Abstract
Background Long-term success in ventricular assist device (VAD) recipients is limited by thromboembolic events, the prediction of which remains elusive. We evaluated the predictive value of aspirin hyporesponsiveness and markers of coagulation and fibrinolysis.
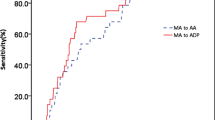
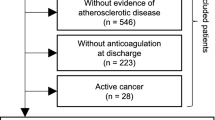
Methods We prospectively enrolled patients scheduled to undergo VAD implantation between June 2004 and March 2006. Once before surgery, daily during hospitalization, and weekly after discharge we assessed platelet function, measured prothrombin activation fragment 1.2 (F1.2) and plasminogen activator inhibitor-1 (PAI-1) concentrations, and evaluated aspirin hyporesponsiveness by whole-blood aggregometry and thromboelastography. All patients received 325 mg oral aspirin daily from at least 7 days before VAD implantation. Follow-up continued until heart transplantation, death or closure of the database.
Results We included 26 patients (median follow-up 315 days, range 9–833 days). In eight (31%) patients, 14 thromboembolic events occurred at a median of 42 (interquartile range 26–131) days. Only six (43%) events based on whole-blood aggregometry and one (7%) based on thromboelastography coincided with aspirin hyporesponsiveness. Within-patient variability was high for both tests (59% and 567%, respectively). Compared with levels before surgery, PAI-1 concentrations were raised for up to 45 days (P <0.0001) and those of F1.2 for up to 3 days (P = 0.0001) after VAD implantation. PAI-1 and F1.2 levels did not rise significantly further before thromboembolic events.
Conclusions Aspirin hyporesponsiveness was not associated with raised risk of future clinical thromboembolic events after VAD implantation. Impaired fibrinolysis, demonstrated by raised PAI-1 concentrations, might, however, indicate a predisposition to such events early after surgery.
Key Points
-
Biological aspirin hyporesponsiveness is common in patients with end-stage systolic heart failure before and after implantation of ventricular assist devices
-
Thromboembolic events occur at a high rate—nearly one-third—in patients with ventricular assist devices
-
No significant association was observed between the presence of aspirin hyporesponsiveness, based on whole-blood aggregometry and thromboelastography assays, and thromboembolic events in patients with ventricular assist devices
-
Plasminogen activator inhibitor-1 values early after ventricular assist device implantation suggest impaired fibrinolysis predisposes patients to thromboembolic events
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Rose EA et al.; Randomized Evaluation of Mechanical Assistance for the Treatment of Congestive Heart Failure (REMATCH) Study Group (2001) Long-term mechanical left ventricular assistance for end-stage heart failure. N Engl J Med 345: 1435–1443
Deng MC et al.; International Society for Heart and Lung Transplantation (2005) Mechanical circulatory support device database of the International Society for Heart and Lung Transplantation: third annual report—2005. J Heart Lung Transplant 24: 1182–1187
Tsukui H et al. (2007) Cerebrovascular accidents in patients with a ventricular assist device. J Thorac Cardiovasc Surg 134:114–123
Houel R et al. (2003) Resistance to aspirin after external ventricular assist device implantation. J Thorac Cardiovasc Surg 126: 1636–1637
Michelson AD (2004) Platelet function testing in cardiovascular diseases. Circulation 110: e489–e493
Cotter G et al. (2004) Lack of aspirin effect: aspirin resistance or resistance to taking aspirin? Am Heart J 147: 293–300
Catella-Lawson F et al. (2001) Cyclooxygenase inhibitors and the antiplatelet effects of aspirin. N Engl J Med 345: 1809–1817
Kurth T et al. (2003) Inhibition of clinical benefits of aspirin on first myocardial infarction by nonsteroidal antiinflammatory drugs. Circulation 108: 1191–1195
Hung J et al. (1995) Cigarette smoking acutely increases platelet thrombus formation in patients with coronary artery disease taking aspirin. Circulation 92: 2432–2436
Cipollone F et al. (2004) Cyclooxygenase-2 expression and inhibition in atherothrombosis. Arterioscler Thromb Vasc Biol 24: 246–255
Undas A et al. (2001) PlA2 polymorphism of β3 integrins is associated with enhanced thrombin generation and impaired antithrombotic action of aspirin at the site of microvascular injury. Circulation 104: 2666–2672
Michelson AD et al. (2000) Platelet GP IIIa PlA polymorphisms display different sensitivities to agonists. Circulation 101: 1013–1018
Larsson PT et al. (1994) Norepinephrine-induced human platelet activation in vivo is only partly counteracted by aspirin. Circulation 89: 1951–1957
Kawasaki T et al. (2000) Increased platelet sensitivity to collagen in individuals resistant to low-dose aspirin. Stroke 31: 591–595
Marshall PW et al. (1997) A comparison of the effects of aspirin on bleeding time measured using the Simplate™ method and closure time measured using the PFA-100™, in healthy volunteers. Br J Clin Pharmacol 44: 151–155
Mueller MR et al. (1997) Variable platelet response to low-dose ASA and the risk of limb deterioration in patients submitted to peripheral arterial angioplasty. Thromb Haemost 78: 1003–1007
Grundmann K et al. (2003) Aspirin non-responder status in patients with recurrent cerebral ischemic attacks. J Neurol 250: 63–66
Gum PA et al. (2001) Profile and prevalence of aspirin resistance in patients with cardiovascular disease. Am J Cardiol 88: 230–235
Zimmermann N et al. (2003) Functional and biochemical evaluation of platelet aspirin resistance after coronary artery bypass surgery. Circulation 108: 542–547
Eikelboom JW et al. (2002) Aspirin-resistant thromboxane biosynthesis and the risk of myocardial infarction, stroke, or cardiovascular death in patients at high risk for cardiovascular events. Circulation 105: 1650–1655
Sane DC et al. (2002) Frequency of aspirin resistance in patients with congestive heart failure treated with antecedent aspirin. Am J Cardiol 90: 893–895
Houël R et al. (2004) Platelet activation and aggregation profile in prolonged external ventricular support. J Thorac Cardiovasc Surg 128: 197–202
Dyszkiewicz-Korpanty AM et al. (2005) Approach to the assessment of platelet function: comparison between optical-based platelet-rich plasma and impedance-based whole blood platelet aggregation methods. Clin Appl Thromb Hemost 11: 25–35
Ivandic BT et al. (2007) Determination of aspirin responsiveness by use of whole blood platelet aggregometry. Clin Chem 53: 614–619
Poston RS et al. (2006) Aprotinin shows both hemostatic and antithrombotic effects during off-pump coronary artery bypass grafting. Ann Thorac Surg 81: 104–110
Aggrolink software version 5.2.1 (Chrono-Log Corp, Haverton, PA)
Luddington RJ (2005) Thrombelastography/thromboelastometry. Clin Lab Haematol 27: 81–90
Bochsen L et al. (2007) Evaluation of the TEG platelet mapping assay in blood donors. Thromb J 5: 3
Feinberg WM et al. (1999) Markers of thrombin and platelet activity in patients with atrial fibrillation: correlation with stroke among 1531 participants in the stroke prevention in atrial fibrillation III study. Stroke 30: 2547–2553
Johansson L et al. (2000) Tissue plasminogen activator, plasminogen activator inhibitor-1, and tissue plasminogen activator/plasminogen activator inhibitor-1 complex as risk factors for the development of a first stroke. Stroke 31: 26–32
Haude M et al. (1995) Guidance of anticoagulation after intracoronary implantation of Palmaz-Schatz stents by monitoring prothrombin and prothrombin fragment 1 + 2. Am Heart J 130: 228–238
Lazar RM et al. (2004) Neurological events during long-term mechanical circulatory support for heart failure: the Randomized Evaluation of Mechanical Assistance for the Treatment of Congestive Heart Failure (REMATCH) experience. Circulation 109: 2423–2427
Thygesen K et al.; Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction (2007) Universal definition of myocardial infarction. J Am Coll Cardiol 50: 2173–2195
Beppu S et al. (1992) High incidence of left ventricular thrombosis and systemic embolism in patients with left ventricular assist system [Japanese]. J Cardiol 22: 713–720
Fries D et al. (2003) Coagulation monitoring and management of anticoagulation during cardiac assist device support. Ann Thorac Surg 76: 1593–1597
Spanier T et al. (1996) Activation of coagulation and fibrinolytic pathways in patients with left ventricular assist devices. J Thorac Cardiovasc Surg 112: 1090–1097
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
F Majeed, WJ Kop, RS Poston and S Kallam declared no competing interests.
MR Mehra has served as a consultant to Ventracor and Thoratec with regard to their mechanical circulatory assist devices.
Rights and permissions
About this article
Cite this article
Majeed, F., Kop, W., Poston, R. et al. Prospective, observational study of antiplatelet and coagulation biomarkers as predictors of thromboembolic events after implantation of ventricular assist devices. Nat Rev Cardiol 6, 147–157 (2009). https://doi.org/10.1038/ncpcardio1441
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpcardio1441
This article is cited by
-
Comparative efficacy of in vitro and in vivo metabolized aspirin in the DeBakey ventricular assist device
Journal of Thrombosis and Thrombolysis (2014)