Abstract
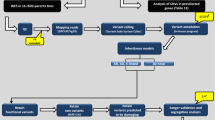
Previous genome-wide linkage studies applied the affected sib-pair design; one investigated extended pedigrees of a genetic isolate. Here, results of a genome-wide high-density linkage scan of attention-deficit/hyperactivity disorder (ADHD) using an array-based genotyping of ∼50 K single nucleotide polymorphism (SNPs) markers are presented. We investigated eight extended pedigrees of German origin that were non-related, not part of a genetic isolate and ascertained on the basis of clinical referral. Two parametric analyses maximizing LOD scores (MOD) and a non-parametric analysis for both a broad and a narrow phenotype approach were conducted. Novel linkage loci across all families were detected at 2q35, 5q13.1, 6q22-23 and 14q12, within individual families at 18q11.2-12.3. Further linkage regions at 7q21.11, 9q22 and 16q24.1 in all families, and at 1q25.1, 1q25.3, 9q31.1-33.1, 9q33, 12p13.33, 15q11.2-13.3 and 16p12.3-12.2 in individual families replicate previous findings. High-resolution linkage mapping points to several novel candidate genes characterized by dense expression in the brain and potential impact on disorder-relevant synaptic transmission. Our study provides further evidence for common gene effects throughout different populations despite the complex multifactorial etiology of ADHD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Faraone SV, Sergeant J, Gillberg C, Biederman J . The worldwide prevalence of ADHD: is it an American condition? World Psychiatry 2003; 2: 104–113.
Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry 2006; 163: 716–723.
Biederman J, Monuteaux MC, Mick E, Spencer T, Wilens TE, Silva JM et al. Young adult outcome of attention deficit hyperactivity disorder: a controlled 10-year follow-up study. Psychol Med 2006; 36: 167–179.
Jacob CP, Romanos J, Dempfle A, Heine M, Windemuth-Kieselbach C, Kruse A et al. Co-morbidity of adult attention-deficit/hyperactivity disorder with focus on personality traits and related disorders in a tertiary referral center. Eur Arch Psychiatry Clin Neurosci 2007; 257: 309–317.
Faraone SV, Perlis RH, Doyle AE, Smoller JW, Goralnick JJ, Holmgren MA et al. Molecular genetics of attention-deficit/hyperactivity disorder. Biol Psychiatry 2005; 57: 1313–1323.
Faraone SV, Khan SA . Candidate gene studies of attention-deficit/hyperactivity disorder. J Clin Psychiatry 2006; 67 (Suppl 8): 13–20.
Friedel S, Saar K, Sauer S, Dempfle A, Walitza S, Renner T et al. Association and linkage of allelic variants of the dopamine transporter gene in ADHD. Mol Psychiatry 2007; 12: 923–933.
Bakker SC, van der Meulen EM, Oteman N, Schelleman H, Pearson PL, Buitelaar JK et al. DAT1, DRD4, and DRD5 polymorphisms are not associated with ADHD in Dutch families. Am J Med Genet B Neuropsychiatr Genet 2005; 132: 50–52.
Smalley SL, Bailey JN, Palmer CG, Cantwell DP, McGough JJ, Del'Homme MA et al. Evidence that the dopamine D4 receptor is a susceptibility gene in attention deficit hyperactivity disorder. Mol Psychiatry 1998; 3: 427–430.
Faraone SV, Perlis RH, Doyle AE, Smoller JW, Goralnick JJ, Holmgren MA et al. Molecular genetics of attention-deficit/hyperactivity disorder. Biol Psychiatry 2005; 57: 1313–1323.
Walitza S, Renner TJ, Dempfle A, Konrad K, Wewetzer C, Halbach A et al. Transmission disequilibrium of polymorphic variants in the tryptophan hydroxylase-2 gene in attention-deficit/hyperactivity disorder. Mol Psychiatry 2005; 10: 1126–1132.
Hebebrand J, Dempfle A, Saar K, Thiele H, Herpertz-Dahlmann B, Linder M et al. A genome-wide scan for attention-deficit/hyperactivity disorder in 155 German sib-pairs. Mol Psychiatry 2006; 11: 196–205.
Ogdie MN, Macphie IL, Minassian SL, Yang M, Fisher SE, Francks C et al. A genomewide scan for attention-deficit/hyperactivity disorder in an extended sample: suggestive linkage on 17p11. Am J Hum Genet 2003; 72: 1268–1279.
Arcos-Burgos M, Castellanos FX, Pineda D, Lopera F, Palacio JD, Palacio LG et al. Attention-deficit/hyperactivity disorder in a population isolate: linkage to loci at 4q13.2, 5q33.3, 11q22, and 17p11. Am J Hum Genet 2004; 75: 998–1014.
Faraone SV, Biederman J, Monuteaux MC . Toward guidelines for pedigree selection in genetic studies of attention deficit hyperactivity disorder. Genet Epidemiol 2000; 18: 1–16.
Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 1997; 36: 980–988.
Schneider S, Margraf J, Unnewehr S . Kinder-DIPS Diagnostisches Interview bei Psychischen Störungen von Kindern. Springer: Berlin, 1995.
Achenbach T, Rescorla L . Manual for the Child Behavior Checklist/6–18. University of Vermont, Department of Psychiatry: Burlington, VT, 2001.
Rosler M, Retz W, Retz-Junginger P, Thome J, Supprian T, Nissen T et al. Tools for the diagnosis of attention-deficit/hyperactivity disorder in adults. Self-rating behaviour questionnaire and diagnostic checklist. Nervenarzt 2004; 75: 888–895.
Döpfner M, Lehmkuhl G . Diagnostik-System für psychische Störungen im Kindes- und Jugendalter nach ICD-10/DSM-IV (DISYPS-KJ), 2nd corrected and extended edition edn. Hans Huber: Bern, 2003.
Sheehan DV, Harnett-Sheehan K, Raj BA . The measurement of disability. Int Clin Psychopharmacol 1996; 11 (Suppl 3): 89–95.
Stiensmeier-Pelster J, Schurmann M, Duda K . Depressions-Inventar fÜr Kinder und Jugendliche (DIKJ), 2nd revised edn. Hogrefe: Göttingen, 2000.
Cattell RB, Weiß R, Osterland J . Grundintelligenztest Skala 1—CFT1. Hogrefe: Goettingen, 1997.
Weiss RH . Grundintelligenztest Skala 2—CFT20. Hogrefe: Goettingen, 1998.
Lehrl S, Triebig G, Fischer B . Multiple choice vocabulary test MWT as a valid and short test to estimate premorbid intelligence. Acta Neurol Scand 1995; 91: 335–345.
Retz-Junginger P, Retz W, Blocher D, Weijers HG, Trott GE, Wender PH et al. Wender Utah rating scale. The short-version for the assessment of the attention-deficit hyperactivity disorder in adults. Nervenarzt 2002; 73: 830–838.
Wender P . Attention-Deficit Hyperactivity Disorder in Adults. Oxford Press: New York, 1995.
Fydrich T, Renneberg B, Schmitz B, Wittchen H-U . SKID II. Interviewheft. Strukturiertes Klinisches Interview fur DSM-IV. Achse II (Persönlichkeitsstörungen). Eine deutschsprachige, erweiterte Bearbeitung der amerikanischen Originalversion des SCID-II von: First, MB, Spitzer, RL, Gibbon, M, Williams, JBW, Benjamin, L (Version 3/96). Hogrefe: Göttingen, 1997.
Wittchen H-U, Wunderlich U, Gruschwitz S, Zaudig M . SKID I. Strukturiertes Klinisches Interview fur DSM-IV. Achse I: Psychische Storungen. Interviewheft und Beurteilungsheft. Eine deutschsprachige, erweiterte Bearbeitung der amerikanischen Originalversion des SCID I. Hogrefe: Göttingen, 1997.
Ruschendorf F, Nurnberg P . ALOHOMORA: a tool for linkage analysis using 10 K SNP array data. Bioinformatics 2005; 21: 2123–2125.
Abecasis GR, Cherny SS, Cookson WO, Cardon LR . Merlin-rapid analysis of dense genetic maps using sparse gene flow trees. Nat Genet 2002; 30: 97–101.
Kruglyak L, Daly MJ, Reeve-Daly MP, Lander ES . Parametric and nonparametric linkage analysis: a unified multipoint approach. Am J Hum Genet 1996; 58: 1347–1363.
Strauch K . Parametric linkage analysis with automatic optimization of the disease model parameters. Am J Hum Genet 2003; 73 (Suppl 1): A2624.
Lander E, Kruglyak L . Genetic dissection of complex traits: guidelines for interpreting and reporting linkage results. Nat Genet 1995; 11: 241–247.
Jain M, Palacio LG, Castellanos FX, Palacio JD, Pineda D, Restrepo MI et al. Attention-deficit/hyperactivity disorder and comorbid disruptive behavior disorders: evidence of pleiotropy and new susceptibility loci. Biol Psychiatry 2007; 61: 1329–1339.
Cordell HJ . Sample size requirements to control for stochastic variation in magnitude and location of allele-sharing linkage statistics in affected sibling pairs. Ann Hum Genet 2001; 65: 491–502.
Fisher SE, Francks C, McCracken JT, McGough JJ, Marlow AJ, MacPhie IL et al. A genomewide scan for loci involved in attention-deficit/hyperactivity disorder. Am J Hum Genet 2002; 70: 1183–1196.
Bakker SC, van der Meulen EM, Buitelaar JK, Sandkuijl LA, Pauls DL, Monsuur AJ et al. A whole-genome scan in 164 Dutch sib pairs with attention-deficit/hyperactivity disorder: suggestive evidence for linkage on chromosomes 7p and 15q. Am J Hum Genet 2003; 72: 1251–1260.
Asherson P, Zhou K, Anney R, Franke B, Buitelaar J, Ebstein R et al. A high density SNP linkage scan with 142 combined subtype ADHD sib pairs identifies linkage regions on chromosomes 9 and 16. Mol Psychiatry 2008; e-pub ahead of print 8 January 2008.
Ogdie MN, Bakker SC, Fisher SE, Francks C, Yang MH, Cantor RM et al. Pooled genome-wide linkage data on 424 ADHD ASPs suggests genetic heterogeneity and a common risk locus at 5p13. Mol Psychiatry 2006; 11: 5–8.
Ogdie MN, Fisher SE, Yang M, Ishii J, Francks C, Loo SK et al. Attention deficit hyperactivity disorder: fine mapping supports linkage to 5p13, 6q12, 16p13, and 17p11. Am J Hum Genet 2004; 75: 661–668.
Niswender KD, Morton GJ, Stearns WH, Rhodes CJ, Myers Jr MG, Schwartz MW . Intracellular signalling. Key enzyme in leptin-induced anorexia. Nature 2001; 413: 794–795.
Okamoto M, Sudhof TC . Mints, Munc18-interacting proteins in synaptic vesicle exocytosis. J Biol Chem 1997; 272: 31459–31464.
Thapar A, Harrington R, McGuffin P . Examining the comorbidity of ADHD-related behaviours and conduct problems using a twin study design. Br J Psychiatry 2001; 179: 224–229.
Acknowledgements
We thank all families for their participation and support. We also greatly appreciate the support from several co-workers, who contributed to organization of the study, data management and technical assistance: Andrea Boreatti-Hümmer, Annette Nowak, Gabriela Ortega, Ulrike Schülter, Nicole Steigerwald, Theresia Töpner. We thank Professor Konstantin Strauch for supporting us in using the program GENEHUNTER-MODSCORE. This study was supported by the Deutsche Forschungsgemeinschaft (DFG: KFO 125, SFB 581, ME 1923/5-1, ME 1923/5-3, GRK 1389/1) and the Bundesministerium für Bildung und Forschung (BMBF: 01GV0605).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Conflict of Interest
The authors declare no competing financial interests.
Author contributions: The study was supervised and directed by KPL, JM, CF and AW. MR, HP, CS and CJ ascertained and clinically characterized the families. JR, TR, MH and SW contributed to clinical characterization of family members. DWC, RB and DAS carried out the genetic analysis. Fine mapping was carried out by JS, CV and JM. Data analyses and genotyping were performed by KPL, MR, TR, AR and co-workers. Statistical analysis was performed by TN, AD and HS; CWK contributed to the power analysis. MR, CF, CJ and KPL wrote and revised the manuscript.
Rights and permissions
About this article
Cite this article
Romanos, M., Freitag, C., Jacob, C. et al. Genome-wide linkage analysis of ADHD using high-density SNP arrays: novel loci at 5q13.1 and 14q12. Mol Psychiatry 13, 522–530 (2008). https://doi.org/10.1038/mp.2008.12
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mp.2008.12
Keywords
This article is cited by
-
Mutations in sphingolipid metabolism genes are associated with ADHD
Translational Psychiatry (2020)
-
Expression of the ADHD candidate gene Diras2 in the brain
Journal of Neural Transmission (2018)
-
Functional Impact of An ADHD-Associated DIRAS2 Promoter Polymorphism
Neuropsychopharmacology (2016)
-
The role of ASTN2 variants in childhood and adult ADHD, comorbid disorders and associated personality traits
Journal of Neural Transmission (2016)
-
MAP1B and NOS1 genes are associated with working memory in youths with attention-deficit/hyperactivity disorder
European Archives of Psychiatry and Clinical Neuroscience (2016)