Abstract
Cognitive behavioral therapy (CBT) techniques offer short-term, goal-oriented psychotherapy. In this respect, it differs from classical psychoanalysis in emphasizing changes in thought patterns and behaviors rather than providing 'deep insight'. Importantly, the beneficial effects of CBT can be achieved in 10–20 sessions, compared with the many years required for classical psychoanalysis. Although CBT is often done on a one-to-one basis, it also lends itself to a group therapeutic setting. CBT was initially used in the treatment of mood disorders, but its use has subsequently been expanded to include various other medical conditions, including chronic pain states. Over the past 18 years, several chronic pain treatment programs have used CBT techniques in the management of fibromyalgia. In this review, the results from 13 programs using CBT, alone or in combination with other treatment modalities, are analyzed. In most studies, CBT provided worthwhile improvements in pain-related behavior, self-efficacy, coping strategies and overall physical function. Sustained improvements in pain were most evident when individualized CBT was used to treat patients with juvenile fibromyalgia. The current data indicate that CBT, as a single treatment modality, does not offer any distinct advantage over well-planned group programs of education or exercise, or both. Its role in the management of fibromyalgia patients needs further research.
Key Points
-
Cognitive behavioral therapy (CBT) has a long track record in the treatment of mood disorders
-
CBT also has a role in the treatment of a variety of chronic medical conditions, including chronic pain syndromes
-
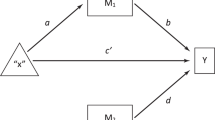
The rationale for use of CBT in the management of patients with fibromyalgia is based, in part, on the physiological links between chronic pain and depression
-
In general, CBT does not seem to provide sustained pain relief in fibromyalgia patients
-
The published literature indicates that the primary utility of CBT in the management of patients with fibromyalgia lies in improving aspects of the syndrome other than pain, including self-efficacy, dysfunctional thought patterns and physical function
-
Current evidence suggests that CBT should be considered as an adjunctive therapy in the management of fibromyalgia patients, particularly those who present with an emotionally distressed and/or dysfunctional profile, although CBT could also be useful for other patient subgroups
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Redd WH (2004) Commentary: the evolution of evidence-based psychotherapy. J Clin Psychol 60: 443–446
Ellis A (1955) New approaches to psychotherapy techniques. J Clin Psychol 11: 207–260
Beck AT (1964) Thinking and depression. I. Theory and therapy. Arch Gen Psychiatry 10: 561–571
Mahoney MJ (1974) Cognition and Behavior Modification. Cambridge, MA: Ballinger
Meichenbaum D (1977) Cognitive-behavior modification: an integrative approach. New York: Plenum
Melzack R and Wall PD (1965) Pain mechanisms: a new theory. Science 150: 971–979
Thieme K et al. (2005) Predictors of pain behaviors in fibromyalgia syndrome. Arthritis Rheum 53: 343–350
Boissevain MD and McCain GA (1991) Toward an integrated understanding of fibromyalgia syndrome. II. Psychological and phenomenological aspects. Pain 45: 239–248
Bradley LA and Alberts KR (1999) Psychological and behavioral approaches to pain management for patients with rheumatic disease. Rheum Dis Clin North Am 25: 215–232
Keefe FJ et al. (2005) Psychological approaches to understanding and treating disease-related pain. Annu Rev Psychol 56: 601–630
Staud R (2002) Evidence of involvement of central neural mechanisms in generating fibromyalgia pain. Curr Rheumatol Rep 4: 299–305
Gracely RH et al. (2002) Functional magnetic resonance imaging evidence of augmented pain processing in fibromyalgia. Arthritis Rheum 46: 1333–1343
Dubner R and Gold M (1999) The neurobiology of pain. Proc Natl Acad Sci USA 96: 7627–7630
Fields HL and Basbaum AI (1994) Central nervous system mechanisms of pain modulation. In Textbook of Pain, edn 4 243–257 (eds Wall PD and Melzack R) Edinburgh: Churchill and Livingstone
Kwiat GC and Basbaum AI (1992) The origin of brainstem noradrenergic and serotonergic projections to the spinal cord dorsal horn in the rat. Somatosens Mot Res 9: 157–173
Basbaum AI and Fields HL (1984) Endogenous pain control systems: brainstem spinal pathways and endorphin circuitry. Annu Rev Neurosci 7: 309–338
Arnold LM et al. (2004) A double-blind, multicenter trial comparing duloxetine with placebo in the treatment of fibromyalgia patients with or without major depressive disorder. Arthritis Rheum 50: 2974–2984
Vitton O et al. (2004) A double-blind placebo-controlled trial of milnacipran in the treatment of fibromyalgia. Hum Psychopharmacol 19 (Suppl 1): S27–S35
Stahl S and Briley M (2004) Understanding pain in depression. Hum Psychopharmacol 19 (Suppl 1): S9–S13
Casey KL (1999) Forebrain mechanisms of nociception and pain: analysis through imaging. Proc Natl Acad Sci USA 96: 7668–7674
Turk DC et al. (1983) Pain and Behavioral Medicine: A Cognitive-Behavioral Perspective. New York: Guilford
Fordyce WE et al. (1985) The behavioral management of chronic pain: a response to critics. Pain 22: 113–125
Weisenberg M (1998) Cognitive aspects of pain and pain control. Int J Clin Exp Hypn 46: 44–61
Vlaeyen JW et al. (2002) Can pain-related fear be reduced? The application of cognitive-behavioural exposure in vivo. Pain Res Manag 7: 144–153
Parker JC et al. (1988) Pain management in rheumatoid arthritis patients. A cognitive-behavioral approach. Arthritis Rheum 31: 593–601
Goldenberg DL et al. (2004) Management of fibromyalgia syndrome. JAMA 292: 2388–2395
Bennett RM (2002) The rational management of fibromyalgia patients. Rheum Dis Clin.North Am 28: 181–199
Mannerkorpi K (2005) Exercise in fibromyalgia. Curr Opin Rheumatol 17: 190–194
Jones KD and Clark SR (2002) Individualizing the exercise prescription for persons with fibromyalgia. Rheum Dis Clin North Am 28: 419–424
Nielson WR et al. (1992) Cognitive behavioral treatment of fibromyalgia syndrome: preliminary findings. J Rheumatol 19: 98–103
White KP and Nielson WR (1995) Cognitive behavioral treatment of fibromyalgia syndrome: a followup assessment. J Rheumatol 22: 717–721
Walco GA and Ilowite NT (1992) Cognitive-behavioral intervention for juvenile primary fibromyalgia syndrome. J Rheumatol 19: 1617–1619
Varni JW et al. (1987) The Varni/Thompson Pediatric Pain Questionnaire. I. Chronic musculoskeletal pain in juvenile rheumatoid arthritis. Pain 28: 27–38
Turk DC et al. (1998) Interdisciplinary treatment for fibromyalgia syndrome: clinical and statistical significance. Arthritis Care Res 11: 186–195
Kerns RD et al. (1985) The West Haven–Yale Multidimensional Pain Inventory (WHYMPI). Pain 23: 345–346
Creamer P et al. (2000) Sustained improvement produced by nonpharmacologic intervention in fibromyalgia: results of a pilot study. Arthritis Care Res 13: 198–204
Burckhardt CS et al. (1991) The fibromyalgia impact questionnaire (FIQ): development and validation. J Rheumatol 18: 728–733
Beck AT et al. (1961) An inventory for measuring depression. Arch Gen Psychiatry 4: 561–571
Ziebland S et al. (1992) Comparison of two approaches to measuring change in health status in rheumatoid arthritis: the Health Assessment Questionnaire (HAQ) and modified HAQ. Ann Rheum Dis 51: 1202–1205
Hassett AL et al. (2000) The role of catastrophizing in the pain and depression of women with fibromyalgia syndrome. Arthritis Rheum 43: 2493–2500
Wolfe F et al. (1990) The American College of Rheumatology 1990 criteria for the classification of fibromyalgia: report of the Multicenter Criteria Committee. Arthritis Rheum 33: 160–172
Degotardi PJ et al. (2005) Development and evaluation of a cognitive-behavioral intervention for juvenile fibromyalgia. J Pediatr Psychol [doi:10.1093/jpepsy/jsj064]
Lemstra M and Olszynski WP (2005) The effectiveness of multidisciplinary rehabilitation in the treatment of fibromyalgia: a randomized controlled trial. Clin J Pain 21: 166–174
Burckhardt CS et al. (1994) A randomized, controlled clinical trial of education and physical training for women with fibromyalgia. J Rheumatol 21: 714–720
Callahan LF et al. (1988) Further analysis of learned helplessness in rheumatoid arthritis using a “rheumatology attitudes index”. J Rheumatol 15: 418–426
Lorig K et al. (1989) Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis Rheum 32: 37–44
Vlaeyen JW et al. (1996) Cognitive-educational treatment of fibromyalgia: a randomized clinical trial. I. Clinical effects. J Rheumatol 23: 1237–1245
Bennett RM et al. (1996) Group treatment of fibromyalgia: a 6 month outpatient program. J Rheumatol 23: 521–528
Nicassio PM et al. (1997) A comparison of behavioral and educational interventions for fibromyalgia. J Rheumatol 24: 2000–2007
Williams DA et al. (2002) Improving physical functional status in patients with fibromyalgia: a brief cognitive behavioral intervention. J Rheumatol 29: 1280–1286
Ware JR and Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30: 473–483
Melzack R (1975) The McGill Pain Questionnaire: major properties and scoring methods. Pain 1: 277–299
Redondo JR et al. (2004) Long-term efficacy of therapy in patients with fibromyalgia: a physical exercise-based program and a cognitive-behavioral approach. Arthritis Rheum 51: 184–192
Kashikar-Zuck S et al. (2005) Efficacy of cognitive-behavioral intervention for juvenile primary fibromyalgia syndrome. J Rheumatol 32: 1594–1602
Siegel DM et al. (1998) Fibromyalgia syndrome in children and adolescents: clinical features at presentation and status at follow-up. Pediatrics 101: 377–382
Gedalia A et al. (2000) Fibromyalgia syndrome: experience in a pediatric rheumatology clinic. Clin Exp Rheumatol 18: 415–419
Dobkin PL et al. (2005) Maintenance of exercise in women with fibromyalgia. Arthritis Rheum 53: 724–731
Turk DC et al. (2002) Psychological evaluation of patients diagnosed with fibromyalgia syndrome: a comprehensive approach. Rheum Dis Clin North Am 28: 219–233
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Bennett, R., Nelson, D. Cognitive behavioral therapy for fibromyalgia. Nat Rev Rheumatol 2, 416–424 (2006). https://doi.org/10.1038/ncprheum0245
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncprheum0245
This article is cited by
-
A web-based educational therapy intervention associated with physical exercise to promote health in fibromyalgia in Brazil: the Amigos De Fibro (Fibro Friends) study protocol
Trials (2023)
-
Digital self-management interventions for osteoarthritis: a systematic scoping review of intervention characteristics, adherence and attrition
Archives of Public Health (2022)
-
Differential Brain Perfusion Changes Following Two Mind–Body Interventions for Fibromyalgia Patients: an Arterial Spin Labelling fMRI Study
Mindfulness (2022)
-
Juvenile primary fibromyalgia syndrome: A Review- Treatment and Prognosis
Pediatric Rheumatology (2021)
-
Attachment-Based Compassion Therapy for Ameliorating Fibromyalgia: Mediating Role of Mindfulness and Self-Compassion
Mindfulness (2020)