Abstract
Secretion of C–C chemokine ligand 2 (CCL2) by mammary tumours recruits CCR2-expressing inflammatory monocytes to primary tumours and metastatic sites, and CCL2 neutralization in mice inhibits metastasis1 by retaining monocytes in the bone marrow. Here we report a paradoxical effect of CCL2 in four syngeneic mouse models of metastatic breast cancer. Surprisingly, interruption of CCL2 inhibition leads to an overshoot of metastases and accelerates death. This is the result of monocyte release from the bone marrow and enhancement of cancer cell mobilization from the primary tumour, as well as blood vessel formation and increased proliferation of metastatic cells in the lungs in an interleukin (IL)-6- and vascular endothelial growth factor (VEGF)-A-dependent manner. Notably, inhibition of CCL2 and IL-6 markedly reduced metastases and increased survival of the animals. CCL2 has been implicated in various neoplasias and adopted as a therapeutic target1,2,3. However, our results call for caution when considering anti-CCL2 agents as monotherapy in metastatic disease and highlight the tumour microenvironment as a critical determinant of successful anti-metastatic therapy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Qian, B. Z. et al. CCL2 recruits inflammatory monocytes to facilitate breast-tumour metastasis. Nature 475, 222–225 (2011)
Lu, X. & Kang, Y. Chemokine (C-C motif) ligand 2 engages CCR2+ stromal cells of monocytic origin to promote breast cancer metastasis to lung and bone. J. Biol. Chem. 284, 29087–29096 (2009)
Wolf, M. J. et al. Endothelial CCR2 signaling induced by colon carcinoma cells enables extravasation via the JAK2-Stat5 and p38MAPK pathway. Cancer Cell 22, 91–105 (2012)
Pietras, K. & Ostman, A. Hallmarks of cancer: interactions with the tumor stroma. Exp. Cell Res. 316, 1324–1331 (2010)
McAllister, S. S. & Weinberg, R. A. Tumor-host interactions: a far-reaching relationship. J. Clin. Oncol. 28, 4022–4028 (2010)
Hanahan, D. & Coussens, L. M. Accessories to the crime: functions of cells recruited to the tumor microenvironment. Cancer Cell 21, 309–322 (2012)
Karnoub, A. E. & Weinberg, R. A. Chemokine networks and breast cancer metastasis. Breast Dis. 26, 75–85 (2007)
Kleer, C. G., van Golen, K. L. & Merajver, S. D. Molecular biology of breast cancer metastasis. Inflammatory breast cancer: clinical syndrome and molecular determinants. Breast Cancer Res. 2, 423–429 (2000)
Palangie, T. et al. Prognostic factors in inflammatory breast cancer and therapeutic implications. Eur. J. Cancer 30, 921–927 (1994)
Ueno, T. et al. Significance of macrophage chemoattractant protein-1 in macrophage recruitment, angiogenesis, and survival in human breast cancer. Clin. Cancer Res. 6, 3282–3289 (2000)
Valković, T., Lucin, K., Krstulja, M., Dobi-Babic, R. & Jonjic, N. Expression of monocyte chemotactic protein-1 in human invasive ductal breast cancer. Pathol. Res. Pract. 194, 335–340 (1998)
Saji, H. et al. Significant correlation of monocyte chemoattractant protein-1 expression with neovascularization and progression of breast carcinoma. Cancer 92, 1085–1091 (2001)
Chavey, C. et al. Oestrogen receptor negative breast cancers exhibit high cytokine content. Breast Cancer Res. 9, R15 (2007)
Goede, V., Brogelli, L., Ziche, M. & Augustin, H. G. Induction of inflammatory angiogenesis by monocyte chemoattractant protein-1. Int. J. Cancer 82, 765–770 (1999)
Li, X. et al. A destructive cascade mediated by CCL2 facilitates prostate cancer growth in bone. Cancer Res. 69, 1685–1692 (2009)
Bonapace, L. et al. If you don’t look, you won’t see: intravital multiphoton imaging of primary and metastatic breast cancer. J. Mammary Gland Biol. Neoplasia 17, 125–129 (2012)
Strachan, D. C. et al. CSF1R inhibition delays cervical and mammary tumor growth in murine models by attenuating the turnover of tumor-associated macrophages and enhancing infiltration by CD8 T cells. OncoImmunology 2, e26968 (2013)
Nilsson, M. B., Langley, R. R. & Fidler, I. J. Interleukin-6, secreted by human ovarian carcinoma cells, is a potent proangiogenic cytokine. Cancer Res. 65, 10794–10800 (2005)
Wani, A. A., Jafarnejad, S. M., Zhou, J. & Li, G. Integrin-linked kinase regulates melanoma angiogenesis by activating NF-κB/interleukin-6 signaling pathway. Oncogene 30, 2778–2788 (2011)
Wei, D. et al. Stat3 activation regulates the expression of vascular endothelial growth factor and human pancreatic cancer angiogenesis and metastasis. Oncogene 22, 319–329 (2003)
Wei, L. H. et al. Interleukin-6 promotes cervical tumor growth by VEGF-dependent angiogenesis via a STAT3 pathway. Oncogene 22, 1517–1527 (2003)
The Cancer Genome Atlas Network. Comprehensive molecular portraits of human breast tumours. Nature 490, 61–70 (2012)
Zhu, J. et al. The UCSC Cancer Genomics Browser. Nature Methods 6, 239–240 (2009)
Goldman, M. et al. The UCSC Cancer Genomics Browser: update 2013. Nucleic Acids Res. 41, D949–D954 (2013)
Schmittgen, T. D. Real-time quantitative PCR. Methods 25, 383–385 (2001)
Aslakson, C. J. & Miller, F. R. Selective events in the metastatic process defined by analysis of the sequential dissemination of subpopulations of a mouse mammary tumor. Cancer Res. 52, 1399–1405 (1992)
Swirski, F. K. et al. Identification of splenic reservoir monocytes and their deployment to inflammatory sites. Science 325, 612–616 (2009)
Wyckoff, J., Gligorijevic, B., Entenberg, D., Segall, J. & Condeelis, J. High-resolution multiphoton imaging of tumors in vivo. Cold Spring Harb. Protoc. 2011, 1167–1184 (2011)
Abramoff, M. D., Magelhaes, P. J. & Ram, S. J. Image Processing with Image. J. Biophotonics Intl 11, 36–42 (2004)
Egawa, G. et al. Intravital analysis of vascular permeability in mice using two-photon microscopy. Sci. Rep. 3, 1932 (2013)
Acknowledgements
We thank R. L. Anderson, N. Hynes, and R. Cardiff for cell lines, R. Thierry and M. Kirschmann for scripts for immunohistochemistry and two-photon imaging analysis, M. Stadler and H.-R. Hotz for bioinformatics, H. Kohler for FACS and S. Bichet for technical support, H. Brinkhaus and P. Loetscher for helpful discussions, D. Dylan for the CSFR1 inhibitor, J. van Rheenen, J. Stein, J. Rietdorf, T. Oertner and S. Bundschuh for helping us set up the multiphoton intravital microscope, and the Bentires-Alj group for feedback. Research in the laboratory of M.B.-A. is supported by the Novartis Research Foundation, the European Research Council (243211-PTPsBDC), the Swiss Cancer League, the Swiss National Foundation, and the Krebsliga Beider Basel. M.-M.C. is supported by the FP7 Marie Curie Fellowship.
Author information
Authors and Affiliations
Contributions
L.B., M.-M.C., T.J. and M.B.-A. designed and performed most of the experiments and wrote the manuscript. K.D.M. and Z.V. performed human biopsy experiments. J.W., M.-M.C. and L.B. performed intravital imaging. All authors prepared the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Extended data figures and tables
Extended Data Figure 1 CCL2 is overexpressed in breast cancer.
a, Positive correlation between immunohistochemical staining score of CCL2 and the number of CD68-positive macrophages per high-power field in human biopsies (n = 30). P = 0.024; data were analysed using R with one-way ANOVA (assuming that the data are normally distributed). The box plot represents the first to the third quartile of the data. Thick line indicates median, the whiskers extend to the minimal and maximal values. b, Kaplan–Meier survival curves showing overall survival of breast cancer patients with high or low CCL2 expression. P = 0.0372, log-rank test. c, CCL2 expression in supernatants of murine breast cancer cell lines grown in vitro. Data are shown as means ± s.e.m., n = 3 wells, one representative of three independent experiments. d, CCL2 expression in sera of mice bearing the indicated tumours for 14 days. Data are shown as means ± s.e.m., n = 3 animals per group, one representative of two independent experiments. e, CCL2 levels in sera (left) and lung homogenate (right) from 4T1.2-tumour-bearing mice during anti-CCL2 or IgG treatment or 10 days after the cessation of treatment. Data are shown as means ± s.e.m., n = 5 mice per group, pooled data from two independent experiments. *P < 0.05, unpaired t-test.
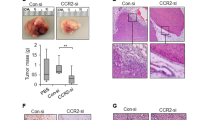
Extended Data Figure 2 Anti-CCL2 treatment reduces breast cancer metastases.
a, Tumour volumes on day 11 of treatment with anti-CCL2 or IgG. Data are shown as mean tumour volumes ± s.e.m., n = 10 mice, pooled data from two independent experiments. NS, not significant (unpaired t-test). b, Representative images of haematoxylin and eosin (H&E)-stained lung sections out of 20 images per group. Black circles indicate metastases. Scale bar, 500 μm. c, Quantification of metastases as percentage of metastatic area per lung area (left) or as metastatic area per lung section (right). Data are shown as means ± s.e.m. of 20 fields of view on 5 sections per animal, n = 4 mice per group, pooled data from two experiments. *P < 0.05, unpaired t-test. d, Effect of anti-CCL2 and IgG treatment on CTCs from tumour-bearing animals on day 11 of treatment. Data are shown as means ± s.e.m. of 20 fields of view on 5 sections per animal, n = 4 mice per group, pooled data from two experiments. *P < 0.05, unpaired t-test. e, Intravital multiphoton images of 4T1–GFP primary tumours on day 7 of treatment with anti-CCL2 antibody or IgG. Left, representative two-dimensional images out of 24 fields from primary tumours (green) 50 μm below the tumour surface, 24 min after intravenous injection of 70 kDa Texas Red–dextran (red). Scale bar, 100 μm. Right, mean numbers of motile tumour cells ± s.e.m. per 30 min acquisition, 6 fields per mouse, n = 4 mice per group. *P < 0.05, unpaired t-test. f, Intravital multiphoton images of vasculature in 4T1–GFP primary tumours on day 7 of treatment. Left, representative two-dimensional images out of 12 fields per group, 50 μm below the tumour surface, 15 min after intravenous injection of 70 kDa Texas Red–dextran (red). Scale bar, 100 μm. Right, mean number of dextran-positive blood vessels counted over 42 min, starting 15 min after injection of Texas Red–dextran. Results are shown as means ± s.e.m., n = 4 mice per group and 3 fields per animal. *P < 0.05, unpaired t-test. g, Left, representative images out of 12 images per group from α-SMA1-stained 4T1.2 tumour sections. Scale bar, 500 μm. Right, quantification of the perimeter of blood vessels covered by α-SMA1 staining. Data are shown as percentage vessel perimeter covered by α-SMA1 ± s.e.m. of 12 fields of view on 4 sections per animal, n = 3 mice per group, pooled data from two experiments. *P < 0.05, unpaired t-test.
Extended Data Figure 3 Macrophages decline in primary 4T1.2 tumours upon treatment with anti-CCL2.
a, Left, total number of SSClowCD11b+CD11c+CD206+MHCII+ macrophages. Right, percentage of CD11c+CD206+MHCII+ macrophages per SSClowCD11b+ cell population. Data are shown as means ± s.e.m., n = 3 mice. *P < 0.05, unpaired t-test. b, Left, total number of Texas-Red-positive SSClowCD11b+ macrophages. Right, percentage of Texas-Red-positive macrophages per SSClowCD11b+ cells, enumerated by flow cytometry of 4T1.2 primary tumours from tumour-bearing mice treated for 14 days, after intravenous injection of Texas Red–dextran. Data are shown as means ± s.e.m., n = 6 mice pooled data of two independent experiments. *P < 0.05, unpaired t-test. c, Concentration of hamster IgG in serum, lung homogenates and tumour during treatment (day 14) and at 10 days after cessation of treatment as detected by ELISA. Data are shown as means ± s.e.m., n = 4 mice per group. *P < 0.05, **P < 0.001, unpaired t-test.
Extended Data Figure 4 Cessation of anti-CCL2 treatment increases lung metastases.
a, Top, representative H&E-stained lung sections from 4T1.2- and Met-1-tumour-bearing mice 10 days after cessation of treatment. Scale bar, 500 µm. Bottom, quantification of lung metastases as percentage of metastatic area per lung area and metastatic area per lung section. Data are shown as means ± s.e.m. of 20 fields of view on 5 sections per animal, n = 4 mice per group, pooled data from two experiments. *P < 0.05, unpaired t-test. One representative image out of 20 is shown per group. b, Left, representative H&E-stained liver sections from 4T1.2-tumour-bearing mice 10 days after cessation of treatment. Scale bar, 500 µm. Right, quantification of liver metastases as metastatic area per lung section. Data are shown as means ± s.e.m. of n = 10 fields of view on 5 sections per animal, n = 2 mice per group. *P < 0.05, unpaired t-test. One representative image out of 10 is shown per group. c, d, 4T1.2-tumour-bearing animals were treated for 24 consecutive days with anti-CCL2 or IgG control. c, Left, representative images of H&E-stained lung sections. Scale bar, 500 μm. Right, lung metastases were quantified as percentage of metastatic area per lung area on day 24 of treatment. Data are shown as means ± s.e.m. of 20 fields of view on 5 lungs sections per animal, n = 4 mice per group. *P < 0.05, unpaired t-test. One representative image out of 20 is shown per group. d, Number of colonies formed by CTCs per ml blood collected on day 24 of treatment. Data are shown as means ± s.e.m. of n = 4 mice per group. *P < 0.05, unpaired t-test.
Extended Data Figure 5 CCL2 drives mutual attraction of monocytes and tumour cells.
a, Fluorescence-activated cell sorting (FACS) plots showing the gating strategy for identification and isolation of inflammatory monocytes. b, Transwell invasion assay of Met-1 cells (left) or 4T1 cells (right) on top of matrigel towards Ly6C+ monocytes (Mono). Data are shown as means of invading cell numbers ± s.e.m., n = 4 independent experiments with each experiment performed in triplicate. *P < 0.05, ANOVA with Bonferroni post-test. c, Transwell invasion assay of Ly6C+ monocytes on top of matrigel towards 4T1 (left) or Met-1 (right) cells. Data are shown as means of invading cell numbers ± s.e.m., n = 3 independent experiments with each experiment performed in triplicate. *P < 0.05, ANOVA with post-hoc Bonferroni correction.
Extended Data Figure 6 Distribution of inflammatory monocytes assessed by flow cytometry during and after treatment in vivo.
a, Top, quantification of Ly6C+Gr1+ monocytes as percentage of SSClowCD11b+ cells on day 14 of anti-CCL2 or IgG treatment and 10 days after treatment interruption in 4T1.2-tumour-bearing animals. Data are shown as means ± s.e.m., n = 8 mice, pooled data from two independent experiments. *P < 0.05, unpaired t-test. Bottom, quantification of total number of monocytes on day 14 of anti-CCL2 or IgG treatment and 10 days after treatment interruption in 4T1.2-tumour-bearing animals. Data are shown as means ± s.e.m., n = 8 mice, pooled data from two independent experiments. *P < 0.05, unpaired t-test. b, Top, quantification of monocytes as Ly6C+Gr1+ monocytes as percentage of SSClowCD11b+ cells on day 14 of anti-CCL2 or IgG treatment and 10 days after treatment interruption in Met-1-tumour-bearing animals. Data are shown as means ± s.e.m., n = 8 mice, pooled data from two independent experiments. *P < 0.05, unpaired t-test. Bottom, quantification of total number of monocytes on day 14 of anti-CCL2 or IgG treatment and 10 days after treatment interruption in 4T1.2-tumour-bearing animals. Data are shown as means ± s.e.m., n = 8 mice, pooled data from two independent experiments. *P < 0.05, unpaired t-test. c, Top left, representative images of Iba1-stained lung and tumour sections on day 14 of treatment. Bottom left, quantification of Iba1 staining. Total numbers of Iba1-positive cells are shown ± s.e.m. of 10 fields of view on 3 lungs sections per animal, n = 3 mice per group. Top right, representative images of Iba1-stained lung and tumour sections 10 days after cessation of the treatment. Bottom right, quantification of Iba1 staining. Total numbers of Iba1-positive cells are shown ± s.e.m. of 10 fields of view on 3 lung sections per animal, n = 3 mice per group. *P < 0.05, ANOVA with post-hoc Bonferroni correction. Scale bar, 100 µm. One representative image out of 10 is shown per group. NS, not significant.
Extended Data Figure 7 Recruitment of adoptively transferred CMTMR-labelled CCR2+ monocytes to the primary tumour and metastatic lung depends on CCL2.
a, Quantification of adoptively transferred CMTMR+ monocytes as total numbers or percentages of SSClowCD11b+ cells in different organs from tumour-bearing animals on day 7 of treatment. BM, bone marrow. Data are shown as means ± s.e.m., n = 5 mice per group, one representative of two independent experiments. *P < 0.05, unpaired t-test. b, Quantification of adoptively transferred CMTMR+ monocytes as total numbers or percentages of SSClowCD11b+ cells in different organs from tumour-bearing animals on day 7 after interruption of the treatments. Data are shown as means ± s.e.m., n = 3 mice per group, one representative of two independent experiments. *P < 0.05, unpaired t-test. NS, not significant.
Extended Data Figure 8 Monocytes support growth of tumour cells in vivo and in vitro.
a, Timeline of the experiments. b, Left, metastatic index in lungs from 4T1.2-tumour-bearing animals on day 24. Data are shown as means ± s.e.m., n = 4 mice per group, one representative of two independent experiments. *P < 0.05, unpaired t-test. Scale bar, 100 µm. Right, the number of tumour cell colonies per ml blood of tumour-bearing animals on day 24 and after removal of the primary tumour. Data are shown as means ± s.e.m., n = 4 mice per group, one representative of two independent experiments. *P < 0.05, unpaired t-test. c, Left, representative images of Iba1-stained lung sections in animals treated as in Extended Data Fig. 8a. Right, quantification of Iba1 staining on day 14 (last day of treatment and the day of tumour removal) and on day 24 (10 days after stopping treatment and tumour removal). Total numbers of Iba1-positive cells are shown ± s.e.m. of 10 fields of view on 3 lungs sections per animal, n = 3 mice per group. *P < 0.05, unpaired t-test. Scale bar, 100 µm. One representative image out of 10 is shown per group. d, Quantification of 4T1.2 cell viability using Trypan Blue 48 h after co-culture with sorted monocytes (Mono). Data are shown as means ± s.e.m., n = 3. *P < 0.05, unpaired t-test. e, Representative images of Iba1, CD31 and Ki67 staining of lung sections from animals treated with CSF1R inhibitor (CSF1Rinh) or vehicle (vhc) after treatment with anti-CCL2 or IgG control. One representative image out of 10 is shown per group.
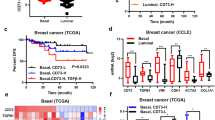
Extended Data Figure 9 Upregulation of CCL2 and IL-6 reduces overall survival in breast cancer patients.
a, Correlation between immunohistochemical score of CCL2 and number of CD31+ vessels per high-power field in biopsies from patients with breast carcinoma (n = 17), P = 0.031. Data were analysed using R with one-way ANOVA (assuming that the data are normally distributed). The box plot represents the first to the third quartile of the data. Thick line indicates median, the whiskers in the box plot extend to the minimal and maximal values. b, Cytokine array showing expression of IL-6 in the supernatant of mono- or co-cultures of 4T1.2 cells and primary monocytes, in the presence or absence of anti-CCL2. c, Quantification of IL-6 expression in cell supernatants of monocytes in mono- or co-culture with 4T1.2 by ELISA. Data are shown as means ± s.e.m., n = 4 independent experiments each with biological triplicates. *P < 0.05, ANOVA with post-hoc Bonferroni correction. d, IL-6 expression levels in primary tumours (left) or in serum (right) on day 14 of treatment and after cessation of treatment (day 24). Data are shown as means ± s.e.m., n = 6 mice per group, pooled data from two independent experiments. *P < 0.05, ANOVA with post-hoc Bonferroni correction. e, Left, Kaplan–Meier survival curves showing overall survival of 400 breast tumour patients expressing either low (blue) or high (red) IL-6 levels. *P < 0.045, log-rank test. Right, Kaplan–Meier survival curves showing overall survival of 148 patients with tumours expressing either CCL2 high/IL-6 low (blue) or CCL2 high/IL-6 high (red) levels. *P < 0.0017, log-rank test. f, Left, quantification of lung metastases. Metastatic area per lung section is shown ± s.e.m. of 20 fields of view on 5 lungs sections per animal, n = 4 mice per group. *P < 0.05, ANOVA with post-hoc Bonferroni correction. Right, number of colonies formed by CTCs per ml blood in animals treated as in Fig. 3c on day 24. Data are shown as means ± s.e.m., n = 10 mice per group, pooled data from two experiments. *P < 0.05, ANOVA with post-hoc Bonferroni correction. g, VEGF-A expression as measured by ELISA in serum from 4T1.2-tumour-bearing animals treated as in Fig. 3c. Data are shown as means ± s.e.m., n = 4 mice per group, pooled data from two experiments. *P < 0.05, ANOVA with post-hoc Bonferroni correction. NS, not significant.
Extended Data Figure 10 Monocytes/macrophages induce p-STAT3 in metastatic lungs upstream of VEGF-A expression.
a, Left, representative images of p-STAT3-stained lung sections from animals treated as in Fig. 4a. Scale bar, 100 µm. Right, quantification of p-STAT3 staining. Total numbers of p-STAT3-positive cells per field are shown ± s.e.m. of 10 fields of view on 3 lungs sections per animal, n = 3 mice per group. b, Left, representative images of p-STAT3-stained lung sections from animals treated as in Fig. 2c. Scale bar, 100 µm. Right, quantification of p-STAT3 staining. Total numbers of p-STAT3-positive cells per field are shown ± s.e.m. of 10 fields of view on 3 lungs sections per animal, n = 3 mice per group. CSF1Rinh, CSF1R inhibitor; vhc, vehicle. *P < 0.05, ANOVA with post-hoc Bonferroni correction. a, b, One representative image out of 10 is shown per group.
Supplementary information
Cancer cell motility in mice bearing 4T1-GFP tumors treated with IgG
A 30-min 2D time-lapse sequence of 4T1.2 GFP-labeled tumor cells (green) in a living mouse treated for 7 days with IgG. Imaging depth 35 m below the tumor capsule. Texas Red Dextran (red) injection and surgery were performed as described in Materials and Methods. Scale bar 100 μm. (MP4 1109 kb)
Cancer cell motility in mice bearing 4T1-GFP tumor treated with anti-CCL2
A 28-minute 2D time-lapse sequence of 4T1.2 GFP-labeled tumor cells (green) in a living mouse treated for 7 days with anti-CCL2 neutralizing antibody. Imaging depth 40 μm below the tumor capsule. Texas Red Dextran (red) injection and surgery were performed as described in the Materials and Methods section. Scale bar100 μm. (MP4 236 kb)
Rights and permissions
About this article
Cite this article
Bonapace, L., Coissieux, MM., Wyckoff, J. et al. Cessation of CCL2 inhibition accelerates breast cancer metastasis by promoting angiogenesis. Nature 515, 130–133 (2014). https://doi.org/10.1038/nature13862
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nature13862
This article is cited by
-
Fatty acid metabolism of immune cells: a new target of tumour immunotherapy
Cell Death Discovery (2024)
-
Effect of tumor-associated macrophages on the pyroptosis of breast cancer tumor cells
Cell Communication and Signaling (2023)
-
Roles of tumor-associated macrophages in anti-PD-1/PD-L1 immunotherapy for solid cancers
Molecular Cancer (2023)
-
The MYBL2–CCL2 axis promotes tumor progression and resistance to anti-PD-1 therapy in ovarian cancer by inducing immunosuppressive macrophages
Cancer Cell International (2023)
-
FAM171B stabilizes vimentin and enhances CCL2-mediated TAM infiltration to promote bladder cancer progression
Journal of Experimental & Clinical Cancer Research (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.