Abstract
About 10% of epithelioid sarcomas have biallelic mutation of the SMARCB1 (SWI/SNF-related, matrix-associated, actin-dependent regulator of chromatin, subfamily b, member 1) gene resulting in a lack of this nuclear protein. It has been suggested that SMARCB1 may be silenced by epigenetic changes in the remaining 90% of tumors. Thus, we hypothesized that the promoter of SMARCB1 is hypermethylated. We also examined SMARCB1 mRNA level to determine if a post-translational change was possible. Thirty-six cases of epithelioid sarcomas were studied. Immunohistochemistry and mutation analysis of the SMARCB1 gene were performed to select appropriate cases. Methylation status was assessed by methylation-specific PCR. Laser capture microdissection of tumor cells followed by real-time PCR was applied to examine the expression of SMARCB1 mRNA. Of 36 epithelioid sarcomas, 31 (86%) displayed a lack of SMARCB1 nuclear protein. In all, 4 (13%) of 31 SMARCB1-negative cases harbored biallelic deletion while 9 (33%) cases showed single-allelic deletion. One (4%) frameshift deletion of exon 3 and one point mutation of exon 7 were also found. In 16 (59%) cases, both alleles were intact. Altogether, 25/31 (81%) SMARCB1-negative cases had at least one intact allele. None of these cases demonstrated promoter hypermethylation. Low levels of SMARCB1 mRNA were found in all cases with tumor tissue extracted RNA (because of the minimal normal cell contamination) but no mRNA could be detected in laser dissected cases (containing only tumor cells). Enhancer of zeste homolog 2 (EZH2) overexpression was not characteristic of epithelioid sarcoma. Thus, loss of SMARCB1 expression in epithelioid sarcoma is caused neither by DNA hypermethylation nor by post-translational modifications. Most likely it is the microRNA destruction of SMARCB1 mRNA but further investigations are needed to elucidate this issue.
Similar content being viewed by others
Main
The SMARCB1 (SWI/SNF-related, matrix-associated, actin-dependent regulator of chromatin, subfamily b, member 1; also known as INI1, BAF47 and hSNF5) gene, located on chromosomal position 22q11.23, encodes a core subunit of the SWI/SNF ATP-dependent chromatin remodeling complex.1 Such observations show these complexes regulate gene expression, at least in part, by inducing a nucleosome conformation that is more approachable to the transcriptional machinery.2 Recently, inactivation of both alleles of the SMARCB1 gene was identified in the majority of malignant rhabdoid tumors, suggesting that loss-of-function mutations of the gene contributed to the oncogenesis of this type of tumor.3 SMARCB1 abnormalities also have been found in other malignant neoplasms including epithelioid sarcoma, epithelioid malignant peripheral nerve sheath tumor, myoepithelial carcinoma, extraskeletal myxoid chondrosarcoma and renal medullary carcinoma.4
Epithelioid sarcoma, described by Enzinger,5 is a rare and distinctive soft tissue neoplasm typically arising in the distal extremities of young adults.6 Many studies reported the absence of nuclear staining of SMARCB1 in approximately 90% of tumors.7, 8, 9, 10 Recent studies of molecular analysis of the SMARCB1 gene revealed only 10% of epithelioid sarcoma cases had both absent SMARCB1 expression and mutation of SMARCB1 that suppress expression. In cases without DNA alterations, either epigenetic changes or post-transcriptional modification could prevent expression of SMARCB1.10 In addition to point mutations and deletions, transcriptional repression by hypermethylation of promoter sequences is an alternative mechanism of inactivation of tumor-suppressor genes in cancer.11, 12 Further mechanisms of epigenetic silencing of gene expression include post-translational modification of histones. The trimethylation of histone-3 on lysine-27 (H3K27me3) is a well-known histone mark associated with gene silencing. H3K27me3 is mediated by the methyltransferase enhancer of zeste homolog 2 (EZH2), which is the enzymatically active component of the polycomb repressor complex 2 (PRC2).13 EZH2 is abnormally overexpressed in a wide range of tumors as compared with corresponding normal tissues, its level of expression being correlated with cancer aggressiveness.14, 15, 16 Recently, studies have shown that EZH2 aberrations are strongly associated with many mesenchymal tumors (synovial sarcoma, Ewing sarcoma and alveolar rhabdomyosarcoma).17 In our study, we carried out an epigenetic investigation to detect the methylation profile in SMARCB1 promoter areas of 25 epithelioid sarcoma cases. Immunohistochemical studies were also carried out to detect the EZH2 protein expression of 36 epithelioid sarcomas.
Materials and methods
Tissue Samples
For this retrospective study, formalin-fixed, paraffin-embedded tumor samples were collected from 36 patients diagnosed with epithelioid sarcoma (World Health Organization classification) from the archives of the Semmelweis University First Department of Pathology (n=17); National Institute of Oncology, Hungary (n=6); the University of Chicago Medical Center (n=9); Department of Laboratory Medicine and Pathology, Mayo Clinic (n=3) and from Scott and White Healthcare Temple Clinic, Texas (n=1). Beside H&E slides, immunohistochemistry was performed for cytokeratin (AE1/AE3), EMA, vimentin, CD34, S100 and SMARCB1 to confirm the diagnosis of epithelioid sarcoma. Main clinical data are summarized in Table 1. The possibility of malignant rhabdoid tumor was excluded by fluorescence in situ hybridization (FISH) and direct sequencing, described later.
Immunohistochemistry
Immunohistochemical staining was performed with Bond Max™ Autostainer (Leica Biosystems Newcastle, Newcastle, UK). Tissue sections of 3 μm thickness were cut from the blocks, after deparaffinization in xylene and retrieval using either the Bond Epitope Retrieval Solution 1 (pH∼6) or the Bond Epitope Retrieval Solution 2 (pH∼9) (Leica Microsystems, Wetzlar, Germany) at 99–100 °C for 20–30 min, were immunostained using a purified mouse anti-BAF47 (SMARCB1) antibody (clone 25; 1:50; BD Transduction Laboratories, San Diego, CA, USA), monoclonal mouse anti-human cytokeratin (clones AE1/AE3; 1:150; Dako Cytomation, Carpinteria, CA, USA), monoclonal mouse anti-human epithelial membrane antigen (clone E29; 1:200; Dako), monoclonal mouse anti-human vimentin, (clone V9; 1:600; Dako), monoclonal mouse anti-human CD34 class II (clone QBEnd 10; 1:300; Dako), polyclonal rabbit anti-S100 (1:1500; Dako) and purified mouse anti-EZH2 antibody (clone 11, 1:25, BD Biosciences, USA). Sections were incubated with the primary antibody for 25 min, followed by using the peroxidase/DAB Bond Polymer Refine Detection System (Leica Microsystems) for visualization.
For SMARCB1, the tumors were scored as having nuclear expression intact or absent. To assess the immunohistochemical labeling of EZH2, we modified the scoring system described by Pacheo et al.18 The intensity of the nuclear staining was evaluated as follow: score 0: no visible staining; score 1: weak; score 2: moderate; score 3: intense. To evaluate the extension of the positive cells was based on the percentage of the cell with positive nuclear stain against the background (score 0: no visible staining; score 1: 1–50%; score 2: 51–75%; score 3: above 75%). Each score contained at least 100 tumor cells to be evaluated. If >30% of the tumor cells carried stronger nuclear intensity, we used the higher nuclear score. The sum of these two scores defined the final score of each sample; if it is above 3, the case was considered as EZH2 positive.
Fluorescence In Situ Hybridization
FISH analysis was carried out on all SMARCB1-negative tumors. In all, 4.5 μl of BCR/ABL Dual Color Translocation Probe Set, consisting of BCR- (SpectrumGreen-labeled, green) and ABL- (SpectrumOrange-labeled, orange) specific probes (Abbott Molecular, Illinois, USA), was applied and covered by coverslips sealed with rubber cement. BCR DNA probe covers the whole 22q.11.2 chromosomal region including both BCR (22q11.23) and SMARCB1 (22q11.23) genes, therefore lack of one or two BCR signals indicate the deletion of SMARCB1 gene too. The sample and probe were denatured and hybridized using the ThermoBrite Denaturation/Hybridization System (Abbott Molecular) by programming 5 min of denaturation at 73 °C, followed by overnight hybridization at 37 °C. Post-hybridization wash was performed in 0.4 × SSC/0.1% NP-40 (73 °C, 2 min) followed by a wash in 2 × SSC/0.1% NP-40 (room temperature, 2 min). The slides were air dried in the dark, then counterstained with 10 μl of 4′,6′-diamidino-2-phenylindole from Vector Laboratories (Burlingame, CA, USA). The FISH signals were visualized by using filter sets and a Nikon Eclipse E600 epifluorescence microscope. Image analysis was performed by using Lucia Cytogenetics image acquisition system (Laboratory Imaging, Republic of Czech).
DNA and RNA Extraction
Genomic DNA (gDNA) and total RNA, for mutational analysis, promoter methylation study and gene expression profile, respectively, were isolated from paraffin-embedded materials in the SMARCB1 expression lacking cases by using RecoverAll Total Nucleic Acid Isolation Kit (Ambion, Austin, TX, USA), according to the respective manufacturers’ instructions. The concentration and integrity of nucleic acids were measured with NanoDrop 1000 (NanoDrop Technologies, Houston, TX, USA). In all, 500–1000 ng of RNA were reverse-transcribed using the High Capacity cDNA Reverse Transcription Kit (Applied Biosystems, Foster City, CA, USA) to prepare first-strand complementary DNA.
SMARCB1 Mutational Analysis
The sequences of the applied primers for exons 2–9 of the SMARCB1 gene (GenBank accession nos. Y17119–126) were the same as previously described K Kohashi et al.19 For the exon 1 (GenBank accession nos. Y17118) a new primer pair were designed: SMARCB1ex1F (5′-TCCTGATCCCTCGCAGCC-3′) and SMARCB1ex1R (5′-CCCGATGAATGGAGACGC-3′). Using the ABI Prism 310 sequence analyzer (Applied Biosystems), PCR products for individual exons were analyzed by direct sequencing. The sequence of individual exons was compared with the reported sequence in GenBank.
Methylation-Specific PCR
DNA (500–1000 ng) was bisulfited using the Cells-to-CpG Bisulfite Conversion Kit (Applied Biosystems) according to the specified protocol of the company. DNA extracted from peripheral blood mononuclear cells and amplificated with Repli-g kit (Qiagen, Hilden, Germany), totally unmethylated product was served as negative control for the methylation-specific PCR and as a template DNA for the methylation with CpG (M.SssI) Methyltransferase (New England Biolabs, Ipswich, MA, USA) as a methylated-positive control. Primers for methylation-specific PCR are designed to anneal specifically to CpG-rich sequences and, thus, selectively amplify either methylated DNA or unmethylated DNA in separate PCRs were shown in Table 2. Approximately 15 ng of the bisulfite-converted gDNA was used for PCR, but the functionally analyzable amounts were much less because of the compromised nature of formalin-fixed, paraffin-embedded samples and degradation during bisulfite conversion. Each of 45 PCR cycles included a denaturation step at 95 °C for 30 s, followed by annealing at 51–58 °C for 30 s and extension at 72 °C for 30 s. PCR products were analyzed by electrophoresis using a 2% agarose gel and visualized after staining with ethidium bromide. If an amplicon for both UM- and M-primer or for M-primer alone could be seen, the gene promoter could be considered methylated.
Laser Capture Microdissection
Laser capture microdissection was carried out with PALM laser microdissector (PALM, Bernried, Germany). Tissue specimens of 5 μm thickness from seven paraffin-embedded blocks were cut onto PALM membrane mounted glass slides. To avoid detachment of paraffin sections we irradiate with UV light at 254 nm for 30 min as it was advised by the manual. To facilitate the identification of the SMARCB1-negative tumor cells a rarely used immuno-laser capture microdissection strategy was applied. To ensure RNase-free conditions, we worked on sterile way during the immunohistochemistry. After deparaffinization and pressure-cooking antigen retrieval, the SMARCB1 immunostaining was done manually using the Max Polymer Detection System (Novolink, Novocastra, Newcastle, UK) to reveal antigen–antibody reaction. Immunostains were air dried for 30 min then two-step dissection was performed using PALM laser microdissector. Three thousand SMARCB1-negative tumor cells were dissected and collected into individual tubes from each case and immediately placed on ice. As positive control, SMARCB1 immunoreactive endothelial cells and lymphocytes were collected. RNA was extracted using the RNAqueus-Micro Kit (Ambion), according to the protocol for laser capture microdissection provided by the manual. Residual DNA was removed by DNase treatment as an optional step.
Quantitative Real-Time Reverse Transcriptase-PCR Analysis (qRT-PCR)
qRT-PCR was applied in order to examine the expression of SMARCB1 in epithelioid sarcoma samples and performed using LightCycler® 480 Resolight Dye (Roche Applied Science, Indianapolis, IN, USA) with AmpliTaq Gold® 360 DNA Polymerase (Applied Biosystems) and primers for SMARCB1 splice variants: SMARCB1sense (5′-TCCGTATGTTCCGAGGTTC-3′) and SMARCB1anti-sense (5′-CTTCCACTTCCGAGGCTTT-3′). Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was used as endogenous control and for calibrator normal human liver was applied. After enzyme activation at 95 °C for 5 min, 45 PCR cycles were performed (denaturation at 95 °C for 10 s, annealing at 59 °C for 10 s and extension at 72 °C for 20 s). Gene expression levels were calculated and determined using the crossing point (CP) values . From the formalin-fixed, paraffin-embedded blocks, we got heterogeneous tissue (containing mainly tumor cells but also normal endothelial, lymphoid, etc, cells), but to obtain pure tumor RNA, that was not possible. Therefore, we performed laser capture microdissection to collect only tumor cells.
Primer Design for Methylation-Specific PCR
Primers were designed to discriminate between methylated and unmethylated alleles following bisulfite treatment and to discriminate between bisulfate modified and unmodified DNA. As the two strands of DNA are no longer complementary after bisulfite treatment, primers can be designed for either modified strand. For convenience, we have designed primers for the sense strand. Short amplicons, between 80 and 117 bp were designed. The primers and annealing temperatures have been described previously (Table 2).
Methylation Analysis of the CpG Islands in the Promoter Region Using Methylation-Specific PCR
The SMARCB1 gene sequence contains many CpG islands. For the methylation analysis, CpG islands with 600 bp of DNA sequence (located in chromosome 22:24129097–24129696 based on UCSC Genome Browser) were chosen. This region is the promoter of the gene and overlap with the sequence of the first exon. To assess the methylation status of all cytosines within the region, we employed the sodium bisulfite treatment and methylation-specific PCR. After treatment with sodium bisulfite, unmethylated cytosines in the DNA were converted to uracils, whereas 5-methylcytosines remained as cytosines. After removal of the bisulfite and completion of the chemical conversion, this modified DNA was used as a template for PCR. With our primers, we could examine altogether 37 different CpG-s in the promoter region.
Results
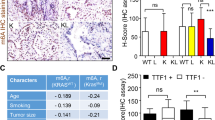
Histology, Immunohistochemistry
Of 36 epithelioid sarcoma cases, 20 (56%) were distal and 16 (45%) proximal type. In 31 (86%) cases, there was no detectable expression of the SMARCB1 gene product in tumor cells with the anti-BAF47 antibody, whereas infiltrating lymphocytes and entrapped non-tumor tissue displayed immunoreactivity. Epithelioid sarcoma cases were characterized as follows: vimentin diffuse positivity, keratin (AE1/AE3) and/or EMA at least focal strong positivity, S100 negativity and SMARCB1 negativity (31 cases; Figure 1). In 5 (14%) SMARCB1-positive cases, there was also CD34 positivity confirming the diagnosis of epithelioid sarcoma (Figure 2). Immunohistology data are summarized in Table 1. All 36 epithelioid sarcoma cases were evaluated and scored for EZH2 protein expression. The mean score was 2.97, which meant that EZH2 overexpression is not a general feature of epithelioid sarcoma (mean 2.97, s.d. 1.56). Twenty-five cases (69%) had a score of 3 or less (mean 2.2, s.d. 1.08) therefore they were considered to be EZH2 negative. The remaining 11 (31%) cases were regarded as positive (mean 4.73, s.d. 0.90; Figure 3) including 9 proximal type and 2 distal type. The highest score 6 was observed, however, only in three (8%) proximal-type cases, based on the age of the patients, location and lack of mutation of the SMARCB1 gene, which is otherwise typical for malignant rhabdoid tumor.20
Typical picture of distal-type epithelioid sarcoma: tumor cells with abundant eosinophilic cytoplasm and small nucleoli (a; H&E stain; 20 × ). Characteristic coexpression of vimentin (b; 20 × ) and cytokeratin (AE1–AE3) (c; 20 × ) is evident. SMARCB1 negativity is obvious in tumor cells while normal stromal cells and lymphocytes are positive (d; 40 × ; case number: 29).
Distal (a; H&E stain; 40 × ) and proximal-type (b; H&E stain; 20 × ) epithelioid sarcoma with EZH2 complete negativity (c; 40 × ) and with strong positivity (d; 20 × ), (c, d: EZH2 immunohistochemistry), (case number 21: a, c; case number 5: b, d). EZH2 positivity (4 or more score) was not a characteristic feature of epithelioid sarcoma.
Deletion and Mutation in SMARCB1
As stated previously, loss of BCR FISH signal also indicate SMARCB1 gene deletion. The ABL gene located on chromosome 9 was regarded as a positive control. Deletion of both BCR alleles results in loss of nuclear protein expression. Four cases showed tumor cells without detectable BCR by FISH in their nucleus and were regarded as biallelic deletion of BCR/SMARCB1. Single-allelic deletion of BCR/SMARCB1 with one BCR signal in the tumor cells was found in 11 cases. In the remaining 16 cases, chromosomal abnormalities could not be detected. Tetrasomy was observed in four cases. Among those 11 cases that showed one allelic deletion, two of them revealed mutation of the retained allele (sequencing all nine exons of the SMARCB1 gene). One of them displayed a deletion in the exon 3 resulting in a frameshift and the other showed a single basepair point mutation in the exon 7. Altogether, we found six cases with genetic aberrations (biallelic alteration) that explain the loss of SMARCB1 function (Figure 4).
Genetic examination of the SMARCB1 gene using FISH (red signals correspond to ABL and green signals to BCR/SMARCB1) and direct sequencing. Left cell showing normal 2–2 signals and right cell displays deletion of one allele of BCR/SMARCB1 gene (a); in the same case sequence profile for a point mutation (GGG/AGG) of exon 7 was observed (b), indicating biallelic damage of SMARCB1 gene (case number 15). Upper normal cell with 2–2 signals and lower cell showing biallelic deletion of BCR/SMARCB1 gene (c; case number: 8).
Methylation Status
First, we tested the primers (designed for CpG islands of SMARCB1 promoter) on negative and positive control DNAs, described previously in Materials and methods section. The whole genome amplified sample, which contains only unmethylated alleles, resulted in PCR products only with unmethylated primers sets, whereas the in vitro (M.SssI methyltransferase) methylated DNA resulted in PCR products with both the methylated and unmethylated primer set. This methylation heterogeneity (methylated and unmethylated products) in our positive sample suggested that the in vitro methylation of the DNA was not totally 100% effective but still clearly indicating the reliability of this method. Twenty-five tumor DNA (bisulfite converted) samples (displaying no biallelic mutation/deletion in the SMARCB1 gene) were analyzed. Methylation-specific PCR was performed using all the designed 14 methylated- and unmethylated-specific primers. Methylation-specific PCR analysis revealed that there were no methylated alleles in the promoter region of SMARCB1, so this tumor-suppressor gene displayed unmethylated status in epithelioid sarcoma (Figure 5).
Methylation-specific PCR of the SMARCB1 gene promoter. Amplification of bisulfite-treated epithelioid sarcoma DNA: note, there are no bands with the methylated primers (a). Pre-amplificated/unmethylated DNA (negative control) (b) and in vitro methylated DNA (positive control) (c) with SMARCB1 methylated and unmethylated-specific primer sets. Primer sets used for amplification are designated as methylated (M) and unmethylated (μM). *Molecular weight marker 1 kb Plus DNA Ladder (Life Technologies, Carlsbad, CA, USA). The accurate size of methylation-specific PCR products are shown in Table 2.
Examination of the SMARCB1 Gene Expression by qRT-PCR
As a result of investigation of the SMARCB1 gene expression, low level of SMARCB1 mRNA was found in RNA samples (16 cases) extracted from tissue blocks (9 cases could not be studied because of degradation of their RNA). We suspected that the stromal or other normal cells (eg, endothelium, lymphocyte, fibroblast, etc) might cause contamination and it results in the appearance of the SMARCB1 mRNA in a variable expression levels among tumor samples depending on the ratio of normal and tumor tissue. Therefore, we decided to carry out laser capture microdissection to collect only tumor cells, which showed no expression of SMARCB1 gene; correspondingly, mRNA could not be detected. For a positive control, we also collected individual stromal and/or normal cells from the tumor-free area, which revealed increased levels of SMARCB1 transcript. GAPDH was amplified in all examined cases as an endogenous control, indicating the presence of mRNA in each sample (Figure 6).
Results of SMARCB1 gene expression from paraffin slides of epithelioid sarcomas. Quantification of mRNA levels for SMARCB1 as determined by qRT-PCR analysis. The data represent mean±s.d. Note the different, usually low levels of individual cases compared with calibrator normal tissue (liver) (a). SMARCB1 immunohistochemistry, performed on membrane mounted slide specific for laser capture microdissection (case number: 5). Note the SMARCB1-negative tumor cells and SMARCB1-positive lymphocytes (b; 40 × ). In the course of laser capture microdissection, SMARCB1-negative tumor cells (c; 40 × ) and lymphocytes (d; 40 × ) were separately dissected for qRT-PCR. Amplification curves of GAPDH (from left to right curve 1 represents lymphocytes, curve 2 tumor cells), SMARCB1 (curve 3 shows lymphocytes); the bottom straight line indicates tumor cells with no amplification of SMARCB1 mRNA (e; the same fifth case).
Discussion
Epigenetic changes may explain hallmark features of cancers and may produce the same effect as genetic damages. A good example is the malignant rhabdoid tumor—epithelioid sarcoma carcinogenesis with the same SMARCB1 protein loss of both tumors but with genetic changes in the malignant rhabdoid tumor and epigenetic changes in epithelioid sarcoma. Epigenetic changes can occur on three levels in general; DNA, RNA and protein, resulting in the same effect as mutation. Hypermethylation of DNA promoter region and histone methylation via EZH2 overexpression of suppressor genes are well known and extensively investigated causes of carcinogenesis and sarcomagenesis. CpG islands are quite numerous in the promoter region of the SMARCB1 gene, suggesting a possible hypermethylation mechanism for gene silencing. In our study, we wanted to determine whether DNA or histone methylation of the promoter region of SMARCB1 could result in nuclear SMARCB1 protein loss in epithelioid sarcoma using methylation-specific PCR and EZH2 immunohistochemistry.
Biallelic damage of the SMARCB1 gene on chromosome 22q11.2 and the consequent absence of nuclear staining of SMARCB1 were first recognized back in 1990 in malignant rhabdoid tumors and were thought as being a specific and characteristic mark for this tumor.21 However, very recently it was shown that loss of SMARCB1 nuclear protein is characteristic for a variety of soft tissue tumors, especially for epithelioid sarcoma. In fact, approximately 90% of epithelioid sarcoma cases have negative nuclear staining. At the same time, it was also revealed that the mechanism of SMARCB1 protein loss is different because the vast majority of epithelioid sarcoma cases did not harbor biallelic mutation of the SMARCB1 gene. This result suggests that epigenetic events may be responsible.
In our study, the initial step was to select the SMARCB1-negative cases and from the negative cases to exclude those cases, which displayed biallelic alterations. We found 31 (86%) SMARCB1-negative epithelioid sarcoma and from these cases, 6 (19%) contained biallelic alterations, thus 25 cases for methylation analysis remained. Our results are in good harmony with others, except the ratio of biallelic mutant cases, which is slightly higher than Kohashi et al.10 This can be explained by the fact that our analysis is the third one in this regard and therefore there are not much data to compare.
The published data regarding the promoter methylation status of SMARCB1 gene are limited. To our best knowledge, only one article investigated the promoter methylation status of SMARCB1 gene in malignant rhabdoid tumor is available which showed no hypermethylation.22 Therefore, we used chemically induced methylation as positive control for the quality assurance of our designed primer sets. To our surprise, we found no hypermethylation in any of our 25 cases using positive and negative controls. We designed 14 methylated and unmethylated-specific primers for this purpose, covering about 40% of the CpG islands of the promoter region. In general, a single methylated and unmethylated primer is sufficient to detect promoter methylation, as it means that the other CpG islands are also methylated.23, 24 The unmethylated DNA status of the promoter region suggests an epigenetic event not on the DNA level, such as histone methylation. EZH2 is the enzymatically active component of the PRC2, which catalyzes the repressive histone methylation H3K27m3 mark thus resulting in gene silencing. We tested the possible overexpression of EZH2 in our 36 epithelioid sarcoma cases and found that EZH2 overexpression is not a general feature of epithelioid sarcoma. The mean score was 2.97, which means the majority of epithelioid sarcoma cases are EZH2 negative. In fact, we found only three cases with the highest score of 6 (each proximal type) indicating that strong positivity is a very rare event among epithelioid sarcomas. In contrast, EZH2 is usually strongly positive in most ‘blastic’ tumors such as neuroblastoma, Ewing sarcoma, alveolar rhabdomyosarcoma, malignant rhabdoid tumor,25, 26 but in these tumors the SMARCB1 nuclear protein is intact except in the malignant rhabdoid tumor where genetic damage occurs. It is well known that repression of E-cadherin by EZH2 is associated with the aggressiveness of many carcinomas,27 but it is still not clear what kind of other genes are silenced by EZH2 in different tumors, although it seems that SMARCB1 is not affected. To our best knowledge, this is the first report of larger series of EZH2 expression in epithelioid sarcoma although five cases with a 16% labeling index were reported by Yamaga K et al.28 It is possible, although unlikely, that the H3K27me3 mark is present without overexpression of EZH2, which could be assessed by chromatin immunoprecipitation followed by PCR.
If there is no epigenetic change on a DNA level, the next step is to examine the mRNA level. We could get proper RNA from 16 out of 25 cases using tissue blocks. In each case, a low but variable level of SMARCB1 mRNA was found depending on the ratio of normal to tumor tissue. It was unknown whether this meant a total lack of expression or low levels of expression. To clarify this issue, we chose seven cases for laser capture microdissection, including cases with very low and also with higher levels of mRNA. Separating tumor cells and normal control cells, tumor cells contained no detectable mRNA, whereas normal cells and the internal control of GAPDH displayed equivalent expression. A lack of mRNA of SMARCB1 gene means that neither normal nor altered SMARCB1 protein exists, ruling out the possibility of epigenetic changes on the protein level, such as protein degradation. These results suggest that the SMARCB1 mRNA is produced then silenced by expression of microRNA. Gene silencing by microRNA resulting in a decreased level or lack of mRNA is a well-known epigenetic mechanism in different tumors.29
In our study, we confirm that the majority of epithelioid sarcomas do not harbor biallelic genetic alterations of the SMARCB1 gene but could not prove the putative role of hypermethylation of DNA and/or histone methylation to silence gene activity. The absence of SMARCB1 mRNA clarifies that altered protein is not responsible and calls attention to the possible role of microRNA. It seems that although the malignant rhabdoid tumor and epithelioid sarcoma (especially proximal type) share morphologic features as well as loss of expression of the SMARCB1 protein, they differ in the molecular mechanisms leading to loss of SMARCB1 protein expression. Indeed, malignant rhabdoid tumors frequently show biallelic loss of the SMARCB1 locus, whereas loss of SMARCB1 in epithelioid sarcomas appears to depend on epigenetic mechanisms.
Accession codes
References
Kalpana GV, Marmon S, Wang W et al. Binding and stimulation of HIV-1 integrase by a human homolog of yeast transcription factor SNF5. Science 1994;266:2002–2006.
Reisman D, Glaros S, Thompson EA . The SWI/SNF complex and cancer. Oncogene 2009;28:1653–1668.
Versteege I, Sevenet N, Lange J et al. Truncating mutations of hSNF5/INI1 in aggressive paediatric cancer. Nature 1998;394:203–206.
Hollmann TJ, Hornick JL . INI1-deficient tumors: diagnostic features and molecular genetics. Am J Surg Pathol 2011;35:e47–e63.
Enzinger FM . Epitheloid sarcoma. A sarcoma simulating a granuloma or a carcinoma. Cancer 1970;26:1029–1041.
Chase DR, Enzinger FM . Epithelioid sarcoma. Diagnosis, prognostic indicators, and treatment. Am J Surg Pathol 1985;9:241–263.
Modena P, Lualdi E, Facchinetti F et al. SMARCB1/INI1 tumor suppressor gene is frequently inactivated in epithelioid sarcomas. Cancer Res 2005;65:4012–4019.
Chbani L, Guillou L, Terrier P et al. Epithelioid sarcoma: a clinicopathologic and immunohistochemical analysis of 106 cases from the French sarcoma group. Am J Clin Pathol 2009;131:222–227.
Hornick JL, Dal Cin P, Fletcher CD . Loss of INI1 expression is characteristic of both conventional and proximal-type epithelioid sarcoma. Am J Surg Pathol 2009;33:542–550.
Kohashi K, Izumi T, Oda Y et al. Infrequent SMARCB1/INI1 gene alteration in epithelioid sarcoma: a useful tool in distinguishing epithelioid sarcoma from malignant rhabdoid tumor. Hum Pathol 2009;40:349–355.
Herman JG, Baylin SB . Gene silencing in cancer in association with promoter hypermethylation. N Engl J Med 2003;349:2042–2054.
Belinsky SA . Gene-promoter hypermethylation as a biomarker in lung cancer. Nat Rev Cancer 2004;4:707–717.
Cao R, Wang L, Wang H et al. Role of histone H3 lysine 27 methylation in Polycomb-group silencing. Science 2002;298:1039–1043.
Varambally S, Dhanasekaran SM, Zhou M et al. The polycomb group protein EZH2 is involved in progression of prostate cancer. Nature 2002;419:624–629.
Kleer CG, Cao Q, Varambally S et al. EZH2 is a marker of aggressive breast cancer and promotes neoplastic transformation of breast epithelial cells. Proc Natl Acad Sci USA 2003;100:11606–11611.
Simon JA, Lange CA . Roles of the EZH2 histone methyltransferase in cancer epigenetics. Mutat Res 2008;647:21–29.
Ciarapica R, Miele L, Giordano A et al. Enhancer of zeste homolog 2 (EZH2) in pediatric soft tissue sarcomas: first implications. BMC Med 2011;9:63.
Pacheco M, Nielsen TO . Histone deacetylase 1 and 2 in mesenchymal tumors. Mod Pathol 2012;25:222–230.
Kohashi K, Oda Y, Yamamoto H et al. Highly aggressive behavior of malignant rhabdoid tumor: a special reference to SMARCB1/INI1 gene alterations using molecular genetic analysis including quantitative real-time PCR. J Cancer Res Clin Oncol 2007;133:817–824.
Venneti S, Le P, Martinez D et al. Malignant rhabdoid tumors express stem cell factors, which relate to the expression of EZH2 and Id proteins. Am J Surg Pathol 2011;35:1463–1472.
Handgretinger R, Kimmig A, Koscielnak E et al. Establishment and characterization of a cell line (Wa-2) derived from an extrarenal rhabdoid tumor. Cancer Res 1990;50:2177–2182.
Zhang F, Tan L, Wainwright LM et al. No evidence for hypermethylation of the hSNF5/INI1 promoter in pediatric rhabdoid tumors. Genes Chromosomes Cancer 2002;34:398–405.
Skiriute D, Vaitkiene P, Saferis V et al. MGMT, GATA6, CD81, DR4, and CASP8 gene promoter methylation in glioblastom. BMC Cancer 2012;12:218.
Wang D, Chen Q, Zhang C et al. DNA hypomethylation of the COX-2 gene promoter is associated with up-regulation of its mRNA expression in eutopic endometrium of endometriosis. Eur J Med Res 2012;17:12.
Wang C, Liu Z, Woo CW et al. EZH2 Mediates epigenetic silencing of neuroblastoma suppressor genes CASZ1, CLU, RUNX3, and NGFR. Cancer Res 2012;72:315–324.
Burdach S, Plehm S, Unland R et al. Epigenetic maintenance of stemness and malignancy in peripheral neuroectodermal tumors by EZH2. Cell Cycle 2009;8:1991–1996.
Cao Q, Yu J, Dhanasekaran SM et al. Repression of E-cadherin by the polycomb group protein EZH2 in cancer. Oncogene 2008;27:7274–7284.
Yamaga K, Osaki M, Kidani K et al. High expression of enhancer of zeste homologue 2 indicates poor prognosis in patients with soft tissue sarcomas. Mol Med Report 2008;1:633–639.
Cowland JB, Hother C, Gronbaek K . MicroRNAs and cancer. APMIS 2007;115:1090–1106.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Papp, G., Changchien, YC., Péterfia, B. et al. SMARCB1 protein and mRNA loss is not caused by promoter and histone hypermethylation in epithelioid sarcoma. Mod Pathol 26, 393–403 (2013). https://doi.org/10.1038/modpathol.2012.190
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2012.190
Keywords
This article is cited by
-
Molecular and immunophenotypic characterization of SMARCB1 (INI1) - deficient intrathoracic Neoplasms
Modern Pathology (2022)
-
A case of primary distal-type epithelioid sarcoma of the lumbar vertebra with a review of literature
Virchows Archiv (2021)
-
Downregulation of SMARCB1/INI1 expression in pediatric chordomas correlates with upregulation of miR-671-5p and miR-193a-5p expressions
Brain Tumor Pathology (2017)
-
Differential microRNA expression profiles between malignant rhabdoid tumor and epithelioid sarcoma: miR193a-5p is suggested to downregulate SMARCB1 mRNA expression
Modern Pathology (2014)
-
The chromatin remodelling component SMARCB1/INI1 influences the metastatic behavior of colorectal cancer through a gene signature mapping to chromosome 22
Journal of Translational Medicine (2013)