Abstract
Chronic lymphocytic leukaemia (CLL) is a frequent disease in which the genetic alterations determining the clinicobiological behaviour are not fully understood. Here we describe a comprehensive evaluation of the genomic landscape of 452 CLL cases and 54 patients with monoclonal B-lymphocytosis, a precursor disorder. We extend the number of CLL driver alterations, including changes in ZNF292, ZMYM3, ARID1A and PTPN11. We also identify novel recurrent mutations in non-coding regions, including the 3′ region of NOTCH1, which cause aberrant splicing events, increase NOTCH1 activity and result in a more aggressive disease. In addition, mutations in an enhancer located on chromosome 9p13 result in reduced expression of the B-cell-specific transcription factor PAX5. The accumulative number of driver alterations (0 to ≥4) discriminated between patients with differences in clinical behaviour. This study provides an integrated portrait of the CLL genomic landscape, identifies new recurrent driver mutations of the disease, and suggests clinical interventions that may improve the management of this neoplasia.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Accession codes
Data deposits
Sequencing, expression and genotyping array data have been deposited at the European Genome-Phenome Archive (EGA, http://www.ebi.ac.uk/ega/), which is hosted at the European Bioinformatics Institute (EBI), under accession number EGAS00000000092.
Change history
22 October 2015
The full size image of Extended Data Fig. 8 in the HTML was incorrectly showing Extended Data Fig. 7; this has been corrected on 22 October 2015.
References
Gaidano, G., Foa, R. & Dalla-Favera, R. Molecular pathogenesis of chronic lymphocytic leukemia. J. Clin. Invest. 122, 3432–3438 (2012)
Zenz, T., Mertens, D., Kuppers, R., Dohner, H. & Stilgenbauer, S. From pathogenesis to treatment of chronic lymphocytic leukaemia. Nature Rev. Cancer 10, 37–50 (2010)
Pekarsky, Y., Zanesi, N. & Croce, C. M. Molecular basis of CLL. Semin. Cancer Biol. 20, 370–376 (2010)
Hamblin, T. J., Davis, Z., Gardiner, A., Oscier, D. G. & Stevenson, F. K. Unmutated Ig VH genes are associated with a more aggressive form of chronic lymphocytic leukemia. Blood 94, 1848–1854 (1999)
Damle, R. N. et al. Ig V gene mutation status and CD38 expression as novel prognostic indicators in chronic lymphocytic leukemia. Blood 94, 1840–1847 (1999)
Crespo, M. et al. ZAP-70 expression as a surrogate for immunoglobulin-variable-region mutations in chronic lymphocytic leukemia. N. Engl. J. Med. 348, 1764–1775 (2003)
Malek, S. N. The biology and clinical significance of acquired genomic copy number aberrations and recurrent gene mutations in chronic lymphocytic leukemia. Oncogene 32, 2805–2817 (2013)
Döhner, H. et al. Genomic aberrations and survival in chronic lymphocytic leukemia. N. Engl. J. Med. 343, 1910–1916 (2000)
Quesada, V. et al. Exome sequencing identifies recurrent mutations of the splicing factor SF3B1 gene in chronic lymphocytic leukemia. Nature Genet. 44, 47–52 (2011)
Puente, X. S. et al. Whole-genome sequencing identifies recurrent mutations in chronic lymphocytic leukaemia. Nature 475, 101–105 (2011)
Landau, D. A. et al. Evolution and impact of subclonal mutations in chronic lymphocytic leukemia. Cell 152, 714–726 (2013)
Fabbri, G. et al. Analysis of the chronic lymphocytic leukemia coding genome: role of NOTCH1 mutational activation. J. Exp. Med. 208, 1389–1401 (2011)
Ramsay, A. J. et al. POT1 mutations cause telomere dysfunction in chronic lymphocytic leukemia. Nature Genet. 45, 526–530 (2013)
Damm, F. et al. Acquired initiating mutations in early hematopoietic cells of CLL patients. Cancer Discov. 4, 1088–1101 (2014)
Rossi, D. et al. Disruption of BIRC3 associates with fludarabine chemorefractoriness in TP53 wild-type chronic lymphocytic leukemia. Blood 119, 2854–2862 (2012)
Ferreira, P. G. et al. Transcriptome characterization by RNA sequencing identifies a major molecular and clinical subdivision in chronic lymphocytic leukemia. Genome Res. 24, 212–226 (2014)
Kulis, M. et al. Epigenomic analysis detects widespread gene-body DNA hypomethylation in chronic lymphocytic leukemia. Nature Genet. 44, 1236–1242 (2012)
Oakes, C. C. et al. Evolution of DNA methylation is linked to genetic aberrations in chronic lymphocytic leukemia. Cancer Discov. 4, 348–361 (2014)
Hudson, T. J. et al. International network of cancer genome projects. Nature 464, 993–998 (2010)
Alexandrov, L. B. et al. Signatures of mutational processes in human cancer. Nature 500, 415–421 (2013)
Khodabakhshi, A. H. et al. Recurrent targets of aberrant somatic hypermutation in lymphoma. Oncotarget 3, 1308–1319 (2012)
Pasqualucci, L. et al. Hypermutation of multiple proto-oncogenes in B-cell diffuse large-cell lymphomas. Nature 412, 341–346 (2001)
Byrd, J. C. et al. Targeting BTK with ibrutinib in relapsed chronic lymphocytic leukemia. N. Engl. J. Med. 369, 32–42 (2013)
Moncunill, V. et al. Comprehensive characterization of complex structural variations in cancer by directly comparing genome sequence reads. Nature Biotechnol. 32, 1106–1112 (2014)
Stephens, P. J. et al. Massive genomic rearrangement acquired in a single catastrophic event during cancer development. Cell 144, 27–40 (2011)
Baca, S. C. et al. Punctuated evolution of prostate cancer genomes. Cell 153, 666–677 (2013)
Rausch, T. et al. Genome sequencing of pediatric medulloblastoma links catastrophic DNA rearrangements with TP53 mutations. Cell 148, 59–71 (2012)
Balatti, V. et al. NOTCH1 mutations in CLL associated with trisomy 12. Blood 119, 329–331 (2012)
Huang, F. W. et al. Highly recurrent TERT promoter mutations in human melanoma. Science 339, 957–959 (2013)
Yamane, A. et al. Deep-sequencing identification of the genomic targets of the cytidine deaminase AID and its cofactor RPA in B lymphocytes. Nature Immunol. 12, 62–69 (2011)
Lawrence, M. S. et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature 499, 214–218 (2013)
Simonis, M., Kooren, J. & de Laat, W. An evaluation of 3C-based methods to capture DNA interactions. Nature Methods 4, 895–901 (2007)
Revilla-i-Domingo, R. et al. The B-cell identity factor Pax5 regulates distinct transcriptional programmes in early and late B lymphopoiesis. EMBO J. 31, 3130–3146 (2012)
Queirós, A. C. et al. A B-cell epigenetic signature defines three biologic subgroups of chronic lymphocytic leukemia with clinical impact. Leukemia 29, 598–605 (2015)
Strefford, J. C. et al. Distinct patterns of novel gene mutations in poor-prognostic stereotyped subsets of chronic lymphocytic leukemia: the case of SF3B1 and subset #2. Leukemia 27, 2196–2199 (2013)
Agathangelidis, A. et al. Stereotyped B-cell receptors in one-third of chronic lymphocytic leukemia: a molecular classification with implications for targeted therapies. Blood 119, 4467–4475 (2012)
Rubio-Perez, C. et al. In silico prescription of anticancer drugs to cohorts of 28 tumor types reveals targeting opportunities. Cancer Cell 27, 382–396 (2015)
Lobry, C., Oh, P. & Aifantis, I. Oncogenic and tumor suppressor functions of Notch in cancer: it’s NOTCH what you think. J. Exp. Med. 208, 1931–1935 (2011)
O'Brien, P., Morin, P., Jr, Ouellette, R. J. & Robichaud, G. A. The Pax-5 gene: a pluripotent regulator of B-cell differentiation and cancer disease. Cancer Res. 71, 7345–7350 (2011)
Villamor, N. et al. NOTCH1 mutations identify a genetic subgroup of chronic lymphocytic leukemia patients with high risk of transformation and poor outcome. Leukemia 27, 1100–1106 (2013)
Bentley, D. R. et al. Accurate whole human genome sequencing using reversible terminator chemistry. Nature 456, 53–59 (2008)
Li, H. & Durbin, R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25, 1754–1760 (2009)
Li, H. et al. The Sequence Alignment/Map format and SAMtools. Bioinformatics 25, 2078–2079 (2009)
Puente, X. S. et al. Whole-genome sequencing identifies recurrent mutations in chronic lymphocytic leukaemia. Nature 475, 101–105 (2011)
Alexandrov, L. B., Nik-Zainal, S., Wedge, D. C., Campbell, P. J. & Stratton, M. R. Deciphering signatures of mutational processes operative in human cancer. Cell Rep. 3, 246–259 (2013)
Delgado, J. et al. Genomic complexity and IGHV mutational status are key predictors of outcome of chronic lymphocytic leukemia patients with TP53 disruption. Haematologica 99, e231–e234 (2014)
Edelmann, J. et al. High-resolution genomic profiling of chronic lymphocytic leukemia reveals new recurrent genomic alterations. Blood 120, 4783–4794 (2012)
Valdés-Mas, R., Bea, S., Puente, D. A., Lopez-Otin, C. & Puente, X. S. Estimation of copy number alterations from exome sequencing data. PLoS ONE 7, e51422 (2012)
Bibikova, M. et al. High density DNA methylation array with single CpG site resolution. Genomics 98, 288–295 (2011)
Bibikova, M. et al. Genome-wide DNA methylation profiling using InfiniumR assay. Epigenomics 1, 177–200 (2009)
Aryee, M. J. et al. Minfi: a flexible and comprehensive Bioconductor package for the analysis of Infinium DNA methylation microarrays. Bioinformatics 30, 1363–1369 (2014)
Kluk, M. J. et al. Gauging NOTCH1 activation in cancer using immunohistochemistry. PLoS ONE 8, e67306 (2013)
van de Werken, H. J. et al. Robust 4C-seq data analysis to screen for regulatory DNA interactions. Nature Methods 9, 969–972 (2012)
van de Werken, H. J. et al. 4C technology: protocols and data analysis. Methods Enzymol. 513, 89–112 (2012)
Heckl, D. et al. Generation of mouse models of myeloid malignancy with combinatorial genetic lesions using CRISPR-Cas9 genome editing. Nature Biotechnol. 32, 941–946 (2014)
Heigwer, F., Kerr, G. & Boutros, M. E-CRISP: fast CRISPR target site identification. Nature Methods 11, 122–123 (2014)
Peto, R. & Pike, M. C. Conservatism of the approximation sigma (O-E)2-E in the logrank test for survival data or tumor incidence data. Biometrics 29, 579–584 (1973)
Acknowledgements
This work was funded by Spanish Ministry of Economy and Competitiveness through the Instituto de Salud Carlos III (ISCIII) and Red Temática de Investigación del Cáncer (RTICC). We are grateful to E. Santos for his continued support to this project, and N. Villahoz and M. C. Muro for their excellent work in the coordination of the CLL Spanish Consortium. C.L.-O. is an Investigator of the Botin Foundation supported by Banco Santander through its Santander Universities Global Division, and E.Ca. and D.T. are Institució Catalana de Recerca i Estudis Avançats-Academia investigators. We acknowledge Partnership for Advanced Computing in Europe (PRACE) for awarding us access to resource Marenostrum based in Spain at the BSC, the Pershing Square Sohn Cancer Research Alliance and European Union’s FP7 through the Blueprint Consortium. We are also very grateful to all patients with CLL who have participated in this study.
Author information
Authors and Affiliations
Contributions
The Chronic Lymphocytic Leukaemia Genome consortium contributed to this study as part of the International Cancer Genome Consortium. Investigator contributions are as follows: T.B., J.D., A.L.-G., A.R.P., M.G. and J.M.H.-R. contributed to sample collection and clinical annotation; M.R., N.V., E.Ca., E.Co., J.M.H.-R. and M.G. were the pathologists who reviewed and confirmed the diagnoses; P.N., C.M.R.-C. and M.A. prepared and supervised the bioethical requirements; M.P., A.E. and C.R. processed samples and performed validation analysis; M.G., I.G. and D.A.P. were responsible for generating libraries, performing exome capture and sequencing; S.B., D.To., M.M., S.G., I.S., G.C., D.M.-G., A.C., X.E. and D.Cos. analysed copy number alterations and structural variants; X.S.P., R.V.-M., J.G.-A. and V.Q. developed the bioinformatic pipeline for analysis of somatic mutations and performed functional data integration; D.Col., M.L.-G. and B.G. were responsible for downstream validation analysis and functional studies; A.N. and K.S. analysed IG gene rearrangements and stereotypes; J.I.M.-S., A.C.Q., G.C., R.B., R.G., N.R., H.G.S. and P.J. performed epigenetic and transcriptomic analysis and 4C-seq experiments; L.B. and A.A.F. performed enhancer analysis and CRISPR experiments; N.V., T.B., A.L.-G. and E.Ca. performed clinical and biological studies; J.L.G., R.R., M.O., D.G.P. and A.V. were in charge of bioinformatics data management; N.L.-B., C.R.-P. and D.Ta. contributed to pathway analysis and in silico prescription. X.S.P., C.L.-O. and E.Ca. directed the research, analysed the data and wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Extended data figures and tables
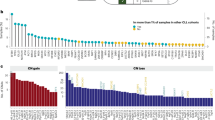
Extended Data Figure 1 Molecular characterization of CLL and MBL subtypes.
a, CLL and MBL cases are divided according to the somatic hypermutation mutational status of their clonotypic IGHV genes into IGHV-MUT (black) and IGHV-UNMUT (grey) subgroups. Clinical and molecular data from 506 cases profiled with four different platforms are shown. Chromosome 13 is shown in detail. Und, undetermined. b, Box plot showing the total number of somatic mutations identified in IGHV-MUT and IGHV-UNMUT cases by WGS (*P < 3 × 10−8). c, Main mutational signatures identified by WGS. d, Relationship between total number of mutations and contribution of signature 2 and the IGHV-status of tumours (red: IGHV-MUT; blue: IGHV-UNMUT; grey: undetermined).
Extended Data Figure 2 Distribution of CNAs and structural variants in 506 cases of CLL and MBL.
a, The total number of CNAs detected per case is indicated on top. Clinicobiological characteristics of patients (CLL/MBL and IGHV status) are shown on the middle row (MBL and IGHV-UNMUT depicted with green lines), together with the presence of chromothripsis. The main DNA copy number alterations identified are shown on the bottom. The presence of a deletion is indicated by a red line, homozygous deletion by a Bordeaux colour, blue lines indicate the presence of a gain, translocation t(14;18) is shown in green, grey lines represent the absence of alteration, and white lines indicate that no information is available for the t(14;18) for that particular case. b, Circular diagram representation of the distribution of structural variants detected in 148 WGS CLL samples. Displayed in the outer layer we show recurrence in CNAs, followed by all the breakpoints derived from large ( > 100 bp) intra- and inter-chromosomal rearrangements (dark blue) in the inner layer. For clarity, we have set the scale of CNAs to 20%, as the maximum, showing sequence gains and losses, as positive (blue) and negative (red) values, respectively. Rearrangements are displayed in absolute counts, indicating that the values in each of the regions do not reflect the recurrence among samples, as some regions with high values derive from one or two cases, normally with complex karyotypes. We highlighted with dashed squares those regions (3p21, 11q23, 13q14, 14q32 and 18q21) with rearrangements observed in more than 5% of cases with WGS. As to rearrangement events, of a total of 358 breakpoints were detected across all 148 samples, 41% of them correspond to interchromosomal translocations, while 59% occurred within chromosomes. Chromosomes 11 and 13 appear as the most rearranged, entailing 25% of all the breaks, followed by chromosomes 3 and 6 (with 8% each). Regarding interchromosomal rearrangements chromosomes 6, 8, 13 and 14 appear as the most translocated, being involved in 32% of all translocations observed. Recurrent breakpoints are indicated by arrows: black arrows for rearrangements affecting 18q21 and BCL2 (four cases with 14q32 and one case with 2p11) and blue arrows for rearrangements affecting 13q14 (nine cases with different chromosomes).
Extended Data Figure 3 Schematic view of the translocations involving BCL2 and patterns of complex structural variants in the WGS of a CLL case.
a, A total of nine translocations t(14;18)(q32;q21) were identified, resulting in the fusion of the IGH enhancer on the 3′ UTR of BCL2, as well as one translocation between the IGK locus on chromosome 2, t(2;18)(p11;q21), which affected the promoter region of BCL2. Cases with these translocations had multiple somatic mutations in the 5′-region of BCL2 (arrowheads and lollipops). RNA-seq data analysis revealed an allelic imbalance, with the rearranged allele usually much more expressed that the germline allele (pie-charts within lollipops showing in red the mutant allele fraction detected by RNA-seq for each somatic mutation), probably reflecting the effect of the translocation on the expression of BCL2 and recruitment of the SHM machinery to this locus. b, Gene expression analysis revealed that the presence of the t(14;18)(q32;q21) resulted in overexpression of BCL2 in these cases when compared with other CLL or MBL cases. c, FISH analysis of CLL cells from case 151 using a dual colour fusion probe for IGH (green) and BCL2 (red). Fusion signals are indicated with arrows. d, Case numbers and genomic coordinates for the detected translocations between immunoglobulin genes and BCL2. e, Circular representation of structural variants detected in six CLL tumours with complex rearrangements including four cases with chromoplexia (samples 16, 141, 294 and 753), chromothripsis (sample 880) and combined (sample 853). Chromosomes are represented in the outer layer, regions lost (red) and gained (blue) detected by SNP arrays are shown in the inner layer. Inter and intrachromosomal rearrangements are represented as black and blue lines, respectively. f, Reconstruction at base pair resolution of the resulting reorganized chromosomes in case 853 including der(X) in yellow, der(2) in dark blue, der(8) in green, and der(11) in red. In these reconstructions, only reorganized fragments larger than 100 bp are represented unless they involve interchromosomal translocations. Rearranged regions are not drawn to scale. Arrows denote inverted fragments relative to their normal and original orientation. Flanking portions of the derivative chromosomes without detected rearrangements are collapsed and shown as broken boxes. Estimated sizes (in Mb) for the resulting derivative chromosomes are shown on the left side, including the fraction (percentage) relative to the corresponding normal chromosome size. Asterisks indicate breakpoints that have been experimentally studied and verified. Genes disrupted by breakpoints are displayed on the left side of each of the proposed derivative chromosomes in purple. g, Whole-chromosome painting confirmed the sequencing reconstruction proposed in b. Simultaneous painting of chromosome 8 (green) and 11 (red) shows a normal chromosome 11 and a shorter chromosome der(11) as well as a normal chromosome 8 and der(8) that contains a fragment of chromosome 11 inserted below the centromeric region. In addition, a small fragment of chromosome 8 is detected in the telomeric region of derivative chromosome 2.
Extended Data Figure 4 Effect of activating mutations in the 3′ UTR non-coding region of NOTCH1.
a, Proportion of RNA-seq reads supporting an aberrant splicing in cases with or without mutations in the 3′ UTR of NOTCH1 (**P < 0.01). b, Immunohistochemistry of CLL cells with antibodies against NOTCH1 showing the nuclear accumulation of NOTCH1 in cells with coding or non-coding mutations in NOTCH1 (case numbers are indicated inside). Original magnification, ×100. c, Clinical and biological features of patients with NOTCH1 mutations. Characteristics of patients with truncating mutations in the coding region of NOTCH1, in the 3′ UTR of NOTCH1, or without mutations in NOTCH1 for Binet, ZAP70, CD38, IGHV status and trisomy 12.
Extended Data Figure 5 Effect of mutations in the PAX5 enhancer on gene expression.
Comparative analysis of gene expression between IGHV-MUT CLL tumours with or without (WT) mutations in the PAX5 enhancer for 15 genes located around the recurrently mutated enhancer in CLL and MBL samples.
Extended Data Figure 6 PAX5 enhancer deletion downregulates PAX5 expression in human B cell lines.
a, PCR analysis of CRISPR/Cas9 deletion of PAX5 enhancer in lymphoblastoid B cells (left) and RAMOS cells (right). b, Quantitative RT–PCR (RT–qPCR) analysis of PAX5 expression in PAX5 enhancer deleted lymphoblastoid B cells (left) and RAMOS cells (right). Bars represent mean relative PAX5 mRNA levels after normalization to GAPDH expression and relative to wild-type cells. Errors bars represent the s.d. between technical triplicates of CRISPR/Cas9-induced mutations in PAX5 enhancer in lymphoblastoid B cells (left) and RAMOS cells (right). c, PCR analysis of CRISPR/Cas9-introduced mutations in the PAX5 enhancer in lymphoblastoid B cells (left) and RAMOS cells (right). d, RT–qPCR analysis of PAX5 expression in PAX5-enhancer-mutated lymphoblastoid B cells (left) and RAMOS cells (right). Bars represent mean relative PAX5 mRNA levels after normalization to GAPDH expression and relative to wild-type cells. Error bars represent the s.d. between technical triplicates (*P < 0.05; **P < 0.01).
Extended Data Figure 7 Distribution of genetic, epigenetic and expression features in CLL.
Distribution of genetic features, family of IGHV rearrangements and BCR stereotypes in naive cell-like CLL cases, intermediate CLL and memory-cell-like CLL cases. a, Frequency of driver mutations. b, c, Copy number alterations (b) and contribution of signature 2 (c) according to the epigenetic classification (green: naive-like; red: memory-like; yellow: intermediate). MBL patients were excluded from this analysis. d, Usage of IGHV families. e, Proportion of cases with stereotyped IGHV sequences. f, Number of cases of each of the stereotyped subsets identified in our series. For the analysis shown in e and f, both CLL and MBL patients were merged. The asterisk on the top of the bars in a and b indicates that the frequency of the genetic feature is higher than expected by chance in one particular epigenetic subgroup (P < 0.05). CP, chromoplexy; CT, chromothripsis. g, Relationship between genetic and epigenetic alterations in CLL. Correlation between the total number of somatic mutations detected by WGS per case and the number of CpGs showing differential methylation per case as compared to naive B cells (r = 0.64, P < 0.001). h, Correlation between the contribution of signature 2 mutations and the number of differential CpGs as in a. Tumours are coloured according to their IGHV status. i, Comparative analysis of CLL and MBL. Principal component analysis of differential methylation (up) and gene expression (bottom) data derived from either CLL tumours or MBL samples, reveals that MBL samples usually clustered with their corresponding IGHV-status CLL samples.
Extended Data Figure 8 Kaplan–Meier plot of time to first treatment stratified by the type of aberration in ATM, BIRC3, TP53 and ZNF292 genes.
TTT curves of the 386 untreated patients with Binet stage A or B. Cases are stratified according to the gene mutation status: wild type (green line), mutated and mutated+deleted (Mut, blue line) or deleted (Del, red line). The log-rank P-;values comparing the mutated (blue line) and the deleted (red line) cases are shown.
Supplementary information
Supplementary Figures
This file contains Supplementary Figures 1-6. (PDF 11515 kb)
Supplementary Tables
This file contains Supplementary Tables 1 and 3-10. (XLSX 1825 kb)
Supplementary Table 2
This zipped file contains the files for Supplementary Table 2. (ZIP 2015 kb)
Rights and permissions
About this article
Cite this article
Puente, X., Beà, S., Valdés-Mas, R. et al. Non-coding recurrent mutations in chronic lymphocytic leukaemia. Nature 526, 519–524 (2015). https://doi.org/10.1038/nature14666
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nature14666
This article is cited by
-
CXCR4 overexpression in chronic lymphocytic leukemia associates with poorer prognosis: A prospective, single-center, observational study
Genes & Immunity (2024)
-
Targeting Pim kinases in hematological cancers: molecular and clinical review
Molecular Cancer (2023)
-
Chronic lymphocytic leukaemia/small lymphocytic lymphoma and mantle cell lymphoma: from early lesions to transformation
Virchows Archiv (2023)
-
Evolutionary history of transformation from chronic lymphocytic leukemia to Richter syndrome
Nature Medicine (2023)
-
Different prognostic impact of recurrent gene mutations in chronic lymphocytic leukemia depending on IGHV gene somatic hypermutation status: a study by ERIC in HARMONY
Leukemia (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.