Abstract
Cutaneous melanoma is epidemiologically linked to ultraviolet radiation (UVR), but the molecular mechanisms by which UVR drives melanomagenesis remain unclear1,2. The most common somatic mutation in melanoma is a V600E substitution in BRAF, which is an early event3. To investigate how UVR accelerates oncogenic BRAF-driven melanomagenesis, we used a BRAF(V600E) mouse model. In mice expressing BRAF(V600E) in their melanocytes, a single dose of UVR that mimicked mild sunburn in humans induced clonal expansion of the melanocytes, and repeated doses of UVR increased melanoma burden. Here we show that sunscreen (UVA superior, UVB sun protection factor (SPF) 50) delayed the onset of UVR-driven melanoma, but only provided partial protection. The UVR-exposed tumours showed increased numbers of single nucleotide variants and we observed mutations (H39Y, S124F, R245C, R270C, C272G) in the Trp53 tumour suppressor in approximately 40% of cases. TP53 is an accepted UVR target in human non-melanoma skin cancer, but is not thought to have a major role in melanoma4. However, we show that, in mice, mutant Trp53 accelerated BRAF(V600E)-driven melanomagenesis, and that TP53 mutations are linked to evidence of UVR-induced DNA damage in human melanoma. Thus, we provide mechanistic insight into epidemiological data linking UVR to acquired naevi in humans5. Furthermore, we identify TP53/Trp53 as a UVR-target gene that cooperates with BRAF(V600E) to induce melanoma, providing molecular insight into how UVR accelerates melanomagenesis. Our study validates public health campaigns that promote sunscreen protection for individuals at risk of melanoma.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Change history
21 January 2015
A Correction to this paper has been published: https://doi.org/10.1038/nature14057
References
Whiteman, D. C. et al. Melanocytic nevi, solar keratoses, and divergent pathways to cutaneous melanoma. J. Natl. Cancer Inst. 95, 806–812 (2003)
Gilchrest, B. A., Eller, M. S., Geller, A. C. & Yaar, M. The pathogenesis of melanoma induced by ultraviolet radiation. N. Engl. J. Med. 340, 1341–1348 (1999)
Yeh, I., von Deimling, A. & Bastian, B. C. Clonal BRAF mutations in melanocytic nevi and initiating role of BRAF in melanocytic neoplasia. J. Natl. Cancer Inst. 105, 917–919 (2013)
Tsao, H., Chin, L., Garraway, L. A. & Fisher, D. E. Melanoma: from mutations to medicine. Genes Dev. 26, 1131–1155 (2012)
Harrison, S. L., MacLennan, R., Speare, R. & Wronski, I. Sun exposure and melanocytic naevi in young Australian children. Lancet 344, 1529–1532 (1994)
Dhomen, N. et al. Oncogenic Braf induces melanocyte senescence and melanoma in mice. Cancer Cell 15, 294–303 (2009)
Pontén, F., Berne, B., Ren, Z. P., Nister, M. & Ponten, J. Ultraviolet light induces expression of p53 and p21 in human skin: effect of sunscreen and constitutive p21 expression in skin appendages. J. Invest. Dermatol. 105, 402–406 (1995)
Rudolph, P., Tronnier, M., Menzel, R., Moller, M. & Parwaresch, R. Enhanced expression of Ki-67, topoisomerase IIα, PCNA, p53 and p21WAF1/Cip1 reflecting proliferation and repair activity in UV-irradiated melanocytic nevi. Hum. Pathol. 29, 1480–1487 (1998)
Pollock, P. M. et al. High frequency of BRAF mutations in nevi. Nature Genet. 33, 19–20 (2002)
Thomas, N. E. et al. Number of nevi and early-life ambient UV exposure are associated with BRAF-mutant melanoma. Cancer Epidemiol. Biomarkers Prev. 16, 991–997 (2007)
Vultur, A. & Herlyn, M. SnapShot: melanoma. Cancer Cell 23, 706 (2013)
Pfeifer, G. P., You, Y. H. & Besaratinia, A. Mutations induced by ultraviolet light. Mutat. Res. 571, 19–31 (2005)
Kato, S. et al. Understanding the function–structure and function–mutation relationships of p53 tumor suppressor protein by high-resolution missense mutation analysis. Proc. Natl Acad. Sci. USA 100, 8424–8429 (2003)
Song, H., Hollstein, M. & Xu, Y. p53 gain-of-function cancer mutants induce genetic instability by inactivating ATM. Nature Cell Biol. 9, 573–580 (2007)
Willis, A., Jung, E. J., Wakefield, T. & Chen, X. Mutant p53 exerts a dominant negative effect by preventing wild-type p53 from binding to the promoter of its target genes. Oncogene 23, 2330–2338 (2004)
Olive, K. P. et al. Mutant p53 gain of function in two mouse models of Li-Fraumeni syndrome. Cell 119, 847–860 (2004)
Dankort, D. et al. BrafV600E cooperates with Pten loss to induce metastatic melanoma. Nature Genet. 41, 544–552 (2009)
Hodis, E. et al. A landscape of driver mutations in melanoma. Cell 150, 251–263 (2012)
Krauthammer, M. et al. Exome sequencing identifies recurrent somatic RAC1 mutations in melanoma. Nature Genet. 44, 1006–1014 (2012)
Patton, E. E. & Zon, L. I. Taking human cancer genes to the fish: a transgenic model of melanoma in zebrafish. Zebrafish 1, 363–368 (2005)
Goel, V. K. et al. Melanocytic nevus-like hyperplasia and melanoma in transgenic BRAFV600E mice. Oncogene 28, 2289–2298 (2009)
Bald, T. et al. Ultraviolet-radiation-induced inflammation promotes angiotropism and metastasis in melanoma. Nature 507, 109–113 (2014)
Noonan, F. P. et al. Neonatal sunburn and melanoma in mice. Nature 413, 271–272 (2001)
Luo, C. et al. Loss of ARF sensitizes transgenic BRAFV600E mice to UV-induced melanoma via suppression of XPC. Cancer Res. 73, 4337–4348 (2013)
Zaidi, M. R. et al. Interferon-γ links ultraviolet radiation to melanomagenesis in mice. Nature 469, 548–553 (2011)
Green, A. et al. Daily sunscreen application and betacarotene supplementation in prevention of basal-cell and squamous-cell carcinomas of the skin: a randomised controlled trial. Lancet 354, 723–729 (1999)
Green, A. C., Williams, G. M., Logan, V. & Strutton, G. M. Reduced melanoma after regular sunscreen use: randomized trial follow-up. J. Clin. Oncol. 29, 257–263 (2011)
Goldenhersh, M. A. & Koslowsky, M. Increased melanoma after regular sunscreen use? J. Clin. Oncol. 29, e557–e558 (2011)
Planta, M. B. Sunscreen and melanoma: is our prevention message correct? J. Am. Board Fam. Med. 24, 735–739 (2011)
Viros, A. et al. Improving melanoma classification by integrating genetic and morphologic features. PLoS Med. 5, e120 (2008)
Workman, P. et al. Guidelines for the welfare and use of animals in cancer research. Br. J. Cancer 102, 1555–1577 (2010)
Li, H. & Durbin, R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25, 1754–1760 (2009)
McKenna, A. et al. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 20, 1297–1303 (2010)
Li, H. et al. The Sequence Alignment/Map format and SAMtools. Bioinformatics 25, 2078–2079 (2009)
Koboldt, D. C. et al. VarScan 2: somatic mutation and copy number alteration discovery in cancer by exome sequencing. Genome Res. 22, 568–576 (2012)
Larson, D. E. et al. SomaticSniper: identification of somatic point mutations in whole genome sequencing data. Bioinformatics 28, 311–317 (2012)
McLaren, W. et al. Deriving the consequences of genomic variants with the Ensembl API and SNP Effect Predictor. Bioinformatics 26, 2069–2070 (2010)
Turajlic, S. et al. Whole genome sequencing of matched primary and metastatic acral melanomas. Genome Res. 22, 196–207 (2012)
Acknowledgements
This work was supported by Cancer Research UK (C107/A10433; C5759/A12328; A13540; A17240), the Wenner-Gren Foundations, Stockholm, Teggerstiftelsen (M.P.) and a FEBS Long-Term Fellowship (B.S.-L.). We thank G. Ashton for technical assistance and A. Young for helpful discussions. We would like to acknowledge the contribution of the melanoma specimen donors and research groups to The Cancer Genome Atlas.
Author information
Authors and Affiliations
Contributions
A.V., B.S.-L. and R.M. designed the study, analysed the data and wrote the paper. M.P. designed and performed experiments and analysed data. S.J.F. designed and performed bioinformatics analysis and analysed data. K.H., J.R., M.R.G., M.C. and N.D. performed experiments. S.E. validated WES SNVs.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Extended data figures and tables
Extended Data Figure 1 Methodology and UVR spectrum.
a, Schematic representation of experimental schedule, showing induction of BRAF(V600E) by tamoxifen at ∼8 weeks of age followed by weekly exposure to UVR starting 4 weeks later, and for up to 6 months. b, Graph showing spectral radiation distribution for the Waldmann UV6 lamp used in these studies. The UVA and UVB regions are indicated. c, Photomicrograph of Trp53 staining in interfollicular and follicular keratinocytes (arrows) 24 h after UVR exposure. Asterisks indicate hair follicles. Scale bar, 50 μm.
Extended Data Figure 2 UVR induced melanocytic proliferation in BRAF(V600E) mice.
Photomicrographs showing 4′,6-diamidino-2-phenylindole (DAPI), S100 and Ki-67 immunofluorescence staining, together with a merged image in cloth-protected and UVR-exposed areas of the mid-dermis from BRAF(V600E) mice 72 h after UVR exposure. The experiment was repeated in 3 different skin sections of 5 animals. Scale bar, 30 μm.
Extended Data Figure 3 UVR induces naevogenesis in BRAF(V600E) mice.
a, Schematic representation of experimental processing of mouse skin. Three skin sections (long rectangular boxes) were cut perpendicular to the longitudinal axis of the mice to span the UVR-exposed and protected areas (as marked by the dotted line) of the tamoxifen-treated shaved area (pink). b, Photomicrograph of H&E-stained representative skin from the protected and UVR-exposed skin of a tamoxifen-treated BRAF(V600E) mouse subjected to UVR exposure and examined at 7 days (n = 5). Dotted line: UVR treatment line demarcation. Scale bar, 0.4 mm. c, Photomicrograph of H&E-stained skin from the boxed black area in b, showing the cloth-protected skin of a tamoxifen-treated BRAF(V600E) mouse subjected to UVR exposure and examined at 7 days. Black boxes show individual naevi. Double-headed arrow shows example of maximum diameter of a single naevus. Scale bar, 300 µm. d, Photomicrograph of H&E-stained skin from the dashed boxed black area in b, showing the UVR-exposed skin of a tamoxifen-treated BRAF(V600E) mouse subjected to UVR exposure and examined at 7 days. Black boxes show individual naevi. Scale bar, 300 µm. e, Photomicrograph of H&E-stained skin from the cloth-protected and UVR-exposed skin of a tamoxifen-treated CreERT2 control mouse subjected to weekly UVR exposure for 6 months. Scale bar, 300 µm. f, Photograph showing macroscopic appearance of protected and UVR-exposed skin from the tamoxifen-treated CreERT2 control mouse shown in a. Original magnification, ×2.
Extended Data Figure 4 UVR-accelerated BRAF(V600E)-driven tumours have similar histology to BRAF(V600E)-driven tumours from non-UVR-exposed animals.
a, Photomicrograph of an H&E-stained tumour from a UVR-treated BRAF(V600E) mouse highlighting the presence of atypical heterogeneous spindle dendritic and pigment-producing cells (black asterisks and arrow respectively, left panel) and atypical plump spindle cells and mitotic figures (white asterisks and black arrowhead respectively, right panel). Scale bar, 25 µm. b, Photomicrograph of an H&E-stained tumour from a UVR-treated BRAF(V600E) mouse highlighting a region of dermal ulceration (black arrow). Scale bar, 0.5 mm. c, Photomicrograph of H&E-stained tumours from non-UVR exposed (left panel) and UVR-exposed (right panel) BRAF(V600E) mice, showing the presence of nuclear pleomorphism (asterisks) in both tumours. Scale bar, 10 µm. d, Photomicrograph of an S100-stained tumour from a UVR-exposed BRAF(V600E) mouse. Scale bar, 100 µm. e, Photomicrograph of an HMB-45/MelanA-stained tumour from a UVR-exposed BRAF(V600E) mouse. Scale bar, 50 µm. f, Photomicrograph of a Ki-67-stained tumour from a UVR-exposed BRAF(V600E) mouse. Scale bar, 50 µm.
Extended Data Figure 5 Sunscreen blocks the short-term effects of UVR exposure.
a, Photomicrograph showing lack of Trp53 staining in the cloth-protected (Protected) and UVR-exposed, sunscreen-protected (UVR+SS) skin of a BRAF(V600E) mouse after 24 h of UVR exposure (n = 5). Scale bar, 40 µm. b, Photomicrograph of H&E-stained skin from the cloth protected (Protected) and UVR-exposed, sunscreen-protected (UVR+SS) regions of a BRAF(V600E) mouse after 24 h of UVR exposure. Scale bar, 300 µm. c, High-magnification photomicrograph of H&E-stained skin from the cloth protected (Protected) and UVR-exposed sunscreen-protected (UVR+SS) regions of a BRAF(V600E) mouse after 24 h of UVR exposure showing absence of apoptotic keratinocytes. d, Photomicrograph of H&E-stained skin from a cloth-protected (Protected; left), UVA-exposed (UVA; centre), and UVA-exposed, sunscreen-protected (UVA+SS; right) skin of a mouse after 72 h of UVR exposure. Scale bar, 300 µm (n = 5). The photomicrographs below the main images show areas of higher magnification of the images above. Asterisk indicates epidermal hypertrophy; D indicates plump collagen bundles densely located in the dermis. Scale bar, 150 µm.
Extended Data Figure 6 UVA-induced epidermal and dermal thickening after UVA radiation is abrogated by the use of sunscreen.
a, Photomicrographs of H&E-stained epidermis from the cloth-protected (Protected) and UVR-exposed, sunscreen-protected (UVR+SS) skin of a BRAF(V600E) mouse 7 days (d) after UVR exposure showing the similarity in the number and size of naevi in the two regions (n = 5). Scale bar, 300 µm. b, Photographs showing the macroscopic appearance of the cloth-protected (Protected) and UVR-exposed, sunscreen-protected (UVR+SS) skin from a BRAF(V600E) mouse 5 months after UVR. c, Photomicrographs of S100, HMB-45/MelanA- and Ki-67-stained tumours from UVR-exposed, sunscreen-protected (UVR+SS) mice. Scale bar, 50 µm.
Extended Data Figure 7 Tumours with a Trp53/TP53 mutation.
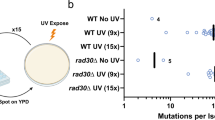
a, Boxplot graph showing median number of SNVs per Mb (SNVs per Mb) in UVR-exposed mutant Trp53, or UVR-exposed wild-type Trp53 (WT-Trp53) tumours. NS, not significant (Mann–Whitney test). b, Photomicrographs of S100, HMB-45/MelanA- and Ki-67-stained tumour sections from a BRAF(V600E)/Trp53(R172H) mouse. Scale bar, 50 µm. c, Kaplan–Meier plot showing melanoma-free survival in control mice (CreERT2; black line); BRAF(V600E) mice (BRAF(V600E) blue line); and BRAF(V600E) mice crossed with PTENflox/+ mice (BRAF(V600E)/ PTENflox/+; orange line). d, Boxplot graphs showing proportion of C-to-T (G-to-A) transitions in human primary melanomas from the TCGA data set (left panel), human metastatic melanomas from the TCGA data set (middle) and human metastatic melanomas from the Yale University data set (right) harbouring wild-type TP53 (TP53 WT) or mutations in TP53 (TP53 mut); WSRT.
Supplementary information
Supplementary Table
This file contains Supplementary Table 1. (XLS 1140 kb)
Rights and permissions
About this article
Cite this article
Viros, A., Sanchez-Laorden, B., Pedersen, M. et al. Ultraviolet radiation accelerates BRAF-driven melanomagenesis by targeting TP53. Nature 511, 478–482 (2014). https://doi.org/10.1038/nature13298
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nature13298
This article is cited by
-
The journey from melanocytes to melanoma
Nature Reviews Cancer (2023)
-
A Cicada Antimicrobial Peptide, Cryptonin, Exhibits Potent Antitumor Activity by Necrosis on Human Melanoma Cells
International Journal of Peptide Research and Therapeutics (2023)
-
Targeting anti-apoptotic pathways eliminates senescent melanocytes and leads to nevi regression
Nature Communications (2022)
-
Inactivation of the Hippo tumor suppressor pathway promotes melanoma
Nature Communications (2022)
-
Ultraviolet light-induced collagen degradation inhibits melanoma invasion
Nature Communications (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.