Abstract
The enteric nervous system (ENS) is recognized as a second brain because of its complexity and its largely autonomic control of bowel function. Recent progress in studying the interactions between the ENS and the central nervous system (CNS) has implicated alterations of the gut/brain axis as a possible mechanism in the pathophysiology of autism spectrum disorders (ASDs), Parkinson’s disease (PD) and other human CNS disorders, whereas the underlying mechanisms are largely unknown because of the lack of good model systems. Human induced pluripotent stem cells (hiPSCs) have the ability to proliferate indefinitely and differentiate into cells of all three germ layers, thus making iPSCs an ideal source of cells for disease modelling and cell therapy. Here, hiPSCs were induced to differentiate into neural crest stem cells (NCSCs) efficiently. When co-cultured with smooth muscle layers of ganglionic gut tissue, the NCSCs differentiated into different subtypes of mature enteric-like neurons expressing nitric oxide synthase (nNOS), vasoactive intestinal polypeptide (VIP), choline acetyltransferase (ChAT) or calretinin with typical electrophysiological characteristics of functional neurons. Furthermore, when they were transplanted into aneural or aganglionic chick, mouse or human gut tissues in ovo, in vitro or in vivo, hiPSC-derived NCSCs showed extensive migration and neural differentiation capacity, generating neurons and glial cells that expressed phenotypic markers characteristic of the enteric nervous system. Our results indicate that enteric NCSCs derived from hiPSCs supply a powerful tool for studying the pathogenesis of gastrointestinal disorders and brain/gut dysfunction and represent a potentially ideal cell source for enteric neural transplantation treatments.
Similar content being viewed by others
Introduction
The principal functions of the gut are to enhance nutrient absorption and transport food scraps, functions that are supported by motility and secretory activity directed mostly by the intramural enteric nervous system (ENS).1, 2 The ENS is composed of numerous neurons (400–600 million in humans), glial cells and the neural connections between them that reside in the myenteric and submucosal plexus.3 Because its structural and chemical complexity resembles that of the central nervous system (CNS) and dominant autonomic control of bowel function, the ENS has been recognized as a second brain in our body.4
Congenital anomalies that interrupt ENS development or acquired diseases can lead to loss of enteric neurons/enteric glia or defects in their function, ultimately causing gastrointestinal (GI) motility disorders, including Hirschsprung’s disease (HSCR), gastroparesis and irritable bowel syndrome.5, 6 Recent progress in studying interactions between the CNS, ENS and GI tract has implicated alterations of the gut/brain axis as a possible mechanism in the pathophysiology of autism spectrum disorders (ASDs), Parkinson’s disease (PD) and other CNS disorders.7, 8, 9, 10 Indeed, the ENS connects the CNS via the afferent and efferent pathways of the parasympathetic and sympathetic nervous systems, although it can function autonomously. Moreover, previous studies have shown that many of the synaptic genes associated with ASDs including the Shanks, neurexins and neuroligins are also expressed in the ENS.11, 12, 13, 14 Therefore, the genetic defects underlying CNS disorders usually cause impairment of the ENS.4, 15 McElhanon et al.16 found that gut disorders including abdominal pain, constipation and diarrhoea are the most common complications of ASD. In addition, recent studies demonstrated that the ENS is impaired during the pathological process of PD.17, 18, 19 The great majority of PD patients have GI motility disorders, and one of the pathological hallmarks of PD, Lewy bodies, are found primarily in vasoactive intestinal polypeptide (VIP)-immunoreactive neuronal cell bodies and processes within the colonic myenteric and submucosal plexus.20, 21 However, the underlying molecular mechanisms that lead to ENS defects and GI disorders and their roles in CNS disorders remain largely unknown.
The in vitro disease modelling using patient-derived stem cells will be of great value in uncovering the mechanisms of disease pathogenesis. Reprogramming human somatic cells to a pluripotent state allows the generation of human induced pluripotent stem cells (hiPSCs).22 The hiPSCs share characteristics with human embryonic stem cells with respect to their self-renewal capacity and pluripotency. Consequently, iPS technology offers a powerful tool for modelling human disease in the culture dish.23, 24, 25 Throughout early embryonic development in vertebrates, vagal neural crest stem cells (NCSCs) enter the foregut and migrate through the developing GI tract, giving rise to the majority of neurons and glial cells in the ENS.26, 27 Thus, the generation of functional enteric neurons from hiPSCs via neural crest specification will provide a valuable tool for modelling human disease and for cell replacement therapies.28, 29, 30, 31
In this study, we successfully induced the differentiation of hiPSCs into NCSCs. When co-cultured with tissues from normal human gut in neural differentiation medium in vitro, hiPSC-derived NCSCs (hiPSC-NCSCs) efficiently differentiated into functional enteric-like neurons. When transplanted into chicken, mouse or human aneural or aganglionic gut tissues, hiPSC-NCSCs showed extensive migration and neural differentiation capacity.
Materials and methods
Cell culture
HDF-hiPSCs (derived from human adult dermal fibroblasts), HEF-hiPSCs (derived from human embryonic dermal fibroblasts), humanized Renilla reniformis-derived green fluorescent protein (hrGFP)-labelled HDF-hiPSCs and human embryonic stem cell lines (H1, H9) were cultured as reported previously.32, 33 Briefly, cells were attached to Matrigel-coated culture plates and were maintained in mTeSR1 medium (Stemcell Technologies, Vancouver, BC, Canada). The medium was changed every day, and cells were routinely passaged in small clumps every 4–5 days by treating with 0.5 mM EDTA (pH 8.0) (Life Technologies, Carlsbad, CA, USA).
Additional experimental procedures
For more detailed and additional information on experimental procedures, please see Supplementary Materials and Methods and Supplementary Tables 1 and 2.
Results
Generation of NCSCs from hiPSCs
Two human iPS cell lines that were generated previously (HDF-hiPSCs and HEF-hiPSCs)32, 33 and the human ES cell lines H1 and H9 were used in this study. Both in vivo and in vitro analyses revealed that these human iPS cells exhibited the essential characteristics of human ES cells, particularly the capacities for self-renewal and differentiation (Supplementary Figures 1A–C). Previous studies have demonstrated that human pluripotent stem cells—human embryonic stem cells and hiPSCs—can differentiate into NCSCs via neural rosette formation.28, 34 Here, dissociated HDF-hiPSCs cultured in suspension in N2B27- and Y27632-containing medium for 5 days formed uniform-sized embryoid bodies (EBs) with defined edges in AggreWell plates (STEMCELL Technologies, Vancouver, BC, Canada). The EBs were then allowed to attach to PO/LN-coated culture plates and cultured in neural crest culture medium (NCCM) for ∼5–7 days before fluorescence-activated cell sorting (FACS) enrichment of p75+/HNK1+ NCSCs (Supplementary Figure 2A). Multiple rosette structures emerged in the centre of the attached EBs, and cells migrated out from the rosette structures to the periphery of the attached EBs (Figure 1a). Immunofluorescence analysis of the migrated cells for neural crest lineage marker expression showed that most of these cells co-expressed neural crest-specific transcription factors, including Sox10, AP2α, Brn3a, Isl1 and Mash1, and some of the differentiated cells expressed the vagal neural crest markers Hoxb2 and Hoxb3 (Figure 1b; Supplementary Figure 2B) that have been shown to play essential roles in the multipotency, delamination, differentiation and migration capacity of NCSCs.35 The cell clusters surrounding the rosettes also co-expressed cell surface markers of NCSCs including p75 and HNK1 (Figure 1b). Moreover, the intermediate filaments Nestin and Vimentin, and the epithelial–mesenchymal transition regulatory factor Slug, were widely expressed by these cells (Figure 1c), consistent with previous findings.28 In accord with these immunocytochemistry data, quantitative PCR (qPCR) analysis showed that mRNAs for the NCSC-specific markers Sox10, Ap2α, p75, HNK1 (Figure 1d), Brn3a, Isl1, Mash1, Hoxb2 and Hoxb3 were highly upregulated, whereas the expression of endogenous pluripotency markers was downregulated rapidly (Supplementary Figure 2C) in a time-dependent manner during the neural crest differentiation of hiPSCs.
Neural crest differentiation of human induced pluripotent stem cells (hiPSCs). (a) Human iPSCs were cultured in mTeSR1 medium and plated on Matrigel-coated plates. After culturing in N2B27 medium for 5 days, dissociated cells formed uniform embryoid bodies (EBs) in AggreWell plates. After replating onto PO/LN-coated plates, multiple rosette structures formed in the centre of the attached EBs. (b) Immunofluorescence analysis showed that cells migrating out from the rosette structures co-expressed the neural crest-specific genes Sox10, Ap2α, p75 and HNK1. (c) Most migratory cells also expressed Nestin, Vimentin and Slug, as shown by immunostaining. (d) quantitative PCR (qPCR) demonstrated that mRNAs for the neural crest stem cell (NCSC)-specific markers Sox10, Ap2α, p75 and HNK1 were highly upregulated after differentiation (normalized to day 4 mRNA expression). Scale bar, 200 μm.
HNK1 and p75 are widely used to enrich human NCSCs from pluripotent stem cells by FACS.28, 29, 34 Here, we isolated p75 and HNK1 double-positive (HNK1+/p75+) cells by FACS and further characterized these hiPSC-derived NCSCs. This analysis showed that the proportion of HNK1+/p75+ cells was 90.45±3.41% among the differentiated HDF-hiPSCs and the differentiation efficiency of this hiPSC line was consistent between individual differentiations (n=4; Figure 2a and Supplementary Figure 3A). Comparable differentiation efficiency was also obtained in other pluripotent stem cell lines (H1, H9) and HEF-hiPSCs (Supplementary Figure 3B). These freshly isolated NCSCs were then cultured on PO/LN-coated dishes in NCCM for adherent culture (Figure 2b). Attached NCSCs maintained their typical cellular morphology and their NCSC identity as evidenced by robust expression of p75 (88.12±1.46%), HNK1 (92.26±1.01%), Sox10 (94.75±1.10%) and AP2α (91.72±1.66%) detected by immunostaining (Figures 2c and d). Isolated NCSCs could be propagated in vitro for up to 15–20 passages with characteristic gene expression (Supplementary Figure 4A), normal karyotype (Supplementary Figure 4B) and self-renewal ability (Supplementary Figure 4C). qPCR analysis further showed that the transcription of the neural crest-specific genes p75, Sox10, Zic1, Pax3 and AP2α was 5- to 10-fold higher in enriched NCSCs than in undifferentiated hiPSCs (Figure 2e).
Enrichment and characterization of human induced pluripotent stem cell-derived neural crest stem cells (hiPSC-NCSCs). (a) HNK1+/p75+ cells were isolated by fluorescence-activated cell sorting (FACS) after differentiation for 10–12 days. (b) NCSCs cultured on PO/LN-coated dishes maintained their typical cellular morphology. (c) hiPSC-NCSCs expressed the neural crest stem cell markers p75, HNK1, Sox10 and AP2α. (d) The percentages of p75+/HNK1+, Sox10+, and AP2α+ cells in isolated hiPSC-NCSCs were analysed, respectively. (e) Quantitative PCR (qPCR) analysis showed that mRNA expression of the NCSC markers p75, Sox10, Zic1, Pax3 and AP2α was 5–10-fold higher in enriched NCSCs than in undifferentiated hiPSCs (**P<0.01). (f) Time-lapse microscopy revealed that these NCSCs possessed considerable migration ability, reaching a peak migration rate of 84.6 μm h−1 (14.1 μm per 10 min). Scale bar, 100 μm.
Extensive migration ability in vivo is one of the characteristic features of NCSCs, and it has been reported that NCSCs migrate caudally along the entire length of the gut at speeds of 35–40 μm h−1 (5.83–6.67 μm per 10 min) in both birds and explants from embryonic mice.36, 37 Here, freshly isolated HNK1+/p75+ cells were replated on PO/LN-coated plates for migration assays. Time-lapse microscopy revealed that these NCSCs possessed considerable migration ability, exhibiting a peak migration rate of 14.1 μm per 10 min and an average migration rate of 4.97±0.64 μm per 10 min (Figure 2f and Supplementary Movie 1).
When suspension-cultured on ultra-low attachment plates in NCCM, FACS-purified HNK1+/p75+ cells formed spheres (Supplementary Figure 5A). These spheres could be passaged every 3–4 days and maintained their sphere-formation ability for at least 10 passages in vitro. We also found that neither plating density nor passage number influenced the sphere-forming efficiency of NCSCs cultured in NCCM (Supplementary Figures 5B and C). Immunostaining indicated that most cells within spheres of passage 10 expressed the NCSC markers HNK1, p75 and Sox10 and the proliferation marker Ki67 (Supplementary Figure 5D).
Multilineage differentiation of hiPSC-derived NCSCs
NCSCs migrate along defined pathways to various tissues and differentiate into a wide array of derivatives, including neurons and glia of the peripheral nervous system, bone, cartilage and smooth muscle.38 We thus explored the potential of hiPSC-derived NCSCs to give rise to various cell types. For neuronal differentiation, NCSCs were cultured in medium containing brain-derived neurotrophic factor, glial cell line-derived neurotrophic factor, nerve growth factor and 10 ng ml−1 neurotrophin-3, ascorbic acid and dibutyryl-cAMP for 3–4 weeks. Of the resulting cells in these cultures, 81.46±4.22% (n=3) co-expressed peripherin and TUBB3 (tubulin-β3), thus confirming their identity as peripheral neurons. We also found that NCSCs could differentiate into Brn3a- and peripherin-positive (Brn3a+/peripherin+) sensory neurons, tyrosine hydroxylase- and TUBB3-positive (TH+/TUBB3+) peripheral sympathetic neurons and Mash1- and peripherin-positive (Mash1+/peripherin+) autonomic neurons with variable efficiency under neural-differentiation conditions (Supplementary Figure 6A). qPCR analysis further confirmed that peripherin, TH, Brn3a and Mash1 mRNA were significantly upregulated during the differentiation process, reaching levels ~2.5–5-fold higher in differentiated cells than in undifferentiated NCSCs (Supplementary Figure 6B).
When cultured initially in medium containing ciliary neurotrophic factor, neuregulin and dibutyryl-cAMP for 2–3 weeks, NCSCs subsequently cultured in vitro for more than 2 months could be induced to efficiently differentiate into Schwann cells. Immunostaining showed that 53.75±9.57% (n=3) of the resulting cells co-expressed the Schwann cell markers S100B and glial fibrillary acidic protein (GFAP) (Supplementary Figure 6C), a result that was further validated by qPCR detection of the corresponding mRNAs (Supplementary Figure 6D).
To assess their mesodermal differentiation potential, we cultured NCSCs in fetal bovine serum-containing medium. Cells with spindle-shaped morphology that exhibited a parallel or spiral arrangement emerged and proliferated actively. FACS analysis showed that NCSC-derived mesenchymal stem cells (MSCs) expressed surface markers typical of human MSCs including CD44, CD73 and CD90, and nearly all were negative for CD34 and CD45. However, CD105 and CD166 were rarely expressed by the NCSC-MSC population (Supplementary Figure 7A), a result consistent with a previous report.28 We further cultured NCSC-MSCs under conditions that specifically promote differentiation into either osteoblasts, adipocytes, chondrocytes or smooth muscle. As confirmed by Alizarin Red S staining, Oil Red O staining, Toluidine Blue staining and anti-α-smooth muscle cell immunostaining, the NCSC-MSCs showed (respectively) osteogenic, adipogenic, chondrogenic (Supplementary Figure 7B) and smooth muscle cell differentiation capacity (Supplementary Figure 7C).39 The qPCR results further confirmed the multilineage differentiation ability of NCSCs-MSCs (Supplementary Figure 7D).
Derivation of enteric-like neurons from hiPSC-NCSCs in vitro
To investigate whether hiPSC-NCSCs can differentiate to enteric-like neurons, we co-cultured them with gut explants for 10 days using a Transwell system40 (Supplementary Figure 8A). After culturing for 6–8 more weeks, NCSCs seeded onto the lower chamber in peripheral neuron differentiation medium were assessed by immunostaining. This analysis showed that the differentiated NCSCs expressed the functional enteric neural markers VIP (16.2±2.29%), choline acetyltransferase (ChAT; 20.08±2.18%), calretinin (24.54±2.40%), tyrosine hydroxylase (TH) (9.56±1.04%) and neuronal nitric oxide synthase (nNOS; 18.4±2.12%) (n=5; Figures 3a and b), indicating that these NCSCs could be induced to differentiate into enteric-like neurons efficiently in a co-culture system. In addition, <5% of the differentiated cells expressed the sympathoadrenal markers chromogranin A, dopamine and phenylethanolamine N-methyltransferase (Supplementary Figure 8B). However, without co-culturing with gut explants, few NCSCs (<1%) differentiated into enteric-like neurons in peripheral neural differentiation conditions. Electrophysiological analysis of enteric-like neurons exhibiting typical neuronal morphology suggested that voltage-dependent currents could be invoked using a voltage-clamp protocol in 56.8% of the recorded cells (n=74; Figure 3c). Moreover, in cells held in current-clamp mode, a short depolarizing pulse elicited an action potential in 54.2% of the recorded cells (n=83; Figure 3d). We also observed rapidly inactivating persistent outward currents and inward currents in response to depolarizing voltage steps that could be blocked by the potassium channel blockers tetraethylammonium and 4-aminopyridine (48%; n=25; Figures 3e and f) and the sodium channel blocker tetrodotoxin (56.5%; n=23; Figures 3g and h), respectively. Moreover, spontaneous postsynaptic currents were recorded and could be blocked by the soluble guanylyl cyclase inhibitor oxadiazolo-quinoxalineone (the binding of oxadiazolo-quinoxalineone is competitive with NO) in 9.30% of patched cells (n=43; Figures 3I and j). These results confirm that hiPSC-derived NCSCs have the ability to differentiate into electrophysiologically mature neurons.
Functional enteric-like neurons derived from human induced pluripotent stem cell-derived neural crest stem cells (hiPSC-NCSCs) in vitro. (a) Differentiated hiPSC-NCSCs were found to express functional enteric neural markers such as vasoactive intestinal polypeptide (VIP), choline acetyltransferase (ChAT), calretinin, tyrosine hydroxylase (TH) and neuronal nitric oxide synthase (nNOS). (b) The percentages of VIP+, ChAT+, calretinin+, TH+ and nNOS+ enteric-like neurons differentiated from hiPSC-NCSCs were analysed, respectively. (c) Electrophysiological recordings obtained in voltage-clamp mode from differentiated cells with a typical neuronal morphology suggested that voltage-dependent currents could be invoked in these cells (56.8%; n=74). (d) Electrophysiological recordings obtained in current-clamp mode (54.2%; n=83). (e, f) Outward current was observed in voltage-clamp mode from differentiated hiPSC-NCSCs and could be blocked by the potassium channel blockers tetraethylammonium (TEA) and 4-aminopyridine (4-AP) (48%; n=25). (g, h) Inward current was observed in voltage-clamp mode from differentiated hiPSC-NCSCs and could be blocked by the sodium channel blocker tetrodotoxin (TTX) (56.6%; n=23). (i, j) Spontaneous activity was recorded in differentiated hiPSC-NCSCs and could be blocked by the soluble guanylyl cyclase inhibitor oxadiazolo-quinoxalineone (ODQ) (9.30%; n=43). Scale bar, 50 μm.
We further performed RNA sequencing to examine changes in global expression profile during the enteric neuron differentiation of hiPSCs. The samples included undifferentiated hiPSCs, freshly isolated p75+/HNK1+ hiPSC-NCSCs, enteric neural crest precursors (hiPSC-ENCPs) from hiPSC-NCSCs (co-cultured with gut explants for 10 days) and enteric-like neurons (hiPSC-ENs) from hiPSC-NCSCs (co-cultured with gut explants for 42 days). The results (GSE79928) demonstrated that the expression profile of undifferentiated hiPSCs was enriched for genes related to pluripotency (Oct4, Sox2, Nanog, Rex1 and others). However, the freshly isolated hiPSC-NCSCs strongly expressed neural crest-specific transcription factors (for example, Sox10, Sox9, FoxD3, Msx1, Msx2, Pax3, Pax7). Significantly, the hiPSC-ENCPs were highly enriched in transcripts associated with vagal neural crest and/or enteric neural progenitors, including Hoxb2, Hoxb3, Hand2 and Ednrb. The hiPSC-ENs differentiated from hiPSC-NCSCs expressed genes involved in neuronal morphogenesis and maintenance, ion channels and functional synaptic components (Mapt, Gap43, Stmn3, Stmn4, Syn1, Syp and Syt1) (Supplementary Figure 9A).
To further confirm these results, we also isolated primary enteric neurons (pENs) (Supplementary Figures 9B and C) from human gut tissues as described previously41 and performed qPCR analysis to compare the expression level of specific genes among hiPSC-ENCPs, hiPSC-ENs and pENs. The results demonstrated that pENs expressed relatively low levels of NCSC markers (Sox10 and p75) and vagal markers (Hoxb2 and Hoxb3); however, they strongly expressed neuronal markers, including peripherin, calretinin, TH and ChAT, that constitute a gene expression profile that is more characteristic of hiPSC-ENs than hiPSC-ENCPs (Supplementary Figure 9D). Taken together, these results indicate that the enteric-like neurons can be efficiently differentiated from hiPSC-NCSCs.
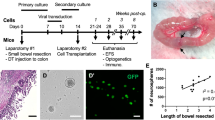
Migration and differentiation of hiPSC-NCSCs in aneural mouse gut in vitro and chick embryos in ovo
It has been reported that the distal one-third of the mouse hindgut at E11.5 is aneural because it is not yet colonized by vagal NCSCs.42 Here, to assess the enteric neuron differentiation potential of hiPSC-NCSCs in aneural mouse gut, we investigated the migration and differentiation capacity of hiPSC-NCSCs in vitro using a hanging drop method, with aneural embryonic hindgut as the recipient tissue. Spheres were formed by culturing hrGFP-NCSCs in suspension for 2 days and were then co-cultured with aneural embryonic hindguts (Supplementary Figure 10). Continuous observation under fluorescence microscopy revealed that cells inside single hrGFP-NCSC spheres progressively migrated into the same hindgut during the co-culture process (Figure 4a). Immunostaining showed that ∼20–30% of the migrated cells retained NCSC characteristics as evidenced by the expression of p75 (26.94±4.31%) and Sox10 (20.20±2.97%) (n=5; Figure 4b). GFAP-positive cells (3.96±0.58%) were detected in the mouse hindgut after NCSC transplantation (n=5; Figure 4c). Most of the NCSCs gave rise to TUBB3+ neurons (71.28±7.28%), whereas some of the hrGFP+ cells differentiated into a more mature nNOS- (26.42±3.17%), ChAT- (26.98±8.76%) or VIP-expressing (20.76±1.84%) neuronal subtype (n=5; Figures 4d and e).
Human induced pluripotent stem cell-derived neural crest stem cells (hiPSC-NCSCs) are capable of migration and differentiation in aneural mouse hindgut in vitro. (a) hiPSC-NCSCs were co-cultured with E11.5 aneural mouse hindgut for 7–12 days. hrGFP+ cells progressively migrated into the same distal hindgut during the co-culture process as observed by serial observation under a fluorescence microscope. The areas between dotted lines indicate the hindgut area. (b) Some of the engrafted cells retained expression of the NCSC markers p75 and Sox10. (c) GFAP-positive cells were detected in the mouse hindgut after NCSC transplantation. (d) Immunostaining showed that most NCSCs differentiated into TUBB3+ neurons, whereas some cells differentiated into a more mature neuronal nitric oxide synthase (nNOS)-, choline acetyltransferase (ChAT)- or vasoactive intestinal polypeptide (VIP)-expressing neuronal subtype. Scale bar, 50 μm. (e) The percentages of p75+, Sox10+, GFAP+, TUBB3+, nNOS+, ChAT+ and VIP+ neurons differentiated from transplanted hrGFP+ hiPSC-NCSCs were analysed, respectively.
We also evaluated the migration and differentiation ability of hiPSC-NCSCs using aneural gut from chick embryos (n=4) and ganglionic hindgut of severe combined immunodeficiency (SCID) mice (n=5) as recipient tissues. hrGFP-NCSCs transplanted into embryonic (E5) chick hindgut appeared to organize into ganglia within the submucosal and myenteric regions, and they were capable of longitudinal migration (Supplementary Figure 11A). A small fraction of engrafted NCSCs retained expression of the neural crest marker p75 (7.54±1.89%) or Sox10 (7.83±1.35%), but some differentiated into neurons expressing TUBB3 (43.47±3.31%) (Supplementary Figure 11B) and a more mature neuron marker VIP (19.80±2.91%) or nNOS (22.59±3.30%) (Supplementary Figure 11C). When transplanted into the hindgut of SCID mice, hrGFP-NCSCs were also capable of migration toward the myenteric and submucosal regions (n=4; Supplementary Figure 12A) in recipient mice. Few of the transplanted cells retained their NCSC identity (as shown by p75 immunostaining; 4.70±1.24%; Supplementary Figure 12B), and some hrGFP+ cells differentiated into GFAP+ glia cells (9.16±1.40%; Supplementary Figure 12C) and mature neurons (VIP+, 17.88±1.55%; calretinin+, 21.28±1.13%; nNOS+, 8.98±0.75%; Supplementary Figure 12D). The migration distance of transplanted hrGFP+ cells was ∼4–8 mm from the transplanted site in recipient SCID mice that is comparable with a previous report studying the transplantation of mouse gut-derived neural crest cells in postnatal mice colon.43
hiPSC-NCSCs can colonize aganglionic human gut tissue in vitro
To determine whether hiPSC-NCSCs have the ability to survive, migrate and differentiate into functional enteric neurons in aganglionic human gut tissue, we further used smooth muscle layers of human aganglionic gut as recipient tissue, including aganglionic gut tissue from HSCR patients and benzalkonium chloride (BAC)-treated ganglionic gut tissue. When co-cultured with the smooth muscle layer of aganglionic gut tissue from HSCR patients, hrGFP-NCSCs exhibited extensive ability to migrate into this recipient tissue by serial observation under fluorescence microscopy (Figure 5a and Supplementary Figure 13A). Most of the gut tissues remained intact after being cultured for 2 weeks (Supplementary Figure 13B). By days 10–13, engrafted cells were radially distributed throughout the smooth muscle regions. Some of the engrafted cells retained expression of the NCSC marker genes p75 (16.58±2.53%) and Sox10 (9.49±2.08%) (n=5; Figure 5b) and of the glial cell marker GFAP (13.12±1.99%) (n=5; Figure 5c). Moreover, some of the transplanted cells differentiated into TUBB3+ neurons (25.21±4.49%); different subtypes of mature neurons expressing nNOS (5.54±1.40%), ChAT (8.62±1.11%), VIP (4.63±0.84%) or TH (2.34±0.59%) were also found in recipient gut tissue (n=5; Figures 5d and e).
Human induced pluripotent stem cell-derived neural crest stem cells (hiPSC-NCSCs) are capable of migration and differentiation in aganglionic gut tissue from Hirschsprung’s disease (HSCR) patients in vitro. (a) hrGFP-NCSCs exhibited extensive ability to migrate into the same human aganglionic gut tissue as observed by serial observation under fluorescence microscopy. (b) Some of engrafted cells retained expression of the NCSC marker genes p75 and Sox10. (c) hrGFP+ cells had the ability to differentiate into GFAP+ glial cells. (d) Transplanted cells differentiated into TUBB3+ neurons; different subtypes of mature neurons expressing neuronal nitric oxide synthase (nNOS), choline acetyltransferase (ChAT), vasoactive intestinal polypeptide (VIP) or tyrosine hydroxylase (TH) were also found in recipient gut tissue. Scale bar, 50 μm. (e) The percentages of p75+, Sox10+, GFAP+, TUBB3+, nNOS+, VIP+, ChAT+ and TH+ neurons differentiated from transplanted hrGFP+ hiPSC-NCSCs were analysed, respectively.
A previous study showed that muscle contraction of the bowel can be recorded by an optical motion capture technique, and they found that the aneural E11.5 mouse bowel displayed uncoordinated contractions in vitro, whereas transplantation of cultured enteric neural progenitors can restore contractility of normal frequency to E11.5 mouse gut explants.42 We then evaluated whether hiPSC-NCSCs could restore the muscle contraction frequency of aganglionic gut tissues from HSCR patients, and we found that the contractions of HSCR aganglionic gut explants were rapid, irregular and significantly more frequent (33.1±3.348 times per s; Supplementary Movie 2) than those of normal ganglionic gut tissues (12.6±1.265 times per s; Supplementary Movie 3; n=10; P<0.01). More importantly, aganglionic gut explants transplanted with neurospheres from hiPSC-NCSCs displayed significantly decreased contraction frequency (13.2±1.398 times per s; Supplementary Movies 4 and 5) that was similar to normal controls (n=10; P>0.05) (Supplementary Figure 13C). These results indicated that hiPSC-NCSCs can restore the intestinal contractile activity of human aganglionic explants.
BAC treatment was found to efficiently induce chemical ablation of myenteric neurons in ganglionic gut tissue, as demonstrated by immunostaining with anti-TUBB3 antibody (Supplementary Figure 14A). When hiPSC-NCSCs were co-cultured with BAC-treated human gut tissue, similar results were observed, with the extensive migration and enteric neuronal differentiation of grafted hrGFP-positive NCSCs, as demonstrated by whole-mount immunostaining of recipient gut tissues with anti-TUBB3 antibody (Supplementary Figure 14B) or immunostaining of tissue sections (Supplementary Figures 15A–D).
Discussion
We described here the generation of enteric-like neurons from hiPSCs via neural crest specification through co-culturing with human gut explants. NCSCs from hiPSCs exhibited the ability to migrate and differentiate into mature neurons expressing phenotypic markers characteristic of enteric neurons, including nNOS, VIP, ChAT and calretinin, upon transplantation into aneural or aganglionic chick, mouse or human gut tissues.
NCSCs have been suggested as powerful tools for the modelling of GI motility disorders and brain/gut dysfunction.5, 44 However, although endoscopic full-thickness biopsy of the gastric wall for the derivation of NCSCs from postnatal human gut is a minimally invasive procedure, intestinal biopsies can still cause side effects or complications, including bowel perforation or excessive bleeding at the biopsy site.45 Moreover, a previous study has shown that NCSCs inside the rat postnatal gut wall are less likely to be truly multipotent, have reduced self-renewal potential and have lost the ability to differentiate into certain subtypes of neurons compared with their fetal-stage counterparts.46 Metzger et al.47 also found that the efficiency of sphere formation from human gut appeared to decrease with increasing postnatal age. However, the small numbers and reduced potential to proliferate of such cells limit their application for disease modelling.
The hiPSCs that have been reprogrammed from somatic cells have the characteristics of indefinite self-renewal capacity and pluripotency, and as such, they offer an ideal in vitro disease model for GI motility disorders. Although it is known that enteric neurons arise from NCSCs, few studies have reported the derivation of enteric neurons from hiPSCs. Therefore, establishing a stable and efficient protocol for the derivation of NCSCs from pluripotent stem cells will provide an ideal cell resource for the generation of enteric neurons. Previous studies showed that human ESCs co-cultured with MS5 or PA6 stromal cells (stromal cell-derived inducing activity) differentiate towards a neural crest fate,48 but the culture conditions for stromal-derived inducing activity have not been fully defined, and it usually requires a longer differentiation process. Furthermore, Kawaguchi et al.49 reported that the forced expression of Sox10 enhances the generation of neural crest progenitors from mouse embryonic stem cells. However, the yield of Sox10-GFP-positive cells was only ~10%.49 Recent studies demonstrated that inhibition of the bone morphogenetic protein and transforming growth factor-β signalling pathways and/or glycogen synthase kinase 3 greatly improved the yield of NCSCs (>90%) from human pluripotent stem cells in a monolayer differentiation protocol.34, 50, 51 To compare the efficiency, repeatability and scalability of the differentiation method from hiPSCs to NCSCs between our method (referred to as ‘bFGF+EGF’) and the published protocols, including ‘LDN+SB’,30 ‘BIO+SB’29 and ‘Chir+SB’,51 we used six hiPSC lines, including two HDF-hiPSC subclones (1 and 2) from the same individual, two iPSC lines from human urine-derived cells (hUC-hiPSCs 1 and hUC-hiPSCs 2)52 and two iPSC lines from human amniotic fluid-derived cells (hAFDC-hiPSCs 1 and hAFDC-hiPSCs 2).53 FACS analysis of the percentage of p75+/HNK1+ in differentiated cell population demonstrated that the ‘LDN+SB’ protocol and our method have better differentiation efficiency and consistency among these hiPSC lines (Supplementary Figures 16 and 17A). Nonetheless, the qPCR analysis for neural crest lineage-specific gene expression among these differentiation protocols demonstrated the NCSCs from our differentiation system expressed relatively higher level neural crest-specific genes, such as p75, HNK1, Sox10 and Ap2α (Supplementary Figure 17B). Therefore, we speculate that the ‘bFGF+EGF’ method through EB formation may recapulate the in vivo neural crest development and provide a new approach for NCSC differentiation from pluripotent stem cells.
A previous study demonstrated that human embryonic stem cell-derived NCSCs with self-renewal and multipotency properties could be maintained in SBio-containing media.29 However, when cultured in SBio-containing medium, freshly isolated hiPSC-derived NCSCs underwent massive apoptosis within 2 days in our study (data not shown). These contradictory results may be attributable to differences in the cell lines and culture conditions used. In this latter context, it has been reported that plating density is critical for the survival of sorted NCSCs, with a minimum of 5–10 × 104 cells per cm2 required when NCSCs are cultured in N2B27 medium containing epidermal growth factor and basic fibroblast growth factor.28 However, we found here that the addition of StemPro neural supplement to NCCM greatly enhanced the survival rate and proliferation potential of sorted NCSCs plated at a lower density (5–10 × 103 cells per cm2).
The iPS technology has opened new opportunities for modelling human diseases and offers a unique way to investigate molecular mechanisms of disease pathogenesis in vitro, such as those of PD54 and Alzheimer’s disease.55 We evaluated the enteric neuron differentiation potential of hiPSC-derived NCSCs, showing that when they were co-cultured with longitudinal muscle layers from gut explants, NCSCs could be induced to differentiate into functional mature enteric-like neurons of different subtypes expressing VIP, ChAT, calretinin or nNOS. Moreover, electrophysiological analysis showed that these cells exhibited functional properties of mature neurons. It is known that a balance between excitatory and inhibitory neurotransmitters controls the movement of gut smooth muscle and that alterations of this balance can contribute to enteric motor dysfunction.3 VIP and NO are primary inhibitory non-adrenergic non-cholinergic transmitters in the gut and are responsible for neurally induced gastric and intestinal relaxation,56 whereas ChAT+ neurons are excitatory muscle motor neurons that can induce cholinergic contractions.57 It was demonstrated that up to 90% of ASD patients suffer from GI problems, and there is a strong correlation between GI disturbances and autism severity.4 Hsiao et al.58 found that oral treatment of ASD model mice with the human commensal Bacteroides fragilis improves gut barrier integrity, to which enteric neurons and glial cells contribute partially,59, 60 and ameliorates defects in communicative, stereotypic, anxiety-like and sensorimotor behaviours highlighting the importance of gut/brain interaction in health and disease.. Braak et al.61 even proposed that a putative environmental pathogen capable of passing the gastric epithelial lining might induce α-synuclein misfolding and aggregation in ENS at a very early stage of PD and reach the brain via the vagal preganglionic innervation of the gut. These results indicate that dysfunction in the gut/brain axis may play an important role in human brain disorders such as ASD and PD because of unknown causes. Therefore, the enteric neuron differentiation model might be used for the establishment of in vitro disease models and provide mechanistic insight into GI disorders or brain/gut dysfunction.
Most recently, Fattahi et al.31 reported the efficient derivation and isolation of ENS progenitors from human PS cells using CD49D as a surface marker and found that in vivo engraftment and migration of these ENS precursors can repopulate the colon and rescue disease-related mortality in the Ednrbs-l/s-l HSCR mouse model. Compared with the data, our study for we believe the first time demonstrates that hiPSC-NCSCs can differentiate into VIP- or calretinin-positive enteric-like neurons. VIP and calretinin have been found to be involved in the pathogenesis of HSCR. Guo et al.62 reported a marked reduction of VIP+ nerve cells and fibres in both the myenteric and submucosal plexuses in affected gut of HSCR patients, an alteration that could lead to uncontrolled contractions that are not followed by relaxation, or to spasms of smooth muscles. The calcium binding protein calretinin plays an important role in calcium homeostasis in the nervous system. Barshack et al.63 found that calretinin is not expressed in aganglionic segments or associated nerve fibres in HSCR that could lead to an accumulation of excess calcium ions inside the cytoplasm and cause neurodegeneration. We also verified that hiPSC-derived enteric neurons are electrophysiologically functional enteric neurons. More importantly, hiPSC-NCSCs can migrate, generate functional enteric neurons and rescue the spasms of smooth muscles in in vitro cultured aganglionic human gut tissues from HSCR patients.
In conclusion, our results indicate that hiPSC-derived enteric NCSCs may supply a powerful tool for studying the pathogenesis of GI disorders, brain/gut dysfunction and ENS development, and they represent a potentially ideal cell resource for autologous cell replacement therapy in GI motility disorders such as HSCR.
References
Lake JI, Heuckeroth RO . Enteric nervous system development: migration, differentiation, and disease. Am J Physiol Gastrointest Liver Physiol 2013; 305: G1–G24.
Avetisyan M, Schill EM, Heuckeroth RO . Building a second brain in the bowel. J Clin Invest 2015; 125: 899–907.
Furness JB . The enteric nervous system and neurogastroenterology. Nat Rev Gastroenterol Hepatol 2012; 9: 286–294.
Grubisic V, Parpura V . The second brain in autism spectrum disorder: could connexin 43 expressed in enteric glial cells play a role? Front Cell Neurosci 2015; 9: 242.
Burns AJ, Thapar N . Neural stem cell therapies for enteric nervous system disorders. Nat Rev Gastroenterol Hepatol 2014; 11: 317–328.
Sharkey KA . Emerging roles for enteric glia in gastrointestinal disorders. J Clin Invest 2015; 125: 918–925.
Mayer EA, Tillisch K, Gupta A . Gut/brain axis and the microbiota. J Clin Invest 2015; 125: 926–938.
Mayer EA, Padua D, Tillisch K . Altered brain-gut axis in autism: comorbidity or causative mechanisms? Bioessays 2014; 36: 933–939.
Lebouvier T, Chaumette T, Paillusson S, Duyckaerts C, Bruley DVS, Neunlist M et al. The second brain and Parkinson's disease. Eur J Neurosci 2009; 30: 735–741.
Neunlist M, Van Landeghem L, Mahe MM, Derkinderen P, des Varannes SB, Rolli-Derkinderen M . The digestive neuronal-glial-epithelial unit: a new actor in gut health and disease. Nat Rev Gastroenterol Hepatol 2013; 10: 90–100.
Huett A, Leong JM, Podolsky DK, Xavier RJ . The cytoskeletal scaffold Shank3 is recruited to pathogen-induced actin rearrangements. Exp Cell Res 2009; 315: 2001–2011.
Raab M, Boeckers TM, Neuhuber WL . Proline-rich synapse-associated protein-1 and 2 (ProSAP1/Shank2 and ProSAP2/Shank3)-scaffolding proteins are also present in postsynaptic specializations of the peripheral nervous system. Neuroscience 2010; 171: 421–433.
Zhang Q, Wang J, Li A, Liu H, Zhang W, Cui X et al. Expression of neurexin and neuroligin in the enteric nervous system and their down-regulated expression levels in Hirschsprung disease. Mol Biol Rep 2013; 40: 2969–2975.
Argyropoulos A, Gilby KL, Hill-Yardin EL . Studying autism in rodent models: reconciling endophenotypes with comorbidities. Front Hum Neurosci 2013; 7: 417.
Grubisic V, Kennedy AJ, Sweatt JD, Parpura V . Pitt-Hopkins mouse model has altered particular gastrointestinal transits in vivo. Autism Res 2015; 8: 629–633.
McElhanon BO, McCracken C, Karpen S, Sharp WG . Gastrointestinal symptoms in autism spectrum disorder: a meta-analysis. Pediatrics 2014; 133: 872–883.
Braak H, Del TK . Invited Article: nervous system pathology in sporadic Parkinson disease. Neurology 2008; 70: 1916–1925.
Braak H, Del TK . Neuroanatomy and pathology of sporadic Parkinson's disease. Adv Anat Embryol Cell Biol 2009; 201: 1–119.
Derkinderen P, Rouaud T, Lebouvier T, Bruley DVS, Neunlist M, De Giorgio R . Parkinson disease: the enteric nervous system spills its guts. Neurology 2011; 77: 1761–1767.
Kupsky WJ, Grimes MM, Sweeting J, Bertsch R, Cote LJ . Parkinson's disease and megacolon: concentric hyaline inclusions (Lewy bodies) in enteric ganglion cells. Neurology 1987; 37: 1253–1255.
Corbille AG, Clairembault T, Coron E, Leclair-Visonneau L, Preterre C, Neunlist M et al. What a gastrointestinal biopsy can tell us about Parkinson's disease? Neurogastroenterol Motil 2016; 28: 966–974.
Takahashi K, Yamanaka S . Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 2006; 126: 663–676.
Robicsek O, Karry R, Petit I, Salman-Kesner N, Muller FJ, Klein E et al. Abnormal neuronal differentiation and mitochondrial dysfunction in hair follicle-derived induced pluripotent stem cells of schizophrenia patients. Mol Psychiatry 2013; 18: 1067–1076.
Madison JM, Zhou F, Nigam A, Hussain A, Barker DD, Nehme R et al. Characterization of bipolar disorder patient-specific induced pluripotent stem cells from a family reveals neurodevelopmental and mRNA expression abnormalities. Mol Psychiatry 2015; 20: 703–717.
Chiang CH, Su Y, Wen Z, Yoritomo N, Ross CA, Margolis RL et al. Integration-free induced pluripotent stem cells derived from schizophrenia patients with a DISC1 mutation. Mol Psychiatry 2011; 16: 358–360.
Heanue TA, Pachnis V . Enteric nervous system development and Hirschsprung's disease: advances in genetic and stem cell studies. Nat Rev Neurosci 2007; 8: 466–479.
Mezey E . The fate of neural crest stem cells: nature vs nurture. Mol Psychiatry 2003; 8: 128–130.
Lee G, Kim H, Elkabetz Y, Al SG, Panagiotakos G, Barberi T et al. Isolation and directed differentiation of neural crest stem cells derived from human embryonic stem cells. Nat Biotechnol 2007; 25: 1468–1475.
Menendez L, Yatskievych TA, Antin PB, Dalton S . Wnt signaling and a Smad pathway blockade direct the differentiation of human pluripotent stem cells to multipotent neural crest cells. Proc Natl Acad Sci USA 2011; 108: 19240–19245.
Kreitzer FR, Salomonis N, Sheehan A, Huang M, Park JS, Spindler MJ et al. A robust method to derive functional neural crest cells from human pluripotent stem cells. Am J Stem Cells 2013; 2: 119–131.
Fattahi F, Steinbeck JA, Kriks S, Tchieu J, Zimmer B, Kishinevsky S et al. Deriving human ENS lineages for cell therapy and drug discovery in Hirschsprung disease. Nature 2016; 531: 105–109.
Ke Q, Li L, Cai B, Liu C, Yang Y, Gao Y et al. Connexin 43 is involved in the generation of human-induced pluripotent stem cells. Hum Mol Genet 2013; 22: 2221–2233.
Cheng F, Ke Q, Chen F, Cai B, Gao Y, Ye C et al. Protecting against wayward human induced pluripotent stem cells with a suicide gene. Biomaterials 2012; 33: 3195–3204.
Chambers SM, Fasano CA, Papapetrou EP, Tomishima M, Sadelain M, Studer L . Highly efficient neural conversion of human ES and iPS cells by dual inhibition of SMAD signaling. Nat Biotechnol 2009; 27: 275–280.
Betancur P, Bronner-Fraser M, Sauka-Spengler T . Assembling neural crest regulatory circuits into a gene regulatory network. Annu Rev Cell Dev Biol 2010; 26: 581–603.
Allan IJ, Newgreen DF . The origin and differentiation of enteric neurons of the intestine of the fowl embryo. Am J Anat 1980; 157: 137–154.
Young HM, Bergner AJ, Anderson RB, Enomoto H, Milbrandt J, Newgreen DF et al. Dynamics of neural crest-derived cell migration in the embryonic mouse gut. Dev Biol 2004; 270: 455–473.
Buitrago-Delgado E, Nordin K, Rao A, Geary L, LaBonne C . NEURODEVELOPMENT. Shared regulatory programs suggest retention of blastula-stage potential in neural crest cells. Science 2015; 348: 1332–1335.
Ross JJ, Hong Z, Willenbring B, Zeng L, Isenberg B, Lee EH et al. Cytokine-induced differentiation of multipotent adult progenitor cells into functional smooth muscle cells. J Clin Invest 2006; 116: 3139–3149.
Sasselli V, Micci MA, Kahrig KM, Pasricha PJ . Evaluation of ES-derived neural progenitors as a potential source for cell replacement therapy in the gut. BMC Gastroenterol 2012; 12: 81.
Smith TH, Ngwainmbi J, Grider JR, Dewey WL, Akbarali HI . An in vitro preparation of isolated enteric neurons and glia from the myenteric plexus of the adult mouse. J Vis Exp 2013; 78: 50688.
Lindley RM, Hawcutt DB, Connell MG, Almond SL, Vannucchi MG, Faussone-Pellegrini MS et al. Human and mouse enteric nervous system neurosphere transplants regulate the function of aganglionic embryonic distal colon. Gastroenterology 2008; 135: 205–216.
Hotta R, Stamp LA, Foong JP, McConnell SN, Bergner AJ, Anderson RB et al. Transplanted progenitors generate functional enteric neurons in the postnatal colon. J Clin Invest 2013; 123: 1182–1191.
Kim YJ, Lim H, Li Z, Oh Y, Kovlyagina I, Choi IY et al. Generation of multipotent induced neural crest by direct reprogramming of human postnatal fibroblasts with a single transcription factor. Cell Stem Cell 2014; 15: 497–506.
Ko CW, Dominitz JA . Complications of colonoscopy: magnitude and management. Gastrointest Endosc Clin N Am 2010; 20: 659–671.
Kruger GM, Mosher JT, Bixby S, Joseph N, Iwashita T, Morrison SJ . Neural crest stem cells persist in the adult gut but undergo changes in self-renewal, neuronal subtype potential, and factor responsiveness. Neuron 2002; 35: 657–669.
Metzger M, Caldwell C, Barlow AJ, Burns AJ, Thapar N . Enteric nervous system stem cells derived from human gut mucosa for the treatment of aganglionic gut disorders. Gastroenterology 2009; 136: 2214–2225.
Pomp O, Brokhman I, Ziegler L, Almog M, Korngreen A, Tavian M et al. PA6-induced human embryonic stem cell-derived neurospheres: a new source of human peripheral sensory neurons and neural crest cells. Brain Res 2008; 1230: 50–60.
Kawaguchi J, Nichols J, Gierl MS, Faial T, Smith A . Isolation and propagation of enteric neural crest progenitor cells from mouse embryonic stem cells and embryos. Development 2010; 137: 693–704.
Lee G, Chambers SM, Tomishima MJ, Studer L . Derivation of neural crest cells from human pluripotent stem cells. Nat Protoc 2010; 5: 688–701.
Chambers SM, Mica Y, Lee G, Studer L, Tomishima MJ . Dual-SMAD inhibition/WNT activation-based methods to induce neural crest and derivatives from human pluripotent stem cells. Methods Mol Biol 2016; 1307: 329–343.
Li D, Wang L, Hou J, Shen Q, Chen Q, Wang X et al. Optimized approaches for generation of integration-free iPSCs from human urine-derived cells with small molecules and autologous feeder. Stem Cell Rep 2016; 6: 717–728.
Kang X, Yu Q, Huang Y, Song B, Chen Y, Gao X et al. Effects of integrating and non-integrating reprogramming methods on copy number variation and genomic stability of human induced pluripotent stem cells. PLoS One 2015; 10: e131128.
Sanchez-Danes A, Richaud-Patin Y, Carballo-Carbajal I, Jimenez-Delgado S, Caig C, Mora S et al. Disease-specific phenotypes in dopamine neurons from human iPS-based models of genetic and sporadic Parkinson's disease. EMBO Mol Med 2012; 4: 380–395.
Israel MA, Yuan SH, Bardy C, Reyna SM, Mu Y, Herrera C et al. Probing sporadic and familial Alzheimer's disease using induced pluripotent stem cells. Nature 2012; 482: 216–220.
Van Geldre LA, Lefebvre RA . Interaction of NO and VIP in gastrointestinal smooth muscle relaxation. Curr Pharm Des 2004; 10: 2483–2497.
Schemann M, Sann H, Schaaf C, Mader M . Identification of cholinergic neurons in enteric nervous system by antibodies against choline acetyltransferase. Am J Physiol 1993; 265 (5 Pt 1): G1005–G1009.
Hsiao EY, McBride SW, Hsien S, Sharon G, Hyde ER, McCue T et al. Microbiota modulate behavioral and physiological abnormalities associated with neurodevelopmental disorders. Cell 2013; 155: 1451–1463.
Savidge TC, Newman P, Pothoulakis C, Ruhl A, Neunlist M, Bourreille A et al. Enteric glia regulate intestinal barrier function and inflammation via release of S-nitrosoglutathione. Gastroenterology 2007; 132: 1344–1358.
Toumi F, Neunlist M, Cassagnau E, Parois S, Laboisse CL, Galmiche JP et al. Human submucosal neurones regulate intestinal epithelial cell proliferation: evidence from a novel co-culture model. Neurogastroenterol Motil 2003; 15: 239–242.
Braak H, de Vos RA, Bohl J, Del TK . Gastric alpha-synuclein immunoreactive inclusions in Meissner's and Auerbach's plexuses in cases staged for Parkinson's disease-related brain pathology. Neurosci Lett 2006; 396: 67–72.
Guo R, Nada O, Suita S, Taguchi T, Masumoto K . The distribution and co-localization of nitric oxide synthase and vasoactive intestinal polypeptide in nerves of the colons with Hirschsprung's disease. Virchows Arch 1997; 430: 53–61.
Barshack I, Fridman E, Goldberg I, Chowers Y, Kopolovic J . The loss of calretinin expression indicates aganglionosis in Hirschsprung's disease. J Clin Pathol 2004; 57: 712–716.
Acknowledgements
This work was supported by the National Basic Research Program of China (2012CBA01302); The National Natural Science Foundation of China (81570487, 81425016, 81271265, 81270646, 81202604, 81371693, 81302223); The Natural Science Foundation of Guangdong Province (S2013030013305, 2014A030313213); Key Scientific and Technological Program of Guangzhou City (201400000003-3, 201300000089, 2010U1-E00551); Guangdong Province Universities and Colleges Pearl River Scholar Funded Scheme (GDUPS, 2013); Frontier and Innovation of Key Technology Project in Science and Technology Department of Guangdong Province (2014B020225007, 2015B020228001, 2016B030229002); Pearl River S&T Nova Program of Guangzhou (2014J2200037); and The Fundamental Research Funds for the Central Universities (13ykpy03).
Author contributions
Substantial contributions to conception and design: AP Xiang, H Xia and W Li; acquisition of data or analysis and interpretation of data: W Li, L Huang, J Zeng, W Lin, K Li, J Sun, W Huang, J Chen, G Wang, Q Ke, J Duan, X Lai, R Chen, M Liu, Y Liu, T Wang, X Yang, Y Chen, H Xia and AP Xiang; drafting the article or revising it critically for important intellectual content: W Li, AP Xiang and H Xia; approval of the final version of the manuscript: AP Xiang, H Xia and W Li.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Molecular Psychiatry website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Li, W., Huang, L., Zeng, J. et al. Characterization and transplantation of enteric neural crest cells from human induced pluripotent stem cells. Mol Psychiatry 23, 499–508 (2018). https://doi.org/10.1038/mp.2016.191
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mp.2016.191
This article is cited by
-
Generation of Functional and Mature Sympathetic Neurons from Human Pluripotent Stem Cells via a Neuroepithelial Route
Journal of Molecular Neuroscience (2024)
-
Tissue engineering of the gastrointestinal tract: the historic path to translation
Journal of Biological Engineering (2022)
-
Rapid and robust derivation of mesenchymal stem cells from human pluripotent stem cells via temporal induction of neuralized ectoderm
Cell & Bioscience (2022)
-
Migration deficits of the neural crest caused by CXADR triplication in a human Down syndrome stem cell model
Cell Death & Disease (2022)
-
Glycan Epitope and Integrin Expression Dynamics Characterize Neural Crest Epithelial-to-Mesenchymal Transition (EMT) in Human Pluripotent Stem Cell Differentiation
Stem Cell Reviews and Reports (2022)