Abstract
Despite the introduction of antiproliferative drug-eluting stents, coronary heart disease remains the leading cause of death in the United States1. In-stent restenosis and bypass graft failure are characterized by excessive smooth muscle cell (SMC) proliferation2,3 and concomitant myointima formation with luminal obliteration. Here we show that during the development of myointimal hyperplasia in human arteries, SMCs show hyperpolarization of their mitochondrial membrane potential (ΔΨm) and acquire a temporary state with a high proliferative rate and resistance to apoptosis. Pyruvate dehydrogenase kinase isoform 2 (PDK2) was identified as a key regulatory protein, and its activation proved necessary for relevant myointima formation. Pharmacologic PDK2 blockade with dichloroacetate or lentiviral PDK2 knockdown prevented ΔΨm hyperpolarization, facilitated apoptosis and reduced myointima formation in injured human mammary and coronary arteries, rat aortas, rabbit iliac arteries and swine (pig) coronary arteries. In contrast to several commonly used antiproliferative drugs, dichloroacetate did not prevent vessel re-endothelialization. Targeting myointimal ΔΨm and alleviating apoptosis resistance is a novel strategy for the prevention of proliferative vascular diseases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Lloyd-Jones, D. et al. Heart disease and stroke statistics—2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 119, 480–486 (2009)
Dzau, V. J., Braun-Dullaeus, R. C. & Sedding, D. G. Vascular proliferation and atherosclerosis: new perspectives and therapeutic strategies. Nature Med. 8, 1249–1256 (2002)
Novak, K. Cardiovascular disease increasing in developing countries. Nature Med. 4, 989–990 (1998)
Green, D. R. & Reed, J. C. Mitochondria and apoptosis. Science 281, 1309–1312 (1998)
Hengartner, M. O. The biochemistry of apoptosis. Nature 407, 770–776 (2000)
Zamzami, N. & Kroemer, G. The mitochondrion in apoptosis: how Pandora’s box opens. Nature Rev. Mol. Cell Biol. 2, 67–71 (2001)
Halestrap, A. P. What is the mitochondrial permeability transition pore? J. Mol. Cell. Cardiol. 46, 821–831 (2009)
Bonnet, S. et al. A mitochondria–K+ channel axis is suppressed in cancer and its normalization promotes apoptosis and inhibits cancer growth. Cancer Cell 11, 37–51 (2007)
Bernardi, P. Modulation of the mitochondrial cyclosporin A-sensitive permeability transition pore by the proton electrochemical gradient. Evidence that the pore can be opened by membrane depolarization. J. Biol. Chem. 267, 8834–8839 (1992)
Roche, T. E. & Hiromasa, Y. Pyruvate dehydrogenase kinase regulatory mechanisms and inhibition in treating diabetes, heart ischemia, and cancer. Cell. Mol. Life Sci. 64, 830–849 (2007)
Azoulay-Zohar, H., Israelson, A., Abu-Hamad, S. & Shoshan-Barmatz, V. In self-defence: hexokinase promotes voltage-dependent anion channel closure and prevents mitochondria-mediated apoptotic cell death. Biochem. J. 377, 347–355 (2004)
Pastorino, J. G., Shulga, N. & Hoek, J. B. Mitochondrial binding of hexokinase II inhibits Bax-induced cytochrome c release and apoptosis. J. Biol. Chem. 277, 7610–7618 (2002)
Clarke, M. C. et al. Apoptosis of vascular smooth muscle cells induces features of plaque vulnerability in atherosclerosis. Nature Med. 12, 1075–1080 (2006)
Bernal-Mizrachi, C. et al. Vascular respiratory uncoupling increases blood pressure and atherosclerosis. Nature 435, 502–506 (2005)
Mitra, A. K., Del Core, M. G. & Agrawal, D. K. Cells, cytokines and cellular immunity in the pathogenesis of fibroproliferative vasculopathies. Can. J. Physiol. Pharmacol. 83, 701–715 (2005)
Newby, A. C. & Zaltsman, A. B. Molecular mechanisms in intimal hyperplasia. J. Pathol. 190, 300–309 (2000)
Acknowledgements
We thank C. Pahrmann for performing all cell cultures and for her technical assistance. We thank J. Thoms for performing immunoblots, H. Wiebold for assistance in organ chamber experiments, J. Lyons and her team for her assistance with the swine study, and S. Ehret, A. Deng and M. Resch for their technical assistance. We thank the UKE Imaging Facility (UMIF, B. Zobiak) and the UKE Animal Facility. Ethicon (Norderstedt, Germany) provided surgical suture materials. We also thank A. Treszl and G. Schoen for their statistical analyses. This study was funded by the German Research Foundation (Deutsche Forschungsgemeinschaft (DFG), SCHR992/3-1 and SCHR992/4-1 to S.S.), the International Society for Heart and Lung Transplantation (ISHLT, to S.S.), the Förderverein des Universitären Herzzentrums Hamburg (to S.S.), the Hermann and Lilly Schilling Foundation (to C.K.), the MINECO (SAF2013-41177-R, to J.P.B.) and the NIH (NIH 1R01HL105299, to P.S.T.).
Author information
Authors and Affiliations
Contributions
T.D. designed the studies, performed surgical procedures, analysed the data and wrote the manuscript. X.H. and D.W. performed confocal immunofluorescence, immunohistochemistry, TMRM assays in vivo and in vitro, endothelial cell assays, the histopathological studies, analysed data and edited the manuscript. L.M. participated in designing experiments, analysed data, edited the manuscript and secured funding. J.H., L.S., J.P.B., A.R., J.M.S. and C.K. participated in designing experiments, analysed data and edited the manuscript. M.S. performed surgical procedures in rats, contributed to molecular biology experiments and flow cytometry. F.I. and A.Y. contributed to the swine coronary artery procedures and edited the manuscript. F.L. contributed to human coronary artery pathohistology data. T.Z. performed organ chamber experiments. L.S.-U. and R.K. contributed to the rabbit experiments. A.S. performed PCR experiments and analysed data. R.I. performed histology and immunological experiments. F.H. edited the manuscript. T.E., S.B. and H.R. edited the manuscript. J.V. performed histologic analyses. R.C.R. contributed to the study design and edited the manuscript. P.S.T. designed experiments, analysed data and edited the manuscript. S.S. designed the studies, performed surgical procedures in rats and rabbits, ran molecular biology experiments in vitro and in vivo, edited the manuscript and secured the funding.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Extended data figures and tables
Extended Data Figure 1 Myointima formation in balloon-injured rat aortas.
a, b, Forty-eight hours after mechanical injury, trichrome (a) and immunofluorescence for SMC-markers (b) identified abundant SMCs in the aortic media. c, The infiltrate at 48 h was composed of CD68+ macrophages, some MPO+ neutrophils, and no CD3+ lymphocytes. d, Phosphorylation of AKT (pAKT), and ERK1 and ERK2 (pERK1/2), was markedly increased as early as 30 min after injury (mean ± s.d., n = 6 animals per group, control after 30 min normalized to healthy media, one-sample t-tests). e, Media cells of injured aortas showed ΔΨm hyperpolarization after 48 h (mean ± s.d., n = 4 animals (healthy media), 6 animals (control after 48 h), Student’s t-test). f, g, A myointima developed over 28 days in injured rat aortas (f, trichrome) and caused luminal obliteration (g, mean ± s.d., n = 5 animals (day 0), 4 animals (day 7), 6 animals (day 28), ANOVA with Bonferroni’s post-hoc test). h, Many infiltrating macrophages and very few neutrophils were observed in the myointima at 7 days. Leukocyte infiltration was sparse at 28 days; no lymphocytes were found (black arrows, internal elastic lamina). i, Tissue IFNγ, MCP-1, MIP-3α, and IL-1β levels were markedly increased at 7 days and were diminished after 28 days (mean ± s.d., n = 3 animals (day 0), 4 animals (day 7 and 28), days 7 and 28 normalized to day 0, one-sample t-test (day 0 versus day 7), Student’s t-test (day 7 versus day 28)). *P < 0.05; **P < 0.01.
Extended Data Figure 2 Characterization of the human internal mammary artery model.
a, b, Sections were co-stained for the SMC markers smoothelin, SM22, and calponin (a) or SMA, smooth muscle myosin (SM) heavy chain and myocardin (b). Co-localization could be observed in the merged pictures (white arrows, internal elastic lamina, pictures are representative of two replicates). Direct comparison between the HMA myointima on day 28 with the myointima in diseased human coronary artery (HCA) samples illustrated close similarities in immunofluorescence morphology. c, The human origin of myointimal cells in 21-day control HMAs was confirmed. Trichrome showed the development of a cell-rich myointima with mild fibrosis. Specimens were stained for SMA, DAPI and human leukocyte antigen class I (HLA I, upper row) or rat major histocompatibility complex class I (rat MHC I, lower row). Cells expressing SMA (red) co-expressed HLA I (green), which resulted in a yellow staining in the merged picture. No co-expression of SMA and rat MHC I was observed.
Extended Data Figure 3 The central role for PDGF in advancing myointima formation.
a, After 28 days, non-denuded HMAs in RNU rats showed only minor myointimal lesions (trichrome, mean ± s.d., n = 5 animals). b, To evaluate a possible rejection process in the xenogeneic HMA setting, host immune activation and graft infiltration were assessed. In the HMA model, xenogeneic HMA were transplanted into RNU rats (middle column). Xenogeneic HMA transplants into immunocompetent hosts (Brown Norway rats; BN, left column) and syngeneic RNU aortic transplants into RNU recipients (right column) served as controls; all analyses were performed after 7 days. Para-aortic BN lymph nodes harboured huge amounts of CD3+ lymphocytes, whereas the number was low in RNU lymph nodes. In IFNγ-Elispot assays with homogenized graft cells and recipient splenocytes, only BN recipients showed strong immune activation, whereas RNU recipients failed to mount a relevant immune response (box 25th to 75th percentile with median, whiskers min–max, quadruplicates of 5 animals (columns 1 and 2) and 4 animals (column 3), ANOVA with Bonferroni’s post-hoc test). Dense CD3+ infiltrates were found in HMA grafts of BN recipients, but not in HMA or RNU aortic grafts in RNU recipients. c, Immunohistochemistry identified myointimal macrophages and neutrophils in HMA control specimens on day 7 and reduced leukocyte infiltration in control specimens on day 28. Lymphocytes were not observed (black arrows, internal elastic lamina). d, HMA tissue levels of the inflammatory cytokines IFNγ, MCP-1, MIP-3α, and IL-1β were elevated during the first 14 days (mean ± s.d., n = 3 animals per group, ANOVA with Bonferroni’s post-hoc test). e, In HMA day 21 vessels, spatial differences of SMC ΔΨm with higher TMRM fluorescence in the luminal areas compared to the areas adjacent to the media were observed. SMC proliferation also mainly occurred in these luminal regions of elevated ΔΨm. DIC, differential interference contrast. f, Tissue PDGF was increased in HMA after injury and peaked after 14 days (mean ± s.d., n = 3 animals per time point, ANOVA with Bonferroni’s post-hoc test). g, Compared to untreated control vessels at day 28 in the rat aortic balloon injury model (Extended Data Fig. 1g), imatinib (PDGF-R blocker)-treated 28-day vessels showed only minor lesions (mean ± s.d., n = 8 animals). *P < 0.05; **P < 0.01.
Extended Data Figure 4 SMC characterization and response to PDGF.
a, b, Cells isolated from fresh HMA were positive for SMA, myocardin, smoothelin, calponin, and SM22α (SM22) as detected by FACS (a, pictures are representative of three replicates) and immunofluorescence (b, pictures are representative of three replicates). Thus, cells were identified as SMCs, but we cannot rule out that cells from other sources (for example, vessel wall stem cells with smooth muscle characteristics) were also involved. c, ΔΨm hyperpolarization, a phenomenon observed at times of maximized net proliferative activity in HMA (Fig. 1f), could be linked to PDGF. When SMCs were incubated with PDGF, ΔΨm hyperpolarization steadily increased over time, reaching its maximum after 48 h (mean ± s.d., 5 replicates of 2 (15 min, 2 h) or 3 (all other groups) independent experiments, ANOVA with Bonferroni’s post-hoc test). d, We found a significant downregulation of c-KIT, SMA and SM22 mRNA versus GAPDH mRNA after incubation with PDGF, all maturity markers for contractile SMCs (mean ± s.d., 13 independent experiments, Student’s t-test). Western blot analysis further revealed a downregulation of myocardin and confirmed SMA reduction. In contrast, SMemb, the embryonic form of smooth muscle myosin heavy chain and a marker for dedifferentiated SMCs, was increased, indicating a PDGF-induced phenotype switch (mean ± s.d., 5 (myocardin and SMA) and 6 (SMemb) independent experiments, PDGF normalized to control, one-sample t-tests). *P < 0.05; **P < 0.01.
Extended Data Figure 5 DCA reduces ΔΨm hyperpolarization and facilitates apoptosis in SMCs.
a, To assess the kinetics of DCA action in vitro, SMCs were pre-incubated with DCA for different time periods and then stimulated with PDGF for 48 h (mean ± s.d., 10 replicates of 3 independent experiments per group, ANOVA with Bonferroni’s post-hoc test). DCA reduced PDGF-induced ΔΨm hyperpolarization irrespective of the pre-incubation period. b, Atherosclerotic plaques from heavily calcified and atherosclerotic human coronary arteries were scraped off the media and cultured in SMC medium. Outgrowing SMCs were picked and expanded. PDGF significantly increased ΔΨm, an effect that was prevented by DCA (mean ± s.d., 10 replicates of 3 independent experiments, ANOVA with Bonferroni’s post-hoc test). c–e, Apoptosis induction with staurosporine significantly increased the number of control SMCs that showed cytochrome C leakage, as identified by diffuse cytochrome C staining throughout the cell (c, mean ± s.d., 10 replicates of 2 independent experiments per group, ANOVA with Bonferroni’s post-hoc test). PDGF significantly reduced cytochrome C release in SMCs and DCA counteracted this PDGF effect. Cytoplasmatic (C) and mitochondrial fractions (M) were isolated for immunoblotting (d, data are representative of 3 independent experiments). Separation was confirmed by the contents of mitochondrial complex V (CV) and cytosolic GAPDH. Cytochrome C was retained inside the mitochondria in control SMCs and was released with staurosporine. PDGF reduced the cytoplasmatic fraction, indicating reduced cytochrome C release, and DCA reversed the PDGF effect. SMC apoptosis was detected by TUNEL staining (e, mean ± s.d., 10 replicates of 2 (column 1) or 3 (columns 2–4) independent experiments, ANOVA with Bonferroni’s post-hoc test). Staurosporine significantly increased the number of apoptotic control SMCs. PDGF treatment decreased the percentage of apoptotic SMCs and DCA reversed this anti-apoptotic effect. *P < 0.05; **P < 0.01.
Extended Data Figure 6 DCA lowers medial and myointimal ΔΨm and facilitates apoptosis in balloon-injured rat aortas.
a, b, Trichrome (a) and immunofluorescence (b) confirmed abundant SMCs in the aortic media of DCA-treated animals 48h after injury. c, Similar to control vessels, the infiltrate mainly contained macrophages and neutrophils, but no CD3+ lymphocytes. d, DCA reduced ΔΨm of medial cells (mean ± s.d., n = 6 animals (control at 48 h) and 4 animals (DCA at 48 h), Student’s t-test). e, Macrophages were the main inflammatory cell population in the developing myointima of immunocompetent DCA animals at 7 days. Very few neutrophils and no lymphocytes were observed. Leukocyte infiltration was markedly alleviated at 28 days (black arrows, internal elastic lamina). f, g, DCA effectively lowered the elevated ΔΨm of myointimal cells on day 7 (f, mean ± s.d., n = 4 animals per group, Student’s t-test), but had little effect on the already reduced ΔΨm at 28 days (g, mean ± s.d., n = 6 animals per group, Student’s t-test). h, i, The percentages of proliferating (Ki67+) and apoptotic (TUNEL+) cells in the myointima were calculated (representative cropped pictures of the myointima are presented). The few myointimal cells in control- and DCA-vessels at 7 days showed high proliferative activity (red, positive y axis), but apoptosis (green, negative y axis) was only observed in DCA-treated animals (h, mean ± s.e.m., n = 4 animals per group). Proliferation and apoptosis were low after 28 days in both groups (i, mean ± s.e.m., n = 5 animals (control at day 28) and 7 animals (DCA at day 28)). *P < 0.05.
Extended Data Figure 7 DCA does not impair endothelial cell migration or vessel re-endothelialization.
The effect of DCA on endothelial cell (EC) migration was assessed in vitro. a, b, A scratch (width 338 μm) was made across a confluent human EC monolayer. The number of cells that migrated into a 340 μm × 338 μm scratch rectangle within 5 h was counted (a, mean ± s.d., triplicates of 3 independent experiments, Student’s t-test) and the time needed to close the scratch was recorded (b, mean ± s.d., n = 5 (EC), 4 (EC + DCA) independent experiments, Student’s t-test). There were no differences between untreated and DCA-treated ECs. c, d, To evaluate vessel re-endothelialization, rat aortas underwent mechanical endothelial denudation by balloon injury. Aortas were recovered after 28 days and stained for rat endothelial cell antigen (c, black arrows, RECA-1). Re-endothelialization was quantified (d, mean ± s.d., n = 5 animals (control at day 28) and 6 animals (DCA at day 28), Student’s t-test) and was similar in both groups. e, f, Endothelial function in both 28-day groups was further assessed in relaxation studies and compared to denuded aortas three days after balloon injury (mean ± s.e.m., n = 9 animals (control at day 28), 11 animals (DCA at day 28) and 3 animals (denuded at day 3)). Freshly recovered aortic segments were pre-constricted and DCA-treated and control vessels, as well as denuded aortas, showed similar endothelium-independent relaxation capacities using nitroglycerin (NTG) as vasodilator (e). However, denuded aortas largely failed to show endothelium-dependent relaxation with acetylcholine (Ach; f). Both DCA-treated and control vessels demonstrated similar and physiologic endothelium-dependent relaxation, indicating functional integrity of the vascular endothelium.
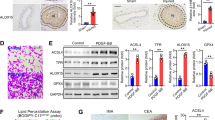
Extended Data Figure 8 PDK2 knockdown in SMCs, HMAs and HCAs.
a, PDK1, PDK2, PDK3 and PDK4 mRNA expression was assessed in control SMCs and normalized to GAPDH (mean ± s.d., 3 independent experiments). PDK1, PDK2 and PDK3 mRNA was detected as shown. Also, PDK1, PDK2 and PDK3 but not PDK4 were detectable in immunoblot analyses (data are representative of 3 independent experiments). b, To confirm in vitro PDK2 knockdown, PDK1 and PDK2 expressions were assessed in immunoblot analyses (data are representative of 3 independent experiments). PDK2 was markedly reduced in PDK2-knockdown SMCs (PDK2-KD-SMC), but not in scramble shRNA-transduced SMCs (scramble-SMC). PDK1 expression remained unaffected by PDK2- or scramble-shRNA constructs. c, To exclude that lentiviral shRNA transduction changed the ΔΨm response to PDGF, scramble-SMCs were stimulated with PDGF (mean ± s.d., 10 replicates of 2 independent experiments, Student’s t-test). Both the baseline potential and the PDGF-triggered increase in ΔΨm were similar to SMCs (see Extended Data Fig. 5a). d, Fresh HMA vessels underwent balloon injury, were divided, and one half was sampled (day -1). The other half was incubated with lentiviral particles containing PDK2 or scrambled shRNA. On the next day, transduced vessels were transplanted into RNU rats. Two days later, vessels were recovered (day 2) for immunoblotting. PDK2 could be detected in untreated HMA vessels (day -1). On day 2, only scrambled control HMAs, but not PDK2-KD vessels showed a PDK2 signal (data are representative of 3 independent experiments). e, f, After 28 days, HMA and HCA samples were stained for DAPI, PDK1, PDK2 and SMA. PDK1 was similarly detectable in all control, scramble and PDK2-KD sections at day 28 (e, pictures are representative of 3 independent experiments). At day 28, HMA control and scramble as well as HCA control showed detectable PDK2 protein, whereas PDK2 fluorescence in HMA and HCA PDK2-KD at day 28 was negligible (f, pictures are representative of 3 independent experiments), demonstrating selective knockdown. **P < 0.01.
Extended Data Figure 9 PDK2 knockdown mimics the DCA effect on SMC ΔΨm and apoptosis.
a, PDK2-KD-SMCs were pre-incubated with DCA and/or stimulated with PDGF. PDK2-KD-SMCs maintained low ΔΨm despite PDGF stimulation and DCA did not further depolarize ΔΨm (mean ± s.d., 10 replicates of 3 (columns 1 and 3) or 4 (column 2) independent experiments, ANOVA with Bonferroni’s post-hoc test). b, c, Apoptosis was induced with staurosporine. Control PDK2-KD-SMCs showed mainly mitochondria-housed cytochrome C in fluorescence stainings (b, mean ± s.d., 10 replicates of 2 independent experiments, ANOVA with Bonferroni’s post-hoc test) and compartment-separated immunoblot analyses (c, data are representative of 2 independent experiments). After induction of apoptosis, cytochrome C leaked into the cytoplasm and PDGF did not suppress cytochrome C leakage. d, PDGF did not induce resistance to apoptosis in PDK2-KD-SMCs (mean ± s.d., 10 replicates of 2 independent experiments per group, ANOVA with Bonferroni’s post-hoc test). e, To establish a link between PDH and ΔΨm, PDH was knocked down (data are representative of 2 independent experiments). f, ΔΨm was significantly increased in PDH siRNA-transfected SMCs and PDGF and DCA no longer affected ΔΨm (mean ± s.d., 10 replicates of 2 (column 2) or 3 (columns 1, 3, 4 and 5) independent experiments, ANOVA with Bonferroni’s post-hoc test). **P < 0.01.
Extended Data Figure 10 VDAC controls ΔΨm and apoptosis.
a, PDGF stimulation of SMCs significantly increased phosphorylated AKT, and ERK1 and ERK2, and increased the expression of HK2 (mean ± s.d., 5 (pAKT and pERK1/2) and 8 (HK2) independent experiments, PDGF normalized to control, one-sample t-tests). b, Immunoblot analysis revealed PDGF-induced upregulation of HK2 expression in SMCs (mean ± s.d., 3 (SMC) independent experiments, data normalized to control, one-sample t-test (control versus PDGF), Student’s t-test (PDGF versus PDGF + DCA)). HK2 upregulation was alleviated by DCA or PDK2-KD (mean ± s.d., 8 (PDK2-KD-SMC) independent experiments, PDGF normalized to control, one-sample t-test). c, Confocal images with mitochondrial (MitoTracker, red), HK2 (green), and nuclear staining (DAPI, blue, data are representative of 2 independent experiments) were captured. Co-localization of green HK2 with red mitochondria generated a yellow colour. SMCs incubated with PDGF increased their yellow signal, an effect that was prevented by DCA. PDGF did not induce HK2-mitochondrial association in PDK2-KD-SMCs. d, Cytoplasmatic (C) and mitochondrial fractions (M) were isolated for immunoblotting (data are representative of 2 independent experiments). In control SMCs and PDK2-KD-SMCs, HK2 was mainly detected in the cytoplasmatic fraction. In SMCs, PDGF caused a partial translocation of HK2 to the mitochondrial compartment. DCA markedly alleviated this translocation. PDGF did not induce HK2 translocation in PDK2-KD-SMCs. e, In the presence of HXK2VBD-cpm, PDGF failed to induce both ΔΨm hyperpolarization (mean ± s.d., 10 replicates of 3 independent experiments, ANOVA with Bonferroni’s post-hoc test) and apoptosis resistance (mean ± s.d., 10 replicates of 3 independent experiments, ANOVA with Bonferroni’s post-hoc test). f, VDAC inhibition by DIDS caused ΔΨm hyperpolarization (mean ± s.d., 10 replicates of 2 independent experiments, Student’s t-test) and rendered SMCs resistant to staurosporine-induced apoptosis (mean ± s.d., 10 replicates of 3 independent experiments, ANOVA with Bonferroni’s post-hoc test). g, The depolarizing effect of DCA on PDGF-treated SMCs was counteracted by DIDS (mean ± s.d., 10 replicates of 3 independent experiments, ANOVA with Bonferroni’s post-hoc test). Although PDGF did not increase ΔΨm in PDK2-KD-SMC, DIDS caused marked mitochondrial hyperpolarization (mean ± s.d., 10 replicates of 2 independent experiments, ANOVA with Bonferroni’s post-hoc test). *P < 0.05; **P < 0.01.
Supplementary information
The surgical hMA implant procedure
hMA underwent balloon injury using a 2-Fr. Fogarty catheter. A median laparotomy was performed in RNU rats, the infra-renal aorta was prepared, clamped, and a short segment was excised. The denuded hMA was implanted as an interposition graft using two end-to-end anastomoses. (AVI 10342 kb)
In vitro EC migration
Human ECs were grown to confluency in the presence or absence of DCA (5mM). A 338µm scratch was made using a pipette tip and cell migration into the scratch was recorded every 5 min over a period of 10h. We did not observe differences in migratory capacity or speed between untreated and DCA-treated ECs. (AVI 3846 kb)
Rights and permissions
About this article
Cite this article
Deuse, T., Hua, X., Wang, D. et al. Dichloroacetate prevents restenosis in preclinical animal models of vessel injury. Nature 509, 641–644 (2014). https://doi.org/10.1038/nature13232
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nature13232
This article is cited by
-
G6PD maintains the VSMC synthetic phenotype and accelerates vascular neointimal hyperplasia by inhibiting the VDAC1–Bax-mediated mitochondrial apoptosis pathway
Cellular & Molecular Biology Letters (2024)
-
Retro-inversion follicle-stimulating hormone peptide-modified nanoparticles for delivery of PDK2 shRNA against chemoresistant ovarian cancer by switching glycolysis to oxidative phosphorylation
Cancer Nanotechnology (2022)
-
A new Mfn-2 related synthetic peptide promotes vascular smooth muscle cell apoptosis via regulating the mitochondrial apoptotic pathway by inhibiting Akt signaling
Journal of Translational Medicine (2021)
-
Therapeutic effect of dichloroacetate against atherosclerosis via hepatic FGF21 induction mediated by acute AMPK activation
Experimental & Molecular Medicine (2019)
-
Hindlimb Ischemia Impairs Endothelial Recovery and Increases Neointimal Proliferation in the Carotid Artery
Scientific Reports (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.