Abstract
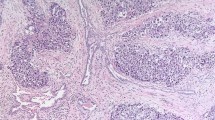
There are considerable geographic, ethnic and temporal variations in the global incidence of testicular cancer. The disease mainly affects Western populations, with average rates in developed areas of the world six times higher than those in developing areas. About 500,000 new cases were diagnosed worldwide in 2002, with the vast majority being germ cell tumors and occurring in young adult males. Traditionally, these tumors are further classified into seminoma and nonseminoma. In this Review, trends in the incidence of germ cell tumors are examined using high-quality cancer-registry data from 41 populations within 14 countries worldwide. To assess whether trends of seminoma and nonseminoma incidence are similar, data were analyzed by birth cohort. These analyses should reveal similar trends if the 10-year difference in the clinical manifestation of cancer between subtypes is caused by differences in the speed of progression from the same early rate-limiting step to the onset of symptomatic disease. In each country, incidence has uniformly increased in successive generations born from around 1920 until very recently. Cohort-specific trends in seminoma incidence are similar to cohort-specific trends in nonseminoma incidence, lending support to the conclusion that the subtypes are epidemiologically and etiologically comparable. The findings presented are related to current theories and evidence regarding the determinants of testicular germ cell cancer.
Key Points
-
A 10-year difference in the clinical manifestation of seminoma and nonseminoma is likely to be the result of disparities in the speed of progression from the same early rate-limiting step to the onset of symptomatic disease
-
With a few notable exceptions, there have been global increases in the incidence of testicular germ cell cancer in successive generations of men born from around 1920 until around the 1960s.
-
The trends in seminoma and nonseminoma incidence by birth cohort are similar, supporting the inference that seminoma and nonseminoma are epidemiologically and aetiologically similar
-
Future studies should focus on generating and testing specific hypotheses that might find the major determinant(s) of testicular cancer
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Moller H and Evans H (2003) Epidemiology of gonadal germ cell cancer in males and females. APMIS 111: 43–46
Looijenga LH and Oosterhuis JW (2002) Pathobiology of testicular germ cell tumors: views and news. Anal Quant Cytol Histol 24: 263–279
Moller H et al. (1993) Survival of Danish cancer patients 1943–1987. Male genital organs. APMIS Suppl 33: 122–136
Schmoll HJ et al. (2004) European consensus on diagnosis and treatment of germ cell cancer: a report of the European Germ Cell Cancer Consensus Group (EGCCCG). Ann Oncol 15: 1377–1399
Moller H (1993) Clues to the aetiology of testicular germ cell tumours from descriptive epidemiology. Eur Urol 23: 8–13
Skakkebaek NE et al. (1987) Carcinoma-in-situ of the testis: possible origin from gonocytes and precursor of all types of germ cell tumours except spermatocytoma. Int J Androl 10: 19–28
Rorth M et al. (2000) Carcinoma in situ in the testis. Scand J Urol Nephrol Suppl 205: 166–186
Dieckmann KP and Pichlmeier U (2004) Clinical epidemiology of testicular germ cell tumors. World J Urol 22: 2–14
Giwercman A et al. (1989) Prevalence of carcinoma in situ and other histopathological abnormalities in testes of men with a history of cryptorchidism. J Urol 142: 998–1001
Giwercman A et al. (1991) Prevalence of carcinoma in situ and other histopathological abnormalities in testes from 399 men who died suddenly and unexpectedly. J Urol 145: 77–80
Dieckmann KP and Loy V (1998) The value of the biopsy of the contralateral testis in patients with testicular germ cell cancer: the recent German experience. APMIS 106: 13–20
Linke J et al. (2005) Prevalence of testicular intraepithelial neoplasia in healthy males. J Urol 173: 1577–1579
Parkin DM et al. (2002) Cancer Incidence in Five Continents Vol VIII. Lyon: IARC Press
Huyghe E et al. (2003) Increasing incidence of testicular cancer worldwide: a review. J Urol 170: 5–11
Moller H (1989) Decreased testicular cancer risk in men born in wartime. J Natl Cancer Inst 81: 1668–1669
Wanderas EH et al. (1995) Trends in incidence of testicular cancer in Norway 1955–1992. Eur J Cancer 31A: 2044–2048
Bergstrom R et al. (1996) Increase in testicular cancer incidence in six European countries: a birth cohort phenomenon. J Natl Cancer Inst 88: 727–733
Richiardi L et al. (2004) Testicular cancer incidence in eight northern European countries: secular and recent trends. Cancer Epidemiol Biomarkers Prev 13: 2157–2166
Moller H (2001) Trends in incidence of testicular cancer and prostate cancer in Denmark. Hum Reprod 16: 1007–1011
Hemminki K and Li X (2004) Familial risk in testicular cancer as a clue to a heritable and environmental aetiology. Br J Cancer 90: 1765–1770
Hemminki K and Li X (2002) Cancer risks in Nordic immigrants and their offspring in Sweden. Eur J Cancer 38: 2428–2434
Ekbom A et al. (2003) Age at immigration and duration of stay in relation to risk for testicular cancer among Finnish immigrants in Sweden. J Natl Cancer Inst 95: 1238–1240
Holford TR (1998) Age-period cohort analysis. In Encyclopedia of Biostatistics, 82–99 (Ed Armitage P and Colton T) Chichester: John Wiley & Sons
Levi F et al. (2003) Trends in testicular cancer incidence in Vaud, Switzerland. Eur J Cancer Prev 12: 347–349
Purdue MP et al. (2005) International patterns and trends in testis cancer incidence. Int J Cancer 115: 822–827
Henderson BE et al. (1979) Risk factors for cancer of the testis in young men. Int J Cancer 23: 598–602
Ross RK et al. (1979) Descriptive epidemiology of testicular and prostatic cancer in Los Angeles. Br J Cancer 39: 284–292
Garner MJ et al. (2005) Epidemiology of testicular cancer: an overview. Int J Cancer 116: 331–339
Akre O et al. (1996) Testicular nonseminoma and seminoma in relation to perinatal characteristics. J Natl Cancer Inst 88: 883–889
Wanderas EH et al. (1998) Maternal health and pre- and perinatal characteristics in the etiology of testicular cancer: a prospective population- and register-based study on Norwegian males born between 1967 and 1995. Cancer Causes Control 9: 475–486
Sabroe S and Olsen J (1998) Perinatal correlates of specific histological types of testicular cancer in patients below 35 years of age: a case-cohort study based on midwives' records in Denmark. Int J Cancer 78: 140–143
Richiardi L et al. (2002) Perinatal determinants of germ-cell testicular cancer in relation to histological subtypes. Br J Cancer 87: 545–550
Moller H and Skakkebaek NE (1999) Risk of testicular cancer in subfertile men: case-control study. BMJ 318: 559–562
Jacobsen R et al. (2000) Risk of testicular cancer in men with abnormal semen characteristics: cohort study. BMJ 321: 789–792
Skakkebaek NE et al. (1998) Germ cell cancer and disorders of spermatogenesis: an environmental connection? APMIS 106: 3–11
Skakkebaek NE et al. (2001) Testicular dysgenesis syndrome: an increasingly common developmental disorder with environmental aspects. Hum Reprod 16: 972–978
Henderson BE et al. (1982) Endogenous hormones as a major factor in human cancer. Cancer Res 42: 3232–3239
Depue RH et al. (1983) Estrogen exposure during gestation and risk of testicular cancer. J Natl Cancer Inst 71: 1151–1155
Sharpe RM and Skakkebaek NE (1993) Are oestrogens involved in falling sperm counts and disorders of the male reproductive tract? Lancet 341: 1392–1395
Aitken RJ et al. (2004) Seeds of concern. Nature 432: 48–52
Schwartz GG (2002) Hypothesis: does ochratoxin A cause testicular cancer? Cancer Causes Control 13: 91–100
Hardell L et al. (2003) Increased concentrations of polychlorinated biphenyls, hexachlorobenzene, and chlordanes in mothers of men with testicular cancer. Environ Health Perspect 111: 930–934
Hardell L et al. (2004) Concentrations of polychlorinated biphenyls in blood and the risk for testicular cancer. Int J Androl 27: 282–290
Surveillance Epidemiology and End Results (SEER) Program (2004) SEER*Stat Database: Incidence—SEER 9 Regs Public-Use (1973–2001). National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch, Bethedsa
Steinitz R et al. (1989) Cancer Incidence in Jewish Migrants to Israel 1961–1981. Lyon: IARC
European Network of Cancer Registries (2001) EUROCIM Version 4.0: European incidence database V2.4, CI5 dictionary. Lyon: IARC
Percy C et al. (1990) International Classification of Diseases for Oncology, edn 2. Geneva: World Health Organization
Parkin DM et al. (1992) Cancer Incidence in Five Continents Vol VI. Lyon: IARC Press
Parkin DM et al. (1997) Cancer Incidence in Five Continents Vol VII. Lyon: IARC Press
Parkin DM et al. (1998) Histological Groups for Comparative Studies. Lyon: IARC
Doll R and Cook P (1967) Summarizing indices for comparison of cancer incidence data. Int J Cancer 2: 269–279
Segi M and Kurihara M (1960) Cancer Mortality for Selected Sites in 24 Countries (1950–1957). Sendai, Japan: Tohoku University of Medicine
Acknowledgements
The analyses and the interpretation of these trends would not be possible were it not for the dedicated work of cancer registries worldwide in providing the high quality data compiled in successive volumes of “Cancer Incidence in Five Continents” for such purposes.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Bray, F., Ferlay, J., Devesa, S. et al. Interpreting the international trends in testicular seminoma and nonseminoma incidence. Nat Rev Urol 3, 532–543 (2006). https://doi.org/10.1038/ncpuro0606
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpuro0606
This article is cited by
-
PDE11A gene polymorphism in testicular cancer: sperm parameters and hormonal profile
Journal of Endocrinological Investigation (2021)
-
Racial differences in testicular cancer in the United States: descriptive epidemiology
BMC Cancer (2020)
-
Testicular cancer in Hispanics: incidence of subtypes over time according to neighborhood sociodemographic factors in California
Cancer Causes & Control (2020)
-
Genomic landscape of platinum resistant and sensitive testicular cancers
Nature Communications (2020)
-
The genomic landscape of testicular germ cell tumours: from susceptibility to treatment
Nature Reviews Urology (2016)