Abstract
In acute myeloid leukaemia, long-term survival is poor as most patients relapse despite achieving remission1. Historically, the failure of therapy has been thought to be due to mutations that produce drug resistance, possibly arising as a consequence of the mutagenic properties of chemotherapy drugs2. However, other lines of evidence have pointed to the pre-existence of drug-resistant cells3. For example, deep sequencing of paired diagnosis and relapse acute myeloid leukaemia samples has provided direct evidence that relapse in some cases is generated from minor genetic subclones present at diagnosis that survive chemotherapy3,4,5, suggesting that resistant cells are generated by evolutionary processes before treatment3 and are selected by therapy6,7,8. Nevertheless, the mechanisms of therapy failure and capacity for leukaemic regeneration remain obscure, as sequence analysis alone does not provide insight into the cell types that are fated to drive relapse. Although leukaemia stem cells9,10 have been linked to relapse owing to their dormancy and self-renewal properties11,12,13, and leukaemia stem cell gene expression signatures are highly predictive of therapy failure14,15, experimental studies have been primarily correlative7 and a role for leukaemia stem cells in acute myeloid leukaemia relapse has not been directly proved. Here, through combined genetic and functional analysis of purified subpopulations and xenografts from paired diagnosis/relapse samples, we identify therapy-resistant cells already present at diagnosis and two major patterns of relapse. In some cases, relapse originated from rare leukaemia stem cells with a haematopoietic stem/progenitor cell phenotype, while in other instances relapse developed from larger subclones of immunophenotypically committed leukaemia cells that retained strong stemness transcriptional signatures. The identification of distinct patterns of relapse should lead to improved methods for disease management and monitoring in acute myeloid leukaemia. Moreover, the shared functional and transcriptional stemness properties that underlie both cellular origins of relapse emphasize the importance of developing new therapeutic approaches that target stemness to prevent relapse.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Sarkozy, C. et al. Outcome of older patients with acute myeloid leukemia in first relapse. Am. J. Hematol. 88, 758–764 (2013)
Goldie, J. H. & Coldman, A. J. The genetic origin of drug resistance in neoplasms: implications for systemic therapy. Cancer Res. 44, 3643–3653 (1984)
Ding, L. et al. Clonal evolution in relapsed acute myeloid leukaemia revealed by whole-genome sequencing. Nature 481, 506–510 (2012)
Krönke, J. et al. Clonal evolution in relapsed NPM1-mutated acute myeloid leukemia. Blood 122, 100–108 (2013)
Garg, M. et al. Profiling of somatic mutations in acute myeloid leukemia with FLT3-ITD at diagnosis and relapse. Blood 126, 2491–2501 (2015)
Parkin, B. et al. Clonal evolution and devolution after chemotherapy in adult acute myelogenous leukemia. Blood 121, 369–377 (2013)
Bachas, C. et al. The role of minor subpopulations within the leukemic blast compartment of AML patients at initial diagnosis in the development of relapse. Leukemia 26, 1313–1320 (2012)
Greaves, M. Evolutionary determinants of cancer. Cancer Discov. 5, 806–820 (2015)
Lapidot, T. et al. A cell initiating human acute myeloid leukaemia after transplantation into SCID mice. Nature 367, 645–648 (1994)
Hope, K. J., Jin, L. & Dick, J. E. Acute myeloid leukemia originates from a hierarchy of leukemic stem cell classes that differ in self-renewal capacity. Nat. Immunol. 5, 738–743 (2004)
Ishikawa, F. et al. Chemotherapy-resistant human AML stem cells home to and engraft within the bone-marrow endosteal region. Nat. Biotechnol. 25, 1315–1321 (2007)
Costello, R. T. et al. Human acute myeloid leukemia CD34+/CD38− progenitor cells have decreased sensitivity to chemotherapy and Fas-induced apoptosis, reduced immunogenicity, and impaired dendritic cell transformation capacities. Cancer Res. 60, 4403–4411 (2000)
Terpstra, W. et al. Fluorouracil selectively spares acute myeloid leukemia cells with long-term growth abilities in immunodeficient mice and in culture. Blood 88, 1944–1950 (1996)
Eppert, K. et al. Stem cell gene expression programs influence clinical outcome in human leukemia. Nat. Med. 17, 1086–1093 (2011)
Ng, S. W. et al. A 17-gene stemness score for rapid determination of risk in acute leukaemia. Nature 540, 433–437 (2016)
Shlush, L. I. et al. Identification of pre-leukaemic haematopoietic stem cells in acute leukaemia. Nature 506, 328–333 (2014)
Wunderlich, M. et al. AML xenograft efficiency is significantly improved in NOD/SCID-IL2RG mice constitutively expressing human SCF, GM-CSF and IL-3. Leukemia 24, 1785–1788 (2010)
Corces-Zimmerman, M. R., Hong, W. J., Weissman, I. L., Medeiros, B. C. & Majeti, R. Preleukemic mutations in human acute myeloid leukemia affect epigenetic regulators and persist in remission. Proc. Natl Acad. Sci. USA 111, 2548–2553 (2014)
The Cancer Genome Atlas Research Network. Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. N. Engl. J. Med. 368, 2059–2074 (2013)
Andersson, A. K. et al. The landscape of somatic mutations in infant MLL-rearranged acute lymphoblastic leukemias. Nat. Genet. 47, 330–337 (2015)
Klco, J. M. et al. Functional heterogeneity of genetically defined subclones in acute myeloid leukemia. Cancer Cell 25, 379–392 (2014)
Goardon, N. et al. Coexistence of LMPP-like and GMP-like leukemia stem cells in acute myeloid leukemia. Cancer Cell 19, 138–152 (2011)
Fong, C. Y. et al. BET inhibitor resistance emerges from leukaemia stem cells. Nature 525, 538–542 (2015)
Subramanian, A. et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl Acad. Sci. USA 102, 15545–15550 (2005)
Qiao, W. et al. PERT: a method for expression deconvolution of human blood samples from varied microenvironmental and developmental conditions. PLoS Comput. Biol. 8, e1002838 (2012)
Kreso, A. & Dick, J. E. Evolution of the cancer stem cell model. Cell Stem Cell 14, 275–291 (2014)
Notta, F., Doulatov, S. & Dick, J. E. Engraftment of human hematopoietic stem cells is more efficient in female NOD/SCID/IL-2Rgc-null recipients. Blood 115, 3704–3707 (2010)
Mazurier, F., Doedens, M., Gan, O. I. & Dick, J. E. Rapid myeloerythroid repopulation after intrafemoral transplantation of NOD-SCID mice reveals a new class of human stem cells. Nat. Med. 9, 959–963 (2003)
Hu, Y. & Smyth, G. K. ELDA: extreme limiting dilution analysis for comparing depleted and enriched populations in stem cell and other assays. J. Immunol. Methods 347, 70–78 (2009)
Bandelt, H. J., Forster, P. & Röhl, A. Median-joining networks for inferring intraspecific phylogenies. Mol. Biol. Evol. 16, 37–48 (1999)
Novershtern, N. et al. Densely interconnected transcriptional circuits control cell states in human hematopoiesis. Cell 144, 296–309 (2011)
Gamazon, E. R. et al. Comprehensive genetic analysis of cytarabine sensitivity in a cell-based model identifies polymorphisms associated with outcome in AML patients. Blood 121, 4366–4376 (2013)
Acknowledgements
This work was supported by grants from the Ontario Institute for Cancer Research with funds from the province of Ontario, the Cancer Stem Cell Consortium with funding from the Government of Canada through Genome Canada and the Ontario Genomics Institute (OGI-047), and the Canadian Institutes of Health Research (CSC-105367), the Canadian Cancer Society, the Terry Fox Foundation, a Canada Research Chair to J.E.D. L.I.S. was funded by the Benjamin Pearl fellowship from the McEwen Centre for Regenerative Medicine and an American Society of Hematology Scholar Award. This research was funded in part by the Ontario Ministry of Health and Long Term Care, whose views are not expressed here. We thank all the members of the Dick laboratory for comments and P. Zandstra for supporting this work.
Author information
Authors and Affiliations
Contributions
L.I.S. and A.M. developed the study and workflow, and performed all the xenografting, cell purification, and genotyping analysis. M.D.M. provided clinical annotated samples from the Princess Margaret Cancer Centre AML biobank. L.H., J.D.M., and T.J.H. performed sequencing. A.T.-G., J.J.F.M., A.R.-B., I.J.-Z., and R.M. performed genotyping. J.L.M. and M.D. supported xenografting, S.A. helped with identification of genetic variants and PDVs. S.W.K.N., V.V., C.X., and G.B. provided gene expression, and statistical, bioinformatic, and perturbation (PERT) analysis. L.I.S. and A.M. wrote the paper. L.I.S., A.M., J.C.Y.W., M.D.M., and J.E.D. revised the paper. J.E.D. provided funding and study supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Additional information
Reviewer Information Nature thanks M. Greaves, R. Levine and the other anonymous reviewer(s) for their contribution to the peer review of this work.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
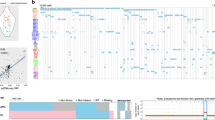
Extended Data Figure 1 Experimental design and estimated order of mutation acquisition for patients in PM AML cohort.
a, Experimental design. Patient samples obtained at diagnosis and relapse were sorted into multiple mature and progenitor populations by flow cytometry. In parallel, samples were injected into NSG or NSG-SGM3 mice, and human myeloid and T cells were sorted from the xenografts. WGS was performed on blasts and T cells, and ddPCR probes were designed for selected variants. These were then analysed by ddPCR in all the cell populations sorted from patient samples and xenografts for calculation of VAF. b, Estimated order of mutation acquisition for patients in PM AML cohort. Estimated order of acquisition of pre-leukaemic (grey) and leukaemic (black) PDVs, based on median joining network analysis.
Extended Data Figure 2 Analysis of relapse origin and clonal relationships for patients 1 and 6.
a, VAFs of PDVs as detected by ddPCR in various cell populations sorted directly from the diagnosis (Dx), relapse (Rel), or remission (Rem) samples of patient 1. No relapse variants were detected by ddPCR in this patient. White squares indicate populations in which no variants were detected. Phylogenetic tree showing clonal relationships for patient 1, based on analysis of VAFs of all pre-leukaemic and leukaemic mutations. The genetic distance between any two respective symbols on the phylogenetic tree was estimated using a neighbour joining method based on the degree of genetic relatedness (Nei’s genetic distance). Each coloured box contains highly related cell populations and xenografts inferred to represent a clone (green, pre-leukaemic; blue, diagnostic; red, relapse; blended blue and red, equal representation of diagnostic and relapse populations). b, VAFs of relapse variants as detected by ddPCR in various cell populations sorted directly from the diagnostic or relapse samples of patient 6, or in CD33+ myeloid cells isolated from xenografts generated from the diagnostic sample of the same patient. Abbreviations and display criteria are the same as in a. Phylogenetic tree showing clonal relationships for patient 6. The display criteria are the same as for a.
Extended Data Figure 3 Analysis of relapse origin and clonal relationships for patient 9.
VAFs of relapse variants as detected by ddPCR in various cell populations sorted directly from the diagnostic, remission, or relapse samples of patient 9, or in CD33+ myeloid cells isolated from xenografts generated from the diagnostic sample of the same patient. Abbreviations and display criteria are the same as in Extended Data Fig. 2a. VAFs of the only PDV detected by ddPCR in diagnostic blasts and in various cell populations sorted directly from the remission sample of patient 9. Phylogenetic tree showing clonal relationships for patient 9. The display criteria are the same as for Extended Data Fig. 2a.
Extended Data Figure 4 Analysis of relapse origin and clonal relationships for patient 2.
VAFs of relapse variants as detected by ddPCR in various cell populations sorted directly from the diagnostic, remission, or relapse samples of patient 2, or in CD33+ myeloid cells isolated from xenografts generated from the diagnostic sample of the same patient. Abbreviations and display criteria as in Extended Data Fig. 2a. VAFs of PDVs as detected by ddPCR in diagnostic blasts and in various cell populations sorted directly from the remission sample of patient 2. Phylogenetic tree showing clonal relationships for patient 2, based on analysis of VAFs of all relapse variants, pre-leukaemic, and leukaemic mutations. The display criteria are the same as for Extended Data Fig. 2a.
Extended Data Figure 5 Analysis of relapse origin and clonal relationships for patient 8.
VAFs of relapse variants as detected by ddPCR in various cell populations sorted directly from the diagnostic, remission, or relapse samples of patient 8, or in CD19+ B or CD33+ myeloid cells isolated from xenografts (DxGFM) generated from the diagnostic sample of the same patient. Abbreviations and display criteria as in Extended Data Fig. 2a. VAFs of PDVs as detected by ddPCR in diagnostic blasts and in various cell populations sorted directly from the remission sample of patient 8. Phylogenetic tree showing clonal relationships for patient 8. The display criteria are the same as for Extended Data Fig. 2a.
Extended Data Figure 6 Analysis of relapse origin and clonal relationships for patient 10.
VAFs of relapse variants as detected by ddPCR in various cell populations sorted directly from the diagnostic, remission, or relapse samples of patient 10, or in CD33+ myeloid cells isolated from xenografts generated from the diagnostic sample of the same patient. Abbreviations and display criteria are the same as in Extended Data Fig. 2a. VAFs of PDVs as detected by ddPCR in diagnostic blasts and in various cell populations sorted directly from the remission sample of patient 10. Phylogenetic tree showing clonal relationships for patient 10. The display criteria are the same as for Extended Data Fig. 2a.
Extended Data Figure 7 Analysis of relapse origin and clonal relationships for patients 4 and 11.
a, VAFs of relapse variants as detected by ddPCR in various cell populations sorted directly from the diagnostic, remission, or relapse samples of patient 4, or in CD33+ myeloid cells isolated from xenografts (DxM) generated from the diagnostic sample of the same patient. Abbreviations and display criteria are the same as in Extended Data Fig. 2a. Phylogenetic tree showing clonal relationships for patient 4. The display criteria are the same as for Extended Data Fig. 2a. b, VAFs of relapse variants as detected by ddPCR in various cell populations sorted directly from the diagnostic or relapse samples of patient 11. Abbreviations and display criteria are the same as in Extended Data Fig. 2a. Phylogenetic tree showing clonal relationships for patient 11. The display criteria are the same as for Extended Data Fig. 2a.
Extended Data Figure 8 Analysis of relapse origin and clonal relationships for patient 12.
VAFs of relapse variants as detected by ddPCR in various cell populations sorted directly from the diagnostic, remission, or relapse samples of patient 12, or in CD19+ B or CD33+ myeloid cells isolated from xenografts generated from the diagnostic sample of the same patient. Abbreviations and display criteria are the same as in Extended Data Fig. 2a. VAFs of the PDVs as detected by ddPCR in diagnostic blasts and in various cell populations sorted directly from the remission sample of patient 12. Phylogenetic tree showing clonal relationships for patient 12. The display criteria are the same as for Extended Data Fig. 2a.
Extended Data Figure 9 ROP and ROC correlate with TCGA gene expression clusters and demonstrate distinct molecular and clinical properties.
a, Gene set enrichment analysis of ROP and ROC clusters in the Princess Margaret Cancer Centre AML and TCGA relapsed AML cohorts. Diagnosis genes were ranked from top upregulated to top downregulated (ROC versus ROP cluster), and this rank list was compared using gene set enrichment analysis with the TCGA top 150 upregulated and top 150 downregulated genes (TCGA ROC-like versus TCGA ROP-like cluster). ROC genes correlate with TCGA ROC-like genes and ROP genes correlate with TCGA ROP-like genes. b, Comparison of genetic and clinical parameters between the TCGA ROC-like and TCGA ROP-like clusters identified distinct genomic and clinical properties associated with relapse origin.
Extended Data Figure 10 AML relapse is associated with increased stemness transcriptional programs and therapy resistance.
a, b, Proportion of bulk leukaemia populations that possess gene expression profiles of undifferentiated (a) or mature myeloid (b) cells, as determined by the perturbation (PERT) deconvolution analysis using gene expression data from known normal haematopoietic cell subsets. c, Leukaemia-initiating cell (LIC) frequency as determined by limiting dilution analysis. d, Gene-expression-based therapy resistance score. For all panels, data are shown for diagnostic (blue) and relapse (red) samples of patients in the PM cohort. Patients for whom the relapse origin (ROP or ROC) was functionally established are boxed.
Supplementary information
Supplementary Table 1
Clinical characteristics of the PM AML cohort. (XLSX 11 kb)
Supplementary Table 2
Immunophenotype of the diagnostic patient samples of the PM AML cohort. (XLSX 13 kb)
Supplementary Table 3
Protein damaging variants (PDVs) in the PM AML cohort. The reference allele (Ref) and alternative allele (Alt) were determined. Variant allele frequency (VAF) from whole genome sequencing of bulk cells from diagnosis (Dx), relapse (Rel) and Dx T cells (Tc) are provided. If the mutation appeared in a gene that was recurrently mutated in AML (more than 1% mutations in the TCGA AML dataset) the mutation is marked as recurrent (Y). If the variant was described in dbSNP, the major allele frequency (MAF) of the SNP from SNP142 is noted. (XLSX 47 kb)
Supplementary Table 4
Relapse variants (RVs) in the PM AML cohort. The reference allele (Ref) and alternative allele (Alt) were determined. Variant allele frequency (VAF) from whole genome sequencing of bulk cells from diagnosis (Dx), relapse (Rel) and Dx T cells (Tc) are provided. (XLSX 525 kb)
Supplementary Table 5
Somatic variants at Dx in the PM AML cohort. (XLSX 337 kb)
Supplementary Table 6
Frequency of nucleotide substitutions for RVs and somatic variants in the PM AML cohort. (XLSX 9 kb)
Supplementary Table 7
LSC frequency determined by limiting dilution assays in xenografts. The inverse of LSC frequency as well as upper and lower estimates are provided. Samples that generated multilineage grafts composed mainly of B cells with a minor CD33+ myeloid population are shaded. (XLSX 10 kb)
Supplementary Table 8
Protein damaging variants (PDVs) and relapse variants (RVs) validated by ddPCR in the PM AML cohort. For each patient, a matrix of sorted cell populations (rows) and variants (columns) is provided. VAFs were calculated from the ddPCR reaction. For patients #2, 8, and 15, NSG-SGM3 xenograft data is also provided. For patients # 8 and 10, diagnosis variants (present in diagnosis blasts and not in relapse blasts) are also provided. The presence of FLT3-ITD was determined by PCR, and the VAF recorded as 50% if positive and 0 if negative. (XLSX 87 kb)
Supplementary Table 9
Differential gene expression between 11 diagnosis and relapse AML samples by RNA sequencing. First worksheet (RC_Dx_Rel), read counts (RC) of RNA sequencing data. Second worksheet (RC_Diff_Exp) differential gene expression by RC. Third worksheet (RPKM_Diff_Exp), RNA sequencing data by RPKM and differential gene expression. Fourth and fifth worksheets, list of genes significantly differentially expressed between the ROP and ROC clusters of the PM AML cohort. Forth (ROc), top 40 genes that are more highly expressed in the ROc cluster. Fifth (ROp) 40 genes that are more highly expressed in the ROp cluster. (XLSX 10972 kb)
Supplementary Table 10
Summary table of results from the 11 AML samples including relapse origin, clinical, genetic and engraftment data. (XLSX 10 kb)
Rights and permissions
About this article
Cite this article
Shlush, L., Mitchell, A., Heisler, L. et al. Tracing the origins of relapse in acute myeloid leukaemia to stem cells. Nature 547, 104–108 (2017). https://doi.org/10.1038/nature22993
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nature22993
This article is cited by
-
RAB27B-regulated exosomes mediate LSC maintenance via resistance to senescence and crosstalk with the microenvironment
Leukemia (2024)
-
SHP-1 inhibition targets leukaemia stem cells to restore immunosurveillance and enhance chemosensitivity by metabolic reprogramming
Nature Cell Biology (2024)
-
Cancer cell plasticity, stem cell factors, and therapy resistance: how are they linked?
Cancer and Metastasis Reviews (2024)
-
Three-Dimensional Tumor Models to Study Cancer Stemness-Mediated Drug Resistance
Cellular and Molecular Bioengineering (2024)
-
FBXO22 promotes leukemogenesis by targeting BACH1 in MLL-rearranged acute myeloid leukemia
Journal of Hematology & Oncology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.