Abstract
Neutralizing antibodies can confer immunity to primate lentiviruses by blocking infection in macaque models of AIDS1,2,3,4. However, earlier studies of anti-human immunodeficiency virus type 1 (HIV-1) neutralizing antibodies administered to infected individuals or humanized mice reported poor control of virus replication and the rapid emergence of resistant variants5,6,7. A new generation of anti-HIV-1 monoclonal antibodies, possessing extraordinary potency and breadth of neutralizing activity, has recently been isolated from infected individuals8. These neutralizing antibodies target different regions of the HIV-1 envelope glycoprotein including the CD4-binding site, glycans located in the V1/V2, V3 and V4 regions, and the membrane proximal external region of gp41 (refs 9, 10, 11, 12, 13, 14). Here we have examined two of the new antibodies, directed to the CD4-binding site and the V3 region (3BNC117 and 10-1074, respectively), for their ability to block infection and suppress viraemia in macaques infected with the R5 tropic simian–human immunodeficiency virus (SHIV)-AD8, which emulates many of the pathogenic and immunogenic properties of HIV-1 during infections of rhesus macaques15,16. Either antibody alone can potently block virus acquisition. When administered individually to recently infected macaques, the 10-1074 antibody caused a rapid decline in virus load to undetectable levels for 4–7 days, followed by virus rebound during which neutralization-resistant variants became detectable. When administered together, a single treatment rapidly suppressed plasma viraemia for 3–5 weeks in some long-term chronically SHIV-infected animals with low CD4+ T-cell levels. A second cycle of anti-HIV-1 monoclonal antibody therapy, administered to two previously treated animals, successfully controlled virus rebound. These results indicate that immunotherapy or a combination of immunotherapy plus conventional antiretroviral drugs might be useful as a treatment for chronically HIV-1-infected individuals experiencing immune dysfunction.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Mascola, J. R. et al. Protection of macaques against pathogenic simian/human immunodeficiency virus 89.6PD by passive transfer of neutralizing antibodies. J. Virol. 73, 4009–4018 (1999)
Moldt, B. et al. Highly potent HIV-specific antibody neutralization in vitro translates into effective protection against mucosal SHIV challenge in vivo. Proc. Natl Acad. Sci. USA 109, 18921–18925 (2012)
Nishimura, Y. et al. Determination of a statistically valid neutralization titer in plasma that confers protection against simian-human immunodeficiency virus challenge following passive transfer of high-titered neutralizing antibodies. J. Virol. 76, 2123–2130 (2002)
Parren, P. W. et al. Antibody protects macaques against vaginal challenge with a pathogenic R5 simian/human immunodeficiency virus at serum levels giving complete neutralization in vitro. J. Virol. 75, 8340–8347 (2001)
Mehandru, S. et al. Adjunctive passive immunotherapy in human immunodeficiency virus type 1-infected individuals treated with antiviral therapy during acute and early infection. J. Virol. 81, 11016–11031 (2007)
Poignard, P. et al. Neutralizing antibodies have limited effects on the control of established HIV-1 infection in vivo. Immunity 10, 431–438 (1999)
Trkola, A. et al. Delay of HIV-1 rebound after cessation of antiretroviral therapy through passive transfer of human neutralizing antibodies. Nature Med. 11, 615–622 (2005)
Burton, D. R. et al. A blueprint for HIV vaccine discovery. Cell Host Microbe 12, 396–407 (2012)
Huang, J. et al. Broad and potent neutralization of HIV-1 by a gp41-specific human antibody. Nature 491, 406–412 (2012)
Klein, F. et al. HIV therapy by a combination of broadly neutralizing antibodies in humanized mice. Nature 492, 118–122 (2012)
Kong, L. et al. Supersite of immune vulnerability on the glycosylated face of HIV-1 envelope glycoprotein gp120. Nature Struct. Mol. Biol. 20, 796–803 (2013)
Walker, L. M. et al. Broad neutralization coverage of HIV by multiple highly potent antibodies. Nature 477, 466–470 (2011)
Walker, L. M. et al. Broad and potent neutralizing antibodies from an African donor reveal a new HIV-1 vaccine target. Science 326, 285–289 (2009)
Wu, X. et al. Rational design of envelope identifies broadly neutralizing human monoclonal antibodies to HIV-1. Science 329, 856–861 (2010)
Gautam, R. et al. Pathogenicity and mucosal transmissibility of the R5-tropic simian/human immunodeficiency virus SHIV(AD8) in rhesus macaques: implications for use in vaccine studies. J. Virol. 86, 8516–8526 (2012)
Nishimura, Y. et al. Generation of the pathogenic R5-tropic simian/human immunodeficiency virus SHIVAD8 by serial passaging in rhesus macaques. J. Virol. 84, 4769–4781 (2010)
Shingai, M. et al. Most rhesus macaques infected with the CCR5-tropic SHIV(AD8) generate cross-reactive antibodies that neutralize multiple HIV-1 strains. Proc. Natl Acad. Sci. USA 109, 19769–19774 (2012)
Walker, L. M. et al. Rapid development of glycan-specific, broad, and potent anti-HIV-1 gp120 neutralizing antibodies in an R5 SIV/HIV chimeric virus infected macaque. Proc. Natl Acad. Sci. USA 108, 20125–20129 (2011)
Sadjadpour, R. et al. Emergence of gp120 V3 variants confers neutralization resistance in an R5 simian-human immunodeficiency virus-infected macaque elite neutralizer that targets the N332 glycan of the human immunodeficiency virus type 1 envelope glycoprotein. J. Virol. 87, 8798–8804 (2013)
Mouquet, H. et al. Complex-type N-glycan recognition by potent broadly neutralizing HIV antibodies. Proc. Natl Acad. Sci. USA 109, E3268–E3277 (2012)
Scheid, J. F. et al. Sequence and structural convergence of broad and potent HIV antibodies that mimic CD4 binding. Science 333, 1633–1637 (2011)
Zhou, T. et al. Structural basis for broad and potent neutralization of HIV-1 by antibody VRC01. Science 329, 811–817 (2010)
Diskin, R. et al. Restricting HIV-1 pathways for escape using rationally designed anti-HIV-1 antibodies. J. Exp. Med. 210, 1235–1249 (2013)
Horwitz, J. A. et al. HIV-1 suppression and durable control by combining single broadly neutralizing antibodies and antiretroviral drugs in humanized mice. Proc. Natl Acad. Sci. USA http://dx.doi.org/10.1073/pnas.1315295110 (2013)
Igarashi, T. et al. Human immunodeficiency virus type 1 neutralizing antibodies accelerate clearance of cell-free virions from blood plasma. Nature Med. 5, 211–216 (1999)
Keele, B. F. et al. Low-dose rectal inoculation of rhesus macaques by SIVsmE660 or SIVmac251 recapitulates human mucosal infection by HIV-1. J. Exp. Med. 206, 1117–1134 (2009)
Endo, Y. et al. Short- and long-term clinical outcomes in rhesus monkeys inoculated with a highly pathogenic chimeric simian/human immunodeficiency virus. J. Virol. 74, 6935–6945 (2000)
Hansen, S. G. et al. Profound early control of highly pathogenic SIV by an effector memory T-cell vaccine. Nature 473, 523–527 (2011)
Montefiori, D. C. Evaluating neutralizing antibodies against HIV, SIV, and SHIV in luciferase reporter gene assays. Curr. Protocols Immunol. Ch. 12, Unit 12 11. (2005)
Polis, M. A. et al. Correlation between reduction in plasma HIV-1 RNA concentration 1 week after start of antiretroviral treatment and longer-term efficacy. Lancet 358, 1760–1765 (2001)
Acknowledgements
We thank K. Tomioka and R. Kruthers for determining plasma viral RNA loads and B. Skopets, W. Magnanelli and R. Petros for diligently assisting in the maintenance of animals and assisting with procedures. We also thank D. R. Burton, The Scripps Institute, for providing anti-dengue virus neutralizing monoclonal antibody (DEN-3). This work was supported by the Intramural Research Program of the National Institute of Allergy and Infectious Diseases, National Institutes of Health (NIH) and, in part, with federal funds from the National Cancer Institute, NIH, under contract HHSN261200800001E.
Author information
Authors and Affiliations
Contributions
M.S., Y.N., M.C.N. and M.A.M. designed the experiments; M.S., Y.N., F.K., H.M., O.K.D., R.P., A.B.-W. and M.P. performed the experiments; M.S., Y.N., F.K., M.P., J.D.L., D.D., M.C.N. and M.A.M. analysed the data; and M.S., Y.N., M.C.N. and M.A.M. wrote the manuscript. M.S. and Y.N. contributed equally to the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Extended data figures and tables
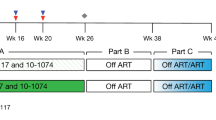
Extended Data Figure 1 Treatment of SHIV-infected macaques with single anti-HIV-1 neutralizing monoclonal antibodies.
Plasma viral loads and total CD4+ T cell numbers before (the initial 84 days of the SHIV-AD8EO infection) and during single monoclonal antibody treatment are shown. KZ6 and MB6 received the 3BNC117 monoclonal antibody and MB8 and MCN were administered the 10-1074 monoclonal antibody. Macaques MB7 and MD5 were not treated.
Extended Data Figure 2 SGA analysis of selected SHIV-AD8EO gp120 sequences, present in rebound virus after single monoclonal antibody immunotherapy, and known to confer resistance to 10-1074 or 3BNC117 monoclonal antibody.
SGA was used to amplify plasma viral RNA after monoclonal antibody treatment from the plasma of animals KZ6 (day 28 (n = 8)), MB6 (day 23 (n = 8)), MB8 (day 23 (n = 9)) and MCN (day 23 (n = 8)). The gp120 sequences at the top are present in the SHIV-AD8EO molecular clone inoculum. Mutations conferring resistance are highlighted in red.
Extended Data Figure 3 Circulating CD4+ T cells in five chronically SHIV-infected macaques treated with two anti-HIV-1 neutralizing monoclonal antibodies.
Plasma viral loads and total CD4+ T-cell numbers before (first 1,100 to 1,140 days) and during the first or second cycle of combination monoclonal antibody treatment are shown.
Extended Data Figure 4 BAL CD4+ T cells in five chronically SHIV-infected macaques treated with two anti-HIV-1 neutralizing monoclonal antibodies.
Plasma viral loads and the percentage of CD4+ T cells in CD3+ gated BAL specimens, before (first 1,100 to 1,140 days) and during the first or second cycle of combination monoclonal antibody treatment, are shown.
Extended Data Figure 5 SGA analysis of selected SHIV-AD8EO gp120 sequences known to confer resistance to 10-1074 or 3BNC117 monoclonal antibody, before and after combination immunotherapy.
a–e, Plasmas from animals DBZ3 (pre (n = 8); day 49 post first treatment (n = 10); day 24 post second treatment (n = 8)) (a), DC99A (pre (n = 10); day 57 post first treatment (n = 6); day 41 post second treatment (n = 7)) (b), DBXE (pre (n = 9), day 28 (n = 8)) (c), DCF1 (pre (n = 14), day 28 (n = 10)) (d) and DCM8 (pre (n = 7), day 28 (n = 11)) (e) were evaluated. The gp120 sequences at the top are present in the SHIV-AD8EO molecular clone inoculum. Mutations conferring resistance are highlighted in red.
Extended Data Figure 6 CD4+ T-cell numbers increase during combination monoclonal antibody treatment of SHIV-AD8EO-infected macaques.
a, b, Levels of viral RNA and total CD4+ T-cell/CD4+ T-cell subsets in symptomatic chronically infected macaques DBXE (a) and DCF1 (b).
Extended Data Figure 7 Assays to identify 10-1074- or 3BNC117-specific neutralizing activities in the plasma of monoclonal-antibody-treated macaques.
a, ID50 values measured in the TZM-bl neutralization assay of 10-1074 and 3BNC117 against HIV-1 strains that are sensitive to one but not the other broadly neutralizing antibody (that is, HIV-1 strain X2088_9 (10-1074 sensitive); HIV-1 strain Q769_d22 (3BNC117 sensitive)). b, Neutralizing activities in plasma before antibody administration (preP), but spiked with 0.01, 0.1, 1, 10 and 100 μg ml−1 of antibodies 10-1074 (blue) or 3BNC117 (green). Neutralizing activities are reported as plasma ID50 titres (left columns) and converted to antibody concentrations (right columns) based on measured ID50 values in a.
Extended Data Figure 8 Monoclonal antibody levels in the plasmas of monotherapy and combination monoclonal antibody macaque recipients.
a–c, Macaques treated with one neutralizing monoclonal antibody (a); macaques receiving two cycles of combination monoclonal antibody treatment (b); macaques receiving a single cycle of combination monoclonal antibody treatment (c). ID50 titres (left columns) and monoclonal antibody concentrations (right columns) were measured in the indicated macaque plasma samples before (Prebleed) and after (Day) monoclonal antibody administration.
Rights and permissions
About this article
Cite this article
Shingai, M., Nishimura, Y., Klein, F. et al. Antibody-mediated immunotherapy of macaques chronically infected with SHIV suppresses viraemia. Nature 503, 277–280 (2013). https://doi.org/10.1038/nature12746
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nature12746
This article is cited by
-
Mucosal application of the broadly neutralizing antibody 10-1074 protects macaques from cell-associated SHIV vaginal exposure
Nature Communications (2023)
-
Antiviral neutralizing antibodies: from in vitro to in vivo activity
Nature Reviews Immunology (2023)
-
Broadly neutralizing anti-HIV-1 antibodies tether viral particles at the surface of infected cells
Nature Communications (2022)
-
HIV cure strategies: which ones are appropriate for Africa?
Cellular and Molecular Life Sciences (2022)
-
Common evolutionary features of the envelope glycoprotein of HIV-1 in patients belonging to a transmission chain
Scientific Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.