Abstract
Highly potent and broadly neutralizing anti-HIV-1 antibodies (bNAbs) have been used to prevent and treat lentivirus infections in humanized mice, macaques, and humans1,2,3,4,5,6,7,8,9,10,11,12. In immunotherapy experiments, administration of bNAbs to chronically infected animals transiently suppresses virus replication, which invariably returns to pre-treatment levels and results in progression to clinical disease. Here we show that early administration of bNAbs in a macaque simian/human immunodeficiency virus (SHIV) model is associated with very low levels of persistent viraemia, which leads to the establishment of T-cell immunity and resultant long-term infection control. Animals challenged with SHIVAD8-EO by mucosal or intravenous routes received a single 2-week course of two potent passively transferred bNAbs (3BNC117 and 10-1074 (refs 13, 14)). Viraemia remained undetectable for 56–177 days, depending on bNAb half-life in vivo. Moreover, in the 13 treated monkeys, plasma virus loads subsequently declined to undetectable levels in 6 controller macaques. Four additional animals maintained their counts of T cells carrying the CD4 antigen (CD4+) and very low levels of viraemia persisted for over 2 years. The frequency of cells carrying replication-competent virus was less than 1 per 106 circulating CD4+ T cells in the six controller macaques. Infusion of a T-cell-depleting anti-CD8β monoclonal antibody to the controller animals led to a specific decline in levels of CD8+ T cells and the rapid reappearance of plasma viraemia. In contrast, macaques treated for 15 weeks with combination anti-retroviral therapy, beginning on day 3 after infection, experienced sustained rebound plasma viraemia when treatment was interrupted. Our results show that passive immunotherapy during acute SHIV infection differs from combination anti-retroviral therapy in that it facilitates the emergence of potent CD8+ T-cell immunity able to durably suppress virus replication.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Barouch, D. H. et al. Therapeutic efficacy of potent neutralizing HIV-1-specific monoclonal antibodies in SHIV-infected rhesus monkeys. Nature 503, 224–228 (2013)
Bolton, D. L. et al. Human immunodeficiency virus type 1 monoclonal antibodies suppress acute simian-human immunodeficiency virus viremia and limit seeding of cell-associated viral reservoirs. J. Virol. 90, 1321–1332 (2016)
Caskey, M. et al. Viraemia suppressed in HIV-1-infected humans by broadly neutralizing antibody 3BNC117. Nature 522, 487–491 (2015)
Gautam, R. et al. A single injection of anti-HIV-1 antibodies protects against repeated SHIV challenges. Nature 533, 105–109 (2016)
Halper-Stromberg, A. et al. Broadly neutralizing antibodies and viral inducers decrease rebound from HIV-1 latent reservoirs in humanized mice. Cell 158, 989–999 (2014)
Hessell, A. J. et al. Early short-term treatment with neutralizing human monoclonal antibodies halts SHIV infection in infant macaques. Nature Med. 22, 362–368 (2016)
Horwitz, J. A. et al. HIV-1 suppression and durable control by combining single broadly neutralizing antibodies and antiretroviral drugs in humanized mice. Proc. Natl Acad. Sci. USA 110, 16538–16543 (2013)
Klein, F. et al. HIV therapy by a combination of broadly neutralizing antibodies in humanized mice. Nature 492, 118–122 (2012)
Lynch, R. M. et al. Virologic effects of broadly neutralizing antibody VRC01 administration during chronic HIV-1 infection. Sci. Transl. Med. 7, 319ra206 (2015)
Moldt, B. et al. Highly potent HIV-specific antibody neutralization in vitro translates into effective protection against mucosal SHIV challenge in vivo. Proc. Natl Acad. Sci. USA 109, 18921–18925 (2012)
Shingai, M. et al. Passive transfer of modest titers of potent and broadly neutralizing anti-HIV monoclonal antibodies block SHIV infection in macaques. J. Exp. Med. 211, 2061–2074 (2014)
Shingai, M. et al. Antibody-mediated immunotherapy of macaques chronically infected with SHIV suppresses viraemia. Nature 503, 277–280 (2013)
Mouquet, H. et al. Complex-type N-glycan recognition by potent broadly neutralizing HIV antibodies. Proc. Natl Acad. Sci. USA 109, E3268–E3277 (2012)
Scheid, J. F. et al. Sequence and structural convergence of broad and potent HIV antibodies that mimic CD4 binding. Science 333, 1633–1637 (2011)
Brenchley, J. M. et al. CD4+ T cell depletion during all stages of HIV disease occurs predominantly in the gastrointestinal tract. J. Exp. Med. 200, 749–759 (2004)
Borrow, P., Lewicki, H., Hahn, B. H., Shaw, G. M. & Oldstone, M. B. Virus-specific CD8+ cytotoxic T-lymphocyte activity associated with control of viremia in primary human immunodeficiency virus type 1 infection. J. Virol. 68, 6103–6110 (1994)
Koup, R. A. et al. Temporal association of cellular immune responses with the initial control of viremia in primary human immunodeficiency virus type 1 syndrome. J. Virol. 68, 4650–4655 (1994)
Davey, R. T., Jr et al. HIV-1 and T cell dynamics after interruption of highly active antiretroviral therapy (HAART) in patients with a history of sustained viral suppression. Proc. Natl Acad. Sci. USA 96, 15109–15114 (1999)
Chun, T. W. et al. Early establishment of a pool of latently infected, resting CD4(+) T cells during primary HIV-1 infection. Proc. Natl Acad. Sci. USA 95, 8869–8873 (1998)
Buzon, M. J. et al. Long-term antiretroviral treatment initiated at primary HIV-1 infection affects the size, composition, and decay kinetics of the reservoir of HIV-1-infected CD4 T cells. J. Virol. 88, 10056–10065 (2014)
Sáez-Cirión, A. et al. Post-treatment HIV-1 controllers with a long-term virological remission after the interruption of early initiated antiretroviral therapy ANRS VISCONTI Study. PLoS Pathog. 9, e1003211 (2013)
Lifson, J. D. et al. Containment of simian immunodeficiency virus infection: cellular immune responses and protection from rechallenge following transient postinoculation antiretroviral treatment. J. Virol. 74, 2584–2593 (2000)
Schoofs, T. et al. HIV-1 therapy with monoclonal antibody 3BNC117 elicits host immune responses against HIV-1. Science 352, 997–1001 (2016)
Igarashi, T. et al. Human immunodeficiency virus type 1 neutralizing antibodies accelerate clearance of cell-free virions from blood plasma. Nature Med. 5, 211–216 (1999)
Liu, J. et al. Antibody-mediated protection against SHIV challenge includes systemic clearance of distal virus. Science 353, 1045–1049 (2016)
Lu, C. L. et al. Enhanced clearance of HIV-1-infected cells by broadly neutralizing antibodies against HIV-1 in vivo. Science 352, 1001–1004 (2016)
Gautam, R. et al. Pathogenicity and mucosal transmissibility of the R5-tropic simian/human immunodeficiency virus SHIV(AD8) in rhesus macaques: implications for use in vaccine studies. J. Virol. 86, 8516–8526 (2012)
Nishimura, Y. et al. Generation of the pathogenic R5-tropic simian/human immunodeficiency virus SHIVAD8 by serial passaging in rhesus macaques. J. Virol. 84, 4769–4781 (2010)
Shingai, M. et al. Most rhesus macaques infected with the CCR5-tropic SHIV(AD8) generate cross-reactive antibodies that neutralize multiple HIV-1 strains. Proc. Natl Acad. Sci. USA 109, 19769–19774 (2012)
Bournazos, S., DiLillo, D. J. & Ravetch, J. V. The role of Fc-FcγR interactions in IgG-mediated microbial neutralization. J. Exp. Med. 212, 1361–1369 (2015)
Endo, Y. et al. Short- and long-term clinical outcomes in rhesus monkeys inoculated with a highly pathogenic chimeric simian/human immunodeficiency virus. J. Virol. 74, 6935–6945 (2000)
Hansen, S. G. et al. Profound early control of highly pathogenic SIV by an effector memory T-cell vaccine. Nature 473, 523–527 (2011)
Foulds, K. E., Donaldson, M. & Roederer, M. OMIP-005: quality and phenotype of antigen-responsive rhesus macaque T cells. Cytometry A 81, 360–361 (2012)
Chun, T. W. et al. Effect of interleukin-2 on the pool of latently infected, resting CD4+ T cells in HIV-1-infected patients receiving highly active anti-retroviral therapy. Nature Med. 5, 651–655 (1999)
Myers, L. E., McQuay, L. J. & Hollinger, F. B. Dilution assay statistics. J. Clin. Microbiol. 32, 732–739 (1994)
Fukazawa, Y. et al. B cell follicle sanctuary permits persistent productive simian immunodeficiency virus infection in elite controllers. Nature Med. 21, 132–139 (2015)
Acknowledgements
We thank A. Peach and T. Lewis for determining plasma viral RNA loads, and K. Rice, R. Engel, R. Petros, and S. Fong for assisting in the maintenance of animals and performing procedures. We thank R. Fast for technical assistance with ultrasensitive viral load assays, and J. Brenchley for performing FACS analyses. We are indebted to Gilead Sciences for providing tenofovir and emtricitabine. The anti-CD8 mAbs, MT807R1 and CD8b255R1, were obtained from the National Institutes of Health (NIH) Nonhuman Primate Reagent Resource supported by HHSN272200900037C and OD10976. We thank the NIH AIDS Research and Reference Reagent Program for TZM-bl cells. This work was supported by the Intramural Research Program of the National Institute of Allergy and Infectious Diseases (NIH), Vaccine Research Center of the National Institute of Allergy and Infectious Diseases (NIH), and, in part, with federal funds from the National Cancer Institute (NIH) under contract number HHSN261200800001E (J.D.L.). The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government. The research was also funded in part by the following grants: Collaboration for AIDS Vaccine Discovery grant OPP1033115 (M.C.N.); NIH Clinical and Translational Science Award (CTSA) program; NIH Center for HIV/AIDS Vaccine Immunology and Immunogen Discovery (CHAVI-ID) 1UM1 AI100663-01 (M.C.N.); Bill and Melinda Gates Foundation grants OPP1092074 and OPP1124068 (M.C.N.); NIH HIVRAD P01 AI100148 (M.C.N.); the Robertson Foundation to M.C.N. M.C.N. is a Howard Hughes Medical Institute Investigator.
Author information
Authors and Affiliations
Contributions
Y.N., M.C.N., and M.A.M. designed experiments; Y.N., R.G., T.-W.C., R.S., K.E.F., M.S., F.K., A.G., J.G., O.K.D., R.J.P., and M.S.S. performed experiments; Y.N., T.-W.C., A.B.-W., M.S.S., J.D.L., R.A.K., A.S.F., M.C.N., and M.A.M. analysed data; Y.N., J.D.L., R.A.K., A.S.F., M.C.N., and M.A.M. wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Additional information
Reviewer Information Nature thanks R. Siliciano and the other anonymous reviewer(s) for their contribution to the peer review of this work.
Extended data figures and tables
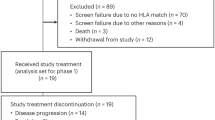
Extended Data Figure 1 Sustained suppression of virus replication by a 2-week course of combination bNAb treatment after intrarectal SHIVAD8-EO challenge.
Plasma viral RNA levels and 10-1074 or 3BNC117 mAb concentrations after bNAb therapy beginning on day 3 after intrarectal challenge are shown (n = 6).
Extended Data Figure 2 Sustained suppression of virus replication by a 2-week course of combination bNAb treatment after intravenous SHIVAD8-EO challenge.
Plasma viral RNA levels and 10-1074 or 3BNC117 mAb concentrations after bNAb therapy beginning on day 3 after intravenous challenge are shown (n = 7).
Extended Data Figure 3 Analyses of selected SHIVAD8 gp120 sequences known to confer resistance to 10-1074 or 3BNC117 mAbs present in virus rebounding after immunotherapy.
Nucleotide sequences present in amplicons, obtained from animals DELV (day 84 after infection), DEWL (day 72 after infection), DF06 (day 99 after infection), or MAF (day 90 after infection) during virus rebound (shown in Extended Data Fig. 2d–g), were evaluated. SHIVAD8-EO gp120 sequences are shown at the top. Mutations conferring resistance to 10-1074 (vertical bars) and 3BNC117 (horizontal bars) are highlighted.
Extended Data Figure 4 CD8+ T-cell responses and memory phenotype.
a, Memory CD8+ T-cell responses to SIVmac239 Gag measured by intracellular cytokine staining as a sum of IFN-γ, IL-2, TNF, CD107a, MIP-1B, and IL-10. Supp, during bNAb-mediated viral suppression; Peak, during peak of virus rebound; Base, after resolution of rebound; Late, during late stage of virus infection; coloured bars, mean; whiskers, s.e.m. b, Polyfunctionality of the CD8+ T-cell responses in macaques inoculated by the intravenous route. c, CD8+ T-cell memory subsets in macaques inoculated by the intravenous route. N, naive; CM, central memory; EM, effector memory; TEM, terminal effector memory.
Extended Data Figure 5 FACS analyses of CD8+ cells in controller animals after administration of depleting anti-CD8 mAbs.
CD8+ lymphocytes were collected from controller monkeys MVJ, DEWL, and DEMR after infusion of the MT807R1anti-CD8α mAb (a, b) or the CD8b255R1 anti-CD8β mAb (c, d) and the CD3+CD8+ and CD3–CD8+ fractions determined.
Extended Data Figure 6 Administration of cART during the acute SHIVAD8-EO infection of macaques does not result in controller status.
cART (tenofovir, emtricitabine, and raltagravir) was administered daily to three animals for 15 weeks beginning on day 3 after intrarectal challenge with 1,000 TCID50 of SHIVAD8-EO.
Rights and permissions
About this article
Cite this article
Nishimura, Y., Gautam, R., Chun, TW. et al. Early antibody therapy can induce long-lasting immunity to SHIV. Nature 543, 559–563 (2017). https://doi.org/10.1038/nature21435
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nature21435
This article is cited by
-
Immune targeting of HIV-1 reservoir cells: a path to elimination strategies and cure
Nature Reviews Microbiology (2024)
-
Early antiretroviral therapy favors post-treatment SIV control associated with the expansion of enhanced memory CD8+ T-cells
Nature Communications (2024)
-
Prevention, treatment and cure of HIV infection
Nature Reviews Microbiology (2023)
-
Probabilities of developing HIV-1 bNAb sequence features in uninfected and chronically infected individuals
Nature Communications (2023)
-
High monoclonal neutralization titers reduced breakthrough HIV-1 viral loads in the Antibody Mediated Prevention trials
Nature Communications (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.