Abstract
Voltage-gated Kv1.3 and Ca2+-dependent KCa3.1 are the most prevalent K+ channels expressed by human and rat T cells. Despite the preferential upregulation of Kv1.3 over KCa3.1 on autoantigen-experienced effector memory T cells, whether Kv1.3 is required for their induction and function is unclear. Here we show, using Kv1.3-deficient rats, that Kv1.3 is involved in the development of chronically activated antigen-specific T cells. Several immune responses are normal in Kv1.3 knockout (KO) rats, suggesting that KCa3.1 can compensate for the absence of Kv1.3 under these specific settings. However, experiments with Kv1.3 KO rats and Kv1.3 siRNA knockdown or channel-specific inhibition of human T cells show that maximal T-cell responses against autoantigen or repeated tetanus toxoid stimulations require both Kv1.3 and KCa3.1. Finally, our data also suggest that T-cell dependency on Kv1.3 or KCa3.1 might be irreversibly modulated by antigen exposure.
Similar content being viewed by others
Introduction
A hallmark of the adaptive immune system is the generation of long-lived, self-renewing memory T cells in response to pathogen-derived antigenic stimuli. Electrophysiology studies have implicated the potassium ion (K+) channel Kv1.3 as having a critical role in the regulation of chronically activated effector memory T (TEM) cell immune responses. K+ channels are tetrameric membrane proteins that selectively conduct K+ across cellular membranes. Out of the 80 distinct K+ channel genes that have been identified in the human genome, only two are dominantly expressed on human T cells; these are the homotetramers of the Shaker-related voltage-gated Kv1.3 (Kcna3) and the Ca2+-dependent KCa3.1 K+ channels (Kcnn4)1. These channels provide the K+ efflux necessary to counter-balance the Ca2+ influx crucial for T-cell activation1,2,3,4.
Functional expression of Kv1.3 and KCa3.1 on T-cell subsets has been extensively characterized using single-cell patch-clamp technique under channel-specific conditions1,5,6,7,8,9. At rest, T cells express low levels of both K+ channels, and both are upregulated upon antigen-specific or mitogen-specific activation. However, chronically activated TEM cells and autoreactive T cells have been reported to preferentially express Kv1.3. The differential expression of these ion channels results in different sensitivity of naive versus autoreactive memory T cells to selective blockers of Kv1.3 and KCa3.1, such as peptide toxin ShK and its derivatives10,11,12,13,14,15,16 and pharmacological inhibitor TRAM-34 (refs 17, 18), respectively.
As single-cell patch clamp revealed that autoreactive TEM cells predominantly utilize Kv1.3, Kv1.3 inhibitors have been evaluated for suppression of autoimmune reactions. Inhibition of Kv1.3 with ShK or its derivatives has shown partial efficacy in preclinical autoimmune disease rat models including experimental autoimmune encephalomyelitis15,19,20, pristane-induced arthritis15, and experimental autoimmune diabetes15, as well as in T-cell-dependent models of delayed-type hypersensitivity (DTH)15,21, allergic contact dermatitis22,23 and asthma24. Despite the ability of Kv1.3 inhibitors to impede preclinical models of autoimmune disease, it is not clear whether inhibition of Kv1.3 is sufficient to fully inhibit pathological T-cell activation and effector function. In the context of single cells, channel blockers abrogate Kv1.3 channel function in patch-clamp experiments. However, only partial inhibition of in vitro T-cell responses has been detected using functional readouts, such as proliferation or cytokine production12,13,14,15,16,20,25,26. This observation raises the possibility that ion channels other than Kv1.3, such as KCa3.1, may have functional activity.
Mouse T cells, unlike rat or human T cells, co-express additional Kv1 channel family members, including Kv1.1, Kv1.4 and Kv1.6 (ref. 27), rendering Kv1.3 redundant, and thereby precludes the translation of mouse T-cell function to humans7. Conversely, selective K+ channel expression in rat T cells phenocopies human T cells7. Thus, in order to characterize the role of Kv1.3 in T-cell responses, we generated a Kcna3 knockout (KO) rat. Characterization of functional responses in Kcna3−/− rats compared with wild-type (WT) rats, together with the use of channel-specific blockers and in vitro antigen recall assays, enables us to assess the individual contributions of Kv1.3 and KCa3.1, providing a more comprehensive analysis of the role of these K+ channels in T-cell function than enabled by electrophysiology methods. These approaches reveal that inhibition of Kv1.3 alone is insufficient to inhibit functional T-cell responses and, moreover, that KCa3.1 compensates for the loss of Kv1.3 in Kcna3−/− rats. Our rat data are translatable to human T cells, as differential utilization of Kv1.3 or KCa3.1 is detected in pathogen-specific T cells as compared with autoreactive T cells, with skewing towards Kv1.3 dependency resulting from repeated antigen stimulation. Collectively, our study demonstrates that repeated exposure to specific antigen might affect whether Kv1.3 or KCa3.1 functionally predominates, and that Kv1.3 and KCa3.1 have complementary and compensatory roles, thereby providing redundant mechanisms to ensure T-cell activation.
Results
KCNA3−/− rat T cells are functionally competent
Mice are not suitable for exploring the role of Kv1.3 and KCa3.1 in T-cell responses due to the expression and redundancy of many Kv1 channel family members in the immune compartment7,27,28. Rats, however, are phenotypically similar to humans in terms of Kv1.3 being the only Kv1 member expressed by T cells (Fig. 1a). Therefore, we generated a rat deficient of Kv1.3 (Kcna3−/−) using zinc finger nuclease targeted deletion on Dark Agouti rats (Supplementary Fig. 1a–c) to ask whether Kv1.3 was required for functional T-cell responses. Kcna3−/− rats appeared phenotypically normal and displayed no gross abnormalities. Analysis of K+ channel mRNA expression confirmed that the Kcna3−/− rat CD4+ and CD8+ T cells did not express Kcna3 transcripts, nor did they express other Kv1 family genes; only KCa3.1 transcripts (Kcnn4) were detectable (Supplementary Fig. 1d). Absence of Kv1.3 protein was validated by flow cytometry (Supplementary Fig. 1e). Electrophysiology provided functional confirmation that Kv1.3 was deleted, as Kv1.3-dependent currents were undetectable (Fig. 1b–d). Detailed characterization of the immune compartment revealed no differences in T- or B-cell populations in Kcna3−/− versus WT rats (Supplementary Fig. 2). Polyclonal activation of splenic T cells with anti-CD3 and anti-CD28 in vitro revealed no differences between Kcna3−/− and WT rat T cells using proliferation and effector cytokine production as functional readouts (Fig. 1e). Consistent with published findings for human T cells, the KCa3.1-specific small molecule inhibitor TRAM-34 inhibited naive WT rat T-cell proliferation in response to polyclonal activation, whereas this response was unaffected by the Kv1.3-specific small molecule inhibitor ShK; IFN-γ production was similarly inhibited by TRAM-34 but not ShK (Fig. 1f). As expected, ShK had no effect on Kcna3−/− T-cell responses; inhibition with TRAM-34 was slightly enhanced in Kcna3−/− as compared with WT.
(a) K+-channel expression in human, rat and mouse T cells. Gene expression of Kv1 family members and KCa3.1 in naive CD4+ T cells from human (left), rat (centre) or mouse (right). Relative expression was determined by normalizing to housekeeping gene RPL19. Electrophysiological and pharmacological tests show null Kv1.3 channel in Kcna3−/− T cells. (b) Representative voltage-currents from WT and Kcna3−/− T cells. Currents were elicited by depolarizing voltage steps from −60 to +40 mV (10 mV increments every 30 s, with −80 mV membrane-holding potential). (c) Kv1.3 channel number in WT (n=40) and Kcna3−/− (n=50) T cells after 48 h activation. The mean Kv1.3 channel numbers were 1667±187 in WT and undetectable in Kcna3−/− T cells. (d) Normalized WT and Kcna3−/− T cell K+ currents before and after Shk inhibition. 89% WT T cell K+ current was blocked by 1 nM Shk, but no Shk-sensitive current was detected in Kcna3−/− T cells. Kcna3−/− T-cell responses to activation. (e) Proliferation (left) and IFN-γ (right) responses to anti-CD3 and anti-CD28 stimulation. Spleen cells from WT or Kcna3−/− rats were stimulated for 3 days. Individual biological replicates (n=4 per group) are shown with mean±s.d. (f) Effects of ShK and TRAM-34 on polyclonal T-cell activation. Data are shown as mean±s.d. (n=4 biological replicates per group). (g) OVA-specific T-cell proliferation responses. Draining lymph node and spleen cells from OVA-immunized WT and Kcna3−/− rats were plated at a 1:10 lymph node:spleen cell ratio and stimulated in vitro with OVA at various concentrations. Data are shown as mean±s.d. (n=4 biological replicates per group). (h,i) Kcna3−/− rat dendritic cell competency. CD4+ (h) or CD8+. (i) T cells isolated from DLN of OVA-immunized WT (blue) and Kcna3−/− (green) rats were co-cultured with APCs from WT (filled circles) or Kcna3−/− (open circles) rats and stimulated with OVA. Proliferation responses were determined at day 3 of culture. Individual biological replicates (n=4 per group) are shown with mean±s.d.
To assess antigen-specific T-cell responses, Kcna3−/− and WT rats were immunized with ovalbumin (OVA) and then in vitro antigen recall assays were performed. Kcna3−/− T-cell recall responses to titred doses of OVA antigen were comparable to WT (Fig. 1g). Antigen presentation in Kcna3−/− rats was also fully competent, as the ability of antigen-presenting cells (APC) derived from OVA-immunized Kcna3−/− rats to mediate CD4+ and CD8+ T-cell OVA-specific recall responses was similar to WT, and vice versa (Fig. 1h,i). These data suggest that Kv1.3 is not required for the appropriate development of antigen-specific T-cell responses.
Kcna3−/− rats mount normal immune responses in vivo
To determine the functional consequence of the loss of Kv1.3 on T-cell responses in vivo, we employed rat models of adjuvant-induced arthritis (AIA) and DTH. AIA is induced by a single injection of complete Freund adjuvant (CFA), and is a model of human rheumatoid arthritis with CD4+ T cells having an important role in disease initiation and maintenance29,30,31. Kcna3−/− rats developed AIA in a manner similar to WT rats, indicating that there were no defects in T-cell activation (Fig. 2a). At day 21, both groups exhibited severe disease with clinical scores of 16.0±0.0 and 15.4±0.6 in WT and KO rats, respectively. DTH is an acute inflammatory immune response initiated by the activation of tissue-resident CD4+ TEM cells following rechallenge with antigen21,32. Kcna3−/− rats mounted an OVA-specific DTH response measurable in the ear that was comparable to WT rats (Fig. 2b). In this model, ShK treatment has been reported to reduce ear swelling when administered during the effector phase, suggesting that blockade of Kv1.3 impairs T-cell-mediated inflammation15. In contrast to published reports15, ShK did not inhibit DTH in our studies, consistent with our observations in Kcna3−/− rats (Fig. 2c).
(a) WT (blue) or Kcna3−/− (green) rats were given a single injection of CFA to induce AIA (filled symbols, n=5 biological replicates per group) or were untreated (open symbols, naive, n=2 per group) and clinical score assessed at day 21. Individual animals are represented by discrete symbols and mean±s.d. are shown. Delayed-type hypersensitivity. (b) WT (blue) or Kcna3−/− (green) OVA-immunized rats were subsequently challenged with OVA (filled symbols, n=6 biological replicates per group) or PBS (open symbols, n=4 per group) and ear swelling was measured 24 h later. Individual animals are represented by discrete symbols and mean±s.d. are shown. Experiment was performed twice, with each experiment delineated by the dotted line. Statistically significant differences are denoted with P values as determined by Student’s t-test. (c) Effect of Kv1.3 blockade on DTH inflammatory responses. WT rats were immunized with OVA then subsequently challenged 1 week later with either PBS or OVA. OVA-rechallenged animals were treated with control anti-ragweed (aRGW) antibody (pink), CTLA4-Ig (orange) or ShK (blue). Ear swelling was measured 24 h later. Individual biological replicates (n=6 per group) are shown with mean±s.d. Experiment was performed three times, with each experiment delineated by dotted lines. Statistically significant differences between ShK and anti-ragweed control groups are denoted with P values; CTLA4-Ig inhibition was statistically significant in all experiments (P<0.0001). (d) Relative gene expression of Kcna3 (Kv1.3), Kcnn4 (KCa3.1), Cd4, Cd8 or Ccr7 was determined on bulk DLN cells by normalizing to housekeeping gene Rpl19. Data are shown as mean±s.d. (e,f) OVA-specific in vitro recall response from OVA-immunized rats with PBS (e) or OVA (f) secondary challenge. Proliferation (left) and IFN-γ (right) responses were determined in the absence or presence of ShK, TRAM-34 or a combination of both (‘combo’). ‘No stim’ denotes unstimulated cell conditions (absence of OVA antigen). Data are shown as mean±s.d.
Analysis of Kcnn4 expression by mRNA showed that KCa3.1 was significantly upregulated in T cells from Kcna3−/− rats both after OVA immunization and OVA-challenge relative to WT rats (a three- to six-fold increase), whereas CD4 and CD8 mRNA levels were unaffected (Fig. 2d). Relative CCR7 expression was comparable between WT and KO, with decreased CCR7 in the OVA-rechallenged rats compared with those receiving PBS, indicating a larger TEM cell fraction (Fig. 2d). Since the expectation was for Kcna3−/− rats to be incapable of mounting an effector response, these results suggest that KCa3.1 can compensate for the absence of Kv1.3.
In vitro OVA-specific recall responses were performed to determine if Kcna3−/− T-cell responses were dependent on KCa3.1. Draining LN and spleen cells from WT or Kcna3−/− rats with DTH were stimulated in vitro with OVA. Antigen-specific recall responses from WT and Kcna3−/− rats were comparable in both proliferation and IFN-γ production (Supplementary Fig. 3). As Kcna3−/− T cells mounted fully competent responses, expression of KCa3.1 was sufficient for T-cell activation. To test whether Kcna3−/− T cells were solely dependent on KCa3.1, OVA-specific recall responses were performed in the presence of ShK, TRAM-34 or a combination of both. Despite treating cells with ShK and TRAM-34 at concentrations well above their reported Kd values (ShK Kd=10 pM (ref. 12), used at 10 nM; TRAM-34 Kd=20 nM (ref. 18), used at 10 μM), full inhibition of proliferation or IFN-γ was not achieved. ShK did not affect OVA-specific recall responses from PBS-rechallenged WT rats (Fig. 2e), but did inhibit recall responses from OVA-rechallenged rats, albeit not completely (Fig. 2f). TRAM-34 alone partially inhibited proliferation and IFN-γ production by either PBS- or OVA-rechallenged T cells (Fig. 2e,f). The combination of ShK and TRAM-34 completely inhibited T-cell responses. For Kcna3−/− T cells, TRAM-34 inhibitory effects were more robust and full inhibition was observed at the highest concentrations under both rechallenge conditions.
Repeated antigen-specific stimulation skews to Kv1.3 dependency
Sensitivity of T cells to ShK increased in DTH rats that received secondary challenge with OVA but not rechallenged with PBS (Fig. 2f). To examine if repeated antigen-specific stimulation would bias T-cell K+ channel dependency from KCa3.1 towards Kv1.3, WT and Kcna3−/− rats were immunized with two different antigens. One antigen, OVA, was administered three times, while the second antigen, myelin basic protein (MBP), was given once, together with OVA in the last immunization (Fig. 3a). In WT draining lymph node CD4+ T cells, Kcna3 transcript levels increased approximately five-fold after three rounds of repeated antigen stimulation, compared with Kcnn4 levels that decreased nearly 70% with repeated OVA stimulation (Fig. 3b). In contrast, expression of KCa3.1 in Kcna3−/− CD4+ T cells increased with each immunization, doubling after three rounds. CCR7 expression in primary OVA-immunized rats was similar to expression in naive CD4+ T cells, but was reduced following the third round of immunization, and no difference was detected between WT versus Kcna3−/− rats (Fig. 3b). Frequencies of CD4+ and CD8+ T cells in WT and Kcna3−/− rat spleens or draining lymph nodes were similar after single or repeated OVA immunization (Supplementary Fig. 4).
(a) Experimental design. WT or Kcna3−/− rats (n=4 per group) were immunized three times with OVA and one time with MBP, administered concurrently during the final immunization. (b) Relative expression of Kcna3 (Kv1.3), Kcnn4 (KCa3.1) or Ccr7 in CD4+ T cells isolated from DLN of WT (blue) or Kcna3−/− (green) rats was calculated by normalizing to housekeeping gene Rpl19. Data are shown as mean±s.d. ‘<l.o.d.’ denotes below limit of detection. (c,d) In vitro recall stimulation was performed using cells harvested from WT (blue) or Kcna3−/− (green) rats immunized three times with OVA and one time with MBP, with OVA (c) or MBP (d) as antigen and proliferation (left) and IFN-γ (right) responses determined after 3-day stimulation. Individual biological replicates (n=4 per group) are shown with mean±s.d. (e,f) Effects of ShK (blue), TRAM-34 (green) and inhibitor combination on T-cell responses to in vitro restimulation with OVA (e) or MBP (f). For combination treatment (combo), cells were cultured with 10 nM ShK and 10 μM TRAM-34. ‘No stim’ denotes unstimulated cell conditions. Data are shown as mean±s.d. (n=4 biological replicates per group).
To determine if the changes in expression observed at the transcriptional level were reflected in functional protein expression, we examined the sensitivity of T cells to specific inhibitors of Kv1.3 and KCa3.1. Upon in vitro stimulation, WT and Kcna3−/− T-cell responses were similar against both OVA (Fig. 3c) and MBP (Fig. 3d). ShK inhibited T-cell responses from WT animals repeatedly immunized with OVA (Fig. 3e) but not from WT animals receiving single immunization with MBP (Fig. 3f). In contrast, TRAM-34 inhibited, albeit not completely, WT T-cell responses regardless of antigen and TRAM-34 effects were enhanced in Kcna3−/− T cells. Complete abrogation of both OVA-specific and MBP-specific WT T-cell responses was observed only with combination treatment with both ShK and TRAM-34, a result achieved in Kcna3−/− T cells with TRAM-34 alone (Fig. 3e,f).
Human T cells gain Kv1.3 dependency with repeated stimulation
As described above, rat T cells become dependent on Kv1.3 following multiple rounds of antigen-specific stimulation. To explore whether human T cells are similarly driven from KCa3.1 towards Kv1.3 dependency through repeated antigen stimulation, we examined human T-cell responses to tetanus toxoid (TT) either directly ex vivo or after multiple rounds of in vitro stimulation. We selected TT as most donors have prior exposure to the antigen from vaccination against tetanus. Ex vivo T-cell responses to stimulation with TT were only weakly inhibited by ShK, but strongly inhibited by TRAM-34, with similar effects observed for CD4+ and CD8+ T cells (Fig. 4a–c). As observed previously in rat T cells, the combination of ShK and TRAM-34 fully abrogated T-cell responses (Fig. 4d). Expression of KCNA3 and KCNN4 by mRNA confirmed that these were the only two K+ channels expressed on these T cells ex vivo (Supplementary Fig. 5a,b). TT-specific T-cell lines were generated by multiple rounds of TT restimulation together with autologous APCs. After four rounds of stimulation, the sensitivity of TT-specific CD4+ T cells to ShK and TRAM-34 was reversed, with ShK inhibiting proliferation and IFN-γ production more profoundly than TRAM-34 (Fig. 4e). Sensitivity to ShK was increased with each round of stimulation while TRAM-34 sensitivity was reduced (Fig. 4f). Supporting the observed differential response to ShK and TRAM-34, expression of KCNA3 and KCNN4 by mRNA showed Kv1.3 was increased and KCa3.1 decreased in TT T cells after four rounds of stimulation relative to expression after the primary stimulation (Fig. 4g and Supplementary Fig. 5a,b). Concomitant increases in Kv1.3 cell surface protein expression were detected in repeatedly stimulated TT-specific T cells (Fig. 4h).
(a,b) Inhibition of CD4+ (a) or CD8+ (b) T-cell proliferation response to TT stimulation as determined by CFSE dilution. One representative donor is shown. Percentages indicated in red denote % reduction in proliferation relative to vehicle-treated cells. Primary (1°) T-cell response to TT was determined in the absence or presence of either 10 nM ShK (n=8 biological replicates) or 1 μM TRAM-34 (n=9). (c) Proliferation responses were determined at day 4; IFN-γ concentrations were measured at day 3. % inhibition was determined by comparing proliferation or IFN-γ concentration in the presence of inhibitor to vehicle control. Data are shown as individual data points with mean±s.d. Statistically significant differences are denoted with P values as determined by Student’s t-test. (d) Inhibition of both Kv1.3 and KCa3.1 fully abrogates TT-specific T cell responses. PBMC from T1D donors were stimulated with TT in the absence or presence of 10 nM ShK, 1 μM TRAM-34 or a combination of both (combo). ‘No stim’ denotes absence of TT. Data are shown as mean±s.d. of replicate wells and are representative of three independent experiments. (e) Proliferation and IFN-γ production of TT-specific T cells following four rounds of stimulation (4°). After three rounds of TT stimulation, cells were rested and then restimulated in the presence of irradiated autologous PBMC with TT in the absence or presence of either 10 nM ShK (n=11 biological replicates) or 1 μM TRAM-34 (n=4). (f) Effect of ShK or TRAM-34 on proliferation or IFN-γ production of TT-specific T cells after increasing rounds of stimulation. Data shown are representative of one donor. (g) Gene expression of KCNA3 and KCNN4 in purified T cells after 1° or 4° TT stimulation. Expression of each channel is presented relative to expression in naive T cells. Data shown are representative of three donors. (h) Kv1.3 surface protein expression on 1° TT or 4° TT cells. Blue histogram represents Kv1.3 staining; grey filled histogram represents isotype control.
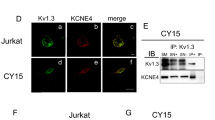
Despite the changes in expression, TT-specific cell lines required both Kv1.3 and KCa3.1 for maximal responsiveness. To confirm this and ask whether Kv1.3 was critical for T-cell activity, we performed siRNA-targeted knockdown of Kv1.3, KCa3.1 or both in the TT-specific recall responses ex vivo and in the TT-specific T cell-lines. Kv1.3 expression was reduced by at least 90% with Kv1.3 or combination siRNA and KCa3.1 expression reduced by about 85% (Fig. 5a). Knockdown of Kv1.3 protein expression was confirmed by flow cytometry (Fig. 5b). In primary TT-stimulated T cells, KCNN4 siRNA knockdown conferred sensitivity to ShK and rendered these cells insensitive to TRAM-34, indicating that, while KCa3.1 is the predominant channel on antigen-specific T cells, Kv1.3 can functionally compensate for the loss KCa3.1 (Fig. 5c,d). Silencing of Kv1.3 enhanced sensitivity to TRAM-34, indicating that endogenous Kv1.3 functionally complements KCa3.1 (Fig. 5c,d). In TT-specific T-cell lines subjected to four rounds of stimulation, knockdown of Kv1.3 reversed the inhibitory effects of ShK and conferred sensitivity to TRAM-34, whereas knockdown of KCa3.1 had minimal impact (Fig. 5e,f). Disruption of both Kv1.3 and KCa3.1 expression rendered T cells unresponsive to in vitro recall stimulation, regardless of the number of exposures to antigen. Thus, in vaccine-induced memory T cells, Kv1.3 and KCa3.1 both have important roles in mediating T-cell responses.
(a) Kv1.3 (left) and KCa3.1 (right) expression was measured in primary TT-stimulated T cells (1° TT) or T cells that underwent four rounds of TT stimulation (4° TT) that were transfected with Kv1.3 siRNA (blue bars), KCa3.1 siRNA (green bars), a combination of both siRNA (orange bars) or scramble control siRNA (grey bars). Relative expression of targeted genes is shown in comparison with scramble siRNA transfected cells. Data are shown as mean±s.d. of triplicate measurements from one representative experiment. (b) Kv1.3 surface protein expression on 1° TT or 4° TT cells following siRNA transfection. Primary (left) or repeatedly stimulated (4°, right) TT cells were transfected with Kv1.3 siRNA (red histograms) or scramble siRNA (blue histograms) and then stained for Kv1.3 48 h later. Grey filled histogram represents isotype control. T-cell responses of 1° TT-stimulated T cells (c,d) or 4° TT-stimulated T cells (e,f) transfected with Kv1.3 siRNA (blue), KCa3.1 siRNA (green), a combination of both (orange) or scramble control siRNA (black). Cells were then restimulated with anti-CD3 (0.5 μg ml−1) in the absence or presence of ShK (c,e) or TRAM-34 (d,f) at the indicated concentrations. Proliferation responses were determined at day 4 of culture by 3H-thymidine incorporation; IFN-γ concentration was measured in culture supernatants harvested 3 days after restimulation. Data are shown as mean±s.d. of replicate wells and are representative of at least two independent experiments.
Autoreactive T cells are primarily dependent on Kv1.3
Unlike vaccine-induced T cells, autoreactive T cells have been chronically exposed to their specific autoantigen, and therefore we asked if there was different K+ ion channel dependency in autoreactive T cells. Peripheral blood mononuclear cells (PBMCs) from HLA-typed Type I diabetes donors were stimulated with a pool of four HLA-DR4-restricted GAD65-derived peptides or with GAD65 protein in the presence of Kv1.3 inhibitor ShK or KCa3.1 inhibitor TRAM-34. ShK inhibited GAD65-specific T-cell proliferation and IFN-γ production, but the effect was only partial; in contrast, T-cell responses were minimally affected by TRAM-34 (Fig. 6a,b). Differential sensitivity to ShK and TRAM-34 was similar whether peptide pool or whole protein was used, and similar effects were observed on both CD4+ and CD8+ T cells (Supplementary Fig. 6b,c). Combined blockade of both Kv1.3 and KCa3.1 resulted in full inhibition of GAD65-specfic T-cell responses (Fig. 6c).
(a) PBMC from HLA-DR4+ T1D donors (n=10 biological replicates) were stimulated with a combination of HLA-DR4-restricted GAD65 peptides in the absence or presence of either 10 nM ShK or 1 μM TRAM-34. (b) PBMC from non-HLA- or HLA-typed T1D donors were stimulated with GAD65 protein (n=13 biological replicates). Proliferation responses (left) were determined at day 4. IFN-γ concentrations (right) were measured 3 days after stimulation. %inhibition was determined by comparing proliferation or IFN-γ concentration in the presence of inhibitor to vehicle control. Data are shown as individual data points with mean±s.d. Statistically significant differences are denoted with P values as determined by Student’s t-test. (c) Inhibition of both Kv1.3 and KCa3.1 fully abrogates autologous autoreactive T cell responses. PBMC from T1D donors were stimulated with GAD65 protein in the absence or presence of 10 nM ShK, 1 μM TRAM-34 or a combination of both (combo). ‘No stim’ denotes unstimulated cell conditions (absence of GAD65 protein). Data are shown as mean±s.d. of replicate wells and are representative of three independent experiments. Gene expression for Kv1.3 (KCNA3, d) and KCa3.1 (KCNN4, e) in GAD65-stimulated purified T cells following siRNA transfection with Kv1.3 siRNA (blue), KCa3.1 siRNA (green) or scramble control siRNA (grey). (f,g) Effects of siRNA knockdown of Kv1.3 or KCa3.1 on sensitivity to inhibitors. PBMC from T1D donor was stimulated with GAD65 protein for 7 days. After 3 days rest, T cells were purified and transfected with Kv1.3 siRNA (blue), KCa3.1 siRNA (green) or scramble control siRNA (grey) and then restimulated with anti-CD3 (0.5 μg ml−1) in the absence or presence of ShK (f) or TRAM-34 (g) at the indicated concentrations. Data are shown as mean±s.d. of replicate wells and are representative of at least two independent experiments.
Complete inhibition was achieved when both ShK and TRAM-34 were present, suggesting that both Kv1.3 and KCa3.1 are functionally expressed. However, Kv1.3 is the predominantly active channel as seen by the greater susceptibility to ShK. To explore whether KCa3.1 is functional in GAD65-specific T cells, Kv1.3 expression was ablated using siRNA knockdown (Fig. 6d). Conversely, KCa3.1 was targeted (Fig. 6e) to determine its relative contribution to regulation of T-cell responses. siRNA knockdown of KCNA3 reversed the inhibitory effects of ShK, rendering GAD65-specific T-cell proliferation and IFN-γ responses unaffected by ShK (Fig. 6f). Susceptibility to TRAM-34 was enhanced, however, indicating that in the absence of Kv1.3, KCa3.1 is present and sufficient to mediate T-cell activation (Fig. 6g). KCNN4 siRNA knockdown had no effect on either ShK or TRAM-34 sensitivity (Fig. 6f,g), validating the notion that Kv1.3 is the predominant channel in GAD65-specific autoreactive T cells.
Kv1.3/KCa3.1 dominance depends on antigen exposure history
Human T cells that have experienced chronic antigen-specific stimulation, either in the autoimmune setting or through repeated in vitro stimulation, were found to be preferentially dependent on Kv1.3. As the T-cell repertoire is diverse and reflects the history of antigen exposure experienced by an individual, we next examined whether T cells from the same donor, but with different antigen specificities, had differential biases for Kv1.3 or KCa3.1. PBMC from T1D donors were stimulated in vitro with either GAD65, representing an antigen recognized by chronically exposed T cells, or a pathogen-derived antigen such as TT, against which a resting memory pool of T cells is present. Comparing the GAD65-specific to TT-specific T-cell responses from the same donor, differential sensitivities to ShK and TRAM-34 were seen. Consistent with earlier data, GAD65-specific T-cell responses were inhibited by ShK (Fig. 7a), whereas TRAM-34 inhibited autologous TT-specific T-cell responses (Fig. 7b and Supplementary Fig. 6a,b). Influenza A hemagglutinin (HA)- and cytomegalovirus (CMV) -specific responses from T1D donors were also inhibited by TRAM-34 but not ShK (Supplementary Figs 7 and 8).
(a,b) ShK inhibits GAD65-specific T1D T cells but not autologous TT-specific T cells. PBMC from T1D donors (n=6 biological replicates) were stimulated with a combination of four HLA-DR4-restricted GAD65 peptides. Proliferation and IFN-γ responses were compared with TT stimulation in the absence or presence of either 10 nM ShK (a) or 1 μM TRAM-34 (b). Data shown are % inhibition of proliferation response as determined by 3H-thymidine incorporation after 4 days primary in vitro stimulation and % inhibition of IFN-γ production after 3 days stimulation. Coloured symbols and corresponding lines represent each individual donor.
Conversion to Kv1.3 dependency is stable
KCa3.1 and Kv1.3 are both functionally expressed in all T cells, regardless of their antigen experience. However, in the initial exposure, KCa3.1 is the predominant channel that is involved in T-cell activation, as evidenced by higher relative gene expression levels and sensitivity to TRAM-34 inhibition. As T cells are repeatedly exposed to antigen, functional K+ channel requirement skews towards Kv1.3, as Kv1.3 relative gene expression is increased and T cells become susceptible to ShK. The conversion from KCa3.1 dependence to Kv1.3 driven by repeated antigen stimulation appears to be part of a progressive differentiation process in memory T cells. Notably, antigen-specific stimulation is a key requirement in this process, as T cells with the conventional CCR7−CD45RO+ TEM phenotype are not affected by ShK when polyclonally activated with anti-CD3 and anti-CD28 antibodies (Fig. 8). This was demonstrated using sorted naive, TEM and central memory (TCM) CD4+ and CD8+ T cells (Fig. 8a–c), purified CD4+ T cells repeatedly stimulated with anti-CD3 (Fig. 8d) and repeatedly anti-CD3 stimulated purified memory CD4+ T cells (Fig. 8e).
(a) Expression of Kv1.3 and KCa3.1 on sorted CD4+ and CD8+ naive, TCM and TEM subsets. CD45RO and CCR7 as markers to define naive, TCM and TEM subsets as shown in dot plots. Expression was determined on ex vivo cell subsets or on sorted T-cell subsets after 4 days stimulation with anti-CD3 and anti-CD28. Kv1.3 and KCa3.1 expression were normalized to RPL19 expression and shown relative to expression in ex vivo naive cells. (b) Effect of ShK on naive, TCM and TEM CD4+ subsets. Sorted cells were stimulated with anti-CD3 and either vehicle or 1 μM ShK. Proliferation was determined at day 4 of stimulation; IFN-γ was measured after 3 days. (c) Bulk PBMC from healthy donors were stimulated with anti-CD3 and anti-CD28 in the absence or presence of 10 nM ShK or 1 μM TRAM-34. IFN-γ production was measured after 3 days stimulation. Proliferation responses were determined at day 7 by CFSE dilution of CD4+- or CD8+-gated cells. Representative dot plots from one donor are shown. % inhibition of proliferation was determined by comparing proliferation in the presence of inhibitor to proliferation of cells in the presence of vehicle control. Data are shown as individual data points with mean±s.d. (n=15 biological replicates). (d) CD4+ T cells repeatedly stimulated with anti-CD3 and anti-CD28. Purified CD4+ T cells from healthy donor were stimulated with 5 μg ml−1 plate-bound anti-CD3 and 2 μg ml−1 soluble anti-CD28 for 4 days. Cells were then harvested, washed, and rested for 3 days. In subsequent stimulations, cells were reactivated with 1 μg ml−1 soluble anti-CD3 and 1 μg ml−1 anti-CD28. In the fourth round of stimulation, cells were cultured with 10-fold increases in ShK concentrations, starting at 10−5 nM. Cell supernatants were harvested 3 days after initiation of last round of stimulation for determination of IFN-γ. Proliferation responses were determined at day 4 by 3H-thymidine incorporation. (e) Purified memory CD4+ T cells were stimulated for six rounds with anti-CD3 and anti-CD28, as described in d.
To address whether the shift to Kv1.3 with repeated antigen stimulation was stable, T cells that had undergone primary in vitro stimulation with TT in the absence or presence of ShK or TRAM-34 were rested, then restimulated. In the primary stimulation, T cells treated with ShK responded as well as vehicle control-treated cells, whereas responses were inhibited by TRAM-34 (Supplementary Fig. 9a). In the secondary stimulation, ShK and TRAM-34 treatment had the same effect on T cells regardless of their prior exposure to channel blockers. T cells treated with TRAM-34 had reduced proliferation and IFN-γ production in the primary stimulation, but were affected by ShK to a similar degree as T cells initially treated with vehicle control or ShK. This suggests that treatment with TRAM-34 did not influence K+ channel expression. These findings were consistent with TT-specific T cells that underwent further rounds of restimulation (Supplementary Fig. 9b). TT T cells having undergone three rounds of stimulation were sensitive to ShK. In the restimulation, T cells retained ShK sensitivity, indicating that prior blockade of Kv1.3 did not induce a shift to KCa3.1 (Supplementary Fig. 9c). Thus, prior exposure to inhibitor did not alter Kv1.3 or KCa3.1 channel dependence, suggesting that the K+ channel requirements are stable and are a function of antigen exposure history.
Discussion
Electrophysiological patch-clamp methods allow specific channel activity to be studied at the single-cell level, and have thus been an invaluable tool contributing to the understanding of the role of Kv1.3 and KCa3.1 in purified, well-defined T-cell subtypes. The limitation of these methods, however, is that T-cell activation under physiological conditions is complex, and two channels cannot be studied simultaneously in the same cell. While exquisite control of voltage and membrane potential allows for study of Kv1.3 and Ca2+ influx for KCa3.1, these factors go hand-in-hand with TCR activation. Thus, while channel blockers can fully abrogate-specific channel function in patch-clamp experiments, we find that in vitro stimulated T-cell responses are only partially inhibited. Others have also observed partial inhibition with ShK and more selective/potent variants, or other Kv1.3 blockers, when functional readouts such as proliferation or cytokine production were used to assess T-cell responses, even at concentrations orders of magnitude greater than Kd values determined by electrophysiology12,13,14,15,16,20,25,26.
We generated a Kv1.3-deficient rat to definitively assess the requirement for Kv1.3 in elaboration of T-cell responses under various stimulation conditions. Kcna3−/− rat T cells were fully functional when polyclonally activated or stimulated with specific antigen in in vitro recall assays, demonstrating that Kv1.3 was not required under these primary activation conditions. Using a CD4+ T-cell-dependent model of arthritis, Kcna3−/− rats developed disease similarly to WT rats, indicating that Kv1.3 deficiency did not compromise immune CD4+ T-cell function. We then used DTH as a model where inflammation has been shown to be dependent on infiltrating TEM cells that express high levels of Kv1.3 (refs 21, 32). DTH studies in Kcna3−/− rats allowed for study of the effects of complete absence of Kv1.3 on generation of inflammatory responses. Ear inflammation in Kcna3−/− rats was not dramatically different from WT, with one experiment showing slightly reduced inflammation but a second having mildly more severe inflammation. Thus, in the complete absence of Kv1.3, T cells were uncompromised in their ability to perform effector functions and mediate inflammation, likely due to the presence of KCa3.1. Our DTH studies in Kcna3−/− rats were consistent with the modest therapeutic effects achieved through pharmacological blockade of Kv1.3. Previous reports have shown that efficacy could be achieved with Kv1.3 inhibitors, but highly variable effects were observed, with reduction ranging from no significant effect to as high as 80%, with various compounds12,13,15,25,26,33,34,35. The complementary and compensatory roles of Kv1.3 and KCa3.1 in T cells is also supported by published studies where treatment with TRAM-34 to block KCa3.1 channels ameliorated inflammation in DTH36. In addition, while our studies have focused on the K+ channels, other channel types such as store-operated Ca2+ entry channel CRAC and non-store-operated Ca2+ channel TRPV1 also have roles in TCR-induced Ca2+ influx and regulation of TCR signalling and T-cell activation37,38.
In addition to demonstrating that Kv1.3 was not required to mediate a TEM-dependent inflammatory response, the DTH model revealed that repeated OVA immunization increased T-cell susceptibility to Kv1.3 inhibition. T cells from rats receiving a single primary immunization, T-cell proliferation and cytokine production were inhibited by TRAM-34 and are relatively insensitive to ShK treatment. Conversely, T cells from rats repeatedly immunized with OVA exhibited increased sensitivity to ShK associated with an increase in Kv1.3 expression.
Importantly, we also observed that the inhibition mediated by single-channel blockers was not complete, and a combination of both ShK and TRAM-34 was required to achieve full abrogation of T-cell responses. These findings indicate that Kv1.3 and KCa3.1 are sufficient to regulate the T-cell response, and suggest that other K+ channels such as the two-pore domain K+ channel TASK1 (refs 39, 40) do not play a significant role. This validated our findings in the Kcna3−/− rat, showing that KCa3.1 was sufficient to mediate normal activation responses in T cells normally reliant on Kv1.3 and that KCa3.1 may compensate for impaired Kv1.3 function mediated by blockers such as ShK. Repeated antigen stimulation conferred a functional Kv1.3 expression phenotype that is consistent with published data using repeatedly activated human autoreactive T cells. CCR7 expression was reduced in T cells isolated from animals chronically exposed to antigen, indicating that T cells were differentiating towards a TEM phenotype. That sensitivity to ShK was elevated in cells having reduced CCR7 expression is consistent with the notion that autoreactive TEM cells would be amenable to Kv1.3 blockade.
On the basis of the rat data, susceptibility to Kv1.3 inhibitor is a property of repeatedly stimulated antigen-specific T cells, with increasing exposures to antigen driving T-cell dependency on KCa3.1 towards Kv1.3 as the prevalent channel. The transition from ShK-insensitivity of primary stimulated antigen-specific T cells to ShK susceptibility following multiple rounds of stimulation suggests that antigen-specific T cells become ‘programmed’ towards Kv1.3 dependency, and that this transition is not well demarcated but becomes enforced with chronic stimulation. Our data supports published reports that T cells isolated from patients with autoimmune disease, including multiple sclerosis, rheumatoid arthritis and Type 1 diabetes (T1D), express high levels of Kv1.3 on a per cell basis11,15,16,20,41. However, demonstration of autoreactive T-cell susceptibility to Kv1.3-targeted inhibition typically requires restimulation with antigen for as many as a dozen times15,16,34. Thus, the requirement for chronic antigen stimulation that we observed for rat T cells may be translatable to autoreactive human T cells.
We report that human T-cell dependency on Kv1.3 was also driven by repeated antigen stimulation. Using TT, CMV and influenza as model pathogens, we demonstrated that in a primary in vitro stimulation response, T-cell proliferation and cytokine production were inhibited by TRAM-34 and were relatively insensitive to ShK treatment. Conversely, T cells from T1D patients stimulated with an autoantigen such as GAD65 were sensitive to ShK, but not TRAM-34. Notably, repeated stimulation with TT increased sensitivity of antigen-specific T cells to ShK, conferring upon these cells a functional Kv1.3 expression phenotype similar to autoreactive T cells. We also observed that the inhibition mediated by ShK or TRAM-34 was not complete under these conditions, and a combination of both was required to achieve full abrogation of T-cell responses. Additionally, silencing of Kv1.3 expression in GAD65-specific and repeated stimulated TT-specific T cells rendered these cells insensitive to ShK, but surprisingly these cells were now sensitive to TRAM-34, indicating that functional KCa3.1 channels were present and active, compensating for the absence of Kv1.3.
Patch-clamp experiments have formed the basis for the Kv1.3/TEM vs. KCa3.1/naive/TCM expression paradigm. However, the conventional definition of TEM cells using surface markers such as CCR7 and CD45RO may not be sufficient to identify those cells that have high functional levels of Kv1.3 expression and are thus more susceptible to Kv1.3 blockade. Antigen-specific T cells are comprised of a mix of TEM and TCM cells on the basis of CCR7 and CD45RO expression, and CD4+ T cells acquire the TEM phenotype following repeated stimulation. However, T cells activated in vitro in the primary stimulation with specific pathogen-derived antigens are not susceptible to Kv1.3 inhibitors such as ShK. Nor are T cells driven to the CCR7−CD45RO+ phenotype through repeated anti-CD3 stimulation, which remain refractory to ShK inhibition. T cells derived from autoimmune disease patients stimulated with autoantigen have a similar mixed CCR7/CD45RO expression profile as pathogen-stimulated T cells, yet autoreactive T cells are amenable to Kv1.3 inhibitors. Of note, Kv1.3-targeted inhibition of TEM cells in the literature is typically demonstrated on antigen-specific human or rat T-cell lines that have been restimulated with antigen for as many as 12 times15,16,34. Thus, a CCR7+CD45RO+ TEM phenotype alone may not necessarily mark the T cell as a target for Kv1.3 inhibition.
On the basis of our combined data from rat and human T cells, susceptibility to Kv1.3 inhibitor is a property of repeatedly stimulated antigen-specific T cells. Activation alone is not sufficient since repeated anti-CD3 stimulation does not increase sensitivity to ShK; instead, it is the number of exposures to antigen that dictates whether Kv1.3 or KCa3.1 is the prevalent channel. The transition from ShK-insensitivity of primary stimulated TT-specific T cells to ShK susceptibility following multiple rounds of stimulation suggested that antigen-specific T cells become ‘programmed’ towards Kv1.3 dependency, and that this transition was not well demarcated but became enforced with chronic stimulation. Repetitive antigen stimulation is a factor that can influence memory T-cell differentiation. For CD8 T cells, multiple antigen encounters, through prime-boost vaccinations or pathogen reencounter, increase memory T-cell numbers and dramatically impact their phenotype and function42,43,44,45. Several hundred genes can potentially be differentially regulated with each subsequent round of antigen encounter, resulting in memory cells with unique transcriptome repertoires46. The mechanisms responsible for conversion from KCa3.1 to Kv1.3 dependency remain to be elucidated.
Collectively, we demonstrate that Kv1.3 is the predominant functionally active channel in T cells subjected to repeated specific antigen exposure and that KCa3.1 compensates for loss of functional Kv1.3 as in the presence of Kv1.3 inhibitors. Prior reports of differential expression of Kv1.3 and KCa3.1 on discrete subsets of T cells and their specific inhibition by selective inhibitors have made these K+ channels attractive therapeutic targets. In particular, the suggested predominance of Kv1.3 on TEM cells has led to profound interest in developing Kv1.3 inhibitors for suppression of autoimmune reactions. Our work supports the possibility of achieving beneficial effects by targeting Kv1.3 in the autoimmune context, but with the caveat that the inhibition of autoreactive T-cell functions may not be complete due to compensatory actions of KCa3.1.
Methods
Kcna3−/− rats
Kcna3−/− rats were generated on Dark Agouti background at SAGE Labs (Boyertown, PA). Zinc finger nuclease targeting produced an 1178, bp deletion in Kcna3 corresponding to genomic coordinates chr2:229,233,225-229,234,403 (m5 genome assembly). Kcna3−/− and WT littermates were housed and maintained at Genentech in accordance with American Association of Laboratory Animal Care guidelines. Eight- to ten-week-old female rats were used in all experiments. All experimental animal studies were conducted under the approval of the Institutional Animal Care and Use Committees of Genentech Lab Animal Research.
Human cells
Human PBMC were isolated from donor blood by Ficoll gradient centrifugation. Blood from healthy control and CMV+ donors was collected as part of the Genentech blood donor program, with written informed consent and approval from the Western Institutional Review Board. T1D patient blood was obtained from BioreclamationIVT (non-HLA-typed, Westbury, NY), and HLA-DR0401-typed T1D blood from Benaroya Research Institute (Seattle, WA).
Electrophysiology
Patch-clamp experiments were performed in whole-cell configuration using a SyncroPatch 768PE system (Nanion Technologies, Germany). Due to the relatively small size of T cells, single-hole, high-resistance (∼10 MΩ) borosilicate glass planar chips were used. Data was acquired with SyncroPatch PatchControl384 1.4.1 software and data analysis was performed with IgroPro 6.3.7.2 (Wavemetrics, OR) and Prism 6 (GraphPad, CA). The intracellular solution used contained (in mM): 50 KCl, 60 KF, 10 NaCl, 20 EGTA and 10 HEPES (pH 7.2, osmolarity 285 mOsm), and extracellular solution contained (in mM): 140 NaCl, 4 KCl, 2 CaCl2, 1 MgCl2, 5 Glucose and 10 HEPES (pH 7.4, osmolarity 300 mOsm). The holding potential for all experiments were set at −80 mV, and currents were elicited by depolarizing voltage steps from −60 to +40 mV (10 mV increments) for kinetic study or by repetitive pulses to 40 mV for all other studies. Currents were sampled at 20 kHz and filtered with Bessel filter. Series resistance was compensated 80% with leak subtraction. Seal resistance (Rseal) was calculated using built-in protocols, and cells with Rseal<500 MΩ were excluded from analysis. Kv1.3 channel numbers per cell were determined by dividing the 1 nM Shk-sensitive whole-cell conductance by the single-channel conductance of Kv1.3 (11 pS) (ref. 47). In pharmacological test, current was elicited every 30 s, 5 min for both before and after applying compound. Patch-clamp measurements are presented as the means±s.e.m.
In vitro cell T-cell assays
Rat T-cell responses to anti-CD3 and anti-CD28 activation were determined using spleen cells from naive animals. 1 × 106 spleen cells were plated on 96-well plates precoated with 5 μg ml−1 anti-rat CD3 (clone G4.18, BD Biosciences) in a final volume of 200 μl complete RPMI media (RPMI 1640 media supplemented with 10% FBS, 2 mM glutamine, 2 μM 2-ME, 1 mM sodium pyruvate, 100 U ml−1 penicillin and 100 μg ml−1 streptomycin) supplemented with 2 μg ml−1 soluble anti-rat CD28 (clone JJ319, BD Biosciences).
In vitro recall responses to OVA were performed using spleen and draining lymph node cells harvested from rats immunized with trinitrophenyl-OVA (TNP-OVA), with cells harvested 10 days post immunization. For in vitro recall responses to multiple antigens, rats were immunized at day 0 with TNP-OVA in CFA at 1 mg ml−1, followed by subsequent immunizations at day 14 and day 28 with TNP-OVA in incomplete Freund’s adjuvant at 1 mg ml−1. At day 28, the rats were additionally immunized with MBP 68-86 peptide in incomplete Freund’s adjuvant at 1 mg ml−1. Cells were harvested at day 38. For antigen-specific in vitro stimulation, DLN cells were plated at 1 × 105 cells per well together with spleen cells at 1 × 106 cells per well in final volume of 200 μl per well in 96-well plates in complete RPMI media. Cells were stimulated with OVA or MBP at 10 μg ml−1 unless otherwise indicated.
For assessment of APC function, CD4+ or CD8+ T cells were purified from draining lymph nodes and spleen of OVA-immunized WT and KO rats using magnetic bead separation (Miltenyi Biotec). Purity of isolated cells was validated using flow cytometry and was >95% for all cell types. For isolation of APCs, spleen cells were additionally depleted of T cells and 1 × 106 T-cell-depleted spleen cells were plated and placed in 37° humidified incubator. After 1 h, nonadherent cells were gently aspirated off to leave adherent APCs. 1 × 105 CD4+ or CD8+ T cells were plated in final volume of 200 μl complete RPMI and OVA added at 10 μg ml−1.
For rat T-cell assays, supernatants were harvested after 3-day culture for quantization of IFN-γ concentrations using rat IFN-γ Quantikine ELISA kit (Kit RIF100, R&D Systems). Proliferation was assessed using CellTiter-Glo (Promega), measuring relative luminescence units following manufacturer’s protocol.
Antigen-specific in vitro cell stimulation of human cells was performed using TT (derived from Clostridium tetani, Calbiochem, EMD Millipore, Billerica, MA or Reagent Proteins, San Diego, CA), a combination of CMV pp65 PepMix (pool of 138 peptides derived from peptide scan through pp65 of human CMV) and IE-1 PepMix (pool of 120 peptides derived from immediate-early protein 1 of human CMV) (JPT Peptide Technolologies, Berlin, Germany), HLA-DR0401-restricted influenza-derived HA306-318 peptide (Benaroya Research Institute), GAD65 protein (Abcam, Cambridge, MA) or a combination of HLA-DR0401-restricted GAD65 P15, GAD65265-284, GAD65273-292 and GAD65553-572 peptides representing frequently recognized epitopes48 (Benaroya Research Institute). TT and GAD65 protein stimulations were performed at 5–10 μg ml−1, CMV PepMix combination stimulation was performed using 5 μg ml−1 of each PepMix, individual GAD65 peptide and HA peptide stimulations were performed at 10 and 2.5 μg ml−1 of each individual GAD65 peptide was used in the combination stimulation. Primary stimulations were cultured for 4–7 days, depending on the readout for proliferation. For repeated stimulations, cells were collected, spun down, washed, then rested for 3 days. For antigen-specific restimulation, frozen autologous PBMC were thawed and irradiated at 2000, rad, then plated with antigen and rested cells. This cycle was repeated for each round of restimulation. Cells were cultured in either complete RPMI media or in RPMI 1640 supplemented with 2 mM L-glutamine, pen/strep and 10% pooled human serum (MP Biomedicals, Santa Ana, CA). In restimulations, media was supplemented with human IL-2T cell growth factor (Hemagen Diagnostics, Columbia, MD).
For anti-CD3 stimulation of human T cells, primary activation was performed using 5 μg ml−1 plate-bound anti-human CD3 (clone SP34-2, BD Biosciences). A total of 2 μg ml−1 soluble anti-human CD28 (clone CD28.2, BD Biosciences) was added for primary activation when indicated. For subsequent restimulations, after 4 days activation, cells were rested for 3 days, then restimulated with 0.5–1 μg ml−1 anti-CD3.
Kv1.3-specific channel blocker ShK was purchased from Bachem (Torrance, CA) and resuspended in PBS. KCa3.1-specific blocker TRAM-34 was purchased from Sigma-Aldrich (St. Louis, MO) and resuspended in DMSO. Cells were preincubated with inhibitors for 30 min at 37 °C in humidified, 5% CO2 incubator, before stimulation.
In human T-cell assays, for carboxyfluorescein succinimidyl ester (CFSE) dilution, cells were labelled with 2.5 μM CFSE for 5 min at room temperature followed by extensive washing, before setting up stimulations. CFSE dilution was assessed by flow cytometry after 7 days. For [3H]-thymidine incorporation proliferation assays, 1 μCi [3H]-thymidine (Perkin-Elmer) in a volume of 50 μl was added to each well for the past 16–18 h of a 4 day culture. Cells were then harvested and [3H]-thymidine incorporation was measured by liquid scintillation counting. IFN-γ concentrations were measured in human cell culture supernatants using ELISA kits specific for human IFN-γ (BD Biosciences or R&D Systems).
Proliferation and IFN-γ data are expressed as either raw data values to show relative strength of responses, as percentages of vehicle-treated control values to allow normalization of inhibitor effects to responses in the absence of inhibitor, or conversion to per cent inhibition.
Flow cytometry
Abs against rat antigens used for staining were all purchased from BD Biosciences: FITC-conjugated CD3 (clone G4.18); PE-conjugated CD25 (clone OX-39), CD45R (clone HIS24), CD45RC (clone OX-22); PerCP-conjugated CD8 (clone OX-8); PE-Cy5-conjugated CD45RA (OX-33); APC-conjugated CD3 (clone 1F4), CD4 (clone OX-35). Abs against human antigens used for staining were all purchased from BD Biosciences: PE-conjugated CD4 (clone RPA-T4), CCR7 (clone 150503); PerCP-conjugated CD4 (clone SK3), CD8 (Clone SK1); APC-conjugated CD25 (clone M-A251), CD45RO (clone UCHL1). FITC-conjugated Kv1.3 Ab was purchased from Sigma-Aldrich. Samples were acquired on a FACSCalibur flow cytometer using CellQuest Pro v5.1.1 software (BD Biosciences) and data analysis performed using FlowJo v6.4.2 software (Tree Star, Inc.). Cell sorting was performed on FACSAria to isolate purified populations of human naive (CCR7+CD45RO−), TCM (CCR7+CD45RO+) and TEM (CCR7−CD45RO+) CD4+ or CD8+ subsets. In some instances CD4+ and memory CD4+ T cells were purified using appropriate MACS cell isolation kits (Miltenyi Biotec). Purity of isolated cells was validated using flow cytometry and was >95% for all cell types. General gating strategy for CD4+ and CD8+ T cells is shown in Supplementary Fig. 6a.
Adjuvant-induced arthritis
Seven- to eight-week-old Kv1.3 KO and WT rats received a single injection of 100 μl complete Freund’s adjuvant at the base of the tail at 1 mg ml−1. Animals were monitored daily and visual scoring for each paw was assessed as follows: 0=no evidence of erythema and swelling; 1=erythema and mild swelling confined to the mid-foot (tarsal) or ankle; 2=erythema and mild swelling extending from the ankle to the mid-foot; 3=erythema and moderate swelling extending from the ankle to the metatarsal joints; 4=erythema and severe swelling encompass the ankle, foot and digits. Mean score=sum of the four paw scores. Disease stages: mild (mean score 1–3), moderate (mean score 4–8) and severe disease (mean score>9).
Delayed-type hypersensitivity response
Seven- to eight-week-old Kv1.3 KO and WT littermate rats were immunized at the base of the tail with 200 μl emulsion containing 100 μg TNP-OVA dissolved in 100 μl PBS mixed with 100 μl of CFA at 1 mg ml−1. On day 7, right pinna ear thickness was measured, and then challenged with injection of 25 μl PBS alone or TNP-OVA dissolved in PBS at 2 mg ml−1. On day 8, right pinna ears were again measured. Delta ear thickness is the thickness of post-challenge measurement subtracting pre-challenge measurement. For studies where treatment was administered, CTLA4-Fc or anti-ragweed was administered at 6 mg kg−1 in PBS delivered three times a week via intraperitoneal route starting on the day before immunization. The generation, production and purification of CTLA4-Fc and anti-ragweed antibodies used in this study has been described elsewhere49. ShK peptide was administered at 200 μg kg−1 on days 6 and 7, before challenge and during challenge, respectively. ShK was delivered in PBS via intravenous route.
RNA isolation and quantitative RT-PCR
For analysis of gene expression, RNA was isolated from cells using RNeasy Mini Kit (Qiagen). TaqMan real-time quantitative RT-PCR was performed using the ABI7500 Real-Time PCR system (Applied Biosystems). Rat TaqMan Gene Expression Assay primer/probe sets were from Applied Biosystems: Kcna3 (Rn00570552_s1), Kcnn4 (Rn00576373_m1), Kcna1 (Rn00597355_s1), Kcna2 (Rn02769834_s1), Kcna4 (Rn02532059_s1), Kcna5 (Rn00564245_s1), Kcna6 (Rn01492950_s1), Kcna7 (Rn01476090_m1), Ccr7 (Rn01465443_m1). Human TaqMan Gene Expression Assay primer/probe sets were from Applied Biosystems: KCNA3 (Kv1.3, Hs00704943_s1), KCNN4 (KCa3.1, Hs00158470_m1), KCNA1 (Kv1.1, Hs00264798_s1), KCNA2 (Kv1.2, Hs00270656_s1), KCNA4 (Kv1.4, Hs00937357_s1), KCNA5 (Kv1.5, Hs00266898), KCNA6 (Kv1.6, Hs00266903_s1), KCNA7 (Kv1.7, Hs00361015_m1), CCR7 (Hs01013469_m1). Mouse TaqMan Gene Expression Assay primer/probe sets were from Applied Biosystems: Kcna3 (Mm00434599_s1), Kcnn4 (Mm00464586_m1), Kcna1 (Mm00439977_s1), Kcna2 (Mm00434584_s1), Kcna4 (Mm00445241_s1), Kcna5 (Mm00524346_s1), Kcna6 (Mm00496625_s1), Kcna7 (Mm01197268_m1). Expression of ribosomal protein L19 was used to normalize copy number. Relative expression levels (fold differences) between groups were determined by ΔΔCt method.
Small interfering RNA knockdown
siRNA knockdown of Kv1.3 and KCa3.1 expression was performed using ON-TARGETplus SMARTpool siRNA (KCNA3, L-006213-00-0005; KCNN4, L-004461-00-0005; negative control pool, D-001810-10) from Thermo Scientific. Cell populations were transfected with siRNA (300 nM final concentration) using Human T-cell Nucleofector Kit (Amaxa) according to manufacturer’s recommended protocol.
Statistics
Statistical analyses were performed using JMP version 9.0.2 software (SAS Institute). We made comparisons for each pair with Student’s t-test, with P values <0.05 considered significant.
Data availability
The data that support the findings of this study are available from the corresponding author upon request.
Additional information
How to cite this article: Chiang, E. Y. et al. Potassium channels Kv1.3 and KCa3.1 cooperatively and compensatorily regulate antigen-specific memory T cell functions. Nat. Commun. 8, 14644 doi: 10.1038/ncomms14644 (2017).
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Cahalan, M. D. & Chandy, K. G. The functional network of ion channels in T lymphocytes. Immunol. Rev. 231, 59–87 (2009).
Wang, J. & Xiang, M. Targeting potassium channels Kv1.3 and KCa3.1: routes to selective immunomodulators in autoimmune disorder treatment? Pharmacotherapy 33, 515–528 (2013).
Feske, S., Wulff, H. & Skolnik, E. Y. Ion channels in innate and adaptive immunity. Annu. Rev. Immunol. 33, 291–353 (2015).
Feske, S., Skolnik, E. Y. & Prakriya, M. Ion channels and transporters in lymphocyte function and immunity. Nat. Rev. Immunol. 12, 532–547 (2012).
Rangaraju, S., Chi, V., Pennington, M. W. & Chandy, K. G. Kv1.3 potassium channels as a therapeutic target in multiple sclerosis. Expert. Opin. Ther. Targets 13, 909–924 (2009).
Wulff, H. & Pennington, M. Targeting effector memory T-cells with Kv1.3 blockers. Curr. Opin. Drug. Discov. Devel. 10, 438–445 (2007).
Beeton, C. & Chandy, K. G. Potassium channels, memory T cells, and multiple sclerosis. Neuroscientist 11, 550–562 (2005).
Panyi, G. Biophysical and pharmacological aspects of K+ channels in T lymphocytes. Eur. Biophys. J. 34, 515–529 (2005).
Chandy, K. G. et al. K+ channels as targets for specific immunomodulation. Trends. Pharmacol. Sci. 25, 280–289 (2004).
Chi, V. et al. Development of a sea anemone toxin as an immunomodulator for therapy of autoimmune diseases. Toxicon 59, 529–546 (2012).
Pennington, M. W. et al. Chemical synthesis and characterization of ShK toxin: a potent potassium channel inhibitor from sea anemone. Int. J. Pept. Protein. Res. 346, 354–358 (1995).
Beeton, C. et al. Targeting effector memory T cells with a selective peptide inhibitor of Kv1.3 channels for therapy of autoimmune diseases. Mol. Pharmacol. 67, 1369–1381 (2005).
Pennington, M. W. et al. Engineering a stable and selective peptide blocker of the Kv1.3 channel in T lymphocytes. Mol. Pharmacol. 75, 762–773 (2009).
Kalman, K. et al. ShK-Dap22, a potent Kv1.3-specific immunosuppressive polypeptide. J. Biol. Chem. 273, 32697–32707 (1998).
Beeton, C. et al. Kv1.3 channels are a therapeutic target for T cell-mediated autoimmune diseases. Proc. Natl Acad. Sci. USA 103, 17414–17419 (2006).
Wulff, H. et al. The voltage-gated Kv1.3 K+ channel in effector memory T cells as new target for MS. J. Clin. Invest. 111, 1703–1713 (2003).
Ghanshani, S. et al. Up-regulation of the IKCa1 potassium channel during T-cell activation: molecular mechanism and functional consequences. J. Biol. Chem. 275, 37137–37149 (2000).
Wulff, H. et al. Design of a potent and selective inhibitor of the intermediate-conductance Ca2+-activated K+ channel, IKCa1: a potential immunosuppressant. Proc. Natl Acad. Sci. USA 97, 8151–8156 (2000).
Li, Z. et al. Selective inhibition of CCR7- effector memory T cell activation by a novel peptide targeting Kv1.3 channel in a rat experimental autoimmune encephalomyelitis model. J. Biol. Chem. 287, 29479–29494 (2012).
Beeton, C. et al. Selective blockade of T lymphocyte K+ channels ameliorates experimental autoimmune encephalomyelitis, a model for multiple sclerosis. Proc. Natl Acad. Sci. USA 98, 13942–13947 (2001).
Matheu, M. P. et al. Imaging of effector memory T cells during a delayed-type hypersensitivity reaction and suppression by Kv1.3 channel block. Immunity 29, 602–614 (2008).
Azam, P., Sankaranarayanan, A., Homerick, D., Griffey, S. & Wulff, H. Targeting effector memory T cells with the small molecule Kv1.3 blocker PAP-1 suppresses allergic contact dermatitis. J. Invest. Dermatol. 127, 1419–1429 (2007).
Ueyama, A. et al. Kv1.3 blockers ameliorate allergic contact dermatitis by preferentially suppressing effector memory T cells in a rat model. Clin. Exp. Dermatol. 38, 897–903 (2013).
Koshy, S. et al. Blocking Kv1.3 channels inhibits Th2 lymphocyte function and treats a rat model of asthma. J. Biol. Chem. 289, 12623–12632 (2014).
Tarcha, E. J. et al. Durable pharmacological responses from the peptide ShK-186, a specific Kv1.3 channel inhibitor that suppresses T cell mediators of autoimmune disease. J. Pharmacol. Exp. Ther. 342, 642–653 (2012).
Schmitz, A. et al. Design of PAP-1, a selective small molecule Kv1.3 blocker, for the suppression of effector memory T cells in autoimmune diseases. Mol. Pharmacol. 68, 1254–1270 (2005).
Koni, P. A. et al. Compensatory anion currents in Kv1.3 channel-deficient thymocytes. J. Biol. Chem. 278, 39443–39451 (2003).
Xu, J. et al. The voltage-gated potassium channel Kv1.3 regulates energy homeostasis and body weight. Hum. Mol. Genet. 12, 551–559 (2003).
Pelegri, C., Morante, M. P., Castellote, C., Franch, A. & Castell, M. Treatment with an anti-CD4 monoclonal antibody strongly ameliorates established rat adjuvant arthritis. Clin. Exp. Immunol. 103, 273–278 (1996).
Kong, Y.-Y. et al. Activated T cells regulate bone loss and joint destruction in adjuvant arthritis through osteoprotegerin ligand. Nature 402, 304–309 (1999).
Hoffmann, J. C. et al. Initiation and perpetuation of rat adjuvant arthritis iis inhibited by the anti-CD2 monoclonal antibody (mAb) OX34. Ann. Rheum. Dis. 56, 716–722 (1997).
Szabo, S. J., Sullivan, B. M., Peng, S. L. & Glimcher, L. H. Molecular mechanisms regulating Th1 immune responses. Annu. Rev. Immunol. 21, 713–758 (2003).
Chhabra, S. et al. Kv1.3 channel-blocking immunomodulatory peptides from parasitic worms: implications for autoimmune diseases. FASEB J. 28, 3952–3964 (2014).
Beeton, C. et al. Selective blocking of voltage-gated K+ channels improves experimental autoimmune encephalomyelitis and inhibits T cell activation. J. Immunol. 166, 936–944 (2001).
Edwards, W. et al. Targeting the ion channel Kv1.3 with scorpion venom peptides engineered for potency, selectivity, and half-life. J. Biol. Chem. 289, 22704–22714 (2014).
Ohya, S. et al. Role of the KCa3.1 K+ channel in auricular lymph node CD4+ T-lymphocyte function of the delayed-type hypersensitivity model. Br. J. Pharmacol. 169, 1011–1023 (2013).
Chen, G. et al. Characterization of a novel CRAC inhibitor that potently blocks human T cell activation and effector functions. Mol. Immunol. 54, 355–367 (2013).
Bertin, S. et al. The ion channel TRPV1 regulates the activation and proinflammatory properties of CD4+ T cells. Nat. Immunol. 15, 1055–1063 (2014).
Meuth, S. G. et al. TWIK-related acid-sensitive K+ channel 1 (TASK1) and TASK3 critically influence T lymphocyte effector functions. J. Biol. Chem. 283, 14559–14570 (2008).
Ehling, P. et al. Human T cells in silico: modelling their electrophysiological behavior in health and disease. J. Theor. Biol. 404, 236–250 (2016).
Rus, H. et al. The voltage-gated potassium channel Kv1.3 is highly expressed on inflammatory infiltrates in multiple sclerosis brain. Proc. Natl Acad. Sci. USA 102, 11094–11099 (2005).
Vezys, V. et al. Memory CD8 T-cell compartment grows in size with immunological experience. Nature 457, 196–199 (2009).
Jameson, S. C. & Masopust, D. Diversity in T cell memory: an embarrassment of riches. Immunity 31, 859–871 (2009).
Rai, D., Martin, M. D. & Badovinac, V. P. The longevity of memory CD8 T cell responses after repetitive antigen stimulations. J. Immunol. 192, 5652–5659 (2014).
Martin, M. D. & Badovinac, V. P. Influence of time and number of antigen encounters on memory CD8 T cell development. Immunol. Res. 59, 35–44 (2014).
Wirth, T. C. et al. Repetitive antigen stimulation induces stepwise transcriptome diversification but preserves a core signature of memory CD8+ T cell differentiation. Immunity 33, 128–140 (2010).
Szigligeti, P. et al. Signaling during hypoxia in human T lymphocytes - critical role of the src protein tyrosine kinase p56Lck in the O2 sensitivity of Kv1.3 channels. J. Physiol. 573, 357–370 (2006).
Yang, J., James, E. A., Sanda, S., Greenbaum, C. & Kwok, W. W. CD4+ T cells recognized diverse epitopes within GAD65: implications for repertoire development and diabetes monitoring. Immunology 138, 269–279 (2012).
Chiang, E. Y. et al. Targeted depletion of lymphotoxin-alpha-expressing TH1 and TH17 cells inhibits autoimmune disease. Nat. Med. 15, 766–773 (2009).
Acknowledgements
We thank William W. Kwok from Benaroya Research Institute at Virginia Mason for expert technical assistance and valuable discussions regarding experimental design of human in vitro T cell assays.
Author information
Authors and Affiliations
Contributions
E.Y.C. designed and performed experiments, analysed the data and wrote the manuscript. T.L. performed electrophysiology experiments and J.C. contributed to assay development and trouble-shooting. S.J., I.P., J.D, J.Z, P.C. and W.P.L. designed and performed in vivo studies. S.W., in collaboration with SAGE Labs, contributed to generation of Kcna3−/− rats. D.H.H., S.M. and C.M.K. contributed to evaluation of channel inhibitors and editing of the manuscript. J.L.G. conceived and supervised the project, analysed the data and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they are employees of Genentech, a member of the Roche group, which develops and markets drugs for profit.
Supplementary information
Supplementary Information
Supplementary Figures 1-9 (PDF 1833 kb)
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Chiang, E., Li, T., Jeet, S. et al. Potassium channels Kv1.3 and KCa3.1 cooperatively and compensatorily regulate antigen-specific memory T cell functions. Nat Commun 8, 14644 (2017). https://doi.org/10.1038/ncomms14644
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/ncomms14644
This article is cited by
-
Structures of the T cell potassium channel Kv1.3 with immunoglobulin modulators
Nature Communications (2022)
-
Higher expression of KCNK10 (TREK-2) K+ channels and their functional upregulation by lipopolysaccharide treatment in mouse peritoneal B1a cells
Pflügers Archiv - European Journal of Physiology (2021)
-
The Kv1.3 K+ channel in the immune system and its “precision pharmacology” using peptide toxins
Biologia Futura (2021)
-
NLRP3-dependent pyroptosis is required for HIV-1 gp120-induced neuropathology
Cellular & Molecular Immunology (2020)
-
Immunosuppressive effects of a novel potassium channel toxin Ktx-Sp2 from Scorpiops Pocoki
Cell & Bioscience (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.