Abstract
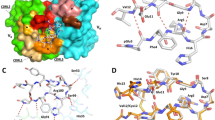
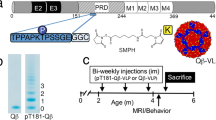
Serum antibodies against amyloid-β peptide (Aβ) in humans with or without diagnosis of Alzheimer's disease (AD) indicate the possibility of immune responses against brain antigens. In an unbiased screening for antibodies directed against brain proteins, we found in AD patients high serum levels of antibodies against the neuronal cytoskeletal protein ankyrin G (ankG); these correlated with slower rates of cognitive decline. Neuronal expression of ankG was higher in AD brains than in nondemented age-matched healthy control subjects. AnkG was present in exosomal vesicles, and it accumulated in β-amyloid plaques. Active immunization with ankG of arcAβ transgenic mice reduced brain β-amyloid pathology and increased brain levels of soluble Aβ42. AnkG immunization induced a reduction in β-amyloid pathology, also in Swedish transgenic mice. Anti-ankG monoclonal antibodies reduced Aβ-induced loss of dendritic spines in hippocampal ArcAβ organotypic cultures. Together, these data established a role for ankG in the human adaptive immune response against resident brain proteins, and they show that ankG immunization reduces brain β-amyloid and its related neuropathology.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Diamond B, Huerta PT, Mina-Osorio P, Kowal C, Volpe BT . Losing your nerves? Maybe it's the antibodies. Nat Rev Immunol 2009; 9: 449–456.
Togo T, Akiyama H, Iseki E, Kondo H, Ikeda K, Kato M et al. Occurrence of T cells in the brain of Alzheimer's disease and other neurological diseases. J Neuroimmunol 2002; 124: 83–92.
Akiyama H, Barger S, Barnum S, Bradt B, Bauer J, Cole GM et al. Inflammation and Alzheimer's disease. Neurobiol Aging 2000; 21: 383–421.
Nitsch RM, Hock C . Targeting beta-amyloid pathology in Alzheimer's disease with Abeta immunotherapy. Neurotherapeutics 2008; 5: 415–420.
Serrano Pozo A, William C, Ferrer I, Delisle M-B, Maurage C-A, Nitsch RM et al. Beneficial effect of human anti-Aβ active immunization (AN1792) on amyloid deposition and neurite morphology. Program No 8255 2009 Neuroscience, Meeting Planner 2009.
Bennett V, Healy J . Organizing the fluid membrane bilayer: diseases linked to spectrin and ankyrin. Trends Mol Med 2008; 14: 28–36.
Paez-Gonzalez P, Abdi K, Luciano D, Liu Y, Soriano-Navarro M, Rawlins E et al. Ank3-dependent SVZ niche assembly is required for the continued production of new neurons. Neuron 2011; 71: 61–75.
Shaw AS, Filbert EL . Scaffold proteins and immune-cell signalling. Nat Rev Immunol 2009; 9: 47–56.
Bertram LBD, Mullin K, Keeney D, Jones J, Basu S, Yhu S et al. Evidence for genetic linkage of Alzheimer's disease to chromosome 10q. Science 2000; 290: 2302–2303.
Myers A, Holmans P, Marshall H, Kwon J, Meyer D, Ramic D et al. Susceptibility locus for Alzheimer's disease on chromosome 10. Science 2000; 290: 2304–2305.
Morgan AR, Turic D, Jehu L, Hamilton G, Hollingworth P, Moskvina V et al. Association studies of 23 positional/functional candidate genes on chromosome 10 in late-onset Alzheimer's disease. Am J Med Genet B Neuropsychiatr Genet 2007; 144B: 762–770.
Cepok S, Zhou D, Srivastava R, Nessler S, Stei S, Bussow K et al. Identification of Epstein-Barr virus proteins as putative targets of the immune response in multiple sclerosis. J Clin Invest 2005; 115: 1352–1360.
Lalive PH, Menge T, Barman I, Cree BA, Genain CP . Identification of new serum autoantibodies in neuromyelitis optica using protein microarrays. Neurology 2006; 67: 176–177.
Horn S, Lueking A, Murphy D, Staudt A, Gutjahr C, Schulte K et al. Profiling humoral autoimmune repertoire of dilated cardiomyopathy (DCM) patients and development of a disease-associated protein chip. Proteomics 2006; 6: 605–613.
Morgan AR, Hamilton G, Turic D, Jehu L, Harold D, Abraham R et al. Association analysis of 528 intra-genic SNPs in a region of chromosome 10 linked to late onset Alzheimer's disease. Am J Med Genet B Neuropsychiatr Genet 2008; 147B: 727–731.
Mohler PJ . Ankyrins and human disease: what the electrophysiologist should know. J Cardiovasc Electrophysiol 2006; 17: 1153–1159.
Zhang X, Bennett V . Restriction of 480/270-kD ankyrin G to axon proximal segments requires multiple ankyrin G-specific domains. J Cell Biol 1998; 142: 1571–1581.
Knobloch M, Konietzko U, Krebs DC, Nitsch RM . Intracellular Abeta and cognitive deficits precede beta-amyloid deposition in transgenic arcAbeta mice. Neurobiol Aging 2007; 28: 1297–1306.
Emmanouilidou E, Melachroinou K, Roumeliotis T, Garbis SD, Ntzouni M, Margaritis LH et al. Cell-produced alpha-synuclein is secreted in a calcium-dependent manner by exosomes and impacts neuronal survival. J Neurosci 2010; 30: 6838–6851.
Aguzzi A, Rajendran L . The transcellular spread of cytosolic amyloids, prions, and prionoids. Neuron 2009; 64: 783–790.
Qazi KR, Gehrmann U, Domange Jordo E, Karlsson MC, Gabrielsson S . Antigen-loaded exosomes alone induce Th1-type memory through a B-cell-dependent mechanism. Blood 2009; 113: 2673–2683.
Morgan D . The role of microglia in antibody-mediated clearance of amyloid-beta from the brain. CNS Neurol Disord Drug Targets 2009; 8: 7–15.
Koenigsknecht-Talboo J, Meyer-Luehmann M, Parsadanian M, Garcia-Alloza M, Finn MB, Hyman BT et al. Rapid microglial response around amyloid pathology after systemic anti-Abeta antibody administration in PDAPP mice. J Neurosci 2008; 28: 14156–14164.
Hsiao K, Chapman P, Nilsen S, Eckman C, Harigaya Y, Younkin S et al. Correlative memory deficits, Abeta elevation, and amyloid plaques in transgenic mice. Science 1996; 274: 99–102.
Zlokovic BV, Deane R, Sagare AP, Bell RD, Winkler EA . Low-density lipoprotein receptor-related protein-1: a serial clearance homeostatic mechanism controlling Alzheimer's amyloid beta-peptide elimination from the brain. J Neurochem 2010; 115: 1077–1089.
Kohler G, Milstein C . Continuous cultures of fused cells secreting antibody of predefined specificity. Nature 1975; 256: 495–497.
Tackenberg C, Brandt R . Divergent pathways mediate spine alterations and cell death induced by amyloid-beta, wild-type tau, and R406W tau. J Neurosci 2009; 29: 14439–14450.
Dzhashiashvili Y, Zhang Y, Galinska J, Lam I, Grumet M, Salzer JL . Nodes of Ranvier and axon initial segments are ankyrin G-dependent domains that assemble by distinct mechanisms. J Cell Biol 2007; 177: 857–870.
Komada M, Soriano P . Beta]IV-spectrin regulates sodium channel clustering through ankyrin-G at axon initial segments and nodes of Ranvier. J Cell Biol 2002; 156: 337–348.
Han L, Cole M, Bellavance F, McCusker J, Primeau F . Tracking cognitive decline in Alzheimer's disease using the mini-mental state examination: a meta-analysis. Int Psychogeriatr 2000; 12: 231–247.
Bordji K, Becerril-Ortega J, Buisson A . Synapses, NMDA receptor activity and neuronal Abeta production in Alzheimer's disease. Rev Neurosci 2011; 22: 285–294.
Holmes C, Boche D, Wilkinson D, Yadegarfar G, Hopkins V, Bayer A et al. Long-term effects of Abeta42 immunisation in Alzheimer's disease: follow-up of a randomised, placebo-controlled phase I trial. Lancet 2008; 372: 216–223, .
Singh VK, Yang YY, Singh EA . Immunoblot detection of antibodies to myelin basic protein in Alzheimer's disease patients. Neurosci Lett 1992; 147: 25–28.
Kellner A, Matschke J, Bernreuther C, Moch H, Ferrer I, Glatzel M . Autoantibodies against beta-amyloid are common in Alzheimer's disease and help control plaque burden. Ann Neurol 2009; 65: 24–31.
Mor F, Izak M, Cohen IR . Identification of aldolase as a target antigen in Alzheimer's disease. J Immunol 2005; 175: 3439–3445.
Mecocci P, Parnetti L, Romano G, Scarelli A, Chionne F, Cecchetti R et al. Serum anti-GFAP and anti-S100 autoantibodies in brain aging, Alzheimer's disease and vascular dementia. J Neuroimmunol 1995; 57: 165–170.
Orgogozo JM, Gilman S, Dartigues JF, Laurent B, Puel M, Kirby LC et al. Subacute meningoencephalitis in a subset of patients with AD after Abeta42 immunization. Neurology 2003; 61: 46–54.
Asuni AA, Boutajangout A, Quartermain D, Sigurdsson EM . Immunotherapy targeting pathological tau conformers in a tangle mouse model reduces brain pathology with associated functional improvements. J Neurosci 2007; 27: 9115–9129.
Masliah E, Rockenstein E, Mante M, Crews L, Spencer B, Adame A et al. Passive immunization reduces behavioral and neuropathological deficits in an alpha-synuclein transgenic model of Lewy body disease. PLoS One 2011; 6: e19338.
Bertram L, Blacker D, Mullin K, Keeney D, Jones J, Basu S et al. Evidence for genetic linkage of Alzheimer's disease to chromosome 10q. Science 2000; 290: 2302–2303.
Ferreira MA, O'Donovan MC, Meng YA, Jones IR, Ruderfer DM, Jones L et al. Collaborative genome-wide association analysis supports a role for ANK3 and CACNA1C in bipolar disorder. Nat Genet 2008; 40: 1056–1058.
Acknowledgements
We thank Dr Annamaria Calella and Dr Sarah Hoey for helpful discussions (University of Zurich); Dr Burkhardt Seifert for help with statistical analysis; Dr Vann Bennett (Duke University Medical Center) for providing us with ankG and ankB recombinant proteins; Dr Uwe Konietzko (University of Zurich) for APP-citrine HEK293 cells; Dr Gang Yu (University of Texas) for HeLa cells expressing the Swedish mutation in APP; Esmeralda Gruber and Dr Anton Gielt for patient care and sampling (University of Zurich); Diana Bundschuh for human DNA genotypig and Sebastian Zurbriggen for help with cell culture (University of Zurich). Rebecca Derungs for help with himmunohistochemistry (University of Zurich). We thank Daniel Schuppli for animal care, Manuela Hitz and Bjorn Henz for technical help in behavioral experiments (University of Zurich). ACS was supported by the Novartis Foundation. AS was supported from the Swiss Commission for Research Partnerships with Developing Countries. LR acknowledges funding support from the Velux foundation, Bangerter Foundation and the Swiss National Science Foundation. MM and RMN were funded by the Swiss National Science Foundation SNSF 3200B0-112616/1, and the National Centre of Competence in Research NCCR ‘Neural Plasticity and Repair’. CH was supported by SNF 320030_125378 and SNF 33CM30_124111. CT was supported from DFG, Ta762/1-1. CB and MG were supported by DFG, (FOR885, GRK1459).
Author contributions
ACS, RMN and MM conceived the study. ACS, RMN, LR, MG, JG, and CH raised funds for the study. ACS, MM, AS, RMN, JB, LR, CT, CB, LK, MTF designed and performed the experiments. TW assisted with the experiments. ACS, RMN, MM, LR, CB, MG, ACS, RMN, MM, supervised the experiments and analyzed the data. ACS, MTF, MM, AS, RMN wrote the drafts of the manuscript. All authors edited the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
A patent application that includes data from this manuscript was filed by the University of Zurich with ACS, MM, JG, CH and RMN listed as inventors.
Additional information
Supplementary Information accompanies the paper on the Molecular Psychiatry website
Rights and permissions
About this article
Cite this article
Santuccione, A., Merlini, M., Shetty, A. et al. Active vaccination with ankyrin G reduces β-amyloid pathology in APP transgenic mice. Mol Psychiatry 18, 358–368 (2013). https://doi.org/10.1038/mp.2012.70
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mp.2012.70
Keywords
This article is cited by
-
AnkG hemizygous mice present cognitive impairment and elevated anxiety/depressive-like traits associated with decreased expression of GABA receptors and postsynaptic density protein
Experimental Brain Research (2017)
-
Statins induce insulin-degrading enzyme secretion from astrocytes via an autophagy-based unconventional secretory pathway
Molecular Neurodegeneration (2015)