Abstract
In this study, we investigate in detail the morphological, clinical and molecular features of 71 consecutive patients with a diagnosis of myeloproliferative neoplasms, unclassifiable. We performed a meticulous morphological analysis and found that most of the cases displayed a hypercellular bone marrow (70%) with normal erythropoiesis without left-shifting (59%), increased granulopoiesis with left-shifting (73%) and increased megakaryocytes with loose clustering (96%). Megakaryocytes displayed frequent giant forms with hyperlobulated or bulbous nuclei and/or other maturation defects. Interestingly, more than half of the cases displayed severe bone marrow fibrosis (59%). Median values of hemoglobin level and white blood cells count were all within the normal range; in contrast, median platelets count and lactate dehydrogenase were increased. Little less than half of the patients (44%) showed splenomegaly. JAK2V617F mutation was detected in 72% of all patients. Among the JAK2-negative cases, MPLW515L mutation was found in 17% and CALR mutations in 67% of the investigated cases, respectively. Finally, by multiple correspondence analysis of the morphological profiles, we found that all but four of the cases could be grouped in three morphological clusters with some features similar to those of the classic BCR–ABL1-negative myeloproliferative neoplasms. Analysis of the clinical parameters in these three clusters revealed discrepancies with the morphological profile in about 55% of the patients. In conclusion, we found that the category of myeloproliferative neoplasm, unclassifiable is heterogeneous but identification of different subgroups is possible and should be recommended for a better management of these patients.
Similar content being viewed by others
Main
In 2001, the WHO classification of Tumors of hematopoietic and lymphoid tissues defined the criteria for the diagnosis of myeloproliferative neoplasms, unclassifiable. The myeloproliferative neoplasm, unclassifiable category initially included cases with definite clinical and pathological features of myeloproliferative neoplasms but lacking the criteria for a specific entity, that is, myeloproliferative neoplasm cases with truly overlapping features. Within this group, two most frequent subtypes of unclassifiable cases were identified: early stages BCR–ABL1-negative myeloproliferative neoplasms incompletely fulfilling the criteria for a diagnosis of full-blown diseases, and patients with bone marrows examined in advanced stages of myeloproliferative neoplasms, in which the previous diagnosis was unknown.1 In the updated version of the WHO classification, another subgroup of myeloproliferative neoplasms, unclassifiable was introduced comprehending cases with evidences of myeloproliferative neoplasms but in whom coexisting inflammatory or neoplastic conditions masked the myeloproliferative features making the case ‘unclassifiable’.2
The unclassifiable category excluded those cases in which the lack of molecular data useful for a correct classification of the disease or a suboptimal histological specimen may impede a correct classification.
In largest series, the prevalence of myeloproliferative neoplasms, unclassifiable ranges from 10 to 15% of all the cases of BCR–ABL1-negative myeloproliferative neoplasms.3, 4 The presenting clinical symptoms are variable depending from the stage of the disease, but usually include mild to marked leukocytosis and/or thrombocytosis with or without anemia. Organomegaly, which is often absent in patients with early phase myeloproliferative neoplasm, unclassifiable, is seen in advanced stage diseases, where marked splenomegaly and hepatomegaly are often present.
Sometimes, splanchnic vein thrombosis can be the presenting symptoms of myeloproliferative neoplasms.5, 6 Recently, we investigated the clinical, morphological and molecular features of a series of patients with myeloproliferative neoplasms associated with splanchnic vein thrombosis and we found that according to the WHO classification, discrepancies can be found between morphological and clinical features in about half of the cases, which prevent a meaningful subtyping. In these cases, a diagnosis of myeloproliferative neoplasms, unclassifiable is often the best fit.7
Molecular analyses have not been extensively investigated in subsets of patients with myeloproliferative neoplasms, unclassifiable so far. A recent study had reported a frequency of CALR mutations of 37.5% in myeloproliferative neoplasms, unclassifiable cases, whereas JAK2-mutated patients accounted for 25% and triple negative (ie, with no JAK2, CALR or MPL mutation) for another 37.5% of the analyzed cases.8
To the best of our knowledge, there are no studies in the literature specifically addressing diagnostic issues in relation to the WHO myeloproliferative neoplasms, unclassifiable category.
This study is based on the hypothesis that myeloproliferative neoplasms, unclassifiable should not be considered as a ‘basket’ in which to put difficult cases but rather to group cases for which further diagnostic efforts are indicated. Thus, our study aims to define in greater detail the morphological, clinical and molecular features of a large series of myeloproliferative neoplasms, unclassifiable patients, particularly focusing on those features, which suggest a similarity or dissimilarity to the classic subtypes of BCR–ABL1-negative myeloproliferative neoplasms, in an attempt at reducing the frequency of cases in this subgroup. This responds to precise clinical needs and may be helpful in accruing patients to more specific therapeutic trials.
Materials and methods
Patients
We collected all the consecutive patients with a diagnosis of myeloproliferative neoplasms, unclassifiable performed in two reference centers: IRCCS Ca’ Granda—Maggiore Policlinico Hospital Foundation (MPHF, n=46) of Milan and Weill Cornell Medical College (WCMC, n=25) of New York in a period spanning from 2007 to 2015. Seventy-one patients were selected among 1394 cases of newly diagnosed BCR–ABL1-negative myeloproliferative neoplasms, corresponding to a median rate of unclassifiable case of 5% (MPHF: 7% and WCMC: 3%).
For each patient, clinical, laboratory and molecular data, together with the bone marrow biopsy specimens, were available. All the patients gave their informed consent.
Methods
Morphological analysis
Bone marrow biopsy at diagnosis was analyzed using hematoxylin–eosin, Giemsa, and Gomori’s silver impregnation. Four experienced hematopathologists (UG, LB, Y-CL and AO) reviewed all the slides at a multi-headed microscope without any knowledge of the clinical data, with the exception of the patient's age. They performed a detailed morphological analysis considering the following morphological variables, as previously published:9 (1) overall bone marrow cellularity in relation to patient's age; (2) amount of erythropoiesis; (3) left-shifting erythropoiesis; (4) amount of granulopoiesis; (5) left-shifting granulopoiesis; (6) myeloid to erythroid ratio; (7) amount of megakaryocytes; (8) loose clusters of megakaryocytes; (9) dense clusters of megakaryocytes; (10) pleomorphic clusters of megakaryocytes; (11) megakaryocytic nuclear hyperlobulation (‘stag horn-like’ morphology); (12) megakaryocytic bulbous nuclei (‘cloudy-like’ or ‘balloon-shaped’ morphology); (13) megakaryocytic naked nuclei; (14) small megakaryocytes; (15) dysmorphic megakaryocyte; (16) grading of bone marrow fibrosis (determined according to the EUMNET consensus).10 Quantitative morphological variables (numbered 1, 2, 4, 6 and 7) were evaluated with three possible categories (‘reduced’, ‘normal’ or ‘increased’), whereas qualitative variables (numbered 3, 5, 8–16) with two (‘absent’ or ‘present’).
Myeloproliferative neoplasms molecular analyses
The JAK2V617F mutation was detected by allele-specific PCR according to the protocol of Baxter et al11 and confirmed by direct Sanger sequencing. For quantitative analysis of the allele burden of the JAK2V617F mutation, we performed RQ-PCR using JAK2 MutaQuant™ (Ipsogen Inc., New Haven, CT, USA).
MPL mutations, in particular W515L, W515K, W515A, S505N and G509C, were tested by direct sequencing of exon 10. Primer used were: MPL10F 5′-TAGCCTGGATCTCCTTGGTG-3′; MPL10R 5′-CCTGTTTACAGGCCTTCGGC-3′.
Mutations in exon 9 of CALR gene were also assessed by bidirectional sequencing approach as previously described.12 All sequencing analyses were performed on ABI PRISM 310 Genetic Analyzer (Applied Biosystems, Warrington, UK) using the Big Dye Terminator v1.1 Cycle Sequencing Kit (Applied Biosystems).
Statistical Analysis
To investigate the correspondence between the morphological profile of each patient included in this study and that of a reference group for which a clear diagnosis of polycythemia vera, primary myelofibrosis or essential thrombocythemia was available, we used a multiple correspondence analysis. A series of 103 cases of BCR–ABL1-negative myeloproliferative neoplasms, reported in a previous study,9 was used as reference group. In particular, it included 25 cases of polycythemia vera (all in the polycythemic phase of the disease), 44 of primary myelofibrosis (MF-0: n=15, MF-1: n=16, MF-2: n=13) and 34 of essential thrombocythemia.
By means of a multiple correspondence analysis with the reference group, we were able to create a multidimensional space in which all 103 reference cases were placed according to their morphological profiles. The first factorial plane of this multidimensional space explained about 94% of the total variance, and on this plane the 71 patients enrolled in this study were placed as supplementary. In this Euclidean space, each point-patient represented the center of gravity of the own morphological profile.
Results
Clinical–Pathological Features of Myeloproliferative Neoplasms, Unclassifiable
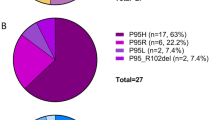
The main clinical–pathological features of the 71 patients evaluated in this study are summarized in Table 1. Regarding laboratory data, the median values of hemoglobin level and white blood cells count were all included in the normal range; the median platelets count and lactate dehydrogenase were instead greater than normal values and less than half of the patients (44%) presented at physical examination with splenomegaly. All our patients were prior evaluated for the presence of the JAK2V617F mutation, which was detected in 51 cases (72%). Among the 20 JAK2-negative cases, two carried the MPLW515L mutation, whereas eight patients carried a mutation in exon 9 of CALR gene: more specifically, we identified four cases of type 1 mutation (del52bp), two cases of type 2 mutation (ins5bp) and two cases carrying other distinct variants, defined as follows: del46bp and del2bp. The remaining eight JAK2-negative patients were not tested neither for CALR nor for MPL mutations.
Morphological Profiles According to the WHO 2008 Classification
Table 2 details the results of the morphological analysis of the 71 cases. In summary, most of the cases displayed a hypercellular bone marrow (70%) with normal erythropoiesis (59%) without left-shifting, and an increased granulopoiesis (73%) with left-shifting. Focusing on megakaryocytes, as expected, loose clusters were present in most of the cases (96%), whereas dense and polymorphic clusters were found in about 32% and 10% of the bone marrow biopsies, respectively. Megakaryocytes displayed frequent giant forms, hyperlobulated or bulbous nuclei and maturation defects.
Interestingly, more than half of the cases (59%) were in the advanced fibrotic stage of the disease (MF-2 or MF-3 according to the EUMNET consensus).10
To investigate the relationship between the morphological profile of each case and the diagnoses of the reference groups, we performed a multiple correspondence analysis. In Figure 1, the horizontal axis contrasts the morphological profiles of the patients affected by essential thrombocythemia versus those affected by primary myelofibrosis, whereas the vertical axis contrasts cases of polycythemia vera versus essential thrombocythemia and primary myelofibrosis. In this figure, each patient with a myeloproliferative neoplasm, unclassifiable is represented by a point and the distance between two patients is proportional to the similarity of their respective profiles. The points indicating the diagnosis represent the centers of gravity of the 103 profiles of the reference groups. As shown in the graph, all but four of the 71 subjects are grouped in three clusters close to the points indicating the diagnosis of the reference groups. This means that 67 cases displayed a morphological profiles similar to those of the reference groups, who determined the structure of the factorial axes and therefore the position of the point of the diagnosis (Table 3).
The degree of accuracy of the map is given by the percentage of total variance represented on the two axes of the map. In this analysis, the percentage of variance explained by the two axes is about 94% (horizontal axis: 77%; vertical axis: 17%).
Discrepancies Between Morphological Profiles and Clinical Features
Four hematologists (AI, DC, NO and FG) were then required to evaluate clinical features of the patients clustered in the three morphological subgroups identified by the multiple correspondence analysis. According to the WHO 2008 criteria, they found that in the cluster of patients with a primary myelofibrosis-like morphology, clinical features were discrepant in 13 out of 25 patients (52%), while in that of patients with an essential thrombocythemia-like morphology, discrepancies were found in 6 out of 26 patients (23%). Interestingly, all the cases with a polycythemia vera-like morphology displayed a discrepant clinical phenotype.
In detail, as reported in Table 4, all the cases with a primary myelofibrosis-like morphological phenotype resulted positive for one of the so-called ‘driver’ mutation (ie, JAK2, CALR or MPL mutations) or carried another clonal marker (trisomy 8, which was detected in all analyzed metaphases in one case), but 13 patients out of 25 did not meet at least three of the four minor diagnostic criteria defined in the updated WHO 2008 classification for primary myelofibrosis (ie, leukoerythroblastosis, increased serum lactate dehydrogenase level, anemia and/or palpable splenomegaly). Interestingly, in six of these unclassified patients, serum erythropoietin levels were inappropriately reduced.
Moreover, considering the cases with an essential thrombocythemia-like morphological phenotype, all of them resulted positive for JAK2, CALR or MPL mutations, or showed no evidence of reactive thrombocytosis, but six patients out of 26 did not meet the first major diagnostic criterion defined in the updated WHO 2008 classification for essential thrombocythemia (ie, platelets count >450 × 109/l).
Finally, none of the patients with a polycythemia vera-like morphological phenotype meets the first major diagnostic criterion defined in the updated WHO 2008 classification for polycythemia vera (ie, hemoglobin >18.5 g/dl in men and >16.5 g/dl in women). Interestingly, three patients out of 14 were negative for both JAK2V617F and exon 12 mutations while carrying in two cases mutations in exon 9 of CALR gene (one type 1 and one type 2 mutation).
Discussion
This study analyzes in detail the clinical, morphological and molecular features of a large series of patients carrying a diagnosis of myeloproliferative neoplasms, unclassifiable. We found that this category is heterogeneous; nevertheless, it was possible to identify different subgroups of patients either from a clinical, or from a morphological point of view.
In our series of myeloproliferative neoplasm, unclassifiable patients, clinical features at presentation were not useful to suggest a specific BCR–ABL1-negative myeloproliferative neoplasm, being represented more frequently by thrombocytosis and, in about half of cases, splenomegaly.
However, some morphological features such as increased bone marrow cellularity, alteration in the myeloid to erythroid ratio, increased number of megakaryocytes with abnormal nuclear features and clustering, together with the presence in more than half of the cases of a significant increase in bone marrow fibrosis, confirmed a diagnosis of myeloproliferative neoplasm in all the patients.
The diagnosis of myeloproliferative neoplasm was also supported by the results of the molecular analyses. In our series, about 86% of the patients carried a so-called ‘driver’ mutation associated with a myeloproliferative phenotype, being JAK2V617F the most frequently represented (72%). In contrast with the study of Kim et al,8 we found a higher rate of JAK2 mutations and a lower rate of CALR mutations and this difference could probably be explained at least in part by the limited number of myeloproliferative neoplasm, unclassifiable cases investigated in the Korean series (ie, 8 versus 71 in this study).
We investigated further which morphological features or the lacking of which did not allow a correct classification of these cases according to the WHO criteria. With this aim, we performed a detailed morphological analysis and a multiple correspondence analysis with reference groups. Three morphological profiles were defined by their similarities to that of classic forms of BCR–ABL1-negative myeloproliferative neoplasms.
According to the WHO classification, in essential thrombocythemia the bone marrow is normocellular for the patients’ age or slightly hypercellular, with normal erythropoiesis and granulopoiesis, and an increased number of large to giants mature megakaryocytes, with hyperlobulated nuclei often forming loose clusters. In essential thrombocythemia, the grade of bone marrow fibrosis is more frequently MF-0 and never more than MF-1.2 In the group of myeloproliferative neoplasms, unclassifiable with an essential thrombocythemia-like morphology, the most frequent discrepancies with the classic morphological profile consisted in a hypercellular bone marrow (50%), with increased granulopoiesis (46%) and an increased number of megakaryocytes sometimes forming dense clusters (15%). Most important, these cases displayed an increased bone marrow fibrosis, ranging from MF-1 to MF-3 in about half of the cases. In this cluster of cases, the main differential diagnosis is between essential thrombocythemia and primary myelofibrosis (Figure 2). The lack of significant atypia of the megakaryocytes does not support a diagnosis of primary myelofibrosis, whereas the frequent finding of a significant increase in bone marrow fibrosis excludes a diagnosis of essential thrombocytemia.
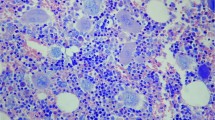
Bone marrow specimen of a 24-year-old female with essential thrombocythemia-like morphology: morphological features do not allow a specific diagnosis. (a) Bone marrow is slightly hypercellular for the patient’s age (HE, 5x); (b) with increased number of megakaryocytes (HE, 10x); (c) sometimes forming little dense clusters, with some atypical forms with bulbous nuclei and increased nuclear to cytoplasmic ratio (HE, 20x). (d) Loose network of reticulin fibers with many intersections can be seen especially in the perivascular area (MF-1) (Gomori, 20x).
The classic morphological profile of primary myelofibrosis, as described in the WHO classification, is characterized by a hypercellular bone marrow, with hyperplastic granulopoiesis and megakaryopoiesis with atypical megakaryocytes often forming dense clusters.2
In the group of myeloproliferative neoplasm, unclassifiable patients with a primary myelofibrosis-like morphology, the overall bone marrow cellularity resulted increased in most of the cases (85%), without a significant hyperplasia of the granulopoietic series. Nevertheless, the myeloid to erythroid ratio resulted increased (89%). In these cases, marked atypia of the megakaryocytes with abnormal, often hypolobated nuclei or a predominance of small dysplastic elements together with a significant increase in bone marrow fibrosis (85%) suggests a differential diagnosis with myelodysplastic/myeloproliferative neoplasms or with the myelofibrotic evolution of a pre-existing myeloproliferative neoplasm (eg, post-polycythemic or post-essential thrombocythemia myelofibrosis) (Figure 3).
Bone marrow specimen of a 64-year-old female, with a previous generic diagnosis of myeloproliferative neoplasm and a primary myelofibrosis-like morphology: morphological features do not allow a specific diagnosis. (a) Hematopoiesis is irregularly distributed (HE, 5x); (b) hypercellular areas with hyperplastic erythropoiesis and granulopoiesis together with dilated sinusoids (HE, 10x) and (c) dense clusters of atypical megakayocytes can be seen (HE, 20x). (d) Diffuse and dense increase in reticulin fibers with extensive intersections and focal bundles of collagen are identifiable (MF-2) (Gomori, 20x).
Regarding the latter differential diagnosis, the latter instance is where you suggest an alternative of myelodysplastic/myeloproliferative neoplasm, particularly in cases with peripheral blood monocytosis where it is necessary to exclude an alternative diagnosis of chronic myelomonocytic leukemia. The search for mutations such as TET2, SRSF2, ASXL1 and SETBP1 in the proper clinical context may be used to support an alternative diagnosis of myelodysplastic/myeloproliferative neoplasms.13, 14 Dysplastic features are regularly seen in cases of myelodysplastic/myeloproliferative neoplasms although they can also occur in advanced stage myeloproliferative neoplasms, unclassifiable. Their presence may cause difficulties and only the knowledge of a previous diagnosis of myeloproliferative neoplasm could support in these rare cases a dysplastic evolution and/or an accelerated phase of a myeloproliferative neoplasm rather than a myelodysplastic/myeloproliferative neoplasm. In the presence of an history of myeloproliferative neoplasm, the identification of increased and clustered CD34-positive hematopoietic precursors also support a diagnosis of an accelerated phase of myeloproliferative neoplasms.
The morphological profile in the polycythemic phase of polycythemia vera is characterized by a marked increase in overall bone marrow cellularity because of panmyelosis with a typical polymorphic aspect of megakaryocytes.2
In our series of myeloproliferative neoplasms, unclassifiable patients with a polycythemia vera-like morphology, bone marrow was more frequently hypercellular (73%) with panmyelotic features, the myeloid to erythroid ratio was frequently normal but the polymorphic aspects of the megakaryocytes clusters were evident only in a small fraction of cases (Figure 4). Moreover, most of them were characterized by a marked increase in bone marrow fibrosis, ranging from MF-2 to MF-3, which probably represents the most important confounding factor.
Bone marrow specimen of a 63-year-old male with a polycythemia vera-like morphology: clinical features do not allow a specific diagnosis. (a) Bone marrow is hypercellular for the patient’s age (HE, 5x); (b) with panmyelosis (HE, 10x); (c) marked increase in the number of megakaryocytes with evident polymorphisms and of the erythropoietic series with left-shifting (Giemsa, 20x). (d) Loose network of reticulin fibers with many intersection can be seen especially in the perivascular area (MF-1) (Gomori, 20x).
These cases need to be differentiated from those of autoimmune myelofibrosis in which proliferation of erythropoiesis and of megakaryocytes is responsible for the hypercellular bone marrow.15 In autoimmune myelofibrosis, megakaryocytes appear morphologically normal, that is, do not display significant atypia as seen in primary myelofibrosis or in other late stages of myeloproliferative neoplasms, and dysplastic features are constantly absent in all hematopoietic lineages. Patients are usually younger than those affected by myeloproliferative neoplasms associated with fibrosis and bone marrow is frequently characterized by lymphoid hyperplasia with reactive lymphoid aggregates and polyclonal plasmacytosis. Finally, JAK2, CALR and MPL mutations have never been found in autoimmune myelofibrosis patients.
In summary, the two most important pathological factors limiting a correct morphological classification of these cases seem to be a morphological profile, which does not completely resemble that of a classic BCR–ABL1-negative myeloproliferative neoplasm, and an advanced bone marrow fibrosis.
Being aware of the limitations of the morphological analysis by the multiple correspondence analysis, we tried to re-classify the cases considering all clinical and molecular data on the basis of the three identified subgroups. Clinical data fitted with morphological features only in 32 out of 67 cases (48%).
In particular, in primary myelofibrosis-like patients minor criteria were frequently lacking, whereas in both the cases with an essential thrombocythemia- or a polycythemia vera-like morphology the absence of one major criteria was the most important confounding factor. Furthermore, among the cases with a polycythemia vera-like morphology, two patients carried mutations in exon 9 of CALR gene (one type 1 and one type 2 mutation), and the latter are actually well-known to be associated only with primary myelofibrosis or essential thrombocythemia.12, 16
This study has several limitations: first, among the 20 cases with unmutated JAK2, mutational status of CALR and MPL genes was not available in eight patients; however, in such cases there was no evidence of reactive thrombocytosis or bone marrow fibrosis. Second, further cooperative studies collecting cases from different institutions are needed to have a more complete representation of this diagnostic category and achieve some more definitive results. Furthermore, a more complete molecular characterization of these cases, comprehending not only the so-called ‘driver’ mutations, is required to better understand whether or not these cases represent only a prodromal or advanced phases of the classic BCR–ABL1-negative myeloproliferative neoplasms. Finally, it has to be emphasized that the clinical evaluation of myeloproliferative neoplasm, unclassifiable cases was based on the WHO 2008 diagnostic criteria, but after the recent introduction of their 2016 revision14 the consensus rate between morphological and clinical diagnosis regarding especially polycythemia vera and primary myelofibrosis is suspected to improve significantly.
In conclusion, this is the first study specifically addressing the issue of a detailed morphological and clinical description of myeloproliferative neoplasm, unclassifiable cases. This diagnostic category is heterogeneous but identification of different subgroups of patients is possible and could probably be necessary for a better management of these patients, with evident clinical consequences.
References
Thiele J, Imbert M, Pierre R et al. Chronic myeloproliferative disease, unclassifiable. In: Jaffe ES, Harris NL, Stein H et al (eds). World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of Haematopoietic and Lymphoid Tissues. IARC Press: Lyon, France, 2001, pp 42–44.
Kvasnicka HM, Bain BJ, Thiele J et al, Myeloproliferative neoplasm, unclassifiable. In: Swerdlow SH, Campo E, Harris NL et al, World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues. IARC Press: Lyon, France, 2008, pp 64–65.
Srour SA, Devesa SS, Morton LM et al. Incidence and patient survival of myeloproliferative neoplasms and myelodysplastic/myeloproliferative neoplasms in the United States, 2001-12. Br J Haematol 2016;174:382–396.
Lin Y, Liu E, Sun Q et al. The prevalence of JAK2, MPL, and CALR mutations in Chinese patients with BCR-ABL1-negative myeloproliferative neoplasms. Am J Clin Pathol 2015;144:165–171.
Thatipelli MR, McBane RD, Hodge DO, Wysokinski WE . Survival and recurrence in patients with splanchnic vein thrombosis. Clin Gastroenterol Hepatol 2010;8:200–205.
Finazzi G, De Stefano V, Barbui T . Are MPNs vascular diseases? Curr Hematol Malig Rep 2013;8:307–316.
Gianelli U, Iurlo A, Cattaneo D et al. Discrepancies between bone marrow histopathology and clinical phenotype in BCR-ABL1-negative myeloproliferative neoplasms associated with splanchnic vein thrombosis. Leuk Res 2015;39:525–529.
Kim SY, Im K, Park SN et al. CALR, JAK2, and MPL mutation profiles in patients with four different subtypes of myeloproliferative neoplasms: primary myelofibrosis, essential thrombocythemia, polycythemia vera, and myeloproliferative neoplasm, unclassifiable. Am J Clin Pathol 2015;143:635–644.
Gianelli U, Bossi A, Cortinovis I et al. Reproducibility of the WHO histological criteria for the diagnosis of Philadelphia chromosome-negative myeloproliferative neoplasms. Mod Pathol 2014;27:814–822.
Thiele J, Kvasnicka HM, Facchetti F et al. European consensus on grading bone marrow fibrosis and assessment of cellularity. Haematologica 2005;90:1128–1132.
Baxter EJ, Scott LM, Campbell PJ et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet 2005;365:1054–1061.
Klampfl T, Gisslinger H, Harutyunyan AS et al. Somatic mutations of calreticulin in myeloproliferative neoplasms. N Engl J Med 2013;369:2379–2390.
Mughal TI, Cross NC, Padron E et al. An International MDS/MPN Working Group's perspective and recommendations on molecular pathogenesis, diagnosis and clinical characterization of myelodysplastic/myeloproliferative neoplasms. Haematologica 2015;100:1117–1130.
Arber DA, Orazi A, Hasserjian R et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood 2016;127:2391–2405.
Vergara-Lluri ME, Piatek CI, Pullarkat V et al. Autoimmune myelofibrosis: an update on morphologic features in 29 cases and review of the literature. Hum Pathol 2014;45:2183–2191.
Nangalia J, Massie CE, Baxter EJ et al. Somatic CALR mutations in myeloproliferative neoplasms with nonmutated JAK2. N Engl J Med 2013;369:2391–2405.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Gianelli, U., Cattaneo, D., Bossi, A. et al. The myeloproliferative neoplasms, unclassifiable: clinical and pathological considerations. Mod Pathol 30, 169–179 (2017). https://doi.org/10.1038/modpathol.2016.182
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2016.182