutant proteins were decreased. We were surprised to find that activities of mitochondrial complexes from fibroblasts and lymphoblasts derived from affected individuals were normal, as determined by different assays.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
van der Knaap, M.S. et al. A new leukoencephalopathy with brainstem and spinal cord involvement and high lactate. Ann. Neurol. 53, 252–258 (2003).
van der Knaap, M.S. & Valk, J. Magnetic Resonance of Myelination and Myelin Disorders (Springer Verlag, Berlin, 2005).
Linnankivi, T. et al. Five new cases of a recently described leukoencephalopathy with high brain lactate. Neurology 63, 688–692 (2004).
Serkov, S.V. et al. Five patients with a recently described novel leukoencephalopathy with brainstem and spinal cord involvement and elevated lactate. Neuropediatrics 35, 1–5 (2004).
Petzold, G.C. et al. Adult onset leucoencephalopathy with brain stem and spinal cord involvement and normal lactate. J. Neurol. Neurosurg. Psychiatry 77, 889–891 (2006).
Eiler, S., Dock-Bregeon, A., Moulinier, L., Thierry, J.C. & Moras, D. Synthesis of aspartyl-tRNA(Asp) in Escherichia coli–a snapshot of the second step. EMBO J. 18, 6532–6541 (1999).
Smeitink, J.A. et al. Distinct clinical phenotypes associated with a mutation in the mitochondrial translation elongation factor EFTs. Am. J. Hum. Genet. 79, 869–877 (2006).
Coenen, M.J. et al. Mutant mitochondrial elongation factor G1 and combined oxidative phosphorylation deficiency. N. Engl. J. Med. 351, 2080–2086 (2004).
DiMauro, S. & Schon, E.A. Mitochondrial respiratory-chain diseases. N. Engl. J. Med. 348, 2656–2668 (2003).
Schapira, A.H. Mitochondrial disease. Lancet 368, 70–82 (2006).
Shoubridge, E.A. Nuclear genetic defects of oxidative phosphorylation. Hum. Mol. Genet. 10, 2277–2284 (2001).
Dittmar, K.A., Goodenbour, J.M. & Pan, T. Tissue-specific differences in human transfer RNA expression. PLoS Genet. 2, e221 (2006).
Park, S.G., Ewalt, K.L. & Kim, S. Functional expansion of aminoacyl-tRNA synthetases and their interacting factors: new perspectives on housekeepers. Trends Biochem. Sci. 30, 569–574 (2005).
Bonnefond, L. et al. Toward the full set of human mitochondrial aminoacyl-tRNA synthetases: characterization of AspRS and TyrRS. Biochemistry 44, 4805–4816 (2005).
Seneca, S. et al. A mitochondrial tRNA aspartate mutation causing isolated mitochondrial myopathy. Am. J. Med. Genet. A. 137, 170–175 (2005).
Jordanova, A. et al. Disrupted function and axonal distribution of mutant tyrosyl-tRNA synthetase in dominant intermediate Charcot-Marie-Tooth neuropathy. Nat. Genet. 38, 197–202 (2006).
Antonellis, A. et al. Glycyl tRNA synthetase mutations in Charcot-Marie-Tooth disease type 2D and distal spinal muscular atrophy type V. Am. J. Hum. Genet. 72, 1293–1299 (2003).
Lee, J.W. et al. Editing-defective tRNA synthetase causes protein misfolding and neurodegeneration. Nature 443, 50–55 (2006).
Antonellis, A. et al. Functional analyses of glycyl-tRNA synthetase mutations suggest a key role for tRNA-charging enzymes in peripheral axons. J. Neurosci. 26, 10397–10406 (2006).
Jacobs, H.T. & Turnbull, D.M. Nuclear genes and mitochondrial translation: a new class of genetic disease. Trends Genet. 21, 312–314 (2005).
't Hart, L.M. et al. Evidence that the mitochondrial leucyl tRNA synthetase (LARS2) gene represents a novel type 2 diabetes susceptibility gene. Diabetes 54, 1892–1895 (2005).
Leegwater, P.A. et al. The gene for leukoencephalopathy with vanishing white matter is located on chromosome 3q27. Am. J. Hum. Genet. 65, 728–734 (1999).
Forshew, T. & Johnson, C.A. SCAMP: a spreadsheet to collate autozygosity mapping projects. J. Med. Genet. 41, e125 (2004).
Gudbjartsson, D.F., Jonasson, K., Frigge, M.L. & Kong, A. Allegro, a new computer program for multipoint linkage analysis. Nat. Genet. 25, 12–13 (2000).
van Kollenburg, B. et al. Glia-specific activation of all pathways of the unfolded protein response in vanishing white matter disease. J. Neuropathol. Exp. Neurol. 65, 707–715 (2006).
Jacobs, E.H. et al. Active heroin administration induces specific genomic responses in the nucleus accumbens shell. FASEB J. 16, 1961–1963 (2002).
Scholte, H.R. et al. Assessment of deficiencies of fatty acyl-CoA dehydrogenases in fibroblasts, muscle and liver. J. Inherit. Metab. Dis. 15, 347–352 (1992).
Smet, J., Devreese, B., van Beeumen, J. & van Coster, R. Nondenaturing polyacrylamide gel electrophoresis as a method for studying protein interactions: applications in the analysis of mitochondrial OXPHOS complexes. in Cell Biology: a Laboratory Handbook (ed. Celis, J.) 259–264 (Academic, San Diego, 2005).
Van Coster, R. et al. Blue native polyacrylamide gel electrophoresis: a powerful tool in diagnosis of oxidative phosphorylation defects. Pediatr. Res. 50, 658–665 (2001).
de Paepe, B. et al. Diagnostic value of immunostaining in cultured skin fibroblasts from patients with oxidative phosphorylation defects. Pediatr. Res. 59, 2–6 (2006).
Acknowledgements
We thank P. Heutink for helpful discussions. We thank J. Powers for critical reading of the manuscript. We thank K. de Groot and T. Vriesman for technical assistance. We are grateful for the generous collaboration of many colleagues and most of all for the contributions from LBSL patients and their families. This study was supported by ZonMW (TOP grant 9120.6002), the Optimix Foundation for Scientific Research and the Centre for Medical Systems Biology (CMSB), a center of excellence approved by the Netherlands Genomics Initiative/Netherlands Organisation for Scientific Research (NWO).
Author information
Authors and Affiliations
Contributions
G.C.S. supervised the genetic study and cloned and purified the wild-type and mutant proteins. T.v.d.K. performed the genome-wide scan. R.J.v.A. and C.G.M.v.B. performed sequence analysis. M.S. and C.F. were involved in the synthetase assay. J.S. and R.V.C. contributed to the measurement of the mitochondrial activities in cultured cells. T.I.M., S.V.S., G.U., M.B., R.S., I.K.-M., J.A.M.S., R.V.C. and M.S.v.d.K. all contributed key patients to the study. J.A.M.S. measured mitochondrial activities on a muscle biopsy of the first patient. J.C.P. contributed to the analysis of the genome-wide scan. M.S.v.d.K. originally described the disease, selected the patients on the basis of MRI criteria and supervised the study. G.C.S. and M.S.v.d.K. designed the study and wrote the paper with contributions from many of the other coauthors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Fig. 1
Conservation of altered amino acids in mtAspRS. (PDF 22 kb)
Supplementary Fig. 2
Splicing variants of exon 3. (PDF 49 kb)
Supplementary Fig. 3
Expression of COXI in fibroblasts. (PDF 22 kb)
Supplementary Table 1
MRI criteria for LBSL. (PDF 7 kb)
Supplementary Table 2
Activities of the repiratory chain complexes. (PDF 8 kb)
Supplementary Table 3
mtAspRS mRNA expression. (PDF 17 kb)
Supplementary Table 4
Primers. (PDF 22 kb)
Rights and permissions
About this article
Cite this article
Scheper, G., van der Klok, T., van Andel, R. et al. Mitochondrial aspartyl-tRNA synthetase deficiency causes leukoencephalopathy with brain stem and spinal cord involvement and lactate elevation. Nat Genet 39, 534–539 (2007). https://doi.org/10.1038/ng2013
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ng2013
This article is cited by
-
DARS2 overexpression is associated with PET/CT metabolic parameters and affects glycolytic activity in lung adenocarcinoma
Journal of Translational Medicine (2023)
-
Mutations in DARS2 result in global dysregulation of mRNA metabolism and splicing
Scientific Reports (2023)
-
Role of Mutations of Mitochondrial Aminoacyl-tRNA Synthetases Genes on Epileptogenesis
Molecular Neurobiology (2023)
-
Neuropathy-associated Fars2 deficiency affects neuronal development and potentiates neuronal apoptosis by impairing mitochondrial function
Cell & Bioscience (2022)
-
Deep learning modeling m6A deposition reveals the importance of downstream cis-element sequences
Nature Communications (2022)