Abstract
Refined cancer models are needed to bridge the gaps between cell line, animal and clinical research. Here we describe the engineering of an organotypic colon cancer model by recellularization of a native human matrix that contains cell-populated mucosa and an intact muscularis mucosa layer. This ex vivo system recapitulates the pathophysiological progression from APC-mutant neoplasia to submucosal invasive tumor. We used it to perform a Sleeping Beauty transposon mutagenesis screen to identify genes that cooperate with mutant APC in driving invasive neoplasia. We identified 38 candidate invasion-driver genes, 17 of which, including TCF7L2, TWIST2, MSH2, DCC, EPHB1 and EPHB2 have been previously implicated in colorectal cancer progression. Six invasion-driver genes that have not, to our knowledge, been previously described were validated in vitro using cell proliferation, migration and invasion assays and ex vivo using recellularized human colon. These results demonstrate the utility of our organoid model for studying cancer biology.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Accession codes
References
Arrowsmith, J. Trial watch: Phase II failures: 2008–2010. Nat. Rev. Drug Discov. 10, 328–329 (2011).
Gout, S. & Huot, J. Role of cancer microenvironment in metastasis: focus on colon cancer. Cancer Microenviron. 1, 69–83 (2008).
Bozic, I. et al. Accumulation of driver and passenger mutations during tumor progression. Proc. Natl. Acad. Sci. USA 107, 18545–18550 (2010).
Jones, S. et al. Comparative lesion sequencing provides insights into tumor evolution. Proc. Natl. Acad. Sci. USA 105, 4283–4288 (2008).
The Cancer Genome Atlas Network. Comprehensive molecular characterization of human colon and rectal cancer. Nature 487, 330–337 (2012).
Copeland, N.G. & Jenkins, N.A. Deciphering the genetic landscape of cancer—from genes to pathways. Trends Genet. 25, 455–462 (2009).
Li, X. et al. Oncogenic transformation of diverse gastrointestinal tissues in primary organoid culture. Nat. Med. 20, 769–777 (2014).
Matano, M. et al. Modeling colorectal cancer using CRISPR-Cas9–mediated engineering of human intestinal organoids. Nat. Med. 21, 256–262 (2015).
Jung, P. et al. Isolation and in vitro expansion of human colonic stem cells. Nat. Med. 17, 1225–1227 (2011).
Gilbert, T.W., Sellaro, T.L. & Badylak, S.F. Decellularization of tissues and organs. Biomaterials 27, 3675–3683 (2006).
Ott, H.C. et al. Regeneration and orthotopic transplantation of a bioartificial lung. Nat. Med. 16, 927–933 (2010).
Ott, H.C. et al. Perfusion-decellularized matrix: using nature's platform to engineer a bioartificial heart. Nat. Med. 14, 213–221 (2008).
Ridky, T.W., Chow, J.M., Wong, D.J. & Khavari, P.A. Invasive three-dimensional organotypic neoplasia from multiple normal human epithelia. Nat. Med. 16, 1450–1455 (2010).
Tuveson, D.A. et al. Endogenous oncogenic KrasG12D stimulates proliferation and widespread neoplastic and developmental defects. Cancer Cell 5, 375–387 (2004).
Biswas, S. et al. Transforming growth factor-β receptor type II inactivation promotes the establishment and progression of colon cancer. Cancer Res. 64, 4687–4692 (2004).
Trobridge, P. et al. TGF-β receptor inactivation and mutant Kras induce intestinal neoplasms in mice via a β-catenin-independent pathway. Gastroenterology 136, 1680–1688.e7 (2009).
Lohi, J. et al. Laminins, tenascin and type VII collagen in colorectal mucosa. Histochem. J. 28, 431–440 (1996).
Vermeulen, L. et al. Single-cell cloning of colon cancer stem cells reveals a multi-lineage differentiation capacity. Proc. Natl. Acad. Sci. USA 105, 13427–13432 (2008).
Liotta, L.A. Tumor invasion and metastases: role of the basement membrane. Warner-Lambert Parke-Davis Award lecture. Am. J. Pathol. 117, 339–348 (1984).
Lau, W., Barker, N. & Clevers, H. WNT signaling in the normal intestine and colorectal cancer. Front. Biosci. 12, 471–491 (2007).
Fearon, E.R. & Vogelstein, B. A genetic model for colorectal tumorigenesis. Cell 61, 759–767 (1990).
Wood, L.D. et al. The genomic landscapes of human breast and colorectal cancers. Science 318, 1108–1113 (2007).
Oshima, H. et al. Suppressing TGFβ signaling in regenerating epithelia in an inflammatory microenvironment is sufficient to cause invasive intestinal cancer. Cancer Res. 75, 766–776 (2015).
Copeland, N.G. & Jenkins, N.A. Harnessing transposons for cancer gene discovery. Nat. Rev. Cancer 10, 696–706 (2010).
Dupuy, A.J., Akagi, K., Largaespada, D.A., Copeland, N.G. & Jenkins, N.A. Mammalian mutagenesis using a highly mobile somatic Sleeping Beauty transposon system. Nature 436, 221–226 (2005).
March, H.N. et al. Insertional mutagenesis identifies multiple networks of cooperating genes driving intestinal tumorigenesis. Nat. Genet. 43, 1202–1209 (2011).
Takeda, H. et al. Transposon mutagenesis identifies genes and evolutionary forces driving gastrointestinal tract tumor progression. Nat. Genet. 47, 142–150 (2015).
Grabundzija, I. et al. Comparative analysis of transposable element vector systems in human cells. Mol. Ther. 18, 1200–1209 (2010).
Brett, B.T. et al. Novel molecular and computational methods improve the accuracy of insertion site analysis in Sleeping Beauty-induced tumors. PLoS One 6, e24668 (2011).
Angus-Hill, M.L., Elbert, K.M., Hidalgo, J. & Capecchi, M.R. T-cell factor 4 functions as a tumor suppressor whose disruption modulates colon cell proliferation and tumorigenesis. Proc. Natl. Acad. Sci. USA 108, 4914–4919 (2011).
Behrens, J. et al. Functional interaction of an axin homolog, conductin, with β-catenin, APC, and GSK3β. Science 280, 596–599 (1998).
Yu, H. et al. Twist2 is a valuable prognostic biomarker for colorectal cancer. World J. Gastroenterol. 19, 2404–2411 (2013).
Xiong, H. et al. Inhibition of JAK1, 2/STAT3 signaling induces apoptosis, cell cycle arrest, and reduces tumor cell invasion in colorectal cancer cells. Neoplasia 10, 287–297 (2008).
Forcet, C. et al. The dependence receptor DCC (deleted in colorectal cancer) defines an alternative mechanism for caspase activation. Proc. Natl. Acad. Sci. USA 98, 3416–3421 (2001).
Aylon, Y. et al. A positive feedback loop between the p53 and Lats2 tumor suppressors prevents tetraploidization. Genes Dev. 20, 2687–2700 (2006).
Yabuta, N. et al. Structure, expression, and chromosome mapping of LATS2, a mammalian homologue of the Drosophila tumor suppressor gene lats/warts. Genomics 63, 263–270 (2000).
Funato, K., Yamazumi, Y., Oda, T. & Akiyama, T. Tyrosine phosphatase PTPRD suppresses colon cancer cell migration in coordination with CD44. Exp. Ther. Med. 2, 457–463 (2011).
Chen, H.J. et al. Comprehensive models of human primary and metastatic colorectal tumors in immunodeficient and immunocompetent mice by chemokine targeting. Nat. Biotechnol. 33, 656–660 (2015).
Katoh, M. Functional and cancer genomics of ASXL family members. Br. J. Cancer 109, 299–306 (2013).
Williams, D.S. et al. Nonsense mediated decay resistant mutations are a source of expressed mutant proteins in colon cancer cell lines with microsatellite instability. PLoS One 5, e16012 (2010).
Henrich, K.O. et al. CAMTA1, a 1p36 tumor suppressor candidate, inhibits growth and activates differentiation programs in neuroblastoma cells. Cancer Res. 71, 3142–3151 (2011).
Kim, M.Y. et al. Recurrent genomic alterations with impact on survival in colorectal cancer identified by genome-wide array comparative genomic hybridization. Gastroenterology 131, 1913–1924 (2006).
Roig, A.I. et al. Immortalized epithelial cells derived from human colon biopsies express stem cell markers and differentiate in vitro. Gastroenterology 138, 1012–1021 (2010).
Gomes, C.C. et al. Assessment of TP53 mutations in benign and malignant salivary gland neoplasms. PLoS One 7, e41261 (2012).
Groden, J. et al. Identification and characterization of the familial adenomatous polyposis coli gene. Cell 66, 589–600 (1991).
Lièvre, A. et al. KRAS mutation status is predictive of response to cetuximab therapy in colorectal cancer. Cancer Res. 66, 3992–3995 (2006).
Ruiz-Ponte, C., Vega, A., Carracedo, A. & Barros, F. Mutation analysis of the adenomatous polyposis coli (APC) gene in northwest Spanish patients with familial adenomatous polyposis (FAP) and sporadic colorectal cancer. Hum. Mutat. 18, 355 (2001).
Maston, G.A., Evans, S.K. & Green, M.R. Transcriptional regulatory elements in the human genome. Annu. Rev. Genomics Hum. Genet. 7, 29–59 (2006).
Chen, H.J. et al. Chemokine 25-induced signaling suppresses colon cancer invasion and metastasis. J. Clin. Invest. 122, 3184–3196 (2012).
Acknowledgements
We thank the members of M.L.S.'s laboratory and N.A.J. and N.G.C.'s laboratory. We also thank H.E. Varmus for providing laboratory resources and helpful discussions. This work was supported by a US National Cancer Institute Physical Sciences-Oncology Center (NCI-PSOC) Young Investigator trans-network grant to H.J.C. and Z.W., US National Institutes of Health (NIH) grant UH2TR000516 to M.L.S., US National Science Foundation (NSF) grants NSF-1106153 to M.L.S. and NSF GRFP-2011131053 to H.J.C., NIH grant R01GM095990 to X.S., an Arnold O. Beckman Postdoctoral fellowship to H.J.C., a Welch Foundation grant C-0627 at Rice University to Y.M. and the Cancer Prevention Research Institute of Texas (CPRIT) (N.G.C. and N.A.J.).
Author information
Authors and Affiliations
Contributions
H.J.C., Z.W., R.S., N.G.C., N.A.J. and M.L.S. conceived the concept, designed the experiments and wrote the manuscript; H.J.C., Z.W., A.B., D.J.S., P.B., L.W., Y. M., S.A.C., S.C., E.H. and L.C.-G. performed the experiments and data analyses; J.S., Z.W., S.M.L., X.S., N.G.C. and N.A.J. contributed to bioinformatics analyses.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Integrated supplementary information
Supplementary Figure 1 Generation and characterization of primary human colonic epithelial cells (hCECs).
(A) Representative images of hCECs grown in 2D cultures or matrigel 3D cultures. In matrigel cultures, individual hCECs progressively formed organiod-like structures (left to right). Scale bars, 100µ (left panel) and 50µ (right panel) in 2D culture; 100µ in 3D culture. White arrows denote micro-crypt domains formed with the multicellular cyst-like structure, which is the typical behavior of physiologically active intestinal stem cells grown in 3D (B) Cells expressing the stem cell marker Lgr5, epithelial markers cytokeratin 18 and 20, tight junction protein zonula occludens-1 (ZO-1) in condition of co-culture with colonic fibroblasts, colon epithelial cell-specific marker A33, and differentiation markers villin (absorptive cells), mucin 2 (goblet cells) and chromogranin A (enteroendocrine cells), were detected by immunostaining of hCECs in 2D culture. Scale bars, 50µ; blue nuclei, DAPI. (C) Quantification of Lgr5+ cells and functionally differentiated cells in hCECs. Error bars indicate S.E.M. n= 3 independent cultures.
Supplementary Figure 2 The procedure of recellularization.
The acellular colon matrix was physically separated into (A) mucosal (20x and 40x in big and small windows, respectively) and (B) submucosal layers. White arrow highlights intact epithelial crypt niches in the mucosal layer. Scale bars, 1mm. (C) Endothelial cells are shown being loaded into an injection needle and (D) being injected into the mucosa layer. Scale bars, 200 µ. The acellular colon matrix (E) was populated with colonic epithelial cells, endothelial cells and myofibroblasts. (F) A colon after recellularization for 6 weeks. Scale bars, 2 mm. (See Supplementary Video 1, 2 and 3 for detailed procedures.)
Supplementary Figure 3 Characterization of human colonic myofibroblasts and microvascular endothelial cells.
(A) Primary cultured colonic myofibroblasts in light microscope (left) or immunostained with anti-human α smooth muscle actin (right). Scale bars, 100µ (left) and 20µ (right). Purple nuclei, DAPI; More than 90% cells were positively stained with α smooth muscle actin; (B) colonic microvascular endothelial cells in light microscope (left) or immunostained with anti- human CD31 (right). Scale bars, 100 µ (left) and 20 µ (right). Blue nuclei, DAPI. More than 90% cells were positively stained with CD31. n= 3 independent cultures.
Supplementary Figure 4 Electron microscopic characterization of ex vivo colon mucosa.
(A) Scanning electron micrographs of mucosa surface, lamina propria and muscularis mucosa show that crypt niches were retained and intestinal fibers were well preserved in composition and ultrastructure during the de-/re-cellularization process. White arrows denote crypt niches; characteristic weaves (W), coils (C) and struts (S) of colonic fibers of laminin and collagen are present in both decellularized and recellularized matrices. Scale bars, 20 µM. (B) Transmission electron micrographs reveal the continuous intactness of muscularis mucosa (MM) layers in both decellularized matrix and recellularized tissue. |<->| designates the location and thickness of MM layers that were repopulated with fibroblasts (<-) in recellularized colon. Features: collagen fibers (\/); lamina filaments (<-). M, mucosa area; SM, submucosal area; scale bars, 500 nM (300 nM in small windows). All of the recellularized tissues have been cultured for 6-7 weeks when they are processed for electron microscopy. (C) No statistical differences in MM thickness were observed among native, recellularized and recellularized colon tissues. Error bars indicate S.E.M. (n= 6 of independent matrix; difference analysis by one-way ANOVA).
Supplementary Figure 5 Molecular characterization of physiologically active crypts recellularized with hCECs.
Immunostaining of the recellularized crypts showed that they contain cells (yellow denoted by white arrows) double positive for the intestinal stem cell marker Lgr5 (red) and proliferative marker Ki67 (green) (top panel) in addition to differentiated colon epithelial cells (Muc1 positive cells, transit amplifying cells), goblet cells (Muc2 positive cells), and enteroendocrine cells (chromogranin A-positive cells) (bottom panels). All the recellularized tissues had been cultured for 4 weeks before they were terminated from culture and prepared for immunostaining. Blue nuclei, DAPI; Scale bars, 20 µM. n= 3 independent cultures.
Supplementary Figure 6 Molecular characterization of recellularized mucosa.
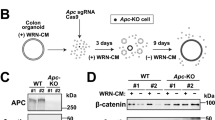
(A) WNT/β-catenin signaling was restored in recellularized mucosa, detected by immunostaining of β-catenin (green). (B) Immunostaining of proliferative marker Ki67 (yellow) revealed the growth dynamic patterns of recellularized crypts. Blue nuclei, DAPI; scale bars, 20 µM. (C) ELISA experiments were performed to measure MUC2 protein levels. Substantially higher MUC2 levels were observed in the culture medium of recellularized colon compared with those in the medium of hCEC cells or decellularized colon matrices alone (student-t test), indicating the recellularized colon’s physiological function of mucous secretion. All of the recellularized tissues or hCEC cells had been cultured for 4 weeks before they were terminated from culture and prepared for immunostaining or MUC2 quantification. n = 5 independent matrices.
Supplementary Figure 7 Quantification of APC and KRASG12D expression in hCECs.
The psi-LVRH1GP (CMV-H1-APC shRNA-SV40-KRASG12D - neomycin) lentivirus, containing both an APC shRNA and a human KRASG12D expression construct, was transduced into hCEC cells. Protein expression levels of APC and a Myc-DDK tag for KRASG12D in hCEC cells were quantified by Western blotting (+). hCEC cells transduced with the backbone vector served used the control (-). β-actin is loading control.
Supplementary Figure 8 Tumor formation in mice injected with APC-KRASG12D hCECs.
2x106 matrigel-embedded parental or APC-KRASG12D hCECs were subcutaneously injected into each flank of 6-8 week old NSG mice (NOD/Shi-scid/IL-2Rγnull mice). The TGF-β signaling pathway was then blocked through the intraperitoneal injection of a TGF-β receptor inhibitor (TGF-β RI Inhibitor III), beginning at two weeks after injection (100mg/kg) with continuing injections three times per week. Six weeks after injection of APC-KRASG12D hCECs, tumor nodules (>250mm3) were visible at 60-80% of the injection sites, while injection of parental hCECs did not induce any tumors. (A) A representative tumor is shown following H+E staining. Scale bars, 100µ. (B) Quantification of tumor formation following injection of APC-KRASG12D hCECs and parental hCECs. ** P=0.0002, comparison in tumor formation by Fisher’s exact test.
Supplementary Figure 9 Creation of a modified SB transposition system for use in human tissues.
(A) Transposition activity was quantified using a fixed dose of transposon-donor plasmid (500 ng T2/Onc1) and varying doses of SB100X transposase plasmid; error bars indicate S.E.M. The activity of transposase reached its peak at a dose of 100ng. n = 5 independent experiments. (B) Average transposon copy numbers in individual hCEC colonies.
Supplementary Figure 10 Functional validation of ten candidate invasion-driver genes using the ex vivo human colon model.
shRNAs against 10 candidate driver genes that were functionally validated in in vitro cell proliferation, invasion and migration assays were used to downregulated expression of these genes in APC shRNA-expressing hCECs. These cells where then used to recellularize acellular colon matrices and the effects of this downregulated expression on neoplastic cell invasion measured (n= 4). Seven candidate genes, including LATS2, significantly promoted submucosa invasion in the ex vivo human colon model (A) Representative H+E-stained image (left panel) and dual immunostained image of cytokeratin and fibronectin (right panel) from an ex vivo colon recellularized with hCECs expressing shRNA against APC and CAMTA1. Scale bars, 100µ in left panel and 20µ in right panel. (B). Quantification of invasive neoplasia formation in ex vivo CRC models. *P<0.05 compared to APC shRNA-expressing hCECs transfected with control vector by 2-sided student t test. All of the recellularized tissues had been cultured for 7 weeks when they were terminated for quantification of tumorigenesis. n = 3 independent matrices.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–10, Supplementary Tables 1–3 and Supplementary Methods (PDF 2273 kb)
Rights and permissions
About this article
Cite this article
Chen, H., Wei, Z., Sun, J. et al. A recellularized human colon model identifies cancer driver genes. Nat Biotechnol 34, 845–851 (2016). https://doi.org/10.1038/nbt.3586
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nbt.3586
This article is cited by
-
An injectable subcutaneous colon-specific immune niche for the treatment of ulcerative colitis
Nature Biomedical Engineering (2023)
-
Building gut from scratch — progress and update of intestinal tissue engineering
Nature Reviews Gastroenterology & Hepatology (2022)
-
Cancer cell survival depends on collagen uptake into tumor-associated stroma
Nature Communications (2022)
-
Decellularized normal and cancer tissues as tools for cancer research
Cancer Gene Therapy (2022)
-
Transcriptomic analysis of tumor tissues and organoids reveals the crucial genes regulating the proliferation of lung adenocarcinoma
Journal of Translational Medicine (2021)