Abstract
Pediatric-type follicular lymphoma and pediatric marginal zone lymphoma are two of the rarest B-cell lymphomas. These lymphomas occur predominantly in the pediatric population and show features distinct from their more common counterparts in adults: adult-type follicular lymphoma and adult-type nodal marginal zone lymphoma. Here we report a detailed whole-exome deep sequencing analysis of a cohort of pediatric-type follicular lymphomas and pediatric marginal zone lymphomas. This analysis revealed a recurrent somatic variant encoding p.Lys66Arg in the transcription factor interferon regulatory factor 8 (IRF8) in 3 of 6 cases (50%) of pediatric-type follicular lymphoma. This specific point mutation was not detected in pediatric marginal zone lymphoma or in adult-type follicular lymphoma. Additional somatic point mutations in pediatric-type follicular lymphoma were observed in genes involved in transcription, intracellular signaling, and cell proliferation. In pediatric marginal zone lymphoma, no recurrent mutation was identified; however, somatic point mutations were observed in genes involved in cellular adhesion, cytokine regulatory elements, and cellular proliferation. A somatic variant in AMOTL1, a recurrently mutated gene in splenic marginal zone lymphoma, was also identified in a case of pediatric marginal zone lymphoma. The overall non-synonymous mutational burden was low in both pediatric-type follicular lymphoma and pediatric marginal zone lymphoma (4.6 mutations per exome). Altogether, these findings support a distinctive genetic basis for pediatric-type follicular lymphoma and pediatric marginal zone lymphoma when compared with adult subtypes and to one another. Moreover, identification of a recurrent point mutation in IRF8 provides insight into a potential driver mutation in the pathogenesis of pediatric-type follicular lymphoma with implications for novel diagnostic or therapeutic strategies.
Similar content being viewed by others
Main
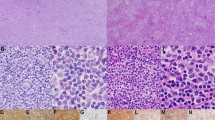
Non-Hodgkin lymphomas are estimated to be the fourth most common malignancy in children and fifth most common in the adolescent and young adult population. Although aggressive mature B-cell lymphomas, including Burkitt lymphoma and diffuse large B-cell lymphoma, comprise a significant proportion of pediatric lymphomas and show many features similar to cases occurring in adults, indolent B-cell lymphomas, including pediatric-type follicular lymphoma and pediatric nodal marginal zone lymphoma, are rare diseases with several distinctive characteristics in presentation and clinical behavior when compared with their adult counterparts.1, 2, 3 Pediatric-type follicular lymphoma is a distinct variant from the adult-type, typically seen between the ages of 3 and 18 years, though cases occurring in young adults have also been described.4, 5 Pediatric-type follicular lymphoma shows a male predominance (approximately 4:1) and most often involves lymph nodes of the cervical regions, though extranodal occurrences in the testis, epididymis, and gastrointestinal tract have been reported.4, 5 The majority of patients with pediatric-type follicular lymphoma, present with localized stage I disease and follow an indolent clinical course. The morphologic features are similar to those of the adult-type follicular lymphoma, with most cases showing increased atypical follicles comprised of cleaved small and larger centroblastic lymphocytes. Despite frequently showing more aggressive cytologic features (often grade 2 or grade 3 in morphology), patients with pediatric-type follicular lymphoma show excellent response rates to local surgical resection or minimal chemotherapy and have very low recurrence rates.4 Pediatric-type follicular lymphoma lacks the characteristic IGH-BCL2; t(14;18)(q32;q21) translocation found in ~80% of adult-type follicular lymphoma with absence of BCL2 protein expression. Recently, Martin–Guerrero et al. described recurrent loss of heterozygosity in 1p36 and association with TNFRSF14 mutations in a small subset of pediatric-type follicular lymphoma patients.6
Comparably, arising from post-germinal center memory B-cells, pediatric nodal marginal zone lymphoma shares similar architectural and immunophenotypic features with the adult-type; however, distinct and characteristically, pediatric nodal marginal zone lymphoma demonstrates a male preponderance (approximately 20:1) and is largely localized to the head and neck regions.7, 8 This lymphoma presents as stage 1 localized disease and carries an excellent prognosis and overall low rate of recurrence.9 Genetic aberrations in pediatric nodal marginal zone lymphoma have been described, with the most frequent alteration seen being trisomy 18 (17%), which is also a frequent cytogenetic abnormality found in adult-type nodal marginal zone lymphoma.10, 11 Similar to pediatric-type follicular lymphoma, definitive diagnosis of pediatric nodal marginal zone lymphoma and separation from similar morphologic entities remains challenging.
Given the propensity for some overlapping features between pediatric-type follicular lymphoma and pediatric nodal marginal zone lymphoma and the paucity of literature describing the genetic landscape of these distinct entities, we performed whole-exome deep sequencing (>140-fold coverage) on 10 cases of pediatric nodal marginal zone lymphoma and pediatric-type follicular lymphoma, as well as Sanger sequencing on two additional cases, to characterize the mutational signature of these rare tumors and search for additional driver mutations and involved biological pathways. Our analysis identified a novel recurrent somatic point mutation in pediatric-type follicular lymphoma in the transcription factor interferon regulator factor 8/interferon consensus-binding protein (IRF8/ICSBP), c.197A>G encoding p.Lys66Arg. Additional somatic variants were observed in pediatric-type follicular lymphoma and pediatric nodal marginal zone lymphoma including mutations in genes involved in transcription, intracellular signaling and cellular organization though there was an overall low rate of non-synonymous mutations (4.6 mutations per case).
Materials and methods
Case Selection
Case records from the Department of Pathology, Stanford University Medical Center and Seattle Children’s Hospital were reviewed from 1996 to 2015 for cases with a diagnosis of marginal zone lymphoma or follicular lymphoma in patients <30 years of age. All hematoxylin and eosin-stained slides, as well as all available supplementary material, were reviewed confirming the previously rendered diagnoses according to WHO criteria.8 A total of 12 cases were identified, 6 cases of pediatric-type follicular lymphoma and 6 cases of pediatric nodal marginal zone lymphoma. From this cohort, the clinical and morphologic features of one pediatric-type follicular lymphoma case with paired tumor-normal (uninvolved lymph node) set were recently reported.12 An additional 22 cases of adult-type follicular lymphoma were selected as additional controls: 14 cases of adult-type follicular lymphoma grade 1–2; 6 cases of adult-type follicular lymphoma grade 3A; and 2 cases of adult-type follicular lymphoma grade 3B. This study was approved by Stanford’s institutional review board.
Exome Library Preparation and Sequencing
Library preparation and exome sequencing were performed as previously described.13, 14 In brief, DNA was extracted from formalin-fixed paraffin embedded tissue using Qiagen DNeasy kits according to the manufacturer’s protocols. The Agilent SureSelect Exon V5 target enrichment system was used to enrich for a 51-Mb exome following Illumina Hiseq 2500 V3 platform sequencing using 100-bp paired-end reads, with high output mode coverage at 200 × with 2 × 100 PE read length.
Alignment, Single-Nucleotide Variant, Copy-Number Variant and Indel Analysis
DNA sequence alignment was performed using BWA-MEM. Mutation analysis was performed with three mutation callers, Mutect (version 1.17), SureCall SNPPET (version 3.0, Agilent Technologies), and Varscan2.15, 16 For all samples, callers were run with default settings in individual sample analysis modes. In order to call a mutation, 20 × coverage of the base analyzed (as defined by the mutation caller itself) was required, as well as coverage in both the forward and reverse directions. Unequal representation of read counts (>80%/20% split) was additionally discounted. For the sample with a paired control, acquired mutations were considered when the allele frequency of the variant in the disease sample at least doubled the allele frequency of the variant in the control sample. For samples without a matched control, a minimum allele frequency of 0.1 was required in addition to the coverage restriction for initial analysis. Single-nucleotide polymorphisms identified in dbSNP, Exome Aggregation Consortium and Exome Variant Server were additionally curated and removed from further analysis. DNA from a paired normal lymph node sample, and three additional lymph nodes in unrelated patients without involvement by lymphoma were also sequenced: variants identified in case samples were compared with these controls to curate recurrent sequencing errors (ie, homopolymer errors, recurrent errors in GC-rich regions). Gene annotations were performed with SeattleSeq138 and Surecall (version 3.0; Agilent Technologies). Indel analysis was performed with GATK, Surecall, and Varscan2. GATK was run according to the Best Practices guidelines, with SureCall and VarScan2 run with default parameters. The above variant filtration was similarly applied to indel analysis. Copy-number variation analysis was performed with CNVSeq, run with default parameters, and analysis performed on the ‘hits’ file.
Sanger Sequencing of IRF8
Sanger sequencing was performed to detect the candidate IRF8 variant with primers designed using PrimerQuest; primers are listed in Supplementary Table S1. Amplified DNA was sequenced and visualized using 4Peaks.17
Multi-Species Alignment and Single-Nucleotide Variant Effect Prediction
Data for the vertebrate MULTIZ alignments were retrieved from the UCSC Genome Browser, assembly ID: hg38. The translated regions comprising IRF8 exon 1 and exon 2 were extracted and analyzed for conservation of K66. Three-dimensional protein structure homology modelling was performed using SWISS-MODEL as described.18 PolyPhen-2 and SIFT prediction algorithms were employed as previously described.19, 20
Results
Whole-Exome Sequencing and Data Analysis of Pediatric-Type Follicular Lymphoma and Pediatric Nodal Marginal Zone Lymphoma
To identify potential driver mutations, as well as characterize the mutational landscape of pediatric-type follicular lymphoma and pediatric nodal marginal zone lymphoma, we performed whole-exome deep sequencing (>140-fold coverage) on six cases of pediatric-type follicular lymphoma, with one paired tumor-normal set, and four cases of pediatric nodal marginal zone lymphoma. All pediatric-type follicular lymphoma and pediatric nodal marginal zone lymphoma cases were identified in patients aged 18 years or less (range: 12–18 years). The cases were reviewed, and the morphologic and immunophenotypic features confirmed the respective diagnoses. The patient demographics and clinical features are detailed in Table 1.
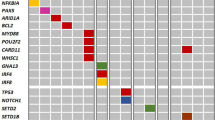
Using our analytic pipeline consisting of three different variant calling algorithms, Mutect, SNPPET, and VarScan, the observed somatic non-synonymous mutational burden per case was low with a mean of 4.6 mutations per case (range 2–13). To minimize false negatives, we employed more lenient filter parameters including a minimum of 10% allele frequency and a 10 read/ single-nucleotide variant coverage requirement. A total of 46 non-synonymous somatic mutations affecting 44 different genes were identified, including both missense mutations and nonsense mutations.3 In pediatric-type follicular lymphoma, we identified 32 single-nucleotide variants in genes involved in transcription, intracellular signaling, and cell proliferation (Table 2). Fewer mutations were detected in pediatric nodal marginal zone lymphoma, with 14 single-nucleotide variants observed in genes involved in cellular adhesion, cytokine regulatory elements, and cellular proliferation (Table 3).
In pediatric-type follicular lymphoma, we identified a recurrent somatic point mutation c.197A>G encoding p.Lys66Arg in the transcription factor interferon regulator factor 8/interferon consensus-binding protein (IRF8/ICSBP). This unique single-nucleotide variant was identified in three of six pediatric-type follicular lymphoma samples (Table 2). It was absent in the corresponding normal tissue sample from case 1. Sanger sequencing confirmed the single-nucleotide variant in all three cases. We further performed Sanger sequencing to detect the IRF8 variant on the remainder of the pediatric-type follicular lymphoma cases, all pediatric nodal marginal zone lymphoma cases and 22 cases of adult-type follicular lymphoma; these cases were negative for the c.197A>G in IRF8 (data not shown). No recurrent somatic mutations were observed in pediatric nodal marginal zone lymphoma.
IRF8 is a member of the IRF family of transcription factors, predominantly expressed in the cells of the immune system, which is a member of complex regulatory networks contributing to hematopoietic differentiation, cell cycle regulation, and apoptosis. The IRF8 protein contains an N-terminal DNA-binding domain and a C-terminal IRF association domain. The p.Lys66Arg alteration is a conservative, charge-neutral residue substitution within the DNA-binding domain of IRF8 (Figure 1a and b): specifically loop 2, which is C-terminal to alpha helix-2 (Figure 1b). Although falling within a long loop region, this position based on extrapolation from the highly homologous family member IRF4 and the crystal structure of PU.1/IRF4/DNA complex, is predicted to affect DNA–protein interaction via the bulkier side group substitution.22 Furthermore, assessment of amino-acid sequence conservation in IRF8 at position 66 revealed 100% sequence identity compared with 97 vertebrate species with aligned genomes (Figure 1c and Supplementary Table S2). In addition, PolyPhen2 and sorting intolerant from tolerant (SIFT) algorithms predict a deleterious effect of the p.Lys66Arg alteration.
Recurrent point mutation in the DNA-binding domain of IRF8. (a) Schematic diagram of the IRF8 protein with demarcation of the DNA-binding domain and IRF association domain. Stars indicate location and number of cases with K66R substitution. (b) Ribbon model of the DNA-binding domain with the side chain of R66 visualized. Inset, ribbon model with wild-type sequence. (c) Multi-species alignment of IRF8 spanning exon 1 and exon 2 (amino acids 1–87) with highlighted conserved lysine at position 66 across multiple species.
Copy-Number Variants and Fusion Detection
Copy-number and/or structural variations are frequently associated with hematolymphoid neoplasms. We evaluated the whole-exome paired-end data set for pediatric-type follicular lymphoma and pediatric nodal marginal zone lymphoma assessing for copy-number alterations and genomic fusion and break points. We employed CNV-seq to identify DNA copy-number variations using a threshold of twofold increase or decrease compared with control.23 As not all of the samples had paired normal tissue, all samples were compared with the paired histologically confirmed uninvolved lymph node (normal tissue) from case 1. With this analysis, no recurrent chromosomal site to suggest large genomic copy-number alterations was identified in pediatric-type follicular lymphoma or pediatric nodal marginal zone lymphoma.
For detection of genomic rearrangements, we used the previously described software tool Fusion and Chromosomal Translocation Enumeration and Recovery Algorithm.24 This highly sensitive and specific method uses paired-end DNA sequencing data to rapidly identify translocations, inversions, and large deletions. Three structural variations were identified in three separate cases of pediatric-type follicular lymphoma (Supplementary Table S3): two variants were deletions spanning the immunoglobulin kappa joining region and the variable region (case 4 and 6), and the third was a deletion present in the immunoglobulin heavy chain variable region (case 1). These deletions likely represented normal immunoglobulin heavy chain and immunoglobulin kappa gene rearrangements (Table 1). No gene fusions were identified in pediatric-type follicular lymphoma. No translocations, inversions, or deletions were identified in pediatric nodal marginal zone lymphoma.
Comparison with Variants in Adult-Type Follicular Lymphoma and Adult-Type Nodal Marginal Zone Lymphoma
Given the similar morphologic and phenotypic features of pediatric-type follicular lymphoma and pediatric nodal marginal zone lymphoma with the corresponding adult types, we sought to compare the identified single-nucleotide variants with published reports for alterations in adult-type follicular lymphoma and adult-type nodal marginal zone lymphoma. No mutations were observed in pediatric-type follicular lymphoma in chromatin regulatory elements (CREBBP, EZH2, KMT2D (MLL2), members of the TNF family (TNFRSF14), NF-kB signaling, or mTORC1;25, 26, 27, 28 however, case 2, which also harbored an IRF8 mutation, contained a mutation in the transcription factor PAX5, p.Gly183Ala. This mutation was not seen in the paired normal tissue; whereas this mutation in PAX5 has not been reported previously in adult-type follicular lymphoma, mutations in G183 have been identified in patients with B-lymphoblastic leukemia.21
Translocations involving BCL2 were not observed by exome sequencing or by fluorescence in situ hybridization studies (Supplementary Table S4). However, in pediatric nodal marginal zone lymphoma, we observed a single case with a non-synonymous mutation in Angiomotin like-1 (AMOTL1) c.2671G>A (p.Ala891Thr); this specific point mutation has been identified previously in a patient with carcinoma of the large intestine (COSMIC ID: COSM1357979). AMOTL1 is a coiled-coil, PDZ-binding and glutamine-rich domain containing protein that has recently been described as recurrently mutated in splenic marginal zone lymphoma.29 AMOTL1 mutations were not observed in pediatric-type follicular lymphoma cases. Moreover, no global copy-number alterations to support trisomies seen in adult-type nodal marginal zone lymphoma, such as trisomy 3 and 18 were seen; however, two of the cases (case 8 and 9) had detected B-cell clonal rearrangements. In keeping with the low incidence of translocations in adult-type nodal marginal zone lymphoma, none were observed in pediatric nodal marginal zone lymphoma. The reported 7q32 deletion and 8q23 gain seen in splenic marginal zone lymphoma were not identified. Mutations in additional genes known to be mutated in marginal zone lymphomas such as those in Kruppel-like factor 2 (KLF2), MYD88, TP53, CDKN2A, NOTCH1, NOTCH2, BRAF, TRAF3, TNFAIP3, CARD11, and others, which have been described in adult marginal zone lymphomas were not seen in pediatric nodal marginal zone lymphoma (Supplementary Table S4).27, 30, 31
Discussion
Pediatric-type follicular lymphoma and pediatric nodal marginal zone lymphoma are extremely rare diseases, which share features with their corresponding adult types, but show distinct differences in clinical behavior. The basis for these distinct differences is not well understood. Here we performed whole-exome deep sequencing on cases of pediatric-type follicular lymphoma and pediatric nodal marginal zone lymphoma to better characterize the genetic landscape of these diseases and identify driver mutations. Both diseases showed overall low somatic mutation rates (on average 4.6 mutations per exome); mutations identified in pediatric-type follicular lymphoma and pediatric nodal marginal zone lymphoma were seen in pathways important for transcription, intracellular signaling and cellular organization. Importantly, we identified a recurrent and specific somatic point mutation in IRF8 present in three cases of pediatric-type follicular lymphoma and absent in the normal tissue from a paired sample. This variant encodes a p.Lys66Arg, which falls within the DNA-binding domain of the protein and is predicted to result in deleterious effects. In addition, IRF8 p.Lys66Arg was not detected in pediatric nodal marginal zone lymphoma or cases of adult-type follicular lymphoma. To our knowledge, this is the first published report detailing the mutational landscape of these diseases and the first description of a potential driver mutation in pediatric-type follicular lymphoma.
In contrast to adult-type follicular lymphoma, which shows a characteristic BCL2 chromosomal translocation, as well as additional common chromosomal and gene changes, the genetic underpinnings of pediatric-type follicular lymphoma development have not been clearly defined.32 Martin–Guerrero et al, recently reported recurrent loss of heterozygosity at 1p36, a site commonly altered in adult-type follicular lymphoma, which was primarily associated with TNFRSF14 mutations.6 EZH2 mutations were also reported in the same cohort, lending some support to potential genetic mechanisms as the adult form.33 IRF8 was recently described as a recurrently mutated gene in a small percentage of cases of adult-type follicular lymphoma.34 Notably, the variants were predominantly located in the C-terminal domain of IRF8 with unclear functional consequences and a recurrent nucleotide change was not reported. Identification of the specific p.Lys66Arg substitution in a significant portion of our pediatric-type follicular lymphoma cohort is highly suggestive of a common and critical alteration, leading to the disease development. Moreover, although a similar gene is implicated between the adult and pediatric forms, the recurrent alteration in the DNA-binding domain suggests potentially a unique disease origin.
The interferon regulatory factor (IRF) superfamily of transcription factors consists of nine members with roles in transcriptional regulation of interferon (IFN)-inducible genes, as well as increasingly recognized roles in immune development and function. IRF8/ICSBP is induced by type II IFN and is expressed by hematopoietic cells, as well as other tissues. IRF8 serves a key role in T-cell and dendritic cell development, as well as differentiation and function of macrophages, T-cells and B cells.34, 35, 36, 37, 38 In B-cells, IRF8, with the highly homologous protein IRF4, functions in pre-B cells to regulate light-chain rearrangement and is required for differentiation from pre-B-cells to immature B-cells.37, 39 IRF8 and IRF4 induce expression of the transcription factors ikaros and aiolos, which serve as negative regulators of pre-B-cell receptor signaling and cell cycle progression through direct c-Myc inhibition.40 Notably, deficiency of IRF4 and IRF8 induces a hyperpoliferative phenotype in pre-B cells, though reconstitution of either IRF4 or IRF8 rescues the normal phenotype.39, 40 Consistent with these roles in immune maturation and regulation, alterations in IRF8, as well as IRF4, have been implicated in B-cell malignancies, largely in adults, including follicular lymphoma, diffuse large B-cell lymphoma, and chronic lymphocytic leukemia.33 This study adds to the complexity and importance of IRF8 in B-cells and B-cell-related neoplasms.
Interactions between IRF8 and IRF4 have recently been described to have a co-regulatory role in Epstein–Barr virus infection.41 IRF8 and IRF4 directly interact with the N-terminal domain of the Epstein–Barr virus-encoded Epstein–Barr virus-associated nuclear antigen 3C forming a molecular complex, which stabilizes IRF4 and leads to proteasome-dependent degradation of IRF8. Notably, an inverse relationship between IRF8 expression and apoptosis resistance via Fas-mediated pathway has been described to correlate with enhanced apoptosis resistance and metastatic potential in vitro.42 Given the association of EBV infection and altered IRF8 activity with development and transformation of several lymphoproliferative disorders, it is intriguing to speculate that IRF8 is the critical link in lymphomagenesis of many hematopoietic disorders.
We additionally identified a mutation in the transcription factor PAX5/BSAP, p.Gly183Ala. This amino acid, G183, has been identified as an important residue mutated in cases of B-lymphoblastic leukemia. On the basis of functional studies, mutations at G183 affect the transcriptional activity of PAX5 and alter susceptibility to neoplasia.21 It is therefore not surprising that this mutation may additionally affect the progression and genesis of pediatric-type follicular lymphoma. This mutation was not present in the matched normal tissue, nor was it seen in the other cases of pediatric-type follicular lymphoma or pediatric nodal marginal zone lymphoma.
Similar to pediatric-type follicular lymphoma, the genetic underpinnings of pediatric nodal marginal zone lymphoma are not well understood. Rizzo et al reported 21% of cases of pediatric nodal marginal zone lymphomas contained genetic alterations detected by fluorescence in situ hybridization and reverse transcription PCR.11 The leading abnormality was trisomy 18 (17%), which has been described in adult-type nodal marginal zone lymphoma.10 Our cohort showed no evidence of copy-number alterations to support trisomy. However, we identified a somatic variant in AMOTL1 in a case of pediatric nodal marginal zone lymphoma, which has also been implicated in the pathogenesis of splenic marginal zone lymphoma.29 This finding suggests that although pediatric nodal marginal zone lymphoma and adult-type nodal marginal zone lymphoma may share some common genetic abnormalities, our cohort is genetically distinct from adult-type nodal marginal zone lymphoma.
Unlike our pediatric-type follicular lymphoma cohort, a recurrent somatic mutation in our pediatric nodal marginal zone lymphoma cases was not identified by whole-exome sequencing. As the mutational burden was relatively lower in pediatric nodal marginal zone lymphoma than in pediatric-type follicular lymphoma (3.25 mutations per case versus 4.8 mutations per case), this might suggest that this disease may lack a common and specific driver. However, recent studies have suggested that somatic mutations in non-coding regions may harbor potential driver mutations and even synonymous alterations of protein coding genes may have functional roles in tumor development.43, 44, 45 Moreover, it has been recently shown that modification of the epigenetic landscape in adult-type follicular lymphoma through mutations in the methyltransferase KMT2D (MLL2) is prolymphomagenic; the possibility that non-coding DNA mutations or epigenetic alterations may drive pediatric nodal marginal zone lymphoma warrants further study.46
Overall, this is the first description of a broad somatic mutational landscape of pediatric-type follicular lymphoma and pediatric nodal marginal zone lymphoma. The data support a different mechanism of development compared with the corresponding adult-type disease, as the typical mutational landscape found in adult-type nodal marginal zone lymphoma and adult-type follicular lymphoma was not present. Moreover, a single recurrent point mutation in IRF8 was identified in a subset of pediatric-type follicular lymphoma cases, which was predicted to produce a deleterious effect. Given the functional role of IRF8 in B cells and transcription, it is intriguing to speculate that this mutation may serve as a driver-promoting disease development.
References
O'Suoji C, Welch JJ, Perkins SL et al. Rare pediatric non-hodgkin lymphomas: A report from children's oncology group study ANHL 04B1. Pediatr Blood Cancer 2016;63:794–800.
Quintanilla-Martinez L, Sander B, Chan JK et al. Indolent lymphomas in the pediatric population: Follicular lymphoma, IRF4/MUM1+ lymphoma, nodal marginal zone lymphoma and chronic lymphocytic leukemia. Virchows Arch 2016;468:141–157.
Swerdlow SH, Campo E, Pileri SA et al. The 2016 revision of the world health organization (WHO) classification of lymphoid neoplasms. Blood 2016;127:2375–2390.
Lorsbach RB, Shay-Seymore D, Moore J et al. Clinicopathologic analysis of follicular lymphoma occurring in children. Blood 2002;99:1959–1964.
Ribeiro RC, Pui CH, Murphy SB et al. Childhood malignant non-hodgkin lymphomas of uncommon histology. Leukemia 1992;6:761–765.
Martin-Guerrero I, Salaverria I, Burkhardt B et al. Recurrent loss of heterozygosity in 1p36 associated with TNFRSF14 mutations in IRF4 translocation negative pediatric follicular lymphomas. Haematologica 2013;98:1237–1241.
Taddesse-Heath L, Pittaluga S, Sorbara L et al. Marginal zone B-cell lymphoma in children and young adults. Am J Surg Pathol 2003;27:522–531.
Swerdlow SH, Campo E, Harris NL et al (eds). WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, 4th edn. International Agency for Research on Cancer: Lyon, France, 2008.
Harris NL, Swerdlow SH, Jaffe ES . Follicular lymphoma. In: Swerdlow SH, Campo E, Harris NL et al (eds). World Health Organization Classification of Tumours, 4th edn. International Agency for Research on Cancer: Lyon, France, 2008, pp 220.
Dierlamm J, Pittaluga S, Wlodarska I et al. Marginal zone B-cell lymphomas of different sites share similar cytogenetic and morphologic features. Blood 1996;87:299–307.
Rizzo KA, Streubel B, Pittaluga S et al. Marginal zone lymphomas in children and the young adult population; characterization of genetic aberrations by FISH and RT-PCR. Mod Pathol 2010;23:866–873.
Karnik T, Ozawa MG, Lefterova M et al. The utility of IgM, CD21, HGAL and LMO2 in the diagnosis of pediatric follicular lymphoma. Hum Pathol 2015;46:629–633.
Palomero T, Couronne L, Khiabanian H et al. Recurrent mutations in epigenetic regulators, RHOA and FYN kinase in peripheral T cell lymphomas. Nat Genet 2014;46:166–170.
Pasqualucci L, Khiabanian H, Fangazio M et al. Genetics of follicular lymphoma transformation. Cell Rep 2014;6:130–140.
Cibulskis K, Lawrence MS, Carter SL et al. Sensitive detection of somatic point mutations in impure and heterogeneous cancer samples. Nat Biotechnol 2013;31:213–219.
Ungewickell A, Bhaduri A, Rios E et al. Genomic analysis of mycosis fungoides and sezary syndrome identifies recurrent alterations in TNFR2. Nat Genet 2015;47:1056–1060.
Ohgami RS, Ma L, Merker JD et al. Next-generation sequencing of acute myeloid leukemia identifies the significance of TP53, U2AF1, ASXL1, and TET2 mutations. Mod Pathol 2015;28:706–714.
Biasini M, Bienert S, Waterhouse A et al. SWISS-MODEL: Modelling protein tertiary and quaternary structure using evolutionary information. Nucleic Acids Res 2014;42:W252–W258.
Adzhubei IA, Schmidt S, Peshkin L et al. A method and server for predicting damaging missense mutations. Nat Methods 2010;7:248–249.
Kumar P, Henikoff S, Ng PC . Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat Protoc 2009;4:1073–1081.
Shah S, Schrader KA, Waanders E et al. A recurrent germline PAX5 mutation confers susceptibility to pre-B cell acute lymphoblastic leukemia. Nat Genet 2013;45:1226–1231.
Escalante CR, Brass AL, Pongubala JM et al. Crystal structure of PU.1/IRF-4/DNA ternary complex. Mol Cell 2002;10:1097–1105.
Xie C, Tammi MT . CNV-seq, a new method to detect copy number variation using high-throughput sequencing. BMC Bioinformatics 2009;10:2105–10-80.
Newman AM, Bratman SV, Stehr H et al. FACTERA: A practical method for the discovery of genomic rearrangements at breakpoint resolution. Bioinformatics 2014;30:3390–3393.
Okosun J, Bodor C, Wang J et al. Integrated genomic analysis identifies recurrent mutations and evolution patterns driving the initiation and progression of follicular lymphoma. Nat Genet 2014;46:176–181.
Okosun J, Wolfson RL, Wang J et al. Recurrent mTORC1-activating RRAGC mutations in follicular lymphoma. Nat Genet 2016;48:183–188.
Kridel R, Sehn LH, Gascoyne RD . Pathogenesis of follicular lymphoma. J Clin Invest 2012;122:3424–3431.
Loeffler M, Kreuz M, Haake A et al. HaematoSys-Project. Genomic and epigenomic co-evolution in follicular lymphomas. Leukemia 2015;29:456–463.
Parry M, Rose-Zerilli MJ, Gibson J et al. Whole exome sequencing identifies novel recurrently mutated genes in patients with splenic marginal zone lymphoma. PLoS ONE 2013;8:e83244.
Clipson A, Wang M, de Leval L et al. KLF2 mutation is the most frequent somatic change in splenic marginal zone lymphoma and identifies a subset with distinct genotype. Leukemia 2015;29:1177–1185.
Martinez N, Almaraz C, Vaque JP et al. Whole-exome sequencing in splenic marginal zone lymphoma reveals mutations in genes involved in marginal zone differentiation. Leukemia 2014;28:1334–1340.
Morin RD, Johnson NA, Severson TM et al. Somatic mutations altering EZH2 (Tyr641) in follicular and diffuse large B-cell lymphomas of germinal-center origin. Nat Genet 2010;42:181–185.
Li H, Kaminski MS, Li Y et al. Mutations in linker histone genes HIST1H1 B, C, D, and E; OCT2 (POU2F2); IRF8; and ARID1A underlying the pathogenesis of follicular lymphoma. Blood 2014;123:1487–1498.
Becker AM, Michael DG, Satpathy AT et al. IRF-8 extinguishes neutrophil production and promotes dendritic cell lineage commitment in both myeloid and lymphoid mouse progenitors. Blood 2012;119:2003–2012.
Ouyang X, Zhang R, Yang J et al. Transcription factor IRF8 directs a silencing programme for TH17 cell differentiation. Nat Commun 2011;2:314.
Xu H, Zhu J, Smith S et al. Notch-RBP-J signaling regulates the transcription factor IRF8 to promote inflammatory macrophage polarization. Nat Immunol 2012;13:642–650.
Ma S, Pathak S, Trinh L et al. Interferon regulatory factors 4 and 8 induce the expression of ikaros and aiolos to down-regulate pre-B-cell receptor and promote cell-cycle withdrawal in pre-B-cell development. Blood 2008;111:1396–1403.
Xu H, Chaudhri VK, Wu Z et al. Regulation of bifurcating B cell trajectories by mutual antagonism between transcription factors IRF4 and IRF8. Nat Immunol 2015;16:1274–1281.
Ma S, Turetsky A, Trinh L et al. IFN regulatory factor 4 and 8 promote ig light chain kappa locus activation in pre-B cell development. J Immunol 2006;177:7898–7904.
Ma S, Pathak S, Mandal M et al. Ikaros and aiolos inhibit pre-B-cell proliferation by directly suppressing c-myc expression. Mol Cell Biol 2010;30:4149–4158.
Banerjee S, Lu J, Cai Q et al. The EBV latent antigen 3C inhibits apoptosis through targeted regulation of interferon regulatory factors 4 and 8. PLoS Pathog 2013;9:e1003314.
Yang D, Thangaraju M, Greeneltch K et al. Repression of IFN regulatory factor 8 by DNA methylation is a molecular determinant of apoptotic resistance and metastatic phenotype in metastatic tumor cells. Cancer Res 2007;67:3301–3309.
Weinhold N, Jacobsen A, Schultz N et al. Genome-wide analysis of noncoding regulatory mutations in cancer. Nat Genet 2014;46:1160–1165.
Fredriksson NJ, Ny L, Nilsson JA et al. Systematic analysis of noncoding somatic mutations and gene expression alterations across 14 tumor types. Nat Genet 2014;46:1258–1263.
Supek F, Minana B, Valcarcel J et al. Synonymous mutations frequently act as driver mutations in human cancers. Cell 2014;156:1324–1335.
Zhang J, Dominguez-Sola D, Hussein S et al. Disruption of KMT2D perturbs germinal center B cell development and promotes lymphomagenesis. Nat Med 2015;21:1190–1198.
Acknowledgements
This work was supported through research funding to Ohgami RS through the Stanford Department of Pathology. We additionally thank Galli S, Lefterova M, Gojenola L, Chui W, West J and Chen R for their support.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Modern Pathology website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Ozawa, M., Bhaduri, A., Chisholm, K. et al. A study of the mutational landscape of pediatric-type follicular lymphoma and pediatric nodal marginal zone lymphoma. Mod Pathol 29, 1212–1220 (2016). https://doi.org/10.1038/modpathol.2016.102
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2016.102
This article is cited by
-
Comparison of histological and molecular features of pediatric-type follicular lymphoma and pediatric nodal marginal zone lymphoma
Virchows Archiv (2023)
-
Follicular lymphoma and marginal zone lymphoma: how many diseases?
Virchows Archiv (2023)
-
Novel markers in pediatric-type follicular lymphoma
Virchows Archiv (2019)