Abstract
The self-organized dynamics of vortex-like rotating waves, which are also known as scroll waves, are the basis of the formation of complex spatiotemporal patterns in many excitable chemical and biological systems1,2,3,4. In the heart, filament-like phase singularities5,6 that are associated with three-dimensional scroll waves7 are considered to be the organizing centres of life-threatening cardiac arrhythmias7,8,9,10,11,12,13. The mechanisms that underlie the onset, maintenance and control14,15,16 of electromechanical turbulence in the heart are inherently three-dimensional phenomena. However, it has not previously been possible to visualize the three-dimensional spatiotemporal dynamics of scroll waves inside cardiac tissues. Here we show that three-dimensional mechanical scroll waves and filament-like phase singularities can be observed deep inside the contracting heart wall using high-resolution four-dimensional ultrasound-based strain imaging. We found that mechanical phase singularities co-exist with electrical phase singularities during cardiac fibrillation. We investigated the dynamics of electrical and mechanical phase singularities by simultaneously measuring the membrane potential, intracellular calcium concentration and mechanical contractions of the heart. We show that cardiac fibrillation can be characterized using the three-dimensional spatiotemporal dynamics of mechanical phase singularities, which arise inside the fibrillating contracting ventricular wall. We demonstrate that electrical and mechanical phase singularities show complex interactions and we characterize their dynamics in terms of trajectories, topological charge and lifetime. We anticipate that our findings will provide novel perspectives for non-invasive diagnostic imaging and therapeutic applications.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Welsh, B. J., Gomatam, J. & Burgess, A. E. Three-dimensional chemical waves in the Belousov–Zhabotinskii reaction. Nature 304, 611–614 (1983)
Rotermund, H. H., Engel, W., Kordesch, M. & Ertl, G. Imaging of spatio-temporal pattern evolution during carbon monoxide oxidation on platinum. Nature 343, 355–357 (1990)
Huang, X. et al. Spiral waves in disinhibited mammalian neocortex. J. Neurosci. 24, 9897–9902 (2004)
Winfree, A. T. Scroll-shaped waves of chemical activity in three dimensions. Science 181, 937–939 (1973)
Fenton, F. & Karma, A. Vortex dynamics in three-dimensional continuous myocardium with fiber rotation: filament instability and fibrillation. Chaos 8, 20–47 (1998)
Clayton, R. H., Zhuchkova, E. A. & Panfilov, A. V. Phase singularities and filaments: simplifying complexity in computational models of ventricular fibrillation. Prog. Biophys. Mol. Biol. 90, 378–398 (2006)
Winfree, A. T. Electrical turbulence in three-dimensional heart muscle. Science 266, 1003–1006 (1994)
Krinsky, V. I. Spread of excitation in an inhomogeneous medium (state similar to cardiac fibrillation). Biofizika 11, 676–683 (1966)
Davidenko, J. M., Pertsov, A. V., Salomonsz, R., Baxter, W. & Jalife, J. Stationary and drifting spiral waves of excitation in isolated cardiac muscle. Nature 355, 349–351 (1992)
Gray, R. A. et al. Mechanisms of cardiac fibrillation. Science 270, 1222–1223 (1995)
Jalife, J. & Gray, R. Drifting vortices of electrical waves underlie ventricular fibrillation in the rabbit heart. Acta Physiol. Scand. 157, 123–132 (1996)
Gray, R. A., Pertsov, A. M. & Jalife, J. Spatial and temporal organization during cardiac fibrillation. Nature 392, 75–78 (1998)
Witkowski, F. X. et al. Spatiotemporal evolution of ventricular fibrillation. Nature 392, 78–82 (1998)
Fenton, F. H. et al. Termination of atrial fibrillation using pulsed low-energy far-field stimulation. Circulation 120, 467–476 (2009)
Luther, S. et al. Low-energy control of electrical turbulence in the heart. Nature 475, 235–239 (2011)
Janardhan, A. H. et al. A novel low-energy electrotherapy that terminates ventricular tachycardia with lower energy than a biphasic shock when antitachycardia pacing fails. J. Am. Coll. Cardiol. 60, 2393–2398 (2012)
Mitrea, B. G., Caldwell, B. J. & Pertsov, A. M. Imaging electrical excitation inside the myocardial wall. Biomed. Opt. Express 2, 620–633 (2011)
Mitrea, B. G., Wellner, M. & Pertsov, A. M. Monitoring intramyocardial reentry using alternating transillumination. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2009, 4194–4197 (2009)
Baxter, W. T., Mironov, S. F., Zaitsev, A. V., Jalife, J. & Pertsov, A. M. Visualizing excitation waves inside cardiac muscle using transillumination. Biophys. J. 80, 516–530 (2001)
Wiggers, C. J. The mechanism and nature of ventricular fibrillation. Am. Heart J. 20, 399–412 (1940)
Svrcek, M., Rutherford, S., Chen, A. Y. H., Provaznik, I. & Smaill, B. Characteristics of motion artifacts in cardiac optical mapping studies. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2009, 3240–3243 (2009)
Rohde, G. K., Dawant, B. M. & Lin, S. F. Correction of motion artifact in cardiac optical mapping using image registration. IEEE Trans. Biomed. Eng. 52, 338–341 (2005)
Seo, K. et al. Structural heterogeneity in the ventricular wall plays a significant role in the initiation of stretch-induced arrhythmias in perfused rabbit right ventricular tissues and whole heart preparations. Circ. Res. 106, 176–184 (2010)
Bourgeois, E. B., Bachtel, A. D., Rogers, J. M., Huang, J. & Walcott, G. P. Simultaneous optical mapping of transmembrane potential and wall motion in isolated, perfused whole hearts. J. Biomed. Opt. 16, 096020 (2011)
Zhang, H., Iijima, K., Huang, J., Walcott, G. P. & Rogers, J. M. Optical mapping of membrane potential and epicardial deformation in beating hearts. Biophys. J. 111, 438–451 (2016)
Christoph, J., Schröder-Schetelig, J. & Luther, S. Electromechanical optical mapping. Prog. Biophys. Mol. Biol. 130, 150–169 (2017)
Provost, J., Lee, W.-N., Fujikura, K. & Konofagou, E. E. Imaging the electromechanical activity of the heart in vivo. Proc. Natl Acad. Sci. USA 108, 8565–8570 (2011)
Bers, D. M. Cardiac excitation–contraction coupling. Nature 415, 198–205 (2002)
Lee, P. et al. Simultaneous measurement and modulation of multiple physiological parameters in the isolated heart using optical techniques. Pflugers Arch. 464, 403–414 (2012)
Periaswamy, S., et al. H. Differential affine motion estimation for medical image registration. In Proc. SPIE 4119 Wavelet Applications in Signal and Image Processing VIII https://doi.org/10.1117/12.408594 (2000)
Jakubowski, M. & Pastuszak, S. Block-based motion estimation algorithms — a survey. Opto. Electron. Rev. 21, 86–102 (2013)
Christoph, J. Intramural Visualization of Scroll Waves in the Heart. PhD thesis, Univ. Göttingen (2015)
Huang, Y.-W., Chen, C.-Y., Tsai, C.-H., Shen, C.-F. & Chen, L.-G. Survey on block-matching motion estimation algorithms and architectures with new results. J. VLSI Signal Process. 42, 297–320 (2006)
Pathmanathan, P. & Gray, R. A. Filament dynamics during simulated ventricular fibrillation in a high-resolution rabbit heart. BioMed Res. Int. 2015, 720575 (2015)
Nash, M. P. & Panfilov, A. V. Electromechanical model of excitable tissue to study reentrant cardiac arrhythmias. Prog. Biophys. Mol. Biol. 85, 501–522 (2004)
Panfilov, A. V., Keldermann, R. H. & Nash, M. P. Drift and breakup of spiral waves in reaction–diffusion–mechanics systems. Proc. Natl Acad. Sci. USA 104, 7922–7926 (2007)
Aliev, R. R. & Panfilov, A. V. A simple two-variable model of cardiac excitation. Chaos Solitons Fractals 7, 293–301 (1996)
Bourguignon, D. & Cani, M.-P. in Computer Animation and Simulation (eds Magnenat-Thalmann, N. et al.) 113–123 (Springer, 2000)
Weise, L. D., Nash, M. P. & Panfilov, A. V. A discrete model to study reaction–diffusion–mechanics systems. PLoS ONE 6, e21934 (2011)
Quintanilla, J. G. et al. KATP channel opening accelerates and stabilizes rotors in a swine heart model of ventricular fibrillation. Cardiovasc. Res. 99, 576–585 (2013)
Omichi, C., et al. Intracellular Ca dynamics in ventricular fibrillation. Am. J. Physiol. Heart Circ. Physiol. 286, H1836–H1844 (2004)
Warren, M., Huizar, J. F., Shvedko, A. G., Zaitsev, A. V. Spatiotemporal relationship between intracellular Ca2+ dynamics and wave fragmentation during ventricular fibrillation in isolated blood-perfused pig hearts. Circ. Res. 101, e90–e101 (2007)
Weiss, J. N., Garfinkel, A., Karagueuzian, H. S., Chen, P. S. & Qu, Z. Early afterdepolarizations and cardiac arrhythmias. Heart Rhythm 7, 1891–1899 (2010)
Wang, L., et al. Optical mapping of sarcoplasmic reticulum Ca2+ in the intact heart: ryanodine receptor refractoriness during alternans and fibrillation. Circ. Res. 122, 1410–1421 (2014)
Acknowledgements
We thank U. Parlitz and N. Otani for discussions, M. Kunze, D. Hornung and U. Schminke for technical assistance, L. Bess for linguistic advice and FujiFilm VisualSonics Inc. and Siemens HealthCare for their technical support. This work was supported by the German Ministry for Education and Research through FKZ 031A147 (S.L.); by the German Center for Cardiovascular Research (S.L. and G.H.); by the German Research Foundation through SFB 1002 Modulatory Units in Heart Failure (S.L., J.C. and G.H.) and SFB 937 Collective Behavior of Soft and Biological Matter (S.L. and J.C.); by the National Science Foundation (NSF) grants 1341190 and 1413037 (F.H.F.); by the American Heart Association (AHA) grant 15POST25700285 (I.U.); by the Human Frontiers Science Program through fellowship LT000840/2014-C (P.B.) and by the Max Planck Society.
Author information
Authors and Affiliations
Contributions
J.C. and S.L. designed research and wrote the paper with F.H.F., G.H., P.B. and R.F.G.; J.C., S.L. and J.S.-S. designed the experiments; I.U. and F.H.F. contributed to the experimental setup; J.C. performed the experiments and analysed the data; M.C., J.S.-S., C.R., I.U. and F.H.F. contributed to the experiments; J.C., P.B. and S.S. provided the numerical simulations. All authors read and approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
J.C. and S.L. are registered as inventors of patent application PCT/EP2015/077001.
Additional information
Reviewer Information thanks A. Holden, J. Jalife, E. Konofagou and the other anonymous reviewer(s) for their contribution to the peer review of this work.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Extended Data Figure 1 Electromechanical vortex filament dynamics during cardiac fibrillation.
a, 3D volumetric ultrasound speckle image showing a contracting isolated pig heart during ventricular tachycardia (same heart as shown in Fig. 1a, b, lateral imaging depth 6 cm). Mechanical filament (red) measured within ventricular wall (white region of interest; see also Fig. 1) between left and right ventricle. b, Validation of ultrasound measurement of mechanical filaments on the epicardium using optical mapping (voltage) confirms co-localized electrical and mechanical phase singularities corresponding to two counter-rotating spiral waves (see also Fig. 1a). c, Breakthrough of an U-shaped intramural mechanical filament (red) on the epicardial surface of a pig heart results in the formation of two transmural filaments during ventricular fibrillation and two phase singularities (green circles) with opposite charge (counter rotation spirals) on the surface (see also Fig. 2a). Optical mapping (voltage and strain rate) confirms filament dynamics observed with 4D ultrasound.
Extended Data Figure 2 3D Imaging of electromechanical activity in the heart using simultaneous ultrasound and fluorescence imaging.
a–f, Reconstruction of the heart shape during simultaneous imaging of electromechanical cardiac activity using ultrasound imaging and panoramic optical mapping. a, Photograph of heart in the Langendorff setup with ultrasound transducer at the bottom of the bath. LA, left atrium. b, 3D optical reconstruction of the surface of the heart obtained by rotating the heart after the experiment. Photorealistic rendering of the surface of the heart on reconstructed 3D surface mesh. c, Rendering (transparent) of 3D volumetric ultrasound speckle data showing the contracting heart from a similar perspective. Fan indicates lateral imaging depth of approximately 6–8 cm that was used for high-speed imaging. d, Optical mapping video images showing a bipolar electrode touching the epicardium of the left ventricle. The electrode is bend at the top, such that the tip is perpendicular to the electrode (only the tip touches the epicardium). The approximate location of the tip is indicated by the white rectangles in a–d, g, i. The 3D reconstruction allows the determination of the position of the electrode’s tip on the heart surface from the two video images. e, Optical calibration target used for optical 3D reconstruction of heart surface. f, Acoustic calibration target for ultrasound imaging used to determine approximate alignment and position of transducer. The inset shows the corresponding ultrasound speckle image of the calibration target at a particular depth. g–j, Focal electromechanical activity in a contracting pig heart mapped with optical mapping and ultrasound during pacing. g, Photorealistic rendering of optically reconstructed heart. The heart is rotated towards the left compared to a, b. h, Action potential wave propagating outwards (green arrows) from stimulation (voltage-sensitive mapping using Di-4-ANNEPS, black–white colour code: dark corresponds to depolarizing tissue or the upstroke of the action potential). i, 3D ultrasound speckle movie data showing same part of the heart (opaque and transparent rendering). j, Elastomechanical activation computed from 3D motion of the tissue acquired with ultrasound. The tissue starts to contract first at the stimulation site. The strain rate and its phase representation pattern exhibit a focal point that coincides with the stimulation site and the focal point that is visible in the optical maps. a–d, g, i, The region in which electrical pacing (stimulation) was applied to the heart is indicated with a rectangle.
Extended Data Figure 3 Volumetric and cross-sectional ultrasound imaging and imaging configurations during ex vivo and in vivo imaging.
a, Isolated pig heart in imaging setup with 4D volumetric ultrasound transducer scanning from beneath the heart through an acoustic window, together with simultaneous panoramic fluorescence imaging (Fig. 1). 4D ultrasound imaging (Acuson sc2000, Siemens AG) was performed using a two-dimensional matrix phased-array transducer (4Z1c) producing volume frames with a pyramidal shape (51–188 volumes per second, maximum opening angle 90 × 90 degrees, 6–14 cm lateral depth). The heart is aligned very similarly within the pyramid-shaped field of view as in an examination of a patient in vivo. b, Isolated rabbit heart in imaging setup with 2D cross-sectional ultrasound transducer scanning from above, together with simultaneous single-camera fluorescence imaging (see also d and Supplementary Video 9). c, Imaging configuration during 4D ultrasound imaging and panoramic multi-camera optical mapping with four cameras (see also a). The optical axis of the cameras and the lateral axis of the ultrasound scanner are approximately perpendicular. d, Imaging configuration during 2D ultrasound imaging and single-camera optical mapping (see also b). The optical axis of the camera and the lateral axis of the ultrasound scanner are approximately perpendicular. The cross-sectional ultrasound imaging plane is positioned and aligned tangentially within the ventricular wall underneath and co-planar to the imaged surface. e, Imaging configuration during 3D ultrasound imaging in vivo. In ultrasound examinations of patients, the human heart is either imaged from outside the body through the chest in a transthoracic echocardiography (TTE) examination, or from within the body in a transoesophageal echocardiography examination using a transoesophageal ultrasound probe. The first measurement configuration provides a clearer picture of the ventricles, whereas the latter measurement provides a clearer picture of the atria. We aimed to mimic the TTE measurement imaging the ventricles using a probe that is routinely used in TTE examinations. In a TTE measurement, the transducer may be positioned on the chest below the heart imaging upwards through two ribs or from underneath the ribs. In one of the various views, the apex of the heart is facing the transducer (apical view), as it is located closest to the transducer array. The atria are located furthest away from the transducer array. The imaging configuration used in our experiment is very similar to this situation (a). The size of the human heart is comparable to the size of the pig hearts used in the ex vivo experiments. f, Frequent imaging configuration during 3D ultrasound imaging with panoramic optical mapping. One camera always imaged the anterior left ventricular wall (similar perspective as in a).
Extended Data Figure 4 Mapping and signal analysis of electromechanical rotor patterns during ventricular fibrillation and tachycardia in isolated Langendorff-perfused hearts.
a, Mapping of epicardial electrical (voltage) rotor activity during ventricular fibrillation on the contracting surface of a rabbit heart. Left, the time-series (black) obtained from the unstabilized fluorescence maps shows substantial motion artefacts, whereas the time-series of the motion-stabilized maps (green) shows a series of action potentials. Right, from the stabilized time-series, it is possible to compute the phase (black), that is, introducing phase jumps at the upstroke of the action potentials. Bottom, the upper image series shows a counter-clockwise-rotating action potential rotor (green) on the contracting heart surface (Supplementary Video 6). The lower image series shows the corresponding phase representation of the rotor and a phase singularity at the tip of the spiral. b, Left, time-series of strain rate obtained from the displacement field. Middle, normalized strain rate (see Methods). Right, zero-crossings of strain rate are used to obtain phase representation. Bottom, rotating wave of dilating (blue) and contracting (red) tissue regions rotating around each other and corresponding phase representation. A circle indicates the position of the mechanical phase singularity. Electrical and mechanical phase singularities are co-localized (Supplementary Video 6). c, Electrocardiogram during ventricular fibrillation (same heart as shown in a, b). Frequency spectra of electrocardiogram (black) and electrical (voltage, green) and elastomechanical (red) patterns measured optically on the epicardial surface of the left ventricular wall (a, b), showing matching dominant frequencies (9 ± 1 Hz). Frequency spectra of the patterns are cumulative spectra of all measurement sites (Supplementary Video 6). d, Electromechanical activity in isolated pig heart during ventricular tachycardia (Fig. 1 and Extended Data Fig. 1b). Top, time-series of action potential activity measured optically using voltage-sensitive optical mapping on anterior left ventricular surface. Middle, time-series of strain rate measured optically in same location as in the top panel on left ventricular surface using fluorescence imaging. Bottom, time-series of strain rate measured within the anterior left ventricular wall using 4D ultrasound imaging. n.u., normalized units. e, Electrocardiogram acquired in the isolated rabbit heart during ventricular fibrillation (Fig. 4i). The arrhythmic episode ended by self-termination of arrhythmic activity and transition into sinus rhythm. Frequency spectra of electrocardiogram and electrical (voltage, green) and elastomechanical (red) patterns measured optically on the epicardial surface and elastomechanical (red) patterns measured using ultrasound at midwall inside the left ventricular wall during arrhythmic episode (including data within 2.0 s before self-termination). The dominant frequencies are 9 ± 1Hz for voltage, calcium and strain. Frequency spectra of the patterns are cumulative spectra of all measurement sites.
Extended Data Figure 5 Coupled voltage and calcium dynamics mapped during ventricular fibrillation.
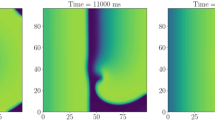
Voltage (action potential, green, voltage-sensitive staining using Di4-ANBDQPQ) and calcium (intracellular calcium, orange, calcium-sensitive staining using Rhod2-AM) vortex wave activity mapped on ventricular surface of the isolated rabbit heart during ventricular fibrillation using dual-imaging29. Recordings were acquired in non-contracting hearts after administering of blebbistatin (4 ml diluted in 700 ml Tyrode, retrograde perfusion with constant reperfusion). a, b, Example time-series (n = 5) of voltage–calcium activity chosen from arbitrary sites on the surface. Time-series show closely coupled voltage–calcium wave dynamics with a dominant frequency of 9 ± 1 Hz and a delay of the calcium activity. a, Activity on the surface within 2 s long (left) and 1 s long intervals (right) to facilitate viewing of the upstrokes and the delay between voltage and calcium. Recordings acquired before administering (a) and after the addition of cromakalim (b, 10 μmol in 1 l Tyrode, retrograde perfusion with constant reperfusion). We did not observe a noticeable difference in the dynamics. c, Voltage (action potential, green, voltage-sensitive staining using Di4-ANBDQPQ) and calcium (intracellular calcium, orange, calcium-sensitive staining using Rhod2-AM) raw movies (black-and-white colour code) mapped on ventricular surface (field of view approximately 1.5 × 1.5 cm2, time in ms) during ventricular fibrillation. The voltage-sensitive data are inverted (dimensionless normalized units (n.u.)), such that bright (or green) areas show depolarized tissue. Bright (or orange) areas in the calcium-sensitive data (dimensionless normalized units (n.u.)), show high intracellular calcium concentrations. The calcium-sensitive images show the same part of the tissue that is shown in the voltage-sensitive images, however, with a delay of 10 ms to compensate for the delay between voltage and calcium and to facilitate analysis of similar wave patterns. The patterns are highly similar and evolve congruently across the surface during ventricular fibrillation. Example image series chosen from a recording with a duration of 20 s. The findings are the same across different recordings. The experiment was repeated twice in n = 2 hearts. However, other studies41,42,43,44 have also shown that in abnormal voltage and calcium regimes the dynamics can have complex interactions and are not always necessarily closely coupled as shown here (see also Supplementary Discussion).
Extended Data Figure 6 Characteristics of epicardial electrical and mechanical phase singularities during ventricular fibrillation in pig and rabbit hearts.
a, b, Mean number of electrical (green) and mechanical (red) phase singularities (PS) during ventricular fibrillation imaged on the epicardial ventricular surface of isolated Langendorff-perfused pig hearts (a; four measurements from n = 3 hearts) and rabbit hearts (b; three measurements from n = 3 hearts). The number of phase singularities fluctuates strongly over time (error bars indicate the standard deviation; see also Fig. 4g). Both the electrical and mechanical average numbers of phase singularities similarly reflect different regimes of ventricular fibrillation (b). We consistently observed a slightly larger number of mechanical phase singularities (factor 1.2 ± 0.1). The average numbers of phase singularities were computed from 10-s long (500 frames per second) or 20-s long (250 frames per second) recordings with 5,000 video images, including >10,000 measurements of phase singularities, the recordings were more than 100 times longer than the average period or lifetime of a rotor. c, Ratio of the mean number of electrical and mechanical phase singularities (ratio = number mechanical PS/number electrical PS) during ventricular fibrillation on epicardial ventricular surface of isolated Langendorff-perfused pig hearts (four measurements from n = 3 hearts) and rabbit hearts (three measurements from n = 3 hearts). The ratio is close to 1 (1.2 ± 0.1) and consistently larger than 1, indicating that more mechanical than electrical phase singularities appear on the surface during ventricular fibrillation. Error bars are large as the number of phase singularities fluctuates strongly (from 0 to approximately 10) over long times (Fig. 4g). Error bars were computed as the standard deviation of the fluctuations of number of phase singularities over time (>1,000 samples or time-steps). The ratio (or centre of the plot) was computed from the simple average of the number of phase singularities (>1,000 samples or time-steps). d, Co-localization factor sigma indicating the precision, with which a mechanical phase singularity describes on average the position of a nearby electrical phase singularity. For large phase singularity numbers (nPS = 6–10; right) the precision is about 0.2 or 1/5 of the average rotor distance (of 1). In this regime, two phase singularities can clearly be separated from each other (Fig. 4a). For the computation of sigma, the average rotor distances and co-localization distances from the distributions as shown in Fig. 3g and Fig. 4a were used. For smaller phase singularity numbers (nPS = 1–3; left) sigma increases, indicating that the precision with which a mechanical phase singularity predicts the location of an electrical phase singularity decreases. The two data points (on the left) describe dynamical regimes with few strongly meandering rotors with linear cores and larger overall deformations of the cardiac muscle (also data point 5 in c) during ventricular fibrillation in rabbit hearts (Fig. 3). However, lower sigmas were observed in both pig and rabbit hearts. Lower sigmas or a higher precision is obtained during ventricular fibrillation with a larger number of smaller rotors and a weaker overall deformation of the cardiac muscle. e, Trajectories of mechanical phase singularities during ventricular fibrillation on the surface of the rabbit heart. Mechanical phase singularities (red dots) computed individually from voltage-sensitive (top) and calcium-sensitive (bottom) imaging data during multimodal fluorescence imaging (voltage, calcium and strain) with interleaved acquisition of the two channels (250 frames per second per channel = 500 frames per second). The plots show the accumulated mechanical phase singularities during a 400-ms long time interval at 2 s (left), 4 s (centre) and 8 s (right) of a 20-s long recording. The positions and trajectories of the mechanical phase singularities computed from the voltage or the calcium data are identical or at least almost identical throughout time. The corresponding strain rate patterns, from which the phase singularities were computed, are also almost identical or highly similar in each frame over time. The positions and trajectories of the mechanical phase singularities and strain rate patterns are also identical or at least almost identical when only one dye is used and one of the channels does not contain a fluorescent signal. The data demonstrate that the optically derived strain rate patterns are robust, that is, independent of fluorescence-induced image intensity fluctuations.
Extended Data Figure 7 Electromechanical dissociation and loss of contractility during very rapid (20 Hz) ventricular fibrillation in pig hearts.
a, Example traces of action potential wave activity measured on the left ventricular epicardial surface of a pig heart during ventricular fibrillation using multimodal optical mapping (voltage and contraction). Before the addition of the KATP channel opener cromakalim (baseline ventricular fibrillation, top), the ventricular muscle exhibits both fibrillatory electrical as well as contractile activity and associated deformations (see also Supplementary Video 12). Owing to the motion of the tissue, the optical traces are superimposed by motion artefacts, visible as modulations of the baseline of the signal. Motion stabilization and motion artefact removal retrieves the action potential wave activity (middle) with substantially reduced motion artefacts. The associated optical maps show spiral vortex wave patterns on the surface of the heart (see also Supplementary Video 12). The dominant frequency of the basal fibrillatory activity is 10.6 ± 1.5 Hz (b). After the addition of cromakalim, the dominant frequency of the electrical activity increases markedly (compared to ref. 40) to 20.5 ± 0.5 Hz, see b. At the same time, we measured that the heart does not exhibit any visible motion any longer (Supplementary Video 12). Because the contractions of the cardiac muscle vanish during very rapid ventricular fibrillation, optical maps and traces of the action potential wave activity can be retrieved without numerical motion tracking and motion stabilization (bottom). The modulations of the baseline of the signals, which can be seen during baseline ventricular fibrillation (10 Hz), do not appear at very rapid ventricular fibrillation (20 Hz), indicating that motion is not present (Supplementary Video 12). The data demonstrate a decoupling of the electromechanical wave dynamics during very rapid ventricular fibrillation induced by cromakalim. b, Loss of contractile activity during very rapid (20 Hz) ventricular fibrillation. Frequency spectra of electrical action potential wave pattern (green) and mechanical activity (red) measured during baseline ventricular fibrillation (top left, maxima at approximately 10 Hz) and very rapid ventricular fibrillation (bottom left, 20 Hz peak). The dominant frequency of the action potential wave activity approximately doubles from 10 Hz to 20 Hz after the addition of cromakalim, as previously described40. At the same time, the contractile motion of the heart vanishes. Correspondingly, a frequency spectrum of the contractile or mechanical activity could not be computed during very rapid ventricular fibrillation. The histograms (middle) show large amplitudes of motion (1–3 pixels displacements of tissue segments within short time spans of 2–3 wave periods) during baseline ventricular fibrillation (top middle) and substantially reduced or vanishing amplitudes of motion (0–0.3 pixels displacements, Supplementary Video 12) during very rapid ventricular fibrillation (bottom middle). The amplitudes of motion were calculated from the displacement data obtained from the motion-tracking procedure. The corresponding maps (top right and bottom right) show the amplitudes of motion measured across the ventricular surface (yellow indicates 2–3 pixels displacement; blue indicates 0 pixels displacement).
Extended Data Figure 8 Anisotropy of electromechanical rotor patterns in elastic excitable media (computer simulation) and effect of mechanical inhomogeneity onto mechanical phase singularities.
a, b, d, Dependence of local strain rate amplitude and strain rate morphology on the direction of wave propagation relative to muscle fibres. The electrical spiral wave pattern (a) and corresponding elastomechanical strain rate patterns (b, d) form in two identically prepared simulation domains with differing underlying vertical (b) and horizontal (d) muscle fibre anisotropy (uniform transverse linear fibre orientation). c, The contractions along the fibre orientation produce stronger strain rate amplitudes when the wave propagates along the fibre orientation (green time-series in b, sampled from the green triangle) and weaker strain rate amplitudes when the wave propagates perpendicular to the fibre orientation (orange time-series in b, sampled from the orange triangle). Overall, the morphology of the strain rate pattern aligns with the fibre orientation and exhibits stronger gradients between dilating and contracting rates of deformation along the fibre orientation than perpendicular to it (polarization). The deformation data were obtained in quasi-2D electromechanical computer simulations with homogeneous active tension development and immediate electromechanical coupling and simulation domains with finite thickness (see Methods). e–h, Sensitivity of phase singularity detection to external perturbations depending on the direction of wave propagation relative to fibres. e, Strain rate pattern superimposed with electrical (blue circle) and elastomechanical phase singularities (red circles) in a domain with uniform vertical fibre anisotropy. Perturbations caused by boundary conditions can distort the phase pattern and lead to the detection of spurious mechanical phase singularities, preferentially along the direction that is perpendicular to the fibre orientation. The spurious mechanical phase singularities propagate outwards away from the spiral wave core. f, Addition of a weak global strain perturbation exacerbates this effect in the direction that is perpendicular to the fibre orientation. g, Phase of strain rate shown in e used for the computation of the phase singularities also reveals anisotropy and polarization. h, The strong strain rate signal parallel to the fibre orientation (green time-series) is largely unaffected by a small perturbation, whereas, for the same perturbation amplitude, the strain rate signal in the low-amplitude region perpendicular to the fibre orientation is distorted more strongly (orange time-series). The deformation was obtained in simulations identical to those shown in a–d. Phase singularities from both the electrical signal and the strain rate were calculated using Hilbert transforms.
Extended Data Figure 9 Measurement of intramural phase singularity dynamics using 2D ultrasound imaging and tracking of a non-moving heart versus a fibrillating contracting heart in 3D ultrasound data and optical mapping.
a, Schematic of the experimental setup for simultaneous fluorescence and 2D ultrasound imaging in intact, Langendorff-perfused rabbit hearts. Left, ultrasound imaging (Vevo 2100, VisualSonics Inc.) with the cross-sectional echocardiographic imaging plane aligned tangentially inside the left ventricular wall (white line). Imaging plane facing fluorescence imaging camera (Extended Data Fig. 3d). Right, action potential, calcium and strain imaging setup for fluorescence imaging. b, Schematic of imaging configuration with action potential wave (phase) imaged on the surface of the heart and rotating mechanical pattern (phase) imaged inside the ultrasound cross-section inside the ventricular wall. The rendering shows a scroll wave (green, computer simulation). c, Optical mapping shows a counter-clockwise rotating action potential wave (AP, green) on the surface of a rabbit heart during ventricular fibrillation (Supplementary Video 9). The electrical vortex is associated with a counter-clockwise rotating pattern of contractile (red) and tensile (blue) rates of strain observed optically with fluorescence imaging on the surface. The mechanical deformation observed in B-mode ultrasound imaging in an imaging plane located beneath the imaged surface and aligned approximately parallel or co-planar to the epicardium shows a phase singularity, corresponding to a counter-clockwise rotating wave in mechanical deformation (Supplementary Video 9). The analysis of the electrical and mechanical vortices reveals co-existing phase singularities (indicated by white circles) on the surface and inside the ventricular wall. d, Tracking of the non-moving heart compared to a fibrillating contracting heart in 3D ultrasound and fluorescence imaging data. Distributions showing magnitudes of tracked displacement vectors resulting from motion tracking of the 3D ultrasound data (blue and red curves) and motion tracking during optical imaging (yellow curve). Influences by speckle noise or possible residual motion onto the motion tracking and motion analysis during ultrasound imaging are minimal in the Langendorff setup. Motion is not visible (Supplementary Video 13, left) when the heart does not contract. In comparison, the small contractions and deformations during ventricular fibrillation can clearly be observed (Supplementary Video 13, right) and can also be detected using motion-tracking algorithms (red curve, 3D ultrasound; yellow curve, optical mapping). The maximum of tracked displacements for the asystolic heart is approximately 0.15 mm. By contrast, during fibrillation, the maximum displacements are clearly shifted towards larger values with a maximum at 0.45 mm. The magnitudes of the tracked displacements during ventricular fibrillation (red curve) are confirmed by the optical measurement performed at the same time (yellow curve). Statistical analysis (two-sample Kolmogorov–Smirnov test) rejects the null hypothesis that the ultrasound-based measurements of tissue displacement during asystole and ventricular fibrillation are from the same continuous distribution at a 1% significance level. For the ultrasound data, the distributions were obtained from 274,444 voxels (asystole) and 165,558 voxels (fibrillation), for which the displacements were tracked in between consecutive volume frames (with Δt = 1 or Δt = 2 or Δt = 3) for the entire video sequence. Then only the maximal displacement in each voxel was stored and considered for the distributions to emphasize the influence of noise. Note in this context that in the asystolic case, tracking yields small displacement magnitudes due to measurement noise resulting presumably from both the algorithm and speckle noise. For a better comparison, the Δt or the temporal distance between volume frames between which motion was detected was adjusted. The asystolic data were imaged at volume rates of 62 volumes per second, whereas the fibrillation data was imaged at volume rates of 91 volumes per second. For the asystolic data (left), displacements were computed in between one and the second next volume frame (Δt = 2), resulting in an effective volume rate of approximately 30 volumes per second. However, the distribution (left) remained unchanged with Δt = 1, Δt = 2 or Δt = 3 frames, indicating that the tissue is static and does not exhibit motion. For the fibrillation data (right), displacements were computed in between one and the third next volume frame (Δt = 3), resulting also in an effective volume rate of approximately 30 volumes per second. With Δt = 1 or Δt = 2 frames, the distribution also remains clearly distinguishable from the non-moving distribution and retains displacement magnitudes well over 0.5 voxels. Note that in this particular fibrillation dataset, the overall strength of motion and deformation is relatively small compared to other datasets (for instance the one shown in Fig. 1). In the optical data, displacements were computed from a frame at time t to a frame at time t + 32 ms (Δt = 16 frames) to achieve a corresponding measurement of tissue displacements at imaging speeds of approximately 30 frames per second and to ensure comparability of the data. The data and the clearly distinguishable visual appearance of the non-moving and fibrillating heart (Supplementary Video 13) demonstrate that the spatiotemporal resolution of the 3D ultrasound imaging is sufficient to resolve elastomechanical deformation patterns during tachyarrhythmias.
Supplementary information
Supplementary Information
This file contains Supplementary Methods, a Supplementary Discussion, Supplementary Table 1 and Supplementary References. (PDF 372 kb)
Vortex filament measured during ventricular tachycardia inside ventricular wall of isolated pig heart imaged at high temporal resolution with panoramic fluorescence imaging (500fps) and 4D ultrasound (Siemens Acuson sc2000, 134vps, 6cm lat. depth, 52×90° opening angle).
The filament was obtained from measurement of mechanical tissue deformation (strain-rate) caused by an action potential scroll wave rotating within the heart wall (c.f. Fig. 1). The u-shaped filament touches the epicardial surface in the same region (near to the left anterior descending coronary artery), where two cores of a figure-of-eight or double action potential spiral wave are located (Extended Data Fig. 1a-b). (MOV 5906 kb)
Filament breakthrough and pairwise phase singularity creation on epicardial surface of left ventricular wall during ventricular fibrillation in isolated pig heart imaged using 4D ultrasound (Siemens Acuson sc2000, 104vps, 6cm lat. depth, 56×90° opening angle).
The creation of a pair of two counter-rotating phase singularities is observed on the surface filming taction potential waves on the epicardium (500fps). Prior to the creation of the phase singularity pair, a u-shaped mechanical filament loop emerges from the depths of the ventricular wall and breaks up into two filaments as it touches the epicardial surface. The phase singularity pair is created at the same time (Extended Data Fig. 1c). (MOV 2536 kb)
Computer simulation of scroll wave activity in bulk-shaped tissue volume.
The electrical action potential scroll wave (green) and corresponding phase rotating around the electrical vortex filament (green line). Rotating elastomechanical rate of deformation pattern (red: contracting, blue: dilating) and corresponding phase. An electromechanical filament of a coupled electromechanical scroll wave consists of a co-localized pair of electrical (green) and mechanical (red) filaments. Fibre orientation is organized in sheets co-planar to the large surfaces of the bulk. The main fibre orientation (uniform linearly transverse in each sheet) rotates throughout the bulk. (MOV 26378 kb)
Motion tracking and motion stabilization of fluorescence imaging recordings showing the contracting, fibrillating left ventricular surface of a rabbit heart (c.f. Fig 3c).
The left image shows the raw unregistered video data including motion artifacts. The right video image shows the tracked and stabilized video data with a significant reduction of motion artifacts. Black dots indicate the tracking following the moving tissue. The action potential wave is retrieved by normalizing the amplitude of the signal in the time-series in each pixel in the co-moving frame. Video showing turbulent electrical action potential wave activity (voltage-sensitive dye di-4-ANEPPS) during ventricular fibrillation. (MOV 17719 kb)
Motion tracking and motion stabilization of fluorescence imaging recordings showing the contracting, fibrillating left ventricular surface of a rabbit heart (c.f. Fig 3c).
The left image shows the raw unregistered video data including motion artifacts. The right video image shows the tracked and stabilized video data with significant reduction of motion artifacts. Black dots indicate the tracking following the moving tissue. The action potential wave is retrieved by normalizing the time-series in each pixel in the co-moving frame. Video showing action potential rotor (voltagesensitive dye di-4-ANEPPS) during ventricular fibrillation. (MOV 12995 kb)
Rotating electrical and mechanical patterns during ventricular fibrillation on the surface of contracting rabbit heart (c.f. Fig 3c, Extended Data Fig. 4a-b).
Action potential spiral wave (left image, green, voltage-sensitive-dye di-4-ANEPPS) produces phase singularity (green circle) in corresponding phase maps indicating rotational core region of electrical activity. Corresponding deformation of the ventricular wall (right image, red-blue) exhibits rotational elasto-mechanical pattern (strain-rate, red: contracting, blue: dilating rates of deformation), which also produces a phase singularity (red circle) in a similar location. (MOV 6584 kb)
Rotating electrical and mechanical patterns during ventricular fibrillation on the surface of contracting rabbit heart.
Turbulent electrical excitation waves with multiple vortices (left, green) produces a similar elasto-mechanical deformation pattern (right, red-blue), where one main counter-clock-wise rotating vortex causes also a counter-clock-wise rotating deformation pattern in the same region. Both patterns exhibit electrical (green circles) and mechanical phase singularities (red circles) which appear in similar locations throughout the sequence. (MOV 13261 kb)
Simultaneous tri-modal measurement of voltage, calcium and strain-rate rotors on the left ventricular surface of a rabbit heart during ventricular fibrillation (c.f. Fig. 3e,f).
Action potential (green) and calcium (orange) vortex waves and elastic deformations (red-blue) and respective phase maps were measured on the contracting epicardium using multi-modal, multi-parametric (tri-modal) fluorescence imaging (voltage-sensitive dye di-4-ANBDQPQ, calcium-sensitive dye Rhod-2AM). Co-localizing vortex core regions displayed by phase singularities (PS, voltage: green circles, calcium: orange circles, strain-rate: red circles). (MOV 19657 kb)
Simultaneous measurement of electrical and mechanical activity on the surface and inside the contracting left ventricular wall of a rabbit heart during ventricular fibrillation (see also Extended Data Fig. 9 a-c).
Action potential vortex waves and elastic deformations were measured on the epicardium using fluorescence imaging (voltage-sensitive, di-4-ANEPPS). Simultaneously, elastic deformations were measured in a co-planar cross-section beneath the filmed surface using 2D ultrasound (279 fps). Similarly rotating rate of deformation patterns (strain-rate, red: contracting, blue: dilating) could be observed on the surface and at midwall. Both mechanical patterns exhibit the same rotational sense and a core region displayed by a phase singularity (red circles). The mechanical patterns are accompanied by electrical action potential vortex wave patterns similarly rotating and exhibiting phase singularities across the heart surface. (MOV 25026 kb)
Arrhythmic pig heart exhibiting wave-like deformations and spiral wave-like rotating deformation and contraction patterns on the ventricular muscle surface in situ.
Two rotational centres are located on the left ventricle (bottom left) and right ventricle (top right), respectively. (MOV 14399 kb)
Electromechanical vortex filament imaged inside contracting and deforming left ventricular wall using 4D ultrasound (91vps, 7cm lateral field of view, 70° × 90° degrees opening angle of pyramid-shaped field of view).
Simultaneously, a counter-clockwise rotating spiral action potential wave was imaged on the ventricular surface using fluorescence imaging (voltage-sensitive, 500fps). Both the action potential spiral wave and the underlying 3D strain-rate pattern exhibit counter- clockwise rotations. The filament touches the epicardial surface close to the spiral wave core. The heart is the same heart as shown in Supplementary Videos 13 and 14. (MOV 2835 kb)
Electromechanical dissociation during very rapid ventricular fibrillation (rapid VF > 20 Hz) in pig heart (c.f. Extended Data Fig.7).
Left: normal VF, heart contracts (dominat frequency electrical waves: 10 Hz). Right: very rapid VF, heart does not exhibit contractile activity even though the heart is electrically active and fibrillates (dominant frequency approximately twice as large: 20 Hz). At the end of the video (t = 26 s), both windows show the heart after the application of Cromakalim and during rapid pacing and induction of VF. The cardiac muscle at first contracts and deforms, but almost immediately stops to contract and exhibits only residual swinging motion, which vanishes after a few seconds. (MOV 23081 kb)
Isolated pig heart imaged with 3D ultrasound.
asystolic non-moving heart (62vps, 12cm lateral field of view, 70° × 90°, recording consists of 45 volume frames, which were repeated 8 times in the video). Right: fibrillating contracting heart (91vps, 7cm lateral field of view, 70° × 90°, >900 volume frames). The influence of the perfusion pump onto the movements of the heart is minimal as the non-contracting, quiet (asystolic) heart does not exhibit any visible and measurable movements in the ultrasound movie. In comparison, the motion of the fibrillating contracting heart is substantially larger and immediately apparent (quantitative motion analysis in Extended Data Fig. 9 d). The asystolic heart did not beat and remained in the same location as shown in the video for several minutes. If the fibrillating heart was imaged at slower volume rates (i.e. 62vps) the visual perception of motion would be even stronger and computed displacement vectors even be larger. The smaller field of view corresponds to about the lower 2/3 part of the heart shown in the right. Both recordings (left, right) were made with the same heart and the spatial resolution is the same. The heart is the same heart as shown in Supplementary Videos 11 and 14. (MOV 2525 kb)
Isolated pig heart imaged with 3D ultrasound (51vps, 12cm lateral field of view, 90° × 90° degrees opening angle of pyramid-shaped field of view).
The heart beats periodically due to the application of electrical pacing stimuli (stimulation site indicated by red dot). After the application of a pacing stimulus, the ventricular wall starts to contract at the stimulation site. The corresponding strain-rate pattern that is obtained after motion tracking reveals a focal, concentric spatio-temporal pattern with contracting rates of strain emanating away from the stimulation site. The heart is the same heart as shown in Supplementary Videos 11 and 13. (MOV 6124 kb)
Rights and permissions
About this article
Cite this article
Christoph, J., Chebbok, M., Richter, C. et al. Electromechanical vortex filaments during cardiac fibrillation. Nature 555, 667–672 (2018). https://doi.org/10.1038/nature26001
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nature26001
This article is cited by
-
Interacting spiral wave patterns underlie complex brain dynamics and are related to cognitive processing
Nature Human Behaviour (2023)
-
High resolution optical mapping of cardiac electrophysiology in pre-clinical models
Scientific Data (2022)
-
Non-monotonous dose response function of the termination of spiral wave chaos
Scientific Reports (2022)
-
Quantifying the unknown impact of segmentation uncertainty on image-based simulations
Nature Communications (2021)
-
Topological turbulence in the membrane of a living cell
Nature Physics (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.