Abstract
IgG4-related disease is a recently recognized systemic syndrome characterized by mass-forming lesions with lymphoplasmacytic infiltration, increase in the number of IgG4+ cells in affected tissues and elevation of serum IgG4 levels. In 2009, we were the first to report skin lesions in patients with IgG4-related disease, but no large case series has been reported and clinicopathological findings remain unclear. To clarify these features, we herein report 10 patients (9 men and 1 woman; median age, 64 years; age range, 46–81 years) with IgG4-related skin disease. All patients had erythematous and itchy plaques or subcutaneous nodules on the skin of the head and neck, particularly in the periauricular, cheek, and mandible regions, except for one patient, whose forearm and waist skin were affected. In addition, eight patients had extracutaneous lesions: these were found on the lymph nodes in six patients, the lacrimal glands in three patients, the parotid glands in three patients, and the kidney in one patient. Histologically examined extracutaneous lesions were consistent with IgG4-related disease; five of six lymph node lesions showed progressively transformed germinal centers-type IgG4-related lymphadenopathy. Cases of IgG4-related skin disease were classified into two histological patterns: those exhibiting a nodular dermatitis pattern and those with a subcutaneous nodule pattern. The infiltrate was rich in plasma cells, small lymphocytes, and eosinophils; the majority of the plasma cells were IgG4+. The IgG4+ cell count was 49–396 per high-power field (mean±s.d., 172±129), with an IgG4+/IgG+ cell ratio ranging from 62 to 92%. Serum IgG4 levels were elevated in all examined patients. In conclusion, patients with IgG4-related skin disease had uniform clinicopathology. Lesions were frequently present on the skin of the periauricular, cheek, and mandible regions, and were frequently accompanied by IgG4-related lymphadenopathy.
Similar content being viewed by others
Main
IgG4-related disease is a recently recognized syndrome characterized by mass-forming lesions with lymphoplasmacytic infiltration, an increased number of IgG4+ cells in the affected tissues, and elevated serum IgG4 levels. It is usually found in middle-aged and older patients, with men predominantly affected, and normally has a favorable clinical response to steroid therapy.1, 2, 3, 4
IgG4-related disease can affect multiple organs, including the pancreas, hepatobiliary tract, lacrimal glands, salivary glands, lungs, kidneys, retroperitoneum, prostate, aorta, and lymph nodes. In most patients with this disease, two or more sites in various combinations are involved.2, 3, 4
In 2009, we first reported skin lesions in patients with IgG4-related disease.5 However, no large case series has been reported so far, and the clinicopathological findings remain unclear.6, 7 Herein, we report the clinicopathological findings in 10 Japanese patients with IgG4-related skin disease.
Materials and methods
Case Selection
All patients with IgG4-related skin disease were diagnosed on the basis of their clinical and pathological features recorded by the Department of Pathology, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Okayama, Japan.
The clinical records and pathology materials for all cases were reviewed, and cases of multicentric Castleman’s disease, malignant lymphoma, and other lymphoproliferative disorders (including rheumatoid arthritis and other immune-mediate conditions) were histologically and clinically excluded from this study.
Histological Examination and Immunohistochemistry
Surgical biopsy specimens were fixed in 10% formaldehyde and embedded in paraffin. Serial sections (4 μm) were cut from each paraffin-embedded tissue block, and several sections were stained with hematoxylin and eosin (H&E) and Elastica-van Gieson. Immunohistochemistry was performed on paraffin sections using an automated Bond Max stainer (Leica Biosystems, Melbourne, Australia). The primary antibodies used were as follows: CD20 (L26 (1:400); Dako), CD3 (LN10 (1:200); Novocastra), CD10 (56C6 (1:100); Novocastra), bcl-2 (3.1 (1:400); Novocastra), IgG (polyclonal (1:10 000); Dako), IgG4 (HP6025 (1:400); The Binding Site), Kappa (NCL-KAP (1:100); Novocastra), and Lambda (NCL-LAM (1:200); Novocastra). The number of IgG4+ or IgG+ cells was estimated for areas with the highest density of positive cells. Three different high-power fields (HPFs; × 10 eyepiece and × 40 objective lenses) in each section were counted, and the average number of positive cells per HPF was calculated;3 eosinophil numbers were also counted.
Unless specified otherwise, all data are represented as the mean±s.d.
In Situ Hybridization
In situ hybridization of κ- and λ-chains was performed by an automated Bond Max stainer (Leica Biosystems).
Results
Clinical Features
The subjects included in this study were nine men and one woman, with a median age of 64 years (age range, 46–81 years) (Table 1). Patients had erythematous and itchy plaques or subcutaneous nodules on the skin of the face, head, and neck, particularly in the periauricular, cheek, and mandible regions, with the exception of one patient in whom the skin of the forearm and waist region were affected (Figure 1). In addition, 8 of 10 patients had extracutaneous lesions; these were found on the lymph nodes in 6 patients (60%), the lacrimal glands in 3 patients (30%), the parotid glands in 3 patients (30%), and the kidney in 1 patient (10%). Histologically examined extracutaneous lesions were consistent with IgG4-related disease. Interestingly, the histological results for five of six lymph node lesions demonstrated progressively transformed germinal centers-type IgG4-related lymphadenopathy, and three patients progressed to systemic IgG4-related lymphadenopathy (Tables 1 and 2).
All eight patients in whom serum IgG4 levels were measured had elevated IgG4 levels (652±543 mg/dl); the serum IgG4/IgG ratios ranged from 14 to 54% (29.5±15.2). Serum IgE levels were elevated in seven of the seven patients in whom serum IgE levels were measured, and peripheral blood eosinophil counts were increased in six of eight patients in whom the eosinophil counts were measured.
Six patients were treated with systemic steroid therapy, which decreased the size of various lesions. However, the lesions increased in size when steroid administration was tapered in five patients.
Pathological Features
Cases of IgG4-related skin disease were classified into two histological patterns: those exhibiting a nodular dermatitis pattern and those with a subcutaneous nodule pattern (Table 2).
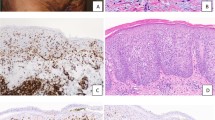
Patients 1–7 exhibited a nodular dermatitis pattern. Their skin lesions showed dermal involvement by perivascular and periadnexal lymphoplasmacytic nodular infiltration, with or without lymphoid follicles. Patients 5–7 demonstrated subcutaneous involvement by perivascular lymphoplasmacytic nodular infiltration. Patients 6 and 7 had fibrosis without a storiform pattern (Figures 2, 3, 4).
Patients 8–10 demonstrated a subcutaneous nodule pattern. Their skin lesions exhibited predominantly subcutaneous lymphoplasmacytic nodular infiltration with lymphoid follicles, and patients 9 and 10 had fibrosis without a storiform pattern (Figure 5).
Obliterative phlebitis was detected in only one patient (Patient 3, Figure 4).
The inflammatory cells were rich in mature and immature plasma cells and small lymphocytes, with varied numbers of eosinophils; the eosinophil counts were 1.3–289/HPF.
On immunohistological examination, the lymphoid infiltrates were a mixed population of CD20+ B cells in nodular aggregates and CD3+ T cells. The germinal centers were CD10+ and Bcl-2−. Light-chain restriction by in situ hybridization was not detected in any of the cases. Although the majority of the plasma cells were IgG4+, the number of IgG4+ cells varied. The IgG4+ cell count was 49–396 cells/HPF (183±121), with an IgG4+/IgG+ cell ratio of 62–92%.
Seven of eight patients with extracutaneous lesions were histologically examined, and the findings were consistent with IgG4-related disease (Table 2). Five of six lymph node lesions demonstrated progressively transformed germinal centers-type IgG4-related lymphadenopathy (Figure 6).
Patient 7: Submandibular lymph node lesion demonstrating progressively transformed germinal centers-type IgG4-related lymphadenopathy. The progressively transformed germinal centers is characterized by scattered large expansile follicles with unusual appearance against a background of normal reactive follicles (arrowhead). (Left) H&E, (right) IgG4 immunostaining.
Discussion
IgG4-related disease frequently involves various organs, such as the lacrimal glands, salivary glands, lymph nodes, lungs, mediastinum, pancreas, hepatobiliary tract, retroperitoneum, aorta, kidneys, and prostate. The general condition of patients at presentation is usually good, with no fever or constitutional symptoms. Common laboratory findings include increased serum IgG4 and IgE levels, although lactate dehydrogenase levels remain unchanged. Patients often have an excellent response to steroid therapy.1, 2, 3, 4
In this report, we have described the clinicopathological details of patients with IgG4-related skin disease. The patients presented with uniform clinicopathology: the lesions frequently involved the skin of the periauricular, cheek, and mandible regions. Interestingly, half of the patients had submandibular progressively transformed germinal centers-type IgG4-related lymphadenopathy, which was recently recognized as a new type of IgG4-related disease.8 This type of IgG4-related lymphadenopathy frequently involves the submandibular lymph nodes, and is accompanied by extranodal lesions, particularly in the lacrimal and salivary glands.8 Interestingly, 6 of 10 patients in this study with IgG4-related skin disease had lacrimal or parotid gland lesions.
The histological features of IgG4-related skin disease are rather nonspecific, being indistinguishable from primary cutaneous lymphoid hyperplasia and other reactive processes. Nonetheless, this diagnosis may have to be considered, particularly for lesions rich in plasma cells and eosinophils, and especially if accompanying mass lesions are observed in sites commonly involved in IgG4-related disease, such as the lacrimal and salivary glands, and lymph nodes. In addition, the presence of large numbers of IgG4+ cells together with a high proportion of IgG4+/IgG+ cells provides a conclusive diagnosis.3
The 2012 Consensus Statement on the pathology of IgG4-related disease emphasizes that the characteristic histopathological appearance of dense lymphoplasmacytic infiltrates, a storiform pattern of fibrosis, and obliterative phlebitis are the most critical factors in diagnosis.3 However, although 4 of our 10 cases exhibited fibrosis, it was not storiform pattern fibrosis. In addition, obliterative phlebitis was detected in only one patient. The number of IgG4+ cells and the IgG4+/IgG+ cell ratio (>40%) were considered to be of secondary importance. The IgG4+ cell counts required for diagnosis differ among the affected organs, ranging from 10 to 200 cells/HPF.3 According to the Consensus Statement, 200 IgG4+ cells/HPF are required for the diagnosis of IgG4-related skin disease.3 In our case series, the IgG4+ cell count ranged from 49 to 396 cells/HPF (183±121). Thus, 7 of 10 cases with IgG4-related skin disease did not meet this diagnostic criteria. However, these criteria were on the basis of a limited number of published studies on IgG4-related skin disease.3 Therefore, the cutoff point for the IgG4+ cell count used to diagnose IgG4-related skin disease needs to be reconsidered. In fact, in a recently published case report of IgG4-related skin disease, the IgG4+ cell count was 47 cells/HPF.7
In our cases of IgG4-related skin disease and previously published studies,6, 7 IgG4+ cell counts were 47 to 425/HPF, and the IgG4+/IgG+ cell ratio was 62 to 100%. On the basis of these results, we propose the following histological diagnostic criteria for IgG4-related skin disease: IgG4+ cell count of >50/HPF and an IgG4+/IgG+ cell ratio of >60%. Needless to say, attaining the IgG4 immunostain threshold does not necessarily imply a diagnosis of IgG4-related disease. For the diagnosis of IgG4-related disease, careful correlation with the histopathological features of the sample and clinical findings is required.3
Hyper-IL-6 syndromes, such as multicentric Castleman’s disease, rheumatoid arthritis, and immune-mediated conditions, sometimes fulfill the diagnostic criteria for IgG4-related disease.9, 10 Recently, we encountered a case of cutaneous involvement of multicentric Castleman’s disease that fulfilled the diagnostic criteria for IgG4-related disease.11 Therefore, it is important to differentiate between IgG4-related skin disease and cutaneous involvement of multicentric Castleman’s disease. In our cases, hyper-IL-6 syndromes were histologically and clinically excluded. These were differentiated by the fact that hyper-IL-6 syndromes are characterized by elevated serum levels of IgG, IgA, IgM, and C-reactive protein; thrombocytosis; anemia, hypoalbuminemia; and hypocholesterolemia. In contrast, IgG4-related disease does not have any of these characteristics.3, 5, 9, 10
In conclusion, patients with IgG4-related skin disease had uniform clinicopathology, with lesions frequently found on the skin of the face, head, and neck, particularly the periauricular, cheek, and mandible regions; these were frequently accompanied by progressively transformed germinal centers-type IgG4-related lymphadenopathy.
References
Sato Y, Ohshima K, Ichimura K et al Ocular adnexal IgG4-related disease has uniform clinicopathology. Pathol Int 2008;58:465–470.
Sato Y, Notohara K, Kojima M et al IgG4-related diseases: historical overview and pathology of hematological disorders. Pathol Int 2010;60:247–258.
Deshpande V, Zen Y, Chan JK et al Consensus statement on the pathology of IgG4-related disease. Mod Pathol 2012;25:1181–1192.
Stone JH, Khosroshahi A, Deshpande V et al Recommendations for the nomenclature of IgG4-related disease and its individual organ system manifestations. Arthritis Rheum 2012;64:3061–3067.
Sato Y, Kojima M, Takata K et al Systemic IgG4-related lymphadenopathy: a clinical and pathologic comparison to multicentric Castleman’s disease. Mod Pathol 2009;22:589–599.
Cheuk W, Lee KC, Chong LY et al IgG4-related sclerosing disease. A potential new etiology of cutaneous pseudolymphoma. Am J Surg Pathol 2009;33:1713–1719.
Kakuchi Y, Yamada K, Suzuki Y et al IgG4-related skin lesions in a patient with IgG4-related chronic sclerosing dacryoadenitis and sialoadenitis. Intern Med 2011;50:1465–1469.
Sato Y, Inoue D, Asano N et al Association between IgG4-related disease and progressively transformed germinal centers of lymph node. Mod Pathol 2012;25:956–967.
Sato Y, Yoshino T . IgG4-related lymphadenopathy. Int J Rheumatol 2012;2012:572–539.
Asano N, Sato Y . Rheumatoid lymphadenopathy with abundant IgG4+ plasma cells: a case of mimicking IgG4-related disease. J Clin Exp Hematopathol 2012;52:57–61.
Takeuchi M, Sato Y, Takata K et al Cutaneous multicentric castleman’s disease mimicking IgG4-related disease. Pathol Res Pract 2012, doi:10.1016/j.prp.2012.09.006 (in press).
Acknowledgements
This work was supported by a Grant-in-Aid for Scientific Research (C) (no. 24591447) from the Japan Society for the Promotion of Science and ‘Research on Measures for Intractable Disease’ Project: matching fund subsidy from Ministry of Health Labour and Welfare, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sato, Y., Takeuchi, M., Takata, K. et al. Clinicopathologic analysis of IgG4-related skin disease. Mod Pathol 26, 523–532 (2013). https://doi.org/10.1038/modpathol.2012.196
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2012.196
Keywords
This article is cited by
-
IgG4-Related Disease: A Retrospective Chinese Study of Features and Treatment Response of 98 Patients Including 4 Rare Cases
Current Medical Science (2021)
-
Imaging findings of primary immunoglobulin G4-related cervical lymphadenopathy
Neuroradiology (2017)
-
A subset of ocular adnexal marginal zone lymphomas may arise in association with IgG4-related disease
Scientific Reports (2015)
-
Dermatologic Disorders in 118 Patients with Autoimmune (Immunoglobulin G4-Related) Pancreatitis: A Retrospective Cohort Analysis
American Journal of Clinical Dermatology (2015)
-
IgG4- related disease: an orphan disease with many faces
Orphanet Journal of Rare Diseases (2014)