Abstract
The 2013 CAP/ASCO HER2 Testing Guidelines Update modified HER2 FISH categories such that some cases with ‘monosomy’, ‘co-amplification/polysomy’, low-level increased HER2 signals or clustered heterogeneity now are considered amplified or equivocal. This study examines the frequency and clinico-pathologic characteristics of breast cancers with equivocal or ‘non-classical’ HER2 FISH results. Breast cancers (2001–2014) with HER2 FISH results, HER2 immunohistochemistry, ER, grade, and age from three institutions (Stanford, UCSF, UWMC) were collected. HER2 FISH was interpreted using the updated recommendations. Amplified cases with non-classical results were grouped into the following categories: (1) ‘monosomy’ (ratio ≥2.0, mean HER2/cell<4.0); (2) ‘co-amplified’ (ratio<2.0, mean HER2/cell ≥6.0); (3) ‘low amplified’ (ratio ≥2.0, mean HER2/cell 4.0–5.9). Heterogeneous cases with clustered HER2-positive cells were also included. Of 8068 cases, 5.2% were equivocal and 4.6% had a ‘non-classical’ HER2 amplified result; 1.4% ‘monosomy', 0.8% ‘co-amplified', 2.1% ‘low amplified’, and 0.3% clustered heterogeneity. These cancers had a high frequency of ER positive (80.4%), Nottingham grade 3 (52.1%) results. The highest percentage of grade 3 cancers (66.7%) and positive HER2 immunohistochemistry (31.7%) was in the ‘co-amplified’ group. The ‘monosomy’ group had the highest percent grade 1 cancers (13.3%) and was most frequently HER2 immunohistochemistry negative (30.1%). Equivocal cases had very similar characteristics to the ‘low-amplified’ category. Cases with non-classical HER2 amplification or equivocal results are typically ER positive, higher grade cancers. ‘Co-amplified’ cases have the highest frequencies of aggressive characteristics and ‘monosomy’ cases the highest frequencies of lower risk features. With little clinical outcomes data currently available on these non-classical HER2 results, these results support the current classification scheme for HER2 FISH, with case-by-case correlation with additional clinical-pathologic factors when evaluating whether to offer HER2-targeted therapies in these non-classical cases.
Similar content being viewed by others
Main
The HER2 protein is overexpressed in an estimated 10–20% of primary breast cancers, and prior to the use of HER2-targeted therapies conferred an aggressive phenotype with poor outcomes.1, 2, 3, 4 The advent of HER2-targeted therapies has significantly improved the disease-free and overall survival in patients with tumors displaying HER2 overexpression.5, 6, 7 Patients with HER2-positive tumors can be offered HER2-targeted therapies, such as trastuzumab (Herceptin), lapatinib (Tykerb), pertuzumab (Perjeta) and ado-trastuzumab emtansine/T-DM1 (Kadcyla). However, these treatments are costly and are not without side effects. Therefore, accurate identification of HER2 amplified tumors is pivotal in proper classification and treatment of these patients.
Although most HER2 FISH cases yield a straightforward (or ‘classical’) negative or positive result by both ratio and mean HER2 signals/cell criteria, ‘non-classical’ FISH results can occur when the ratio and signals/cell data would independently yield different results or results are close to a threshold. In 2013 the American Society of Clinical Oncology (ASCO) and the College of American Pathologists (CAP) published updated guidelines for the testing of HER2 in breast cancer.1 With this guideline update the previous HER2 FISH categories were modified such that cases amplified only by HER2:CEP17 ratio ≥2.0 but with mean HER2 signals/cell<6 were now considered amplified (both CEP17 ‘monosomy’-like cases with<4 HER2 signals/cell and ‘low amplified’ cases with between 4 and 6 mean HER2 signals/cell included), as were cases with a negative ratio but>6 mean HER2 signals/cell (‘co-amplified/polysomy’ cases). A clearer definition of heterogeneous cases with clustered populations with HER2 amplification making up >10% of the invasive cancer tested also was included and considered amplified. In addition, the equivocal category was modified to include cases negative by ratio (<2.0) but between 4 and 6 mean HER2 signals/cell. However, the pathology and clinical literature is limited with regard to these the clinical-pathologic features and outcomes of cases in these ‘non-classical’ HER2 FISH categories. Challenges exist among each category, specifically regarding definitions of each chromosomal abnormality/genetic alteration, consensus on interpretation of FISH results and application of the results to clinical situations and management decisions.
The aim of this study was to examine the frequency and clinico-pathologic features of breast cancer with non-classical amplification and equivocal FISH results. Because of the rarity of these cases, data from three major institutions (Stanford, UCSF, and UWMC) were used. Clinical outcomes data were not available.
Materials and methods
After IRB approval at each institution, the pathology databases from Stanford, UCSF, and UWMC were searched for invasive breast cancer cases with HER2 FISH results from 2001 to 2014. Both results from diagnostic core biopsies and surgical specimens were included. Data on the HER2/CEP17 ratio and mean HER2 signals/cell and CEP17 signals/cell for each case were required for a case to be included in the study. The raw HER2 FISH results were interpreted as amplified, equivocal, and non-amplified using the updated 2013 recommendations and the frequencies of these overall categories were recorded. Clinical outcomes were not available.
Cases were then further segregated into categories as defined in Figure 1. ‘Classic amplified’ cases were defined as positive by both ratio ≥2.0, and mean HER2/cell ≥6.0, and ‘classic non-amplified’ cases as negative by both ratio<2.0, and mean HER2 signal/cell<4.0. Equivocal cases were defined as ratio<2.0 and mean HER2 signals/cell between 4.0 and 5.9. Amplified cases with non-classical results were grouped into the following so-named categories defined as follows: (1) ‘monosomy’ (ratio ≥2.0, mean HER2/cell<4.0); (2) ‘co-amplified/polysomy’ (ratio<2.0, mean HER2/cell ≥6.0); (3) ‘low amplified’ (ratio ≥2.0, mean HER2/cell 4.0–5.9). Cases with clusters of amplified cells representing at least 10% of the population were defined as heterogeneous.
The following information was collected from the pathology database from each institution on each ‘non-classic’ and equivocal case as well as a subset of the classical amplified and non-amplified cases: patient age at diagnosis, clinically reported ER status, Nottingham grade and HER2 immunohistochemistry results. The frequencies of different clinical-pathologic characteristics were then calculated for each of these parameters.
Results
HER2 FISH data were available for a total of 8068 cases from the three institutions (Stanford=2449, UCSF=3001, and UWMC=2959). Overall frequencies of the major diagnostic HER2 FISH categories according to the 2013 HER2 guidelines update were 16.0% amplified (both ‘classic’ and ‘non-classic’ types), 5.2% equivocal, and 78.8% non-amplified. In all, 11.4% of the total cases were ‘classical’ amplification and 4.6% were ‘non-classical’ amplification, with non-classical amplified results accounting for 28.8% of the total amplified category. (See Figure 2) The majority of the ‘non-classical’ amplified results were low amplified (44.3% of ‘non-classical’ amplified results; 2.1% of total cases), followed by monosomy (31.9% of ‘non-classical’ amplified; 1.4% of total cases), co-amplified (17.6% of ‘non-classical’ amplified; 0.8% of total cases), and heterogeneous (6.2% of ‘non-classical’ amplified; 0.3% of total cases) (See Figure 3).
Overall frequencies of HER2 FISH result categories. Classic amplified cases were defined as positive by both ratio ≥2.0 and mean HER2/cell ≥6.0 and classic non-amplified cases as negative by both ratio<2.0 and mean HER2 signal/cell<4.0. Equivocal cases were defined as ratio<2.0 and mean HER2 signals/cell between 4.0 and 5.9.
Breakdown of ‘Non-classical’ amplified results. Amplified cases with non-classical results were grouped into the following categories defined as follows: (1) ‘monosomy’ (ratio ≥2.0, mean HER2/cell<4.0); (2) ‘co-amplified/polysomy’ (ratio<2.0, mean HER2/cell ≥6.0); (3) ‘low amplified’ (ratio ≥2.0, mean HER2/cell 4.0–5.9). Cases with clusters of amplified cells representing at least 10% of the population were defined as heterogeneous.
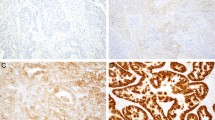
Table 1 and Figure 4 show a summary of the collected clinical-pathologic characteristics for each category of HER2 FISH results.
Overall, ‘non-classical’ amplified cases had a high frequency of ER-positive cancers (78.8%), which was similar to equivocal (82.2%) and classic non-amplified cases (81.3%), whereas the classically amplified cases were less-commonly ER positive (69.2%). Of the ‘non-classical’ amplified categories, the co-amplified and heterogeneous cases had the lowest frequencies of ER-positive cases (75% and 72.2%, respectively) and the low amplified and equivocal cases had the highest (81% and 82%, respectively).
‘Non-classical’ amplified and equivocal cases also had a high frequency of grade 3 cancers (48% and 45.1%, respectively), which was closer to the frequency of grade 3 cancers seen in classic amplified cases (39.2%) than in classic non-amplified cases (21.1%). Conversely, grade 1 cancers were uncommon in the ‘non-classical’ amplified (9.8%) and equivocal cases (9.1%), similar to classic amplified cases (3.5%) and dis-similar to the classic non-amplified cases, which had the highest frequency of grade 1 cancers (25.1%). Of the ‘non-classical’ amplified categories, monosomy cases had the highest frequency of grade 1 cancers (13.3%) and the co-amplified and heterogeneous cases had the highest frequencies of grade 3 cancers (66.7% and 63.2%, respectively).
With the exclusion of heterogeneous cases, the majority of the ‘non-classical’ amplified and equivocal cases were equivocal (+2) by immunohistochemistry (62%). Discordant immunohistochemistry negative (0–1+), FISH-positive cases occurred in 8.5% of all the ‘non-classical’ amplified cases. This was more frequent than in the classic amplified category (2.9% immunohistochemistry negative). The monosomy category had the highest percentage of HER2 immunohistochemistry negative cases (30.1%), but this discordance was also very frequent in both the low-amplified (21.6%) and equivocal categories (25.4%). Co-amplified cases had the highest percentage of positive HER2 immunohistochemistry (31.7%).
The equivocal and low-amplified categories had strikingly similar frequencies of all characteristics. Equivocal and low-amplified cases by definition have the same range of mean HER2 signals/cell (4.0–5.9) and were noted to vary only in the mean CEP17 signals/cell (CEP17 mean of 3.2 for equivocal and 1.9 for low amplified).
The highest frequency of patients younger than 50-year old was seen in the classic amplified cases (38%), followed by ‘non-classic’ amplified (33.8%), classic non-amplified (30%) and equivocal categories (28.1%). Similar mean ages were noted across categories.
Discussion
This multi-institutional review of breast cancer HER2 FISH results provides insight into the frequency of cases with ‘non-classical’ amplification (positive by only ratio or signals/cell criteria but not by both) or equivocal FISH results and their common clinico-pathologic features. Taken together, ‘non-classical’ amplified and equivocal cases account for as much as 9.8%, or close to 1 in 10, of HER2 FISH test results. In general, these categories had high frequencies of ER positivity, similar to the non-amplified category, but were also frequently high grade.
The 2013 CAP/ASCO HER2 guidelines update clearly established that any of the ‘non-classical’ amplified categories we examined are considered a HER2-positive result that makes a patient eligible for HER2-targeted therapies. However, these categories were variably defined prior to the update and remain poorly understood owing to their limited representation in clinical trials. As defined in this study, ‘non-classical’ amplified cases may account for over a quarter of all FISH amplified results, can cause discordance with HER2 immunohistochemistry results and discordance with other clinical-pathologic features. For this reason, the 2013 guidelines update also contains supplemental material discussing these ‘non-classical’ cases in more depth and emphasizing that, while patients should be considered eligible for HER2-targeted therapy, the other clinical-pathologic features present should be considered in making treatment decisions.1
In the face of the limited clinical outcomes data on these cases, acknowledgment of the ‘non-classical’ nature of these HER2 ‘amplified’ or equivocal cases can help explain results that seem discordant and help highlight the clinical options in each case. Table 2 proposes a series of comments (based on the 2013 CAP/ASCO HER2 testing guidelines update) that can be included in pathology reports when reporting HER2 FISH results that are non-classical or equivocal. A more detailed discussion of our results broken down by these categories is as follows:
Monosomy
One of the more controversial ‘non-classical’ amplified categories is cases with very low mean HER2 signals/cell (<4) but an amplified result by HER2:CEP17 ratio>2.0. This frequently occurs in the setting of loss of one CEP17 control signal such that there are <2.0 mean CEP17 signals 2–3 mean HER2 signals/cell. Although we have not technically determined if the cases in our series have true monosomy (loss of a chromosome) or loss of a portion of the chromosome, for ease of category definitions in this study, we have defined cases in this category (ratio ≥2.0 and mean HER2 signals/cell <4) as such. Because of their low mean HER2 signals/cell, these cases will only be scored as amplified when using a dual probe HER2 FISH assay. Subset analysis of the HERA trial data did not suggest reduced trastuzumab benefit for cases that had <4 average HER2 signals/cell and ratio ≥2.0 (although these cases were limited in number), so based on this data, the 2013 CAP/ASCO Guidelines update included such cases in the amplified category.8 However, in the N9831 trastuzumab trial the only cases that did not receive definite trastuzumab benefit were cases that were centrally immunohistochemistry negative and had a FISH ratio>2.0.9 Other studies suggest a reduced response rate to HER2-targeted therapies, without a perceptible effect on the time to progression.10
We saw a low overall frequency of monosomy cases across our institutions, accounting for only 1.4% of all cases. However, monosomy was the ‘non-classical’ amplified category that had the highest percentage of grade 1 cancers (13.3%) and negative HER2 immunohistochemistry results (30.1%), both of which would be considered discordant with a HER2-positive FISH result in any given case. For the monosomy group, we suggest consideration about whether to treat with chemotherapy plus HER2-targeted therapy be based on correlation with all clinico-pathologic characteristics, on a case-by-case basis. For instance, patients with ratio-positive monosomy results that are high grade and HER2 positive by immunohistochemistry might be better candidates for HER2-targeted therapy than patients with low grade, HER2 negative cancers by immunohistochemistry. In addition, if a HER2 immunohistochemistry test has not been performed (as would occur at laboratories that do FISH first or FISH only), concurrent immunohistochemistry may provide additional valuable information when there is a monosomy ‘amplified’ FISH result.
Co-amplified/Polysomy
Cases with increased HER2 and increased CEP17 signals can result in a negative ratio (<2.0) but a positive result by mean HER2 signals/cell (≥6.0). The 2013 CAP/ASCO HER2 Guidelines update classifies these cases as positive for HER2 gene amplification stating that ‘if HER2 signals per cell are >6, assay should be considered positive regardless of ratio’ (see Table 8 of 2013 CAP/ASCO HER2 Guidelines Update) and emphasize that the mean HER2 signals/cell should be reported in addition to the ratio data.1 Data suggest that most cases with these characteristics are not true polysomy (gains of whole chromosomes) but rather co-amplification of the HER2 gene and peri-centromertic regions and therefore should be referred to as ‘co-amplified'.2, 11, 12
The reported frequency of ‘polysomy’ cases ranges from 10 to 54% of breast cancer cases (variable definitions used), with some investigators demonstrating poor prognosis amongst these patients13, 14, 15, 16 In our study, using the definition of ratio<2.0 and mean HER2/cell ≥6.0, co-amplified cases were rare, accounting for only 0.8% of all cases across our institutions.
There is little data on the response of co-amplified cases to HER2-targeted therapies in the absence of HER2 overexpression by immunohistochemistry. However, of the ‘non-classical’ amplified cases in our study, co-amplified cases had the highest percentage of concurrent 3+ HER2 immunohistochemistry (31.7%), with only 13.2% HER2 negative by immunohistochemistry. The recent HERA trial re-analysis of HER2 results by Stoss et al.17 also found cases with ≥6.0 HER2 signals/cell and ratio<2.0 had the highest rates of concurrent 3+ positive immunohistochemistry results across all 2013 HER2 FISH categories. Co-amplified cases in our study also had the highest frequency of grade 3 cancers across all categories (66.7%). Testing by both immunohistochemistry and FISH may be important in some of these cases if results are discordant. Overall, our results support the current classification of co-amplified cases as HER2 amplified with consideration for HER2-targeted treatment.
‘Low Amplified’ and Equivocal
Overall, these two categories were the most common of the non-classical categories in our multi-institutional study, with 5.2% of cases equivocal and 2.1% low amplified. Per the 2013 Guidelines Update, cases with low-level amplification of HER2 (between 4 and 6 mean HER2 signals/cell) are considered amplified if the mean CEP17 signals results in a HER2:CEP17 ratio ≥2.0 (‘non-classical’ low amplified in this study), but would be considered equivocal if the mean CEP17 signals creates a ratio<2.0. Given that these two groups have the same range of mean HER2 signals/cell and the control CEP17 signal is what drives the difference in classification, it is not surprising that our study found almost identical frequencies of additional clinico-pathologic characteristic in these two groups. Both the low-amplified and equivocal cases in our study series had high frequencies of ER positivity, and low frequencies of concurrent 3+ HER2 results by immunohistochemistry. The recent HERA trail re-analysis found similar low rates of 3+ positive immunohistochemistry results in low-amplified and equivocal cases and high frequencies of equivocal immunohistochemistry results.17
With respect to response to HER2-targeted therapies, retrospective review of the original HERA trial results suggest there was still benefit from trastuzumab therapy in the low-amplified group (cases with between 4 and 9 signals/cell).8 Other studies suggest a reduced responsiveness to trastuzumab-based neoadjuvant treatments and decreased time to progression in patients with low-amplified cancers.18, 19, 20 The N9831 trial showed improved disease-free survival for trastuzumab-treated cancers that had a ratio<2.0 by FISH, including cases with 2.0–5.0 mean HER2 signals/cell, but they had all initially tested HER2 positive locally.9 The Update Committee agreed with the FDA statement in the US package insert of trastuzumab that ‘Definitive conclusions cannot be drawn regarding efficacy within other subgroups owing to the small number of events’ in the first generation of trastuzumab trials. Therefore, the 2013 guideline recommendation is to consider low amplified cases positive ‘without the need for further testing'. However, for equivocal cases additional testing was recommended in the guideline.
The supplement to the guidelines does point out that for equivocal cases, co-amplification of the CEP17 region is occasionally observed, which may be the reason behind the ratio being<2.0. In the recent HERA trail re-analysis, 61.1% of the cases that fell in the 2013 equivocal category were noted to have more than three CEP17 signals/cell.17 Similarly, the mean CEP17 signals/cell in our study for the equivocal cases was 3.24. For such cases the guidelines recommend either retesting by other methods (such as immunohistochemistry or single-probe ISH test), retesting on other samples, or FISH using alternative chromosome 17 control probes on the same sample. We have also previously observed high frequencies of cases with intermixed, non-clustered populations of amplified cells in equivocal cases.21 These intermixed amplified cells are non-clustered and together with the majority of non-amplified cells, average to create an equivocal range result. The clinical significance of these ‘mosaic-type’ heterogeneity cases is unclear, but examining the cell counting sheets and reporting the percent amplified cells may be one approach to explain an equivocal result in cases with such findings.
Heterogeneity
The literature on HER2 heterogeneity in breast cancer is fraught with many different definitions, including the non-clustered form (or ‘mosaic’ form), making any conclusions about clinically significant HER2 heterogeneity challenging, with reported frequencies ranging from 1.3 to 54%.22, 23, 24, 25, 26, 27, 28, 29, 30 The updated 2013 ASCO/CAP guidelines recommend defining cases with heterogeneity for HER2 amplification as amplified if the amplified cells are clustered and represent at least 10% of the cancer population being examined.1 Although several studies have shown that tumors with intermixed genetic heterogeneity are associated with low-level HER2 amplification and equivocal HER2 expression, and serve as an independent risk factor for decreased disease-free survival, regional, or clustered heterogeneity as defined by the 2013 Guidelines Update is not well-studied and it is unclear how common this is.24, 26
In our multi-institutional study, clustered heterogeneity was identified in <1% of total cases and these cases were frequently HER2 immunohistochemistry positive (in the FISH amplified areas), grade 3 cancers. This frequency is likely an underestimate as cases in our institutional databases prior to the more specific 2013 definition may not have uniformly been categorized as cases with separate clustered populations of cells. To better identify heterogeneous cases on FISH, the recommendations entail either having the pathologist scan the entire sample under fluorescence to determine whether more than one population is present, and/or utilizing the HER2 immunohistochemistry to guide scoring (see Data Supplement 8, 2013 Guidelines Update), then reporting the percentage of tumor with each FISH/immunohistochemistry pattern.1
Our study is limited by the populations presenting to our institutions and their testing methodologies, but offers a unique look at the frequency and characteristics of different categories of HER2 FISH in a non-trial setting. Although additional clinical outcomes data, such as responses to HER2-targeted therapies in these ‘non-classical’ amplified and equivocal categories, would be ideal, the rarity of these types makes them unlikely to be well-studied in current clinical trial settings. Our results support the concept that the HER2 ‘non-classical’ amplified and equivocal cases frequently have features intermediate between classical amplified and non-amplified cases. In addition, they support the recommendation to consider all the clinico-pathologic features on a case-by-case basis when determining whether to offer HER2-targeted therapies in these difficult cases.
References
Wolff AC, Hammond EH, Hicks DG et al, Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Update. J Clin Oncol 2013; 31: 3997–4010.
Ballinger TJ, Sanders ME, Abramson VG . Current HER2 testing recommendations and clinical relevance as a predictor of response to targeted therapy. Clin Breast Ca 2015; 15: 171–180.
Press MF, Bernstein L, Thomas PA et al, HER-2/neu gene amplification characterized by fluorescence in situ hybridization: poor prognosis in node-negative breast carcinomas. J Clin Oncol 1997; 15: 2894–2904.
Slamon DJ, Clark GM, Wong SG et al, Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 1987; 235: 177–182.
Slamon DJ, Leyland-Jones B, Shak S et al, Use of chemotherapy, plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med 2001; 344: 783–792.
Pogue-Geile KL, Kim C, Jeong JH et al, Predicting degree of benefit from adjuvant tratstuzumab in NSABP trial B-31. J Natl Cancer Inst 2013; 105: 1782–1788.
Perez EA, Romond EH, Suman VJ et al, Four-year follow up of trastuzumab plus adjuvant chemotherapy for operable human epidermal growth factor receptor 2-postive breast cancers: joint analysis of data from NCCTG N9831 and NSABP B-31. J Clin Oncol 2011; 29: 3366–3373.
Dowsett M, Procter M, McCaskill-Stevens W et al, Disease free survival according to degree of HER2 amplification for patients treated with adjuvant chemotherapy with or without 1 year of trastuzumab: The HERA trial. J Clin Oncol 2009; 27: 2962–2969.
Perez EA, Reinholz MM, Hillman DW et al, HER2 and chromosome 17 effect on patient outcome in the N9831 adjuvant trastuzumab trial. J Clin Oncol 2010; 28: 4307–4315.
Risio M, Casorzo L, Redana S et al, HER2 gene-amplified breast cancers with monosomy of chromosome 17 are poorly responsive to trastuzumab-based treatment. Oncol Rep 2005; 13: 305–309.
Vranic S, Teruya B, Repertinger S et al, Assessment of HER2 gene status in breast carcinomas with polysome of chromosome 17. Cancer 2011; 117: 48–53.
Marchio C, Lambros MB, Gugliotta P et al, Does chromosome 17 centromere copy number predict polysomy in breast cancer? A fluorescence in situ hybridization and microarray-based CGH analysis. J Pathol 2009; 219: 16–24.
Vanden BI, Van Loo P, Drijkoningen M et al, Polysomy 17 in breast cancer: clinicopathologic significance and impact on HER-2 testing. J Clin Oncol 2008; 26: 4869–4874.
Hanna WM, Ruschoff J, Bilious M et al, HER2 in situ hybridization in breast cancer: clinical implications of polysomy 17 and genetic heterogeneity. Mod Pathol 2014; 27: 4–18.
Watters AD, Going JJ, Cooke TG, Bartlett JM . Chromosome 17 aneusomy is associated with poor prognostic factors in invasive breast carcinoma. Breast Cancer Res Treat 2003; 77: 109–114.
Kaufman PA, Broadwater G, Lezon-Geyda K et al, CALGB 150002: correlation of HER2 and chromosome 17 (ch17) copy number with trastuzumab (T) efficacy in CALGB 9840, paclitaxel (P) with or without T in HER2+ and HER2- metastatic breast cancer (MBC). J Clin Oncol 2007; 25: 1009.
Stoss OC, Scheel A, Nagelmeier I et al, Impact of updated HER2 testing guidelines in breast cancer—re-evaluation of HERA trial fluorescence in situ hybridization data. Mod Pathol 2015; 28: 1528–1534.
Arnould L, Arveux P, Couturier J et al, Pathologic complete response to trastuzumab-based neoadjuvant therapy is related to the level of HER-2 amplification. Clinc Cancer Res 2007; 13: 6404–6409.
Han HS, Kim JS, Park JH et al, Weekly paclitaxel and trastuzumab as a first-line therapy in patients with HER2-overexpressing metastatic breast cancer: magnitude of HER2/neu amplification as a predictive factor for efficacy. J Korean Med Sci 2009; 24: 910–917.
Lee HJ, Seo AN, Kim EJ et al, HER2 heterogeneity affects trastuzumab responses and survival in patients with HER2-positive metastatic breast cancer. Am J Clin Pathol 2014; 142: 755–766.
Allison KH, Dintzis S, Schmidt R . Frequency of HER2 heterogeneity by fluorescence in situ hybridization according to CAP expert panel recommendations: Time for a new look on how to report heterogeneity. Am J Clin Pathol 2011; 136: 864–871.
Vance GH, Barry TS, Bloom KJ et al, Genetic heterogeneity in HER2 testing in breast cancer: panel summary and guidelines. Arch Pathol Lab Med 2009; 133: 611–612.
Bartlett AI, Starcyznski J, Robson T et al, Heterogeneous HER2 gene amplification: impact on patient outcome and a clinically relevant definition. Am J Clin Pathol 2011; 136: 266–274.
Seol H, Lee HJ, Choi Y et al, Intratumoral heterogeneity of HER2 gene amplification in breast cancer: its clinicopathologic significance. Mod Pathol 2012; 25: 938–948.
Chang MC, Malowany JI, Mazurkiewicz J et al, ‘Genetic heterogeneity’ in HER2/neu testing by fluorescence in situ hybridization: a study of 2,522 cases. Mod Pathol 2012; 25: 638–688.
Lee HJ, Kim JY, Park SY et al, Clinicopathologic significance of the intratumoral heterogeneity of HER2 gene amplification in HER2-positive breast cancer patients treated with adjuvant trastuzumab. Am J Clin Pathol 2015; 144: 570–578.
Lee S, Jung W, Hong SW et al, Evaluation of intratumoral HER-2 heterogeneity by fluorescence in situ hybridization in invasive breast cancer: a single institution study. J Korean Med Sci 2011; 20: 1001–1006.
Perschuk LP, Axiotis CA, Feldman JG et al, Marked intratumoral heterogeneity of the proto-oncogene HER-2/neu determined by three different detection systems. Breast J 1999; 5: 369–374.
Hanna W, Nofech-Mozes S, Kahn HJ . Intratumoral heterogeneity of HER2/neu in breast cancer – a rare event. Breast J 2007; 13: 122–129.
Brunelli M, Manfrin E, Martignoni G et al, Geneotypic intratumoral heterogeneity in breast carcinoma with HER2/neu amplification: evaluation according to ASCO/CAP criteria. Am J Clin Pathol 2009; 131: 678–682.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ballard, M., Jalikis, F., Krings, G. et al. ‘Non-classical’ HER2 FISH results in breast cancer: a multi-institutional study. Mod Pathol 30, 227–235 (2017). https://doi.org/10.1038/modpathol.2016.175
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2016.175
This article is cited by
-
Standardized pathology report for HER2 testing in compliance with 2023 ASCO/CAP updates and 2023 ESMO consensus statements on HER2-low breast cancer
Virchows Archiv (2024)
-
Atypical Co-amplification with Co-localization of HER2 Gene in Breast Cancer: Combined IHC/FISH Approach as per ASCO/CAP 2018 Guidelines for Targeted Therapy Eligibility
Indian Journal of Surgical Oncology (2024)
-
A clinicopathological study and survival analysis of 99 breast cancers with HER2/CEP17 ratio ≥ 2.0 and an average HER2 copy number < 4.0 per cell in China
BMC Cancer (2023)
-
HER2-low breast cancer: evolution of HER2 expression from primary tumor to distant metastases
BMC Cancer (2023)
-
HER2 amplification by next-generation sequencing to identify HER2-positive invasive breast cancer with negative HER2 immunohistochemistry
Cancer Cell International (2022)