Abstract
Men who enter active surveillance because their biopsy exhibits only Gleason grade 3 (G3) frequently have higher grade tumor missed by biopsy. Thus, biomarkers are needed that, when measured on G3 tissue, can predict the presence of higher grade tumor in the whole prostate. We evaluated whether PTEN loss, chromosome 8q gain (MYC) and/or 8p loss (LPL) measured only on G3 cores is associated with un-sampled G4 tumor. A tissue microarray was constructed of prostatectomy tissue from patients whose prostates exhibited only Gleason score 3+3, only 3+4 or only 4+3 tumor (n=50 per group). Cores sampled only from areas of G3 were evaluated for PTEN loss by immunohistochemistry, and PTEN deletion, LPL/8p loss and MYC/8q gain by fluorescence in situ hybridization. Biomarker results were compared between Gleason score 6 vs 7 tumors using conditional logistic regression. PTEN protein loss, odds ratio=4.99, P=0.033; MYC/8q gain, odds ratio=5.36, P=0.010; and LPL/8p loss, odds ratio=3.96, P=0.003 were significantly more common in G3 cores derived from Gleason 7 vs Gleason 6 tumors. PTEN gene deletion was not statistically significant. Associations were stronger comparing Gleason 4+3 vs 6 than for Gleason 3+4 vs 6. MYC/8q gain, LPL/8p loss and PTEN protein loss measured in G3 tissue microarray cores strongly differentiate whether the core comes from a Gleason 6 or Gleason 7 tumor. If validated to predict upgrading from G3 biopsy to prostatectomy these biomarkers could reduce the likelihood of enrolling high-risk men and facilitate safe patient selection for active surveillance.
Similar content being viewed by others
Main
Increasing recognition of over-treatment of prostate cancer has stimulated use of active surveillance as a management strategy in select men with low grade, low volume prostate cancer.1, 2 For many active surveillance programs, a key eligibility criterion is biopsy Gleason score 6 or less with no Gleason pattern 4 tumor. However, studies of men with low-risk tumors who were eligible for active surveillance but instead opted for immediate prostatectomy have shown that standard 12 core biopsy misses higher grade tumor in 25–35% of cases with only Gleason 6 on biopsy.1, 3, 4 As active surveillance programs generally perform surveillance (repeat) biopsies on a regular basis, most men under-sampled by the initial biopsy are subsequently detected with higher grade disease and offered curative treatment. Most of these men are found to have Gleason 3+4 tumors at surgery, and have a high probability of cure. However, in 17–32% of these cases Gleason 4+3 or 4+4 (or higher) tumors are found upon prostatectomy, and it is not known if the delay in treatment of such cases compromises the chance of cure.5, 6, 7
Currently, there is a lack of data on biomarkers that consistently show an association with Gleason upgrading from biopsy to radical prostatectomy. Along with others, we have shown that alterations in PTEN (protein or copy number alteration), MYC/8q and LPL/8p are consistently associated with both higher Gleason score tumors, and increased risk of progression or death after prostatectomy.8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18 In particular, we recently showed that PTEN loss is associated with upgrading from Gleason 6 to 7.19
As a result of the consistency with which PTEN loss and chromosome 8p/8q alterations have been associated with aggressive prostate cancer phenotype, they may have potential for identifying men who appear eligible for active surveillance (ie, biopsy Gleason 6) but who actually harbor higher grade tumor that was not detected by biopsy. As active surveillance is most often restricted to men with only Gleason pattern 3 on biopsy, the ideal tissue biomarker would be able to indicate the presence of un-sampled pattern 4 in the prostate when measured on biopsy cores exhibiting only Gleason pattern 3. Therefore, we evaluated whether measurement of PTEN gene or protein, chromosome 8q (MYC) gain, 8p (LPL) loss in Gleason grade 3 (G3) tumor cores could distinguish those that came from Gleason 3+3=6 vs Gleason 3+4 or 4+3=7 tumors.
Materials and methods
All biomarker analyses for the primary analyses were measured only on the G3 component of Gleason 6 or Gleason 7 tumors.
Study Subjects
Records were reviewed retrospectively for men who underwent radical prostatectomy at Johns Hopkins Hospital from 2001 to 2009 to identify those with available paraffin-embedded tumor tissue whose prostatectomy specimen exhibited only a single Gleason score, that is, either Gleason 3+3 only, 3+4 only or 4+3 only. The protocol was approved by the Johns Hopkins Institutional Review Board. Cases were graded according to ISUP 2005.20 Year of surgery was restricted to ensure that no specimens had been stored for >10 years at the time of biomarker analyses. Tumors from men with Gleason 3+3 were identified and matched by age at surgery (±5 years; median 2 years), year of surgery (±3 years; median 1 year), and race to one case of Gleason 3+4 and one case of Gleason 4+3. Fifty men were selected in each of the three Gleason score categories. All tumors had to have adequate tumor volume to accommodate removal of 4 × 0.6 mm tissue cores. Also, cases of 3+3=6 tumor were excluded if there was any tertiary Gleason pattern 4.
Tissue Microarray Construction
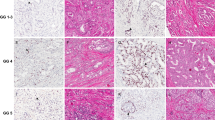
For each patient, four 0.6 mm cores of tumor nodule and four 0.6 mm cores of surrounding benign prostate tissue were manually punched and assembled into a 20 × 20 spot tissue microarray using a Beecher microarrayer as previously described.21 For Gleason 7, tumor cores were sampled from both G3 and G4 areas of tumor (Figure 1). Matched sets (Gleason 3+3, 3+4, 4=3) were placed on the same tissue microarray block, ensuring that comparison groups were processed identically, thus avoiding bias because of batch effects. In cases with Gleason pattern 4, all cores were obtained from separate areas of Gleason pattern 3 and Gleason pattern 4 from ‘index’ tumors (eg, the largest and highest grade tumor in the prostate) that contained both patterns. In other words, the Gleason pattern 3 and 4 were spatially adjacent and part of the same overall tumor nodule. Formalin-fixed and paraffin-embedded cell lines with and without targeted disruption of both PTEN alleles were used as positive and negative controls for immunohistochemistry.12 In addition, benign tissues from a variety of organs were also included as positive controls for staining.
(a) Sampling scheme to select Gleason pattern 3 and Gleason pattern 4 tumor cores from matched cases of Gleason score 3+3, 3+4 and 4+3 for tissue microarray construction. (b) Schematic of tissue microarray construction. Note that four cores from each Gleason pattern were selected for the tissue microarray.
PTEN Immunohistochemistry
PTEN immunohistochemistry was performed manually as previously described12 on 4 μm tissue microarray sections using a rabbit monoclonal α-PTEN antibody (clone D4.3, Cell Signaling Technologies). Tissue microarray slides were scanned using the Aperio ScanScope CS virtual slide scanner (Aperio, Vista, CA, USA) and composite tissue microarray core images were viewed using the TMAJ software package (http://tmaj.pathology.jhmi.edu). Scoring of PTEN expression in tumor cells was performed by two pathologists (ADM and BG), blinded with respect to fluorescence in situ hybridization (FISH) results, pathologic stage and final Gleason score at radical prostatectomy, as well as patient outcome. PTEN protein was visually scored using a dichotomous system,12, 14 and classified as lost if the intensity was markedly decreased or entirely negative across all tumor cells compared with the surrounding benign glands and/or stroma. Each individual patient was classified as markedly decreased for PTEN if any of his tumor spots were classified as markedly decreased. Cases heterogeneous for PTEN loss, in which some tumor cells stained positive, whereas others showed loss within the same core, were recorded as having PTEN loss if >10% of tumor cells within the core were negative or markedly decreased.12 Inter-observer reproducibility for this scoring system (eg, diagnosing a given core with PTEN loss or not) has been shown to be excellent 12 and in this study was 95% for all cores with cancer.
PTEN FISH
From the same tissue microarray blocks used for PTEN protein and chromosome 8 FISH, five sections of 5-μm thickness were cut for FISH analysis. Hematoxylin and eosin (H&E) sections were also cut before and after the sections for FISH and reviewed to insure the sections contained cancer and identify regions of interest. FISH analysis was performed on deparaffinized sections using PTEN and centromere 10 probe kits (Abbott Molecular, Des Plaines, IL, USA). Sixty representative nuclei from the invasive tumor were scored by a trained cytogenetic technologist with overall evaluation by one of us (RBJ). Abnormal criteria were established though evaluation of 93 normal prostate biopsies included on the tissue microarrays, as well as evaluation of the distribution of signal patterns among prostate cancer biopsies on the arrays. PTEN gene loss was defined as PTEN/CEN10 ratio <0.8 and ≥60% of cells enumerated with 0–1 PTEN signals. Cases were further categorized as having homozygous PTEN deletion if >10% of nuclei had 0 PTEN signals. The remaining cases were classified as hemizygous PTEN gene deletion. Cases with PTEN homozygous and hemizygous gene deletion typically had PTEN/CEN10 ratios <0.60 and >0.60/<0.80, respectively. Some cases had gain or loss of a whole chromosome 10. Gain of chromosome 10 required >30% nuclei with three or more PTEN and CEN10 signals. Loss of a whole chromosome 10 required >60% of nuclei with one PTEN and CEN10 signals. Rare cases had two PTEN signals and three CEN10 signals. Such cases were classified as hemizygous PTEN gene deletion.
Chromosome 8q and 8p Alterations (FISH)
The method for LPL and MYC FISH has been previously described in detail.8 Briefly, dual-probe hybridization was performed on tissue microarrays using a centromere 8 probe (chromosome enumeration probe 8 (CEP8); Abbott Molecular) together with a locus-specific probe. An 8p22 probe (LPL gene; Abbott Molecular) and 8q24 probe (MYC gene; Abbott Molecular) were the locus-specific probes. Abnormal criteria were established through evaluation of normal biopsies included on the tissue microarrays. These normal values were similar to those reported by Tsuchiya et al.8 The copy number status of 8p22, 8q24 and CEP8 in a tissue microarray biopsy was classified as normal, gain, duplication or loss. A case was classified as normal if <30% of nuclei had 3 or more signals and <60% of nuclei had 0 or 1 signal for all the probes. LPL was classified as loss if the LPL/CEP8 ratio was <0.85 or if 60% or more nuclei had 0 or 1 LPL signal. MYC was classified as gain if 30% or more nuclei had three or more MYC probe signals. For the MYC gene duplication category, in addition to the gain criteria, it was necessary that the overall mean MYC/CEP8 ratio be >1.3. If both LPL and CEP8 were lost and MYC was normal, MYC was classified as having relative gene duplication.
Statistical Analysis
The primary end point was prostatectomy Gleason 6 vs Gleason 7 (3+4 and 4+3 combined). The primary analyses evaluated whether G3 cores from Gleason 7 tumors were more likely than G3 cores from Gleason 6 tumors to exhibit PTEN protein loss (immunohistochemistry), PTEN gene deletion (FISH), LPL/8p gene loss or MYC/8q gene gain (FISH). For most analyses, PTEN hemizygous or homozygous gene deletion were combined, and MYC/8q gain or duplication were combined. Analyses were done with the patient as unit of analysis, that is, a patient was classified as having the specified biomarker alteration (‘high risk’ status) if any of his G3 tumor cores exhibited the high-risk alteration; otherwise he was classified as ‘normal’ for that biomarker. The sample size was selected to provide power ≥80% to detect a minimum increase of 20% in the prevalence of PTEN protein loss (immunohistochemistry) in Gleason 7 tumors, assuming that the prevalence was ≤10% in Gleason 6 tumors. Descriptive characteristics were compared among Gleason 3+3, 3+4 and 4+3 using analysis of variance with blocking on matched set, or Mantel–Haenszel χ2 test for continuous and categorical variables, respectively. We compared the status of each biomarker with Gleason 7 vs 6 using conditional logistic regression to accommodate matched sets of GS3+3, 3+4 and 4+3. A secondary analysis compared Gleason 6 separately with Gleason 3+4 and to Gleason 4+3. All analyses were performed using SAS v9.3 (SAS Institute, Cary, NC, USA).
Results
There were 50 men in each of the three Gleason score categories (6, 3+4 and 4+3), matched on age (±5 years; median 3 years), race, and year of surgery (±3 years; median 1 year). Of these, 142 (95%) had at least one core of G3 tumor that was informative for all four candidate biomarkers; these 142 men formed the basis for analysis.
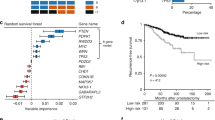
The characteristics of men in each of the three Gleason score groups are shown in Table 1. As expected, both PSA and prostatectomy stage increased significantly with Gleason score. When evaluated only in G3 cores, PTEN protein loss (by immunohistochemistry), MYC/8q gene gain and LPL/8p gene loss (both by FISH) increased significantly with Gleason score, but the association with PTEN gene deletion was not statistically significant, although deletion appeared more frequent among Gleason 4+3 patients. Figure 2a shows the trend between expression of each biomarker with increasing Gleason score. One or more high-risk biomarker alterations were present in G3 cores from 23% of Gleason 3+3 tumors vs 63% of Gleason 3+4 tumors vs 72% of Gleason 4+3 tumors, P<0.0001 for trend. If Gleason score was dichotomized to 6 vs 7, the association with PTEN protein loss, MYC/8q gene gain and LPL/8p gene loss remained significant (P=0.01, <0.0001, <0.0001, respectively), whereas the association with PTEN gene deletion was not statistically significant (P=0.538) (data not shown). None of the four biomarkers were significantly associated with race, age, PSA, PSA density, number of positive biopsy cores, body mass index or year of surgery (data not shown), with the exception of a significant decrease in age associated with MYC/8q gain, P=0.021. PTEN protein loss and LPL/8p gene loss were significantly associated with worse clinical stage, P=0.002 and 0.006, respectively. PTEN protein loss was significantly correlated with PTEN gene deletion, P<0.0001, and LPL/8p loss, P=0.001, but not with MYC/8q gain, P=0.386 (Table 2).
(a) Frequency of PTEN protein loss, PTEN gene deletion, MYC/8q gene gain and LPL/8p gene loss in Gleason pattern 3 cores from matched Gleason score 3+3, 3+4 and 4+3 tumors (n=142). (b) Frequency of biomarker alteration in a grade 3 core is associated with biomarker alteration in at least one matched grade 4 core in Gleason score 7 tumors. *Number of tumors with indicated biomarker alteration in a grade 3 core.
In univariate logistic regression analyses, PTEN protein loss, MYC/8q gene gain and LPL/8p gene loss in a G3 core were associated with a statistically significant four- to fivefold increase in the odds that the tumor was Gleason 7 vs Gleason 6, but PTEN gene deletion (hemizygous or homozygous deletion) was not statistically significant (Table 3). In multivariable models, MYC/8q gain and LPL/8p loss, or MYC/8q gain and PTEN protein loss were independently predictive (both models are considered because the strong collinearity between PTEN protein loss and LPL/8p gene loss makes it questionable to evaluate both variables in the same model).22 Adjustment for age, PSA, clinical stage, number of positive biopsy cores, body mass index or year of surgery did not change the association between biomarkers and prostatectomy Gleason score (data not shown), so only the biomarker results are shown. We also evaluated the impact of having alteration in more than one biomarker. Compared with having no biomarker alterations, having 1, 2 or 3–4 different biomarker alterations in a G3 core was associated with increased likelihood of a Gleason 7 tumor, odds ratio=6.04 (P=0.003), 9.26 (P=0.002) or 10.04 (P=0.015), respectively (data not shown). Forty-one patients (29%) had two or more different biomarker alterations in a G3 core.
In secondary analyses, models were separately constructed with Gleason 6 vs 3+4, and Gleason 6 vs 4+3 (Table 4). For all four biomarkers, associations were stronger with Gleason 4+3 than with Gleason 3+4. For Gleason 3+4, only the association with MYC/8q gain was statistically significant, although all but PTEN gene deletion show elevated odds ratios. In contrast, for Gleason 4+3, PTEN protein loss, MYC/8q gain and LPL/8p loss all show significant positive associations. We also evaluated whether the likelihood of a Gleason 7 tumor increased with the number of G3 cores or percentage of G3 cores exhibiting biomarker alteration. Using either metric, there was a significant association between increased ‘dose’ of cores with MYC/8q gain or LPL/8p loss and likelihood that the cores came from a Gleason 7 tumor. In contrast, having more than one core with PTEN protein loss did not increase the risk of a Gleason 7 tumor beyond the increase observed for one core (data not shown).
Considering all cores (G3 and G4) from patients with Gleason 7 tumors, we evaluated whether biomarker alteration in a G3 core occurred more commonly when the alteration was also present in one of the matched G4 cores. Among tumors with a biomarker alteration in at least one G3 core, 65–78% of tumors also had the alteration in at least one of the matching G4 cores (Figure 2b). These data indicate that alterations in these candidate biomarkers in Gleason 7 tumors rarely occur in G3 glands without concomitant alteration in the G4 glands.
Discussion
Most current protocols for active surveillance depend on biopsy pathology as a major determinant of eligibility, with detection of Gleason G4 frequently indicating the need for treatment rather than surveillance. A limitation of these protocols is that needle biopsy underestimates tumor grade in 25–35% of cases, and in such cases, the true grade may require several rounds of surveillance (follow-up) biopsies before it is revealed or it may be missed altogether.23 Until a signature of aggressive phenotype independent of Gleason grade is developed, biomarkers that can indicate if a biopsy G3 is associated with un-sampled G4 tumor would be a major improvement in our ability to safely assign men to active surveillance. In this study, we have demonstrated that a G3 core that exhibits PTEN protein loss, MYC/8q gene gain or LPL/8p gene loss is much more likely to have come from a Gleason 7 than Gleason 6 tumor, and that the association is even stronger for Gleason 4+3 than 3+4 tumors. PTEN hemiozygous or homozygous gene deletion appeared to be somewhat more common in G3 cores from Gleason 7 tumors, but the difference was not statistically significant.
Our findings suggest that occurrence of these biomarker alterations in G3 tumor foci is a strong indicator of the likely presence of adjacent G4 tumor that was not sampled by the biopsy, and thus, a more aggressive phenotype than expected for a purely pattern 3 histology. Furthermore, we observed that, in Gleason 7 tumors, biomarker alteration in G3 glands is much more likely when the matching G4 glands also exhibit the alteration. These findings are consistent with a recent study that sequenced TMPRSS2 and ERG loci from Gleason 3+4 tumors from four patients whose tumors exhibited a TMPRSS2–ERG fusion event, and found that adjacent G3 and G4 tumor foci exhibited identical breakpoints, indicating that the two Gleason patterns were clonally related.24 In two cases, there was loss of one PTEN allele in both components, yet the Gleason G4 tumor showed loss of both PTEN alleles.24 This finding suggested that, at least at times, a Gleason pattern 4 tumor may clonally evolve from the adjacent Gleason pattern 3 lesion or that they both came from a common precursor lesion and PTEN gene deletion may be a characteristic of such molecular progression.24 Kovtun et al25 also found by next-generation sequencing that tumors with mixed G3 and G4 also showed strong evidence of a clonal relationship. Our study does not address the question of whether a G3 only lesion that was remotely located in the prostate away from any G4 lesion would also have an increased prevalence of PTEN loss, 8p loss or 8q24 gain. Future studies are required to address this important question.
There has been little evaluation of PTEN as a predictor of aggressive phenotype in patients managed by (or eligible for) active surveillance, and we are not aware of studies that have evaluated MYC/8q or LPL/8p in such patients. In a Swedish watchful waiting cohort, a signature associated with embryonic stem cells, p53 mutation or inactivation, and PTEN loss was strongly associated with higher Gleason grade, and with a threefold increase in risk of death.26 In transurethral resection of the prostate specimens from 675 men managed conservatively, Cuzick et al16 observed PTEN protein loss was significantly more prevalent in Gleason 7 (20%) than Gleason 6 tumors (3%). Although not managed conservatively, a small series comparing tumors classified as clinically insignificant according to Epstein criteria (ie, Gleason 6, <3 cores positive, ≤50% of any core involved with tumor; the same criteria used by many institutions to define eligibility for active surveillance) vs clinically significant tumors (predominantly Gleason ≥7), PTEN protein loss was observed in 0/7 insignificant tumors vs 8/19 significant tumors.27
We believe this is the first proof of concept demonstration that biological characteristics of the Gleason pattern 3 component of a Gleason score 7 tumor are distinctly and significantly different than that of a Gleason score 6 tumor, indicating that biopsy Gleason 6 can at times be misleading. The results imply that interrogation of molecular features within a Gleason 6 biopsy can augment the ability of standard Gleason grading by traditional histopathology to predict overall prostate pathology. Indeed, in a recent study, members of our group showed that PTEN protein loss in Gleason 6 biopsies was much more common in tumors that were upgraded to Gleason 7 at prostatectomy compared with tumors that remained Gleason 6 at prostatectomy.19 If replicated in additional studies, these results may stimulate a widespread change in practice to include PTEN immunohistochemistry in apparently low volume Gleason 6 tumors to help determine appropriateness for active surveillance. Further studies using prostate needle biopsies to measure all three biomarkers from this study are clearly warranted.
It is not clear why PTEN gene deletion by FISH did not correlate with increased Gleason score, whereas PTEN protein loss by immunohistochemistry did. Although PTEN gene deletion by FISH did correlate with PTEN protein loss in a highly significant matter (P<0.0001), there were still several discrepancies between these, especially at the individual core level. The largest discrepancy was when PTEN protein was markedly decreased by immunohistochemistry but there was no apparent loss by FISH (21 of 58 discrepant spots; 36%). Along with others, we have previously shown that in 30–40% of cases with PTEN immunohistochemistry loss, there is no underlying PTEN gene deletion detected by FISH.12, 28 The simplest explanation is that, while PTEN protein loss in prostate cancer occurs almost always by deletion (and not point mutations for example), the deletions can be quite small and many of these may not be picked up by the relatively large PTEN FISH probe used in our assay. It is not clear how our results may differ if we use the newer four-color PTEN FISH probes, which are suggested to be more sensitive and specific for finding PTEN deletions than a two-color approach.29, 30 Discrepancy between immunohistochemistry and FISH could also arise if assessment of FISH was performed in a different area than was lost by immunohistochemistry. This could result in cases in which PTEN protein loss by immunohistochemistry is heterogeneous in the tumor core, yet is easily recognized; however, if the part of the core that was not lost by immunohistochemistry was counted by FISH, the case would be likely recorded as having no FISH abnormality. In nine tissue microarray spots, FISH scoring indicated a homozygous deletion yet there was no protein loss recorded by immunohistochemistry. There appeared to be a number of potential reasons for this, perhaps the most important of which is that PTEN immunohistochemistry can be difficult to interpret in a small percentage of cases. Although there was 95% concordance in PTEN calls by different observers in this study overall, in some cores (including 3/9 of the above-described cores), different observers scored the immunohistochemistry differently, indicating that these cores were difficult to call by immunohistochemistry. In one core, there was a clear decrease in immunohistochemistry staining, however, this was not enough to reach a threshold for calling the core markedly decreased. We have shown previously that the specificity of immunohistochemistry staining using this assay is extremely high (eg, ≥95% for mutant cell lines), 12 so it is unlikely that a significant fraction of cores would be misclassified as positive staining when indeed there is no PTEN protein present.
The study has a number of strengths, including matching of Gleason 6 and 7 tumors on age, race and year of surgery, use of well-validated assays, high-quality tissue microarray constructed with tumor samples that exhibited only a single Gleason score and were <10 years old, and inclusion of multiple cores from each grade component. However, there are some limitations. First, the biomarkers were assayed in tissue microarray cores taken from prostatectomy specimens, not biopsies. Although targeted sampling of the index tumor by this approach is an imperfect model of the relatively blind sampling conducted with typical transrectal ultrasound biopsies, it may be a reasonable model of the type of targeted sampling that is becoming increasingly available with MRI-guided biopsies. However, it is clear that additional validation of the joint utility of these biomarkers in a series of biopsies from active surveillance patients is necessary to determine whether biomarker alterations in Gleason 3+3=6 biopsies are more common in patients who are upgraded to Gleason ≥7 during follow-up or surgery. These studies in biopsy specimens are ongoing. Second, as a combination of MRI–ultrasound fusion-guided biopsies with standard systematic biopsies increases the ability to identify tumors with Gleason 7 and higher,31, 32, 33 future studies using the biomarkers herein along with MRI-guided biopsies should be performed to determine the relative value of each; in particular, whether these biomarkers add prognostic information beyond Gleason. Third, the sample size of 142 patients is moderate, and only a relatively small percentage of patients exhibited PTEN protein loss (15%), PTEN gene deletion (14%) and MYC/8q gain (20%). The cohort size and use of only recent cases limited the ability to evaluate clinical outcomes such as biochemical recurrence or metastasis. However, ample data from other studies demonstrate that these biomarker alterations are prognostic for clinical outcomes. Furthermore, associations we observed between biomarker status and grade were not modified by adjustment for other relevant pre-surgical prognostic features.
Conclusions
PTEN protein loss, MYC/8q gain or LPL/8p loss in a G3 tumor core is a strong indicator that the core comes from a Gleason 7 tumor, and occurs even more frequently in G3 cores from Gleason 4+3 than 3+4. Among Gleason 7 tumors, the predominance of these biomarker alterations in both the G3 and G4 cores provides additional evidence that such tumors may be clonally related in many cases. Further, the results suggest that histological Gleason pattern 3 sampled from a Gleason 7 cancer is often biologically distinct from Gleason pattern 3 from a Gleason 6 tumor. Combined with recent data showing that PTEN protein loss is more common in Gleason 6 tumors that are upgraded at prostatectomy,11, 19, 30 and, showing that a PTEN immunohistochemistry assay based on our highly validated approach 12 can now be implemented readily in CLIA-certified pathology laboratories using automated staining systems with a commercial anti-PTEN antibody, 18 these results suggest that these biomarkers may have significant clinical utility for identifying men who are not suitable candidates for active surveillance.
References
Tosoian JJ, JohnBull E, Trock BJ et al. Pathological outcomes in men with low risk and very low risk prostate cancer: implications on the practice of active surveillance. J Urol 2013;190:1218–1222.
Carter HB . Active surveillance for prostate cancer: an underutilized opportunity for reducing harm. J Natl Cancer Inst Monogr 2012;2012:175–183.
Porten SP, Whitson JM, Cowan JE et al. Changes in prostate cancer grade on serial biopsy in men undergoing active surveillance. J Clin Oncol 2011;29:2795–2800.
Epstein JI, Feng Z, Trock BJ et al. Upgrading and downgrading of prostate cancer from biopsy to radical prostatectomy: incidence and predictive factors using the modified Gleason grading system and factoring in tertiary grades. Eur Urol 2012;61:1019–1024.
Tosoian JJ, Sundi D, Trock BJ et al. Pathologic outcomes in favorable-risk prostate cancer: comparative analysis of men electing active surveillance and immediate surgery. Eur Urol 2016;69:576–581.
Xia J, Trock BJ, Cooperberg MR et al. Prostate cancer mortality following active surveillance versus immediate radical prostatectomy. Clin Cancer Res 2012;18:5471–5478.
Iremashvili V, Manoharan M, Rosenberg DL et al. Pathological findings at radical prostatectomy in patients initially managed by active surveillance: a comparative analysis. Prostate 2012;72:1573–1579.
Tsuchiya N, Slezak JM, Lieber MM et al. Clinical significance of alterations of chromosome 8 detected by fluorescence in situ hybridization analysis in pathologic organ-confined prostate cancer. Genes Chromosomes Cancer 2002;34:363–371.
Chen H, Liu W, Roberts W et al. 8q24 allelic imbalance and MYC gene copy number in primary prostate cancer. Prostate Cancer Prostatic Dis 2010;13:238–243.
de Muga S, Hernandez S, Agell L et al. Molecular alterations of EGFR and PTEN in prostate cancer: association with high-grade and advanced-stage carcinomas. Mod Pathol 2010;23:703–712.
El Gammal AT, Bruchmann M, Zustin J et al. Chromosome 8p deletions and 8q gains are associated with tumor progression and poor prognosis in prostate cancer. Clin Cancer Res 2010;16:56–64.
Lotan TL, Gurel B, Sutcliffe S et al. PTEN protein loss by immunostaining: analytic validation and prognostic indicator for a high risk surgical cohort of prostate cancer patients. Clin Cancer Res 2011;17:6563–6573.
Zafarana G, Ishkanian AS, Malloff CA et al. Copy number alterations of c-MYC and PTEN are prognostic factors for relapse after prostate cancer radiotherapy. Cancer 2012;118:4053–4062.
Liu W, Xie CC, Thomas CY et al. Genetic markers associated with early cancer-specific mortality following prostatectomy. Cancer 2013;119:2405–2412.
Yoshimoto M, Ding K, Sweet JM et al. PTEN losses exhibit heterogeneity in multifocal prostatic adenocarcinoma and are associated with higher Gleason grade. Mod Pathol 2013;26:435–447.
Cuzick J, Yang ZH, Fisher G et al. Prognostic value of PTEN loss in men with conservatively managed localised prostate cancer. Br J Cancer 2013;108:2582–2589.
Mithal P, Allott E, Gerber L et al. PTEN loss in biopsy tissue predicts poor clinical outcomes in prostate cancer. Int J Urol 2014;21:6.
Ahearn TU, Pettersson A, Ebot EM et al. A prospective investigation of PTEN loss and ERG expression in lethal prostate cancer. J Natl Cancer Inst 2016;108.
Lotan TL, Carvalho FL, Peskoe SB et al. PTEN loss is associated with upgrading of prostate cancer from biopsy to radical prostatectomy. Mod Pathol 2014;28:129–137.
Epstein JI, Allsbrook WC Jr, Amin MB et alCommittee IG.. The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma. Am J Surg Pathol 2005 29:1228–1242.
Fedor HL, De Marzo AM . Practical methods for tissue microarray construction. Methods Mol Med 2005;103:89–101.
McGee D, Reed D, Yano K . The results of logistic analyses when the variables are highly correlated: an empirical example using diet and CHD incidence. J Chronic Dis 1984;37:713–719.
Han JS, Toll AD, Amin A et al. Low prostate-specific antigen and no Gleason score upgrade despite more extensive cancer during active surveillance predicts insignificant prostate cancer at radical prostatectomy. Urology 2012;80:883–888.
Sowalsky AG, Ye H, Bubley GJ et al. Clonal progression of prostate cancers from Gleason grade 3 to grade 4. Cancer Res 2013;73:1050–1055.
Kovtun IV, Cheville JC, Murphy SJ et al. Lineage relationship of Gleason patterns in Gleason score 7 prostate cancer. Cancer Res 2013;73:3275–3284.
Markert EK, Mizuno H, Vazquez A et al. Molecular classification of prostate cancer using curated expression signatures. Proc Natl Acad Sci USA 2011;108:21276–21281.
Nagao K, Yamamoto Y, Hara T et al. Ki67 and BUBR1 may discriminate clinically insignificant prostate cancer in the PSA range <4 ng/ml. Jpn J Clin Oncol 2011;41:555–564.
Han B, Mehra R, Lonigro RJ et al. Fluorescence in situ hybridization study shows association of PTEN deletion with ERG rearrangement during prostate cancer progression. Mod Pathol 2009;22:1083–1093.
Yoshimoto M, Ludkovski O, DeGrace D et al. PTEN genomic deletions that characterize aggressive prostate cancer originate close to segmental duplications. Genes Chromosomes Cancer 2012;51:149–160.
Phin S, Moore MW, Cotter PD . Genomic rearrangements of PTEN in prostate cancer. Front Oncol 2013;3:240.
Siddiqui MM, Rais-Bahrami S, Truong H et al. Magnetic resonance imaging/ultrasound-fusion biopsy significantly upgrades prostate cancer versus systematic 12-core transrectal ultrasound biopsy. Eur Urol 2013;64:713–719.
Futterer JJ, Briganti A, De Visschere P et al. Can clinically significant prostate cancer be detected with multiparametric magnetic resonance imaging? A systematic review of the literature. Eur Urol 2015;68:1045–1053.
Rastinehad AR, Abboud SF, George AK et al. Reproducibility of multiparametric MRI and fusion-guided prostate biopsy: multi-institutional external validation by a propensity score matched cohort. J Urol, advance online publication, 23 January 2016 (e-pub ahead of print).
Acknowledgements
This work was supported by grants from NIH RC2CA148086 (BJT, RBJ, BSK, SWF, JWS, HBC and ADM); and NIH 5P50CA058236 (BJT, TLL and ADM).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Grant support from Myriad Genetics, Inc. (BJT and ADM). The remaining authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Trock, B., Fedor, H., Gurel, B. et al. PTEN loss and chromosome 8 alterations in Gleason grade 3 prostate cancer cores predicts the presence of un-sampled grade 4 tumor: implications for active surveillance. Mod Pathol 29, 764–771 (2016). https://doi.org/10.1038/modpathol.2016.63
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2016.63
This article is cited by
-
Should Grade Group 1 (GG1) be called cancer?
World Journal of Urology (2022)
-
Genomic and phenotypic heterogeneity in prostate cancer
Nature Reviews Urology (2021)
-
Genetic alterations in the 3q26.31-32 locus confer an aggressive prostate cancer phenotype
Communications Biology (2020)
-
The expression of MYC is strongly dependent on the circular PVT1 expression in pure Gleason pattern 4 of prostatic cancer
Medical Molecular Morphology (2020)
-
Cancer overdiagnosis: a biological challenge and clinical dilemma
Nature Reviews Cancer (2019)